Abstract
Renal cell carcinoma (RCC) represents over 80 % of kidney cancer, and about 30 % of the patients with RCC develop metastasis after the surgery. Invasion of basement membrane (BM) and extracellular matrix (ECM) is an essential event in tumor invasion and metastasis. Matrix metalloproteinases (MMPs), which digest the main components of BM and ECM, are expressed in RCC. Heparanase, which degrades heparan sulfate proteoglycans, is predominantly expressed in high-grade RCCs with a positive correlation with pathological tumor stage and poor prognosis. Bone metastasis is common among the patients with RCC, and increased osteoclastic activity was observed at metastatic sites. Receptor activator of nuclear factor κB ligand (RANKL), which plays an important role in osteoclastogenesis, is predominantly expressed in high-grade RCC and its expression level is associated with bone metastasis and prognosis. Epithelial-mesenchymal transition (EMT), a switch of epithelial cells to sarcomatoid phenotype, is considered to be critical step during metastasis, and Snail, a major regulator of EMT, is predominantly expressed in high-grade RCC, and high Snail expression is a worse prognostic factor. Accordingly, heparanase, RANKL and Snail may be targets for the development of anti-tumor therapies for RCCs.



Similar content being viewed by others
References
Eble JN, Sauter G, Epstein JI, Sesterhenn IA (eds) (2005) World Health Organization Classification of Tumors. Pathology and Genetics of Tumors of the Urinary System and Male Genital Organs. IARC Press, Lyon
Jung K, Lein M, Laube C, Lichtinghagen R (2001) Blood specimen collection methods influence the concentration and the diagnostic validity of matrix metalloproteinase 9 in blood. Clin Chim Acta 314:241–244
Fuhrman SA, Lasky LC, Limas C (1982) Prognostic significance of morphologic parameters in renal cell carcinoma. Am J Surg Pathol 6:655–663
Jung K, Nowak L, Lein M, Priem F, Schnorr D, Loening SA (1997) Matrix metalloproteinases 1 and 3, tissue inhibitor of metalloproteinase-1 and the complex of metalloproteinase-1/tissue inhibitor in plasma of patients with prostate cancer. Int J Cancer 74:220–223
Janzen NK, Kim HL, Figlin RA, Belldegrun AS (2003) Surveillance after radical or partial nephrectomy for localized renal cell carcinoma and management of recurrent disease. Urol Clin North Am 30:843–852
Suzuki K, Mizuno R, Mikami S, Tanaka N, Kanao K, Kikuchi E, Miyajima A, Nakagawa K, Oya M (2012) Prognostic significance of high nuclear grade in patients with pathologic T1a renal cell carcinoma. Jpn J Clin Oncol 42:831–835
Eccles SA (1999) Heparanase: breaking down barriers in tumors. Nat Med 5:735–736
Engbring JA, Kleinman HK (2003) The basement membrane matrix in malignancy. J Pathol 200:465–470
Chambers AF, Matrisian LM (1997) Changing views of the role of matrix metalloproteinases in metastasis. J Natl Cancer Inst 89:1260–1270
Curran S, Murray GI (2000) Matrix metalloproteinases: molecular aspects of their roles in tumour invasion and metastasis. Eur J Cancer 36:1621–1630
Shiomi T, Lemaitre V, D’Armiento J, Okada Y (2010) Matrix metalloproteinases, a disintegrin and metalloproteinases, and a disintegrin and metalloproteinases with thrombospondin motifs in non-neoplastic diseases. Pathol Int 60:477–496
Kugler A, Hemmerlein B, Thelen P, Kallerhoff M, Radzun HJ, Ringert RH (1998) Expression of metalloproteinase 2 and 9 and their inhibitors in renal cell carcinoma. J Urol 160:1914–1918
Lein M, Jung K, Laube C, Hubner T, Winkelmann B, Stephan C, Hauptmann S, Rudolph B, Schnorr D, Loening SA (2000) Matrix-metalloproteinases and their inhibitors in plasma and tumor tissue of patients with renal cell carcinoma. Int J Cancer 85:801–804
Vlodavsky I, Beckhove P, Lerner I, Pisano C, Meirovitz A, Ilan N, Elkin M (2012) Significance of heparanase in cancer and inflammation. Cancer Microenviron 5:115–832
Nakajima M, Irimura T, Di Ferrante N, Nicolson GL (1984) Metastatic melanoma cell heparanase. Characterization of heparan sulfate degradation fragments produced by B16 melanoma endoglucuronidase. J Biol Chem 259:2283–2290
Dall’Oglio MF, Ribeiro-Filho LA, Antunes AA, Crippa A, Nesrallah L, Goncalves PD, Leite KR, Srougi M (2007) Microvascular tumor invasion, tumor size and Fuhrman grade: a pathological triad for prognostic evaluation of renal cell carcinoma. J Urol 178:425–428
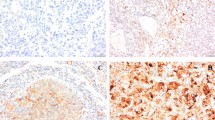
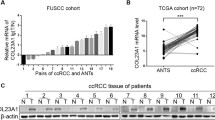
Mikami S, Oya M, Shimoda M, Mizuno R, Ishida M, Kosaka T, Mukai M, Nakajima M, Okada Y (2008) Expression of heparanase in renal cell carcinomas: implications for tumor invasion and prognosis. Clin Cancer Res 14:6055–6061
Zekri J, Ahmed N, Coleman RE, Hancock BW (2001) The skeletal metastatic complications of renal cell carcinoma. Int J Oncol 19:379–382
Dougall WC (2012) Molecular pathways: osteoclast-dependent and osteoclast-independent roles of the RANKL/RANK/OPG pathway in tumorigenesis and metastasis. Clin Cancer Res 18:326–335
Wittrant Y, Theoleyre S, Chipoy C, Padrines M, Blanchard F, Heymann D, Redini F (2004) RANKL/RANK/OPG: new therapeutic targets in bone tumours and associated osteolysis. Biochim Biophys Acta 1704:49–57
Zhang J, Dai J, Yao Z, Lu Y, Dougall W, Keller ET (2003) Soluble receptor activator of nuclear factor κB Fc diminishes prostate cancer progression in bone. Cancer Res 63:7883–7890
Jones DH, Nakashima T, Sanchez OH, Kozieradzki I, Komarova SV, Sarosi I, Morony S, Rubin E, Sarao R, Hojilla CV, Komnenovic V, Kong YY, Schreiber M, Dixon SJ, Sims SM, Khokha R, Wada T, Penninger JM (2006) Regulation of cancer cell migration and bone metastasis by RANKL. Nature 440:692–696
Wittrant Y, Lamoureux F, Mori K, Riet A, Kamijo A, Heymann D, Redini F (2006) RANKL directly induces bone morphogenetic protein-2 expression in RANK-expressing POS-1 osteosarcoma cells. Int J Oncol 28:261–269
Mikami S, Katsube K, Oya M, Ishida M, Kosaka T, Mizuno R, Mochizuki S, Ikeda T, Mukai M, Okada Y (2009) Increased RANKL expression is related to tumour migration and metastasis of renal cell carcinomas. J Pathol 218:530–539
Lipton A, Fizazi K, Stopeck AT, Henry DH, Brown JE, Yardley DA, Richardson GE, Siena S, Maroto P, Clemens M, Bilynskyy B, Charu V, Beuzeboc P, Rader M, Viniegra M, Saad F, Ke C, Braun A, Jun S (2012) Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: a combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer 48:3082–3092
Keizman D, Ish-Shalom M, Maimon N, Gottfried M (2013) Are bisphosphonates an indispensable tool in the era of targeted therapy for renal cell carcinoma and bone metastases? World J Urol (in press)
Kijima T, Fujii Y, Suyama T, Okubo Y, Yamamoto S, Masuda H, Yonese J, Fukui I (2009) Radiotherapy to bone metastases from renal cell carcinoma with or without zoledronate. BJU Int 103:620–624
Nieto MA (2011) The ins and outs of the epithelial to mesenchymal transition in health and disease. Annu Rev Cell Dev Biol 27:347–376
Grunert S, Jechlinger M, Beug H (2003) Diverse cellular and molecular mechanisms contribute to epithelial plasticity and metastasis. Nat Rev Mol Cell Biol 4:657–665
Canel M, Serrels A, Frame MC, Brunton VG (2013) E-cadherin-integrin crosstalk in cancer invasion and metastasis. J Cell Sci 126:393–401
Thiery JP (2003) Epithelial-mesenchymal transitions in development and pathologies. Curr Opin Cell Biol 15:740–746
Alves CC, Carneiro F, Hoefler H, Becker KF (2009) Role of the epithelial-mesenchymal transition regulator Slug in primary human cancers. Front Biosci 14:3035–3050
Batlle E, Sancho E, Franci C, Dominguez D, Monfar M, Baulida J, Garcia De Herreros A (2000) The transcription factor snail is a repressor of E-cadherin gene expression in epithelial tumour cells. Nat Cell Biol 2:84–89
Katagiri A, Watanabe R, Tomita Y (1995) E-cadherin expression in renal cell cancer and its significance in metastasis and survival. Br J Cancer 71:376–379
Esteban MA, Tran MG, Harten SK, Hill P, Castellanos MC, Chandra A, Raval R, O’Brien TS, Maxwell PH (2006) Regulation of E-cadherin expression by VHL and hypoxia-inducible factor. Cancer Res 66:3567–3575
Evans AJ, Russell RC, Roche O, Burry TN, Fish JE, Chow VW, Kim WY, Saravanan A, Maynard MA, Gervais ML, Sufan RI, Roberts AM, Wilson LA, Betten M, Vandewalle C, Berx G, Marsden PA, Irwin MS, Teh BT, Jewett MA, Ohh M (2007) VHL promotes E2 box-dependent E-cadherin transcription by HIF-mediated regulation of SIP1 and snail. Mol Cell Biol 27:157–169
Harten SK, Shukla D, Barod R, Hergovich A, Balda MS, Matter K, Esteban MA, Maxwell PH (2009) Regulation of renal epithelial tight junctions by the von Hippel–Lindau tumor suppressor gene involves occludin and claudin 1 and is independent of E-cadherin. Mol Biol Cell 20:1089–1101
Mikami S, Katsube K, Oya M, Ishida M, Kosaka T, Mizuno R, Mukai M, Okada Y (2011) Expression of Snail and Slug in renal cell carcinoma: E-cadherin repressor Snail is associated with cancer invasion and prognosis. Lab Invest 91:1443–1458
Acknowledgments
This work was supported in part by Grant-in-Aid for Scientific Research (C) (No. 25460422) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan (MEXT) (S.M.), Grain-in-Aid for Scientific Research (B) (No. 24390374) from MEXT (M.O.), and Grant-in-Aid for Scientific Research (A) (No. 24249022) from MEXT (Y.O.) and Third Term 10-year Strategy for Cancer Control (Y.O.) from the Foundation of Promotion of Cancer Research, and Project for Development of Innovative Research on Cancer Therapeutics (P-Direct) from MEXT (S. M., R.M, T.K. and M.O.).
Conflicts of interest
None of the authors has any conflicts of interest associated with this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was shown in the symposium, “Molecular and Morphological approach of research on renal cell carcinoma”, at the Annual Meeting and Scientific Assembly of the 44th Annual Meeting of the Japanese Society for Clinical Molecular Morphology as “atypia of the renal cell carcinoma, invasion and metastasis” and was invited for submission to Medical Molecular Morphology.
Rights and permissions
About this article
Cite this article
Mikami, S., Oya, M., Mizuno, R. et al. Invasion and metastasis of renal cell carcinoma. Med Mol Morphol 47, 63–67 (2014). https://doi.org/10.1007/s00795-013-0064-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00795-013-0064-6