Abstract
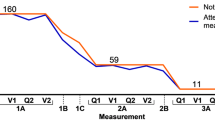
The present study describes the pathological progression of longitudinally followed cases with levodopa-responsive Parkinson’s disease who came to autopsy during the Sydney Multicenter Study of Parkinson’s disease. Standardised clinical and neuropathological assessments over five epochs of time verified three different clinicopathological groups. A group of younger onset patients with a typical long duration clinical course of Parkinson’s disease. This group of cases had Lewy body distributions consistent with the Braak staging of disease. In this group, brainstem Lewy bodies dominate in those surviving to 5 years; by 13 years, 50% of cases have a limbic distribution of Lewy bodies; and by 18 years, all will have at least this pathological phenotype. Approximately 25% of cases had an early malignant, dementia-dominant syndrome and severe neocortical disease consistent with dementia with Lewy bodies. The last group had an older onset, shorter survival, and a more complex disease course with higher Lewy body loads and a higher proportion with additional neuropathologies. These cases with higher loads of Lewy bodies and shorter survivals suggest that widespread Lewy body pathology either occurs at the onset of clinical disease or rapidly infiltrates the brain. In these cases with shorter survivals, there was more plaque pathology, supporting a more aggressive and linked phenotype. Our data suggest that the selection of similar study cohorts by pathology alone would not be able to differentiate the three different phenotypes identified. The data are also not consistent with a unitary concept of the pathogenesis of Lewy body disease.
Similar content being viewed by others
References
Beyer MK, Larsen JP, Aarsland D (2007) Gray matter atrophy in Parkinson disease with dementia and dementia with Lewy bodies. Neurology 69:747–754
Braak H, Del Tredici K, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Braak H, Rub U, Jansen Steur EN, Del Tredici K, de Vos RA (2005) Cognitive status correlates with neuropathologic stage in Parkinson disease. Neurology 64:1404–1410
Braak H, Rub U, Del Tredici K (2006) Cognitive decline correlates with neuropathological stage in Parkinson’s disease. J Neurol Sci 248:255–258
Fenelon G, Mahieux F, Huon R, Ziegler M (2000) Hallucinations in Parkinson’s disease: prevalence, phenomenology and risk factors. Brain 123(Pt 4):733–745
Galvin JE, Pollack J, Morris JC (2006) Clinical phenotype of Parkinson disease dementia. Neurology 67:1605–1611
Halliday G, Ng T, Rodriguez M, Harding A, Blumbergs P, Evans W, Fabian V, Fryer J, Gonzales M, Harper C, Kalnins R, Masters CL, McLean C, Milder DG, Pamphlett R, Scott G, Tannenberg A, Kril J (2002) Consensus neuropathological diagnosis of common dementia syndromes: testing and standardising the use of multiple diagnostic criteria. Acta Neuropathol 104:72–78
Harding AJ, Broe GA, Halliday GM (2002) Visual hallucinations in Lewy body disease relate to Lewy bodies in the temporal lobe. Brain 125:391–403
Hely MA, Morris JG, Rail D, Reid WG, O’Sullivan DJ, Williamson PM, Genge S, Broe GA (1989) The Sydney Multicentre Study of Parkinson’s disease: a report on the first 3 years. J Neurol Neurosurg Psychiatry 52:324–328
Hely MA, Morris JG, Reid WG, O’Sullivan DJ, Williamson PM, Rail D, Broe GA, Margrie S (1994) The Sydney Multicentre Study of Parkinson’s disease: a randomised, prospective five year study comparing low dose bromocriptine with low dose levodopa–carbidopa. J Neurol Neurosurg Psychiatry 57:903–910
Hely MA, Morris JG, Traficante R, Reid WG, O’Sullivan DJ, Williamson PM (1999) The Sydney Multicentre Study of Parkinson’s disease: progression and mortality at 10 years. J Neurol Neurosurg Psychiatry 67:300–307
Hely MA, Morris JG, Reid WG, Trafficante R (2005) Sydney Multicenter Study of Parkinson’s disease: non-l-dopa-responsive problems dominate at 15 years. Mov Disord 20:190–199
Hely MA, Morris JGL, Reid WGJ, Adena MA, Halliday GM (2008) Sydney Multicenter Study of Parkinson’s disease: the inevitability of dementia at 20 years. Mov Disord (in press)
Hurtig HI, Trojanowski JQ, Galvin J, Ewbank D, Schmidt ML, Lee VM, Clark CM, Glosser G, Stern MB, Gollomp SM, Arnold SE (2000) Alpha-synuclein cortical Lewy bodies correlate with dementia in Parkinson’s disease. Neurology 54:1916–1921
Jellinger KA, Seppi K, Wenning GK, Poewe W (2002) Impact of coexistent Alzheimer pathology on the natural history of Parkinson’s disease. J Neural Transm 109:329–339
Jellinger KA, Wenning GK, Seppi K (2007) Predictors of survival in dementia with lewy bodies and Parkinson dementia. Neurodegener Dis 4:428–430
Kempster PA, Williams DR, Selikhova M, Holton J, Revesz T, Lees AJ (2007) Patterns of levodopa response in Parkinson’s disease: a clinico-pathological study. Brain 130:2123–2128
Levy G (2007) The relationship of Parkinson disease with aging. Arch Neurol 64:1242–1246
Lewis SJ, Foltynie T, Blackwell AD, Robbins TW, Owen AM, Barker RA (2005) Heterogeneity of Parkinson’s disease in the early clinical stages using a data driven approach. J Neurol Neurosurg Psychiatry 76:343–348
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del Ser T, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A, Kosaka K, Lee VM, Lees A, Litvan I, Londos E, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ, Yamada M (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65:1863–1872
Papapetropoulos S, Gonzalez J, Lieberman A, Villar JM, Mash DC (2005) Dementia in Parkinson’s disease: a post-mortem study in a population of brain donors. Int J Geriatr Psychiatry 20:418–422
Parkkinen L, Kauppinen T, Pirttila T, Autere JM, Alafuzoff I (2005) Alpha-synuclein pathology does not predict extrapyramidal symptoms or dementia. Ann Neurol 57:82–91
Reid WGJ, Broe GA, Hely MA, Morris JGL, Williamson PM, O’Sullivan DJ, Rail D, Genge SA, Moss NG (1989) The neuropsychology of de novo patients with idiopathic Parkinson’s disease: the effects of age of onset. Int J Neurosci 48:205–217
Reid WGJ (1992) The evolution of dementia in idiopathic Parkinson’s disease: neuropsychological and clinical evidence in support of subtypes. Int Psychogeriatr 4(Suppl 2):147–160
Reid WGJ, Hely MA, Morris JGL, Broe GA, Adena M, O’Sullivan DJ, Williamson PM (1996) A longitudinal study of Parkinson’s disease: clinical and neuropsychological correlates of dementia. J Clin Neurosci 3:327–333
The National Institute on Aging, Reagan Institute Working Group on Diagnostic Criteria for the Neuropathological Assessment of Alzheimer’s Disease (1997) Consensus recommendations for the postmortem diagnosis of Alzheimer’s disease. Neurobiol Aging 18: S1–S2
Williams DR, Lees AJ (2005) Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: a retrospective autopsy study. Lancet Neurol 4:605–610
Acknowledgments
Brain donations were made to the Prince of Wales Medical Research Institute Tissue Resource Centre, which is supported by the National Health and Medical Research Council of Australia (Enabling Grant #282933) and the Prince of Wales Medical Research Institute. The work was supported through research grants from the National Health and Medical Research Council of Australia (project #222727; fellowship #157212). We wish to thank Heather McCann and Karen Murphy for research assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Halliday, G., Hely, M., Reid, W. et al. The progression of pathology in longitudinally followed patients with Parkinson’s disease. Acta Neuropathol 115, 409–415 (2008). https://doi.org/10.1007/s00401-008-0344-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-008-0344-8