Abstract
Purpose
To determine whether there was an association between adjunctive therapy with IgM-enriched immunoglobulin (IgM) and the 30-day mortality rate in patients with septic shock.
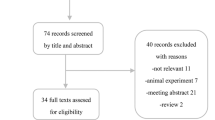
Methods
In 2008 we introduced IgM as a possible adjunctive therapy to be provided within 24 h after shock onset in the management protocol for patients with septic shock. In this retrospective study we included the adult patients suitable for IgM therapy admitted to our ICU from January 2008 to December 2011. An unadjusted comparison between patients who did or did not receive IgM therapy, a multivariate logistic model adjusted for confounders and propensity score-based matching were used to evaluate the association between early IgM treatment and mortality.
Results
One hundred and sixty-eight patients were included in the study. Of these, 92 (54.8 %) received IgM therapy. Patients who did or did not receive IgM were similar with regards to infection characteristics, severity scores and sepsis treatment bundle compliance. Patients who received IgM were more likely to have blood cultures before antibiotics and to attain a plateau inspiratory pressure less than 30 cmH2O (p < 0.05). The 30-day mortality rate was reduced by 21.1 % (p < 0.05) in the group that received IgM compared to the group that did not. The multivariate adjusted regression model (OR 0.17; CI 95 % 0.06–0.49; p = 0.001) and the propensity score-based analysis (OR 0.35; CI 95 % 0.14–0.85; p = 0.021) confirmed that IgM therapy was associated with reduced mortality at 30 days after the onset of septic shock.
Conclusions
Our experience indicates that early adjunctive treatment with IgM may be associated with a survival benefit in patients with septic shock. However, additional studies are needed to better evaluate the role of IgM therapy in the early phases of septic shock.

Similar content being viewed by others
References
Sakr Y, Elia C, Mascia L, Barberis B, Cardellino S, Livigni S et al (2013) The influence of gender on the epidemiology of and outcome from severe sepsis. Crit Care 17:R502
Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R et al (2008) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med 34:17–60
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM et al (2013) Surviving sepsis campaign guidelines committee including the pediatric subgroup: surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Intensive Care Med 39:165–228
Barochia AV, Cui X, Vitberg D, Suffredini AF, O’Grady NP, Banks SM et al (2010) Bundled care for septic shock: an analysis of clinical trials. Crit Care Med 38:668–678
Reinhart K, Brunkhorst FM, Bone H-G, Bardutzky J, Dempfle C-E, Forst H et al (2010) Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2 k guidelines of the German Sepsis Society [Deutsche Sepsis-Gesellschaft e.V. (DSG)] and the German Interdisciplinary Association of Intensive Care and Emergency Medicine [Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI)]. Ger Med Sci 8
Shankar-Hari M, Spencer J, Sewell WA, Rowan KM, Singer M (2012) Bench-to-bedside review: immunoglobulin therapy for sepsis-biological plausibility from a critical care perspective. Crit Care 16:206
Taccone FS, Stordeur P, De Backer D, Creteur J, Vincent J-L (2009) Gamma-globulin levels in patients with community-acquired septic shock. Shock 32:379–385
Giamarellos-Bourboulis EJ, Apostolidou E, Lada M, Perdios I, Gatselis NK, Tsangaris I et al (2013) Kinetics of circulating immunoglobulin M in sepsis: relationship with final outcome. Crit Care 17:R247
Werdan K, Pilz G, Bujdoso O, Fraunberger P, Neeser G, Schmieder RE et al (2007) Score-based immunoglobulin therapy of sepsis (SBITS) study group. Score-based immunoglobulin G therapy of patients with sepsis: the SBITS study. Crit Care Med 35:2693–2701
Alejandria MM, Lansang MA, Dans LF, Mantaring JB 3rd (2013) Intravenous immunoglobulin for treating sepsis and septic shock. Cochrane Database Syst 9:CD001090
Turgeon AF, Hutton B, Fergusson DA, McIntyre L, Tinmouth AA, Cameron DW et al (2007) Meta-analysis: intravenous immunoglobulin in critically ill adult patients with sepsis. Ann Intern Med 146:193–203
Kreymann KG, de Heer G, Nierhaus A, Kluge S (2007) Use of polyclonal immunoglobulins as adjunctive therapy for sepsis or septic shock. Crit Care Med 35:2677–2685
Laupland KB, Kirkpatrick AW, Delaney A (2007) Polyclonal intravenous immunoglobulin for the treatment of severe sepsis and septic shock in critically ill adults: a systematic review and meta-analysis. Crit Care Med 35:2686–2692
Girardis M, Rinaldi L, Donno L, Marietta M, Codeluppi M, Marchegiano P et al (2009) Effects on management and outcome of severe sepsis and septic shock patients admitted to the intensive care unit after implementation of a sepsis program: a pilot study. Crit Care 13:R143
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D et al (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 29:530–538
Karatzas S, Boutzouka E, Venetsanou K, Myrianthefs P, Fildisis G, Baltopoulos G (2002) The effects of IgM-enriched immunoglobulin preparations in patients with severe sepsis: another point of view. Crit Care 6:543–544
Tugrul S, Ozcan PE, Akinci O, Seyhun Y, Cagatay A, Cakar N et al (2002) The effects of IgM-enriched immunoglobulin preparations in patients with severe sepsis. Crit Care 6:357–362
Le Gall JR, Lemeshow S, Saulnier F (1993) A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H et al (1996) The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. Intensive Care Med 22:707–710. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine
Magiorakos A-P, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281
Rosenbaum PR, Rubin DB (1985) Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am Stat 39:33–38
Soares MO, Welton NJ, Harrison DA, Peura P, Shankar-Hari M, Harvey SE et al (2012) An evaluation of the feasibility, cost and value of information of a multicentre randomised controlled trial of intravenous immunoglobulin for sepsis (severe sepsis and septic shock): incorporating a systematic review, meta-analysis and value of information analysis. Health Technol Assess 16:1–186
Tamayo E, Fernández A, Almansa R, Carrasco E, Goncalves L, Heredia M et al (2012) Beneficial role of endogenous immunoglobulin subclasses and isotypes in septic shock. J Crit Care 27:616–622
Norrby-Teglund A, Haque KN, Hammarström L (2006) Intravenous polyclonal IgM-enriched immunoglobulin therapy in sepsis: a review of clinical efficacy in relation to microbiological aetiology and severity of sepsis. J Intern Med 260:509–516
Trautmann M, Held TK, Susa M, Karajan MA, Wulf A, Cross AS et al (1998) Bacterial lipopolysaccharide (LPS)-specific antibodies in commercial human immunoglobulin preparations: superior antibody content of an IgM-enriched product. Clin Exp Immunol 111:81–90
Ehrenstein MR, Notley CA (2010) The importance of natural IgM: scavenger, protector and regulator. Nat Rev Immunol 10:778–786
Rieben R, Roos A, Muizert Y, Tinguely C, Gerritsen AF, Daha MR (1999) Immunoglobulin M-enriched human intravenous immunoglobulin prevents complement activation in vitro and in vivo in a rat model of acute inflammation. Blood 93:942–951
Hoffman JN, Fertmann JM, Vollmar B, Laschke MW, Jauch KW, Menger MD (2008) Immunoglobulin M-enriched human intravenous immunoglobulins reduce leukocyte-endothelial cell interactions and attenuate microvascular perfusion failure in normotensive endotoxemia. Shock 29:133–139
Stehr SN, Knels L, Weissflog C, Schober J, Haufe D, Lupp A et al (2008) Effects of IGM-enriched solution on polymorphonuclear neutrophil function, bacterial clearance, and lung histology in endotoxemia. Shock 29:167–172
Cavazzutti I, Rinaldi L, Braccini S, Bertolotti V, Andreotti A, Busani S et al (2009) Effects of intravenous IgM-enriched immunoglobulins on muscle tissue microcirculation in septic shock: a preliminary report. Intensive Care Med 35:s239
Yavuz L, Aynali G, Aynali A, Alaca A, Kutuk S, Ceylan BG (2012) The effects of adjuvant immunoglobulin M-enriched immunoglobulin therapy on mortality rate and renal function in sepsis-induced multiple organ dysfunction syndrome: retrospective analysis of intensive care unit patients. J Int Med Res 40:1166–1174
Schedel I, Dreikhausen U, Nentwig B, Höckenschnieder M, Rauthmann D, Balikcioglu S et al (1991) Treatment of gram-negative septic shock with an immunoglobulin preparation: a prospective, randomized clinical trial. Crit Care Med 19:1104–1113
Rodríguez A, Rello J, Neira J, Maskin B, Ceraso D, Vasta L et al (2005) Effects of high-dose of intravenous immunoglobulin and antibiotics on survival for severe sepsis undergoing surgery. Shock 23:298–304
Berlot G, Vassallo MC, Busetto N, Bianchi M, Zornada F, Rosato I et al (2012) Relationship between the timing of administration of IgM and IgA enriched immunoglobulins in patients with severe sepsis and septic shock and the outcome: a retrospective analysis. J Crit Care 27:167–171
Jacobs S, Sobki S, Morais C, Tariq M (2002) Effect of pentaglobin and piperacillin on survival in a rat model of faecal peritonitis: importance of intervention timings. Acta Anaesthesiol Scand 44:88–95
Acknowledgments
We wish to thank Mervyn Singer and Matteo Bassetti for critical revisions of the manuscript and their clever suggestions.
Conflicts of interest
Cavazzuti Ilaria and Massimo Girardis have consulted for Biotest-Germany, the remaining authors have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Take-home message: Adjunctive treatment with IgM early on resulted in a 20 % reduction of the absolute 30-day risk of mortality in patients with septic shock treated using evidence-based guidelines.
Rights and permissions
About this article
Cite this article
Cavazzuti, I., Serafini, G., Busani, S. et al. Early therapy with IgM-enriched polyclonal immunoglobulin in patients with septic shock. Intensive Care Med 40, 1888–1896 (2014). https://doi.org/10.1007/s00134-014-3474-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-014-3474-6