Abstract
Objective
In a cohort of mechanically ventilated patients to compare the automatic tidal volume (V T)–respiratory rate (RR) combination generated by adaptive support ventilation (ASV) for various lung conditions.
Design and setting
Prospective observational cohort study in the 11-bed medicosurgical ICU of a general hospital.
Patients
243 patients receiving 1327 days of invasive ventilation on ASV.
Measurements
Daily collection of ventilator settings, breathing pattern, arterial blood gases, and underlying clinical respiratory conditions categorized as: normal lungs, ALI/ARDS, COPD, chest wall stiffness, or acute respiratory failure.
Results
Overall the respiratory mechanics differed significantly with the underlying conditions. In passive patients ASV delivered different V T–RR combinations based on the underlying condition, providing higher V T and lower RR in COPD than in ALI/ARDS: 9.3 ml/kg (8.2–10.8) predicted body weight (PBW) and 13 breaths/min (11–16) vs. 7.6 ml/kg (6.7–8.8) PBW and 18 breaths/min (16–22). In patients actively triggering the ventilator the V T–RR combinations did not differ between COPD, ALI/ARDS, and normal lungs.
Conclusions
ASV selects different V T–RR combinations based on respiratory mechanics in passive, mechanically ventilated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adaptive support ventilation (ASV) is an automatic ventilation mode in which minute volume (MV) is controlled by a combination of tidal volume (V T) and respiratory rate (RR) based on respiratory mechanics [1, 2]. In passive patients unable to trigger a breath the ventilator generates pressure-controlled breaths and automatically adjusts the inspiratory pressure (Pinsp) and the timing to achieve the target V T and RR. In active patients able to trigger a breath the ventilator generates pressure support breaths, automatically adjusting Pinsp to achieve the target V T, and it delivers additional pressure-controlled breaths if the patient's RR is below the target RR [1, 2]. The target V T–RR combination is based on the Otis et al. [3] equation, which determines an RR that minimizes work of inspiration for a clinician-set MV based on the time constant of the respiratory system. The time constant can be estimated on a breath-by-breath basis by the expiratory time constant (RCexp) obtained from the expiratory flow-volume curve [3–5].
In keeping with the above working principles ASV attempts to generate desirable V T–RR combinations according to underlying respiratory mechanics and, more specifically, according to RCexp. This result was preliminarily suggested by a study in which eight patients with chronic obstructive pulmonary disease (COPD; i. e., with long RCexp) ventilated with ASV had higher V T and lower RR than five patients with acute lung injury (ALI)/acute respiratory distress syndrome (ARDS; i. e., with short RCexp) [6]. However, the statistical analysis was not reported, and the study was conducted only in passive patients. Therefore the actual ability of ASV to vary its ventilatory pattern based on respiratory mechanics is still an open issue, especially in actively breathing patients. Indeed, by necessity in active patients ASV controls the ventilatory pattern less tightly as the patient regains control over RR. Moreover, the assessment of RCexp has been described only for controlled ventilation settings, and RCexp may be less accurate in actively breathing patients [4, 5].
The present prospective observational study was designed to examine in a large group of passive and active patients whether ASV varies the V T–RR combination based on respiratory mechanics in passive patients and, to a certain extent, also in actively breathing patients. To do so patients with various categories of lung diseases and respiratory mechanics were compared with patients with no lung disease and normal respiratory mechanics. This work has been already presented in abstract form [7].
Methods and materials
Patients
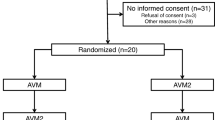
Patients admitted between January and August 2004 to the 11-bed adult general intensive care unit of Font Pré Hospital (Toulon, France) were included if they were invasively ventilated. Patients for whom leaks were an issue (noninvasive ventilation and bronchopleural fistula) were not included. All patients were ventilated with a Galileo Gold ventilator (Hamilton Medical, Bonaduz, Switzerland) using ASV as the primary mode. A detailed method section is available on the electronic supplementary material. During the 210 days of the study 322 patients were admitted to the ICU, 262 of whom received mechanical ventilation (243 invasive, 19 noninvasive) for a total of 1,357 days [97 women; median age 65 years, interquartile range (IQR) 49–76; median Simplified Acute Physiology Score II score 50, interquartile range 39–59]. ASV was used on 1,327 of these 1,357 days (98%). The patients were passive for 717 days and active for 610 days (46%). ASV was not used in two patients; one had a bronchopleural fistula, and another was a pediatric patient (with the physician lacking ASV experience in this situation).
Ethical considerations
This observational and descriptive study was approved by the ethics committee of the French Society of Critical Care (SRLF). Before starting the study ASV was used in the unit as a routine clinical care for more than 2 years, and 90% of the patients received ASV as a default mode. Because the study was purely observational and descriptive and involved no intervention, the investigators believed it possible to waive the informed consent. Information to the patients and the families regarding the ventilatory treatment was given according to the general practice in the unit.
Definitions
For any given patient each ventilation-day was categorized using one of the five following clinical conditions:
-
Normal lungs: no underlying respiratory disease, normal chest radiography, and PaO2/FIO2 ratio of 300 mmHg or higher;
-
ALI/ARDS: as defined by the American–European Consensus Conference [8];
-
COPD: as defined by the “gold” criteria [9];
-
Chest wall stiffness: presence of cyphoscoliosis, morbid obesity, or a neuromuscular disorder [10];
-
Acute respiratory failure (ARF): PaO2/FIO2 ratio of 300 mmHg or less without the ARDS/ALI criteria from the American–European Consensus Conference [8].
For any given patient each ventilation day was categorized as passive or active, the latter being defined by a patient's spontaneous RR being more than 75% of the total RR. Daily categorization makes it possible for a given patient to be categorized differently based on his changing condition. The categorization was performed daily between 8 and 9 a. m. based on the medical team's consensual decision taking into account the medical history, chest examination, daily chest radiography, daily arterial blood gases, and any other examination results that may have been performed.
ASV description and settings
ASV has been fully described in previous papers [1, 2, 11]. In short, MV is set by the clinician and controlled by a combination of V T and RR based on breath-by-breath estimation of RCexp [4, 5] according to the minimal work of breathing concept developed by Otis et al. [3]. MV is expressed as a percentage (% MV) of physiological MV: 100% MV being equal to 0.1 l/kg predicted body weight (PBW) per minute, i. e., 7 l/min for 70 kg PBW. The patient's PBW is calculated according to height and gender [12] and entered through a specific control in the ASV control panel. In active and passive patients, the starting % MV was initially set at 110%. The % MV was later adjusted according to the desired PaCO2 in passive patients and according to the clinical condition in active patients.
Failure of ASV
ASV failure was defined by one of the following conditions: (a) total inspiratory pressure (Pinsp + PEEP) of 35 cmH2O or higher, to allow the user to take over and manually adjust V T or inspiratory pressure; (b) bronchopleural fistula onset during ventilation, because of lack of information about the accuracy of RCexp measurement in cases of leak; (c) abnormal respiratory rhythms, because of the ASV response-time which can be much slower than the patient's rhythm; (d) patient-ventilator asynchrony defined clinically and on the pressure-flow traces [13], to allow the user to manually adjust inspiratory pressure. Patients who failed ASV were switched to a volume-controlled or pressure support mode.
Data collection
Recording was performed at 6 a. m., with arterial blood gas analysis by an independent investigator. Ventilator settings (PBW, % MV, PEEP, and FIO2), breathing pattern (V T, total and spontaneous RR, T I, T E), and respiratory mechanics parameters were read from the ventilator display along with arterial blood gas results. Airway pressure and flow were measured using the proximal pneumotachograph (single-use flow sensor, PN 279331, Hamilton Medical, Bonaduz, Switzerland, linear between –120 and 120 l/min with a ± 5% error of measure). In passive patients static compliance (Cstat) and inspiratory resistance (Rins) were measured using the least squares fit method [14]. RCexp was automatically calculated on a breath-to-breath basis as the ratio between the volume and the simultaneous expiratory flow measured at the point corresponding to 75% of the expiratory tidal volume [4, 5].
Statistical analysis
Values are given as medians with their 25th and 75th quartiles (IQR). Comparisons were carried out using a nonparametric analysis of variance. Differences were considered significant at p < 0.05. When significant differences were observed, two-by-two multiple comparisons were performed using Dunn's method (SigmaStat, version 3.0, SPSS, Chicago, Ill., USA).
Results
In both passive ventilation days (Table 1) and active ventilation days (Table 2) RCexp differed significantly according to the clinical respiratory conditions: short (0.51 s, IQR 0.42–0.64) in passive ALI/ARDS as compared to passive COPD (1.00 s, 0.77–1.31, p < 0.05). This was also true for active ALI/ARDS (0.57 s, 0.40–0.71) as compared to active COPD (0.89 s, 0.64–1.15, p < 0.005). The shortest RCexp values were observed in chest wall stiffness and the longest in COPD (Tables 1, 2).
On passive normal ventilation days V T was significantly lower (8.3 ml/kg, IQR 7.7–9.1) than in passive COPD (9.3 ml/kg, 8.2–10.8, p < 0.05) and higher than in passive ALI/ARDS (7.6 ml/kg, 6.7–8.8, p < 0.05; Table 1, Fig. 1). On passive normal ventilation days RR (14 breaths/min, IQR 13–16) was significantly lower than in passive ALI/ARDS (18 breaths/min, 16–22, p < 0.05) and equivalent to passive COPD (13 breaths/min, 11–16; Table 1, Fig. 1).
The spirograms of COPD, ALI/ARDS, and normal patients during all the ventilation days (left), passive ventilation days (middle), and active ventilation days (right). Each spirogram was drawn using the median values of V T per predicted body weight (summit of triangle), the median value of T I (ascending part of triangle), the median value of T E (descending part of triangle), and the base of the triangle is T I + T E = T TOT. The horizontal statistical difference lines refer to T TOT; T TOT in ALI/ARDS was significantly lower than in normal patients and COPD for all ventilation days and passive ventilation days. Vertical statistical difference line V T/PBW: V T/PBW in ALI/ARDS was significantly lower than in normal patients and COPD for all ventilation days and passive ventilation days; V T/PBW in normal patients was significantly lower than in COPD for all ventilation days and passive ventilation days. * p < 0.05 using the Dunn's method for two-by-two multiple comparisons
On active ventilation days the lowest V T was found in patients with chest wall stiffness (7.0 ml/kg, IQR 6.0–7.8), and V T was significantly lower than in active normal (7.9 ml/kg, 7.3–8.8, p < 0.05) and active COPD (8.5 ml/kg, 7.7–9.5, p < 0.05; Table 2). The lowest RR was found in active COPD (17 breaths/min, IQR 14–24), and it was significantly lower than in active chest wall stiffness (24 breaths/min, 21–28, p < 0.05) and ARF (20 breaths/min, 17–25, p < 0.05; Table 2).
According to the predefined criteria, ASV failed in one patient due to a bronchopleural fistula after a lung biopsy and in five ALI/ARDS patients due to a total inspiratory pressure greater than 35 cmH2O. One patient was switched to a home care ventilator for adaptation to long-term ventilation. A normal weaning procedure was followed in 116 patients, with a reintubation rate of 8% within the first 48 h, and 47 patients required a tracheotomy (19%).
Discussion
According to the categorization used, the present study found that ASV delivered different V T–RR combinations depending on the clinical conditions in passive patients and, to a lesser extent, in active patients. Different clinical conditions were associated with different values of RCexp, and this has not been reported previously. According to the categorization used, the RCexp was short in chest wall stiffness and in ALI/ARDS, long in COPD patients. This holds true in passive (Table 1) and active patients (Table 2). Possibly because of some overlap in clinical conditions the RCexp between active ALI/ARDS and ARF patients did not differ significantly (Table 2). In COPD patients the respiratory system does not behave as a simple monocompartmental model, and it can hardly be described by a single RCexp value. In the present study RCexp was longer in COPD than in any other groups, which may be due to the measurement at 75% of V T [5].
In keeping with the preliminary report from Belliato and coworkers [6], the present study found that ASV delivered higher V T and lower RR in clinical conditions associated with long time constants (COPD) than in conditions associated with short time constants (ALI/ARDS; Table 1, Fig. 1). It should be pointed out, however, that the RR in passive COPD was not different than in normal passive patients (Table 1). One explanation is that the % MV set in the COPD patients was higher than in the normal lungs. This can also be explained by the Otis equation, which takes the form; RR ≈ 1/RCexp; the higher the RCexp, the smaller is the relative decrease in RR [3]. In the present case despite an RCexp 28% higher in passive COPD than in passive normal patients RR was only 7% lower (Table 1). From a practical point of view this means that the Otis equation might be more “sensitive” when adapting RR where RCexp is short (ALI/ARDS and chest wall stiffness) than where RCexp is long (COPD).
In actively breathing patients V T–RR differences are evident only under the most extreme clinical conditions: chest wall stiffness vs. normal and COPD patients (Table 2). This can be explained by active breathing patients partially controlling their V T–RR combination. It has been shown that the level of assistance only marginally influences the patient's RR [15] while V T depends on the complex interaction of assistance level, work of the patient's muscles, and the patient's ventilatory requirement and drive [16]. From a methodological point of view, in active patients the categorization was possibly more difficult (due to the resolution of the pulmonary disease). A lack of statistical significance can also be argued, because the number of active ALI/ARDS ventilation days was only 25 (17 patients). Finally, more generally, and especially in active patients, the question arises about the pertinence of adjusting V T–RR on the basis of respiratory mechanics only, while from a physiological perspective, RR and V T also depend on respiratory drive, cortical inputs, and other mechanical and chemical feedback [17].
In patients with chest wall stiffness the total respiratory compliance is reduced mainly because of chest wall abnormalities. In fact ASV delivered a low V T and high RR combination because of chest wall and not lungs reduced compliance. Whether such V T–RR combination is optimal in this condition deserves further investigation.
ASV in the subgroup of ALI/ARDS patients warrants further comments. In passive ALI/ARDS patients the V T/PBW ratio was 7.6 ml/kg and the median total inspiratory pressure was 30 cmH2O (27–36). These values are slightly higher than those recommended by the ARDS Network [18], but they are similar to baseline values (7.4 ml/kg) reported in recent studies on ALI/ARDS [19, 20]. Although it was consistent with a general policy of V T reduction in ALI/ARDS, ASV resulted in higher V T values than the 6 ml/kg recommendation, which in turn is strongly challenged [21]. Several reports show that recommendations about reducing V T in ARDS are not widely applied [22, 23]. Automatic adjustment of V T can be an additional tool to help applying a V T reduction policy. In the present study 5 out of 26 ARDS patients had a total inspiratory pressure above 35 cmH2O. Three of these were head trauma patients in whom high minute volume and therefore Pinsp was required to keep normal-low values of PaCO2 (permissive respiratory acidosis contraindicated). The remaining two patients had morbid obesity, and high Pinsp was thought to be related to low chest wall compliance. In these two patients a higher Pinsp would have been acceptable in clinical practice.
Finally, two recent studies suggest that ventilation with large V T in patients without acute lung injury is an important risk factor for developing ALI/ARDS [24, 25]. On the other hand, a V T/PBW ratio below 9.0 ml/kg was associated with the least risk for developing ALI/ARDS [26]. Interestingly, with normal lung conditions the present study found a V T/PBW ratio of 8.1 ml/kg (IQR 7.5–8.9), suggesting that ASV prevents high V T-related lung injury in mechanically ventilated patients with normal lungs.
The present study reports the possibility of using ASV as a quasi exclusive mode of ventilation (98% of ventilation days) from the beginning of ventilation to the weaning phase. By design this study did not aim to compare ASV with any other ventilation strategy nor to evaluate clinical outcomes. There were very few primary contraindications to ASV utilization, and almost all patients were ventilated with ASV. Following previous preliminary study [27], this is the first report of the use of a closed-loop system over long periods of time in a large cohort of patients, both passively and actively breathing, and with various pulmonary disorders.
Automatic selection of the V T–RR combination in mechanically ventilated patients may have additional advantages. Respiratory mechanics are prone to change rapidly in mechanically ventilated ICU patients, and clinicians are unlikely to make the necessary ventilator adjustments at the right moment. Importantly, breath-by-breath evaluation of respiratory mechanics is not easily available at the bedside, and even so it may not be followed by immediate intervention. Publications showing the beneficial effects of any type of automatic ventilation are rare indeed, but the few available ones suggest the possibility of shortening the duration of ventilation, the duration of weaning, and the number of ventilator manipulations [28–30]. The number of clinician interventions to modify the settings was not collected in the present study, but previous investigation found that the use of ASV resulted in fewer manipulations in cardiac postoperative patients [28].
In conclusion, this observational study confirms ASV ability to select different V T–RR combinations based on respiratory mechanics in passive mechanically ventilated patients. In actively breathing patients the differences of V T–RR combinations associated with ASV were less clear despite different RCexp values. In the present study we report the possibility of using ASV as a quasi exclusive mode of ventilation, a strategy that needs to be further evaluated.
References
Brunner JX, Iotti GA (2002) Adaptive support ventilation (ASV). Minerva Anesthesiol 68:365–368
Campbell RS, Branson RD, Johannigman JA (2001) Adaptive support ventilation. Respir Care Clin N Am 7:425–440
Otis AB, Fenn WO, Rahn H (1950) Mechanics of breathing in man. J Appl Physiol 2:592–607
Brunner JX, Laubsher TP, Banner MJ, Iotti G, Brashi A (1995) Simple method to measure total expiratory time constant based on passive expiratory flow-volume curve. Crit Care Med 23:1117–1122
Lourens MS, Van Den Berg B, Aerts JG, Verbraak AFM, Hoogsteden HC, Bogaard JM (2000) Expiratory time constants in mechanically ventilated patients with and without COPD. Intensive Care Med 26:1612–1618
Belliato M, Palo A, Pasero D, Iotti GA, Mojoli F, Brashi A (2004) Evaluation of adaptive support ventilation in paralysed patients and in a physical lung model. Int J Artif Organs 27:709–716
Arnal JM, Nafati C, Wysocki M, Donati SY, Granier I, Durand-Gasselin J (2004) Utilization of an automatic mode of ventilation (ASV) in a mixed ICU population: prospective observational study. Intensive Care Med 30:S84
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Le Gall JR, Morris A, Spragg R (1994) Report of the American–European Consensus Conference on acute respiratory distress syndrome: definitions, mechanism, relevant outcomes, and clinical trial coordination. Consensus Committee. Am J Respir Crit Care Med 149:818–824
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, Van Weel C, Zielinski J (2007) Global strategy for the diagnosis, management, and prevention of COPD—2006 update. Am J Respir Crit Care Med (epub ahead of print: 16 May)
MacDuff A, Grant IS (2003) Critical care management of neuromuscular disease, including long term ventilation. Curr Opin Crit Care 9:106–112
Tassaux D, Dalmas E, Gratadour P, Jolliet P (2002) Patient-ventilator interactions during partial ventilatory support: a preliminary study comparing the effects of adaptive support ventilation with synchronized intermittent mandatory ventilation plus inspiratory pressure support. Crit Care Med 30:801–807
Devine BJ (1974) Gentamicin therapy. Drug Intell Clin Pharm 8:650–655
Geogopoulos D, Prinianakis D, Kondili E (2006) Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Med 32:34–47
Iotti GA, Braschi A, Brunner JX, Smits T, Olivei M, Palo A, Veronesi R (1995) Respiratory mechanics by least squares fitting in mechanically ventilated patients: applications during paralysis and during pressure support ventilation. Intensive Care Med 21:406–413
Marantz S, Patrick W, Webster K, Roberts D, Oppenheimer L, Younes M (1996) Response of ventilator dependant patient s to different levels of proportional assist. J Appl Physiol 80:397–403
Jaber S, Delay JM, Matecki S, Sebbane M, Eledjam JJ, Brochard L (2005) Volume-guaranteed pressure support facing acute change in ventilatory demand. Intensive Care Med 31:1181–1188
Kondili E, Prinianakis G, Georgopoulos D (2003) Patient-ventilator interaction. Br J Anaesth 91:106–119
Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 18:1301–1308
National Heart, Lung and Blood Institute Acute Respiratory Distress Syndrome Clinical Trials Network, Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med 354:2213–2224
National Heart, Lung and Blood Institute Acute Respiratory Distress Syndrome Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL (2006) Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 354:2564–2575
Deans K, Minneci P, Cui X, Banks S, Natanson C, Eichacker P (2005) Mechanical ventilation in ARDS: one size does not fit all. Crit Care Med 33:1141–1143
Weinert CR, Gross C, Marinelli WA (2003) Impact of randomized trial results on acute lung injury ventilator therapy in teaching hospitals. Am J Respir Crit Care Med 167:1304–1309
Young MP, Manning HL, Wilson DL, Mette SA, Riker RR, Leiter JC, Liu SK, Bates JT, Parsons PE (2004) Ventilation of patients with acute lung injury and acute respiratory distress syndrome: has new evidence changed clinical practice? Crit Care Med 32:1260–1265
Gajic O, Frutos-Vivar F, Esteban A, Hubmayr RD, Anzueto A (2005) Ventilator settings as a risk factor for acute respiratory distress syndrome in mechanically ventilated patients. Intensive Care Med 31:922–926
Bonetto C, Terragni P, Ranieri M (2005) Does high tidal volume generate ALI/ARDS in healthy lungs? Intensive Care Med 31:893–895
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R, St Sauver JL, Lymp JF, Afessa B, Hubmayr RD (2004) Ventilator-induced lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 32:1817–1824
Iotti GA, Belliato M, Polito A, Pasero D, Beduneau G, Brochard L, Mancebo J, Ranieri MV (2005) Safety and effectiveness of adaptive support ventilation (ASV) in acute respiratory failure. Intensive Care Med 31:S168
Sultzer CF, Chioléro R, Chassot PG, Mueller XM, Revelly JP (2001) Adaptive support ventilation for tracheal extubation after cardiac surgery. Anesthesiology 95:1339–1345
Petter AH, Chiolero RL, Cassina T, Chassot PG, Muller XM, Revelly JP (2003) Automatic “respirator/weaning” with adaptive support ventilation: the effect on duration of endotracheal intubation and patient management. Anesth Analg 97:1743–1750
Lellouche F, Mancebo J, Jolliet P, Roeseler J, Schortgen F, Dojat M, Cabello B, Bouadma L, Rodriguez P, Maggiore S, Reynaert M, Mersmann S, Brochard L (2006) A multicenter randomized trial of computer-driven protocolized weaning from mechanical ventilation. Am J Respir Crit Care Med 174:894–900
Acknowledgements
We are indebted to Mrs. Sandy Miller for her technical assistance in preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
J.-M.A. was supported by Hamilton Medical in presenting the results of this study at international congress. M.W. is an employee of Hamilton Medical and as the Head of Medical Research was involved in the initial discussions regarding the design of the study and in helping to write the manuscript. He was not involved in collecting and analyzing the data. This study was conducted in the Intensive Care Unit of Font Pré Hospital, Toulon, France.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Arnal, JM., Wysocki, M., Nafati, C. et al. Automatic selection of breathing pattern using adaptive support ventilation. Intensive Care Med 34, 75–81 (2008). https://doi.org/10.1007/s00134-007-0847-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-007-0847-0