Summary
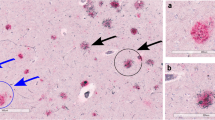
Alzheimer’s disease entails multiple neuronal systems and results from neuronal cytoskeletal degeneration of only a few types of nerve cells. Essential for neuropathological diagnosis is assessment of the presence of neurofibrillary tangles and neuropil threads. The destructive process begins in predisposed cortical induction sites, thereafter invading other portions of the cerebral cortex and specific sets of subcortical nuclei in a predictable sequence with little variation. The location of the tangle-bearing neurons and severity of the pathology allow the distinction of six stages in disease propagation (transentorhinal I–II: clinically silent cases; limbic III–IV: incipient Alzheimer’s disease; neocortical V–VI: fully-developed Alzheimer’s disease). The pattern of appearance of the neurofibrillary changes bears a striking resemblance to the inverse sequence of cortical myelination. The average myelin content is a negative image of the density of intraneuronal lipofuscin deposits. Pigment-laden neurons endowed with a long, thin, and sparsely myelinated axon are prone to develop AD-related changes. The emergence of the first neurofibrillary changes, at whatever age these occur, signals the onset of a degenerative process that persists until death. An extended period of time elapses between the beginning of histologically verifiable lesions and the appearance of initial clinical symptoms. Once initiated, however, cytoskeletal deterioration inexorably progresses, and neither remission nor recovery is observed.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Preview
Unable to display preview. Download preview PDF.
Similar content being viewed by others
References
Amaral DG, Insausti R (1990) Hippocampal formation. In: Paxinos G (ed) The human nervous system. Academic Press, San Diego, pp 711–755
Bancher C, Brunner C, Lassmann H, Budka H, Jellinger K, Wiche G, Seitelberger F, Grundke-Iqbal I, Wisniewski HM (1989) Accumulation of abnormally phosphorylated tau precedes the formation of neurofibrillary tangles in Alzheimer’s disease. Brain Res 477: 90–99
Bancher C, Braak H, Fischer P, Jellinger KA (1993) Neuropathological staging of Alzheimer lesions and intellectual status in Alzheimer’s and Parkinson’s disease. Neurosci Lett 162: 179–182
Bancher C, Jellinger K, Lassmann H, Fischer P (1996) Correlations between mental state and quantitative neuropathology in the Vienna longitudinal study on dementia. Eur Arch Psychiatr Clin Neurosci 246: 137–146
Beyreuther K, Masters CL (1991) Amyloid precursor protein (APP) and beta amyloid-4 amyloid in the etiology of Alzheimer’s disease: precursor product relationships in the derangement of neuronal function. Brain Pathol 1: 241–252
Braak H (1980) Architectonics of the human telencephalic cortex. Springer, Berlin Heidelberg New York, pp 1–147
Braak H, Braak E (1984) Architectonics as seen by lipofuscin stains. In: Peters A, Jones EG (eds) Cerebral cortex, vol 1. Cellular organization of the cerebral cortex. Plenum Press, New York, pp 59–104
Braak H, Braak E (1991) Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol 82: 239–259
Braak H, Braak E (1992) The human entorhinal cortex: normal morphology and lamina-specific pathology in various diseases. Neurosci Res 15: 6–31
Braak H, Braak E (1994) Pathology of Alzheimer’s disease. In: Calne DB (ed) Neurodegenerative diseases. Saunders, Philadelphia, pp 585–613
Braak H, Braak E (1996) Development of Alzheimer-related neurofibrillary changes in the neocortex inversely recapitulates cortical myelogenesis. Acta Neuropathol 92: 197–201
Braak H, Braak E (1997a) Aspects of cortical destruction in Alzheimer’s disease. In: Hyman BT, Duyckaerts, Christen Y (eds) Connections, cognition and Alzheimer’s disease. Springer, Berlin Heidelberg New York Tokyo, pp 1–16
Braak H, Braak E (1997b) Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging 18: 351–357
Braak H, Duyckaerts C, Braak E, Piette F (1993) Neuropathological staging of Alzheimer-related changes correlates with psychometrically assessed intellectual status. In: Corian B, Iqbal K, Nicolini M, Winblad B, Wisniewski H, Zatta PF (eds) Alzheimer’s disease: advances in clinical and basic research. Wiley, Chichester, pp 131–137
Braak E, Braak H, Mandelkow EM (1994) A sequence of cytoskeleton changes related to the formation of neurofibrillary tangles and neuropil threads. Acta Neuropathol 87: 554–567
Braak H, Braak E, Yilmazer D, Schultz C, Bohl J (1995) Age-related changes of the human cerebral cortex. In: Cruz-Sanchez FF, Ravid R, Cuzner ML (eds) Neuropathological diagnostic criteria for brain banking (Biomedical Health Research, vol 10). IOS Press, Amsterdam, pp 14–19
Braak H, Griffing K, Braak E (1997) Neuroanatomy of Alzheimer’s disease. Alzheimer’s Res 3: 235–247
Braak H, Braak E, deVos RAI, Jansen ENH, Bratzke H (1998) Neuropathological hallmarks of Alzheimer’s and Parkinson’s diseases. Progr Brain Res (in press)
Cras P, Smith MA, Richey PL, Siedlak SL, Mulvihill P, Perry G (1995) Extracellular neurofibrillary tangles reflect neuronal loss and provide further evidence of extensive protein cross-linking in Alzheimer’s disease. Acta Neuropathol 89: 291–295
Dickson DW, Crystal HA, Mattiace LA, Masur DM, Blau AD, Davies P, Yen SH, Aronson MK (1991) Identification of normal and pathological aging in prospectively studied nondemented elderly humans. Neurobiol Aging 13: 179–189
Duyckaerts C, He Y, Seilhean D, Delaère P, Piette F, Braak H, Hauw JJ (1994) Diagnosis and staging of Alzheimer’s disease in a prospective study involving aged individuals. Neurobiol Aging [Suppl 1] 15: 140–141
Duyckaerts C, Delaère P, He Y, Camilleri S, Braak H, Piette F, Hauw JJ (1995) The relative merits of tau-and amyloid markers in the neuropathology of Alzheimer’s disease. In: Bergener M, Finkel SI (eds) Treating Alzheimer’s and other dementias. Springer, New York, pp 81–89
Esiri MM, Hyman BT, Beyreuther K, Masters C (1997) Aging and dementia. In: Graham DL, Lantos PI (eds) Greenfield’s neuropathology. Arnold, London, pp 153–234
Flechsig P (1920) Anatomie des menschlichen Gehirns und Rückenmarks auf myelogenetischer Grundlage. Thieme, Leipzig
German DC, White CL, Sparkman DR (1987) Alzheimer’s disease: neurofibrillary tangles in nuclei that project to the cerebral cortex. Neuroscience 21: 305–312
Goedert M (1993) Tau protein and the neurofibrillary pathology of Alzheimer’s disease. Trends Neurosci 16: 460–465
Goedert M, Trojanowski JQ, Lee VMY (1997) The neurofibrillary pathology of Alzheimer’s disease. In: Rosenberg RN (ed) The molecular and genetic basis of neurological disease, 2nd edn. Butterworth-Heinemann, Boston, pp 613–627
Hansen LA, Samuel W (1997) Criteria for Alzheimer’s disease and the nosology of dementia with Lewy bodies. Neurology 48: 126–132
Hof PR, Cox K, Young WG, Celio MR, Rogers J, Morrison JH (1991) Parvalbumin-immunoreactive neurons in the neocortex are resistant to degeneration in Alzheimer’s disease. J Neuropathol Exp Neurol 50: 451–462
Hof PR, Nimchinsky EA, Celio MR, Bouras C, Morrison JH (1993) Calretinin-immunoreactive neocortical interneurons are unaffected in Alzheimer’s disease. Neurosci Lett 152: 145–149
Hyman BT, Gomez-Isla T (1994) Alzheimer’s disease is a laminar, regional, and neural system specific disease, not a global brain disease. Neurobiol Aging 15: 353–354
Hyman BT, van Hoesen GW, Damasio AR, Barnes CL (1984) Alzheimer’s disease: cell-specific pathology isolates the hippocampal formation. Science 225: 1168–1170
Hyman BT, van Hoesen GW, Kromer LJ, Damasio AR (1986) Perforant pathway changes and the memory impairment of Alzheimer’s disease. Ann Neurol 20: 472–481
Hyman BT, van Hoesen GW, Damasio AR (1990) Memory-related neural systems in Alzheimer’s disease: an anatomic study. Neurology 40: 1721–1730
Iqbal K, Alonso AC, Gong CX, Khatoon S, Singh TJ, Grundke-Iqbal I (1994) Mechanism of neurofibrillary degeneration in Alzheimer’s disease. Mol Neurobiol 9: 119–123
Jellinger K, Braak H, Braak E, Fischer P (1991) Alzheimer lesions in the entorhinal region and isocortex in Parkinson’s and Alzheimer’s diseases. Ann NY Acad Sci 640: 203–209
Kemper TL (1978) Senile dementia: a focal disease in the temporal lobe. In: Nandy E (ed) Senile dementia: a biomedical approach. Elsevier, Amsterdam, pp 105–113
Kemper TL (1984) Neuroanatomical and neuropathological changes in normal aging and in dementia. In: Albert ML (ed) Clinical neurology of aging. Oxford University Press, Oxford, pp 9–52
Lewis DA, Campbell MJ, Terry RD, Morrison JH (1987) Laminar and regional distributions of neurofibrillary tangles and neuritic plaques in Alzheimer’s disease: a quantitative study of visual and auditory cortices. J Neurosci 7: 1799–1808
Mirra SS, Heyman A, McKeel D, Sumi SM, Crain BJ, Brownlee LM, Vogel FS, Hughes JP, van Belle G, Berg L (1991) The consortium to establish a registry for Alzheimer’s disease (CERAD). II. Standardization of the neuropathologic assessment of Alzheimer’s disease. Neurology 41: 479–486
Nagy Z, Vatter-Bittner B, Braak H, Braak E, Yilmazer DM, Schultz C, Hanke J (1997) Staging of Alzheimer-type pathology: an interrater-intrarater study. Dementia 8: 248–251
Nieuwenhuys R (1994) The neocortex: an overview of its evolutionary development, structural organization and synaptology. Anat Embryol 190: 307–337
Nieuwenhuys R (1996) The greater limbic system, the emotional motor system and the brain. Prog Brain Res 107: 551–580
Ohm TG, Müller H, Braak H, Bohl J (1995) Close-meshed prevalence rates of different stages as a tool to uncover the rate of Alzheimer’s disease-related neurofibrillary changes. Neuroscience 64: 209–217
Ohm TG (1997) Does Alzheimer’s disease start early in life? Mol Psychiat 2: 21–25
Rapoport SI (1988) Brain evolution and Alzheimer’s disease. Rev Neurol (Paris) 144: 79–90
Regeur L, Jensen GB, Pakkenberg H, Evans SM, Pakkenberg B (1994) No global neocortical nerve cell loss in brains from patients with senile dementia of Alzheimer’s type. Neurobiol Aging 15: 347–352
Samuel W, Galasko D, Masliah E, Hansen LA (1996) Neocortical Lewy body counts correlate with dementia in the Lewy body variant of Alzheimer’s disease. J Neuropathol Exp Neurol 55: 44–52
Selkoe DJ (1994) Alzheimer’s disease: a central role for amyloid. J Neuropathol Exp Neurol 53: 438–447
Trojanowski JQ, Shin RW, Schmidt ML, Lee VMY (1995) Relationship between plaques, tangles, and dystrophic processes in Alzheimer’s disease. Neurobiol Aging 16: 335–340
van Hoesen GW, Hyman BT (1990) Hippocampal formation: anatomy and the patterns of pathology in Alzheimer’s disease. Progr Brain Res 83: 445–457
Van Hoesen GW, Hyman BT, Damasio AR (1991) Entorhinal cortex pathology in Alzheimer’s disease. Hippocampus 1: 1–8
Vogt C, Vogt O (1919) Allgemeine Ergebnisse unserer Hirnforschung. J Psychol Neurol 25: 279–262
Yakovlev PI, Lecours AR (1967) The myelogenetic cycles of regional maturation of the brain. In: Minkowksi A (ed) Regional development of the brain in early life. Blackwell, Oxford, pp 3–70
Zilles K (1990) Cortex. In: Paxinos G (ed) The human nervous system. Academic Press, New York, pp 757–802
Zola-Morgan S, Squire LR (1993) Neuroanatomy of memory. Ann Rev Neurosci 16: 547–563
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 1998 Springer-Verlag Wien
About this paper
Cite this paper
Braak, H., Braak, E. (1998). Evolution of neuronal changes in the course of Alzheimer’s disease. In: Jellinger, K., Fazekas, F., Windisch, M. (eds) Ageing and Dementia. Journal of Neural Transmission. Supplementa, vol 53. Springer, Vienna. https://doi.org/10.1007/978-3-7091-6467-9_11
Download citation
DOI: https://doi.org/10.1007/978-3-7091-6467-9_11
Publisher Name: Springer, Vienna
Print ISBN: 978-3-211-83114-4
Online ISBN: 978-3-7091-6467-9
eBook Packages: Springer Book Archive