Abstract
Background
Diabetes is a known risk factor for early postoperative complications. Even so, the incidence of acute postoperative complications following routine hernia surgery is seldom described, and the risk for reoperation for recurrence has hardly been studied. Our aim was to explore if diabetes is a significant risk factor for complications after inguinal hernia surgery.
Methods
All inguinal hernia repairs registered in the Swedish Hernia Register between 2002 and 2011 were identified. Information on comorbidity and postoperative complications was obtained through cross-referencing with the National Patient Register at the National Board of Health and Welfare. Complicated diabetes was defined as diabetes with secondary manifestations (corresponding to aDCSI >0). The hazards for postoperative complications and reoperation for recurrence after the index hernia operation were calculated.
Results
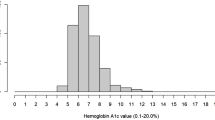
Altogether 162,713 inguinal hernia repairs on 143,041 patients were registered. Of these, the number of patients with diabetes was 4816 (3.4 %), including 1123 (0.8 %) patients with complicated diabetes (aDCSI > 0). A significantly increased risk for postoperative complications was observed up to 30 days after hernia surgery when adjusted for gender, age, BMI, history of liver disease, kidney disease or HIV/AIDS, type of hernia and surgical method (odds ratio 1.35, 95 % confidence interval 1.14–1.60). No significantly increased risk for reoperation up until December 31, 2011, was observed in either patient group.
Conclusion
Diabetes seems to increase the risk for postoperative complications within 30 days of inguinal hernia surgery, especially for complicated diabetes. Diabetes does not seem to increase the long-term risk for reoperation for recurrence.

Similar content being viewed by others
References
Jackson RS et al (2012) Hyperglycemia is associated with increased risk of morbidity and mortality after colectomy for cancer. J Am Coll Surg 214(1):68–80
Vilar-Compte D et al (2008) Hyperglycemia as a risk factor for surgical site infections in patients undergoing mastectomy. Am J Infect Control 36(3):192–198
Ramos M et al (2008) Relationship of perioperative hyperglycemia and postoperative infections in patients who undergo general and vascular surgery. Ann Surg 248(4):585–591
Malmstedt J et al (2006) Influence of perioperative blood glucose levels on outcome after infrainguinal bypass surgery in patients with diabetes. Br J Surg 93(11):1360–1367
Golden SH et al (1999) Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care 22(9):1408–1414
Brem H, Tomic-Canic M (2007) Cellular and molecular basis of wound healing in diabetes. J Clin Invest 117(5):1219–1222
The Swedish Hernia Register. Data on coverage. www.svensktbrackregister.se. Accessed July 8, 2016.
Nilsson H et al (2007) Mortality after groin hernia surgery. Ann Surg 245(4):656–660
Ludvigsson JF et al (2009) The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol 24(11):659–667
Ludvigsson JF et al (2011) External review and validation of the Swedish national inpatient register. BMC Public Health 11:450
Chang HY et al (2012) Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care 18(11):721–726
The National Swedish Diabetes Register Annual Report (2012)
Kolluru GK, Bir SC, Kevil CG (2012) Endothelial dysfunction and diabetes: effects on angiogenesis, vascular remodeling, and wound healing. Int J Vasc Med 2012:918267
Lerman OZ et al (2003) Cellular dysfunction in the diabetic fibroblast: impairment in migration, vascular endothelial growth factor production, and response to hypoxia. Am J Pathol 162(1):303–312
McMurry JF Jr (1984) Wound healing with diabetes mellitus. Better glucose control for better wound healing in diabetes. Surg Clin North Am 64(4):769–778
van Ramshorst GH et al (2010) Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg 34(1):20–27
De Berardis G et al (2012) Association of aspirin use with major bleeding in patients with and without diabetes. JAMA 307(21):2286–2294
Hujoel PP, Stott-Miller M (2011) Retinal and gingival hemorrhaging and chronic hyperglycemia. Diabetes Care 34(1):181–183
Ochoa-Gonzalez F et al (2016) Metformin induces cell cycle arrest, reduced proliferation, wound healing impairment in vivo and is associated to clinical outcomes in diabetic foot ulcer patients. PLoS One 11(3):e0150900
Ilhan YS et al (2005) The effect of an angiotensin converting enzyme inhibitor on intestinal wound healing. J Surg Res 128(1):61–65
Zandifar E et al (2012) The effect of captopril on impaired wound healing in experimental diabetes. Int J Endocrinol 2012:785247
Ljungqvist O (2010) Insulin resistance and outcomes in surgery. J Clin Endocrinol Metab 95(9):4217–4219
Ljungqvist O, Nygren J, Thorell A (2000) Insulin resistance and elective surgery. Surgery 128(5):757–760
Thorell A, Nygren J, Ljungqvist O (1999) Insulin resistance: a marker of surgical stress. Curr Opin Clin Nutr Metab Care 2(1):69–78
Black E et al (2003) Decrease of collagen deposition in wound repair in type 1 diabetes independent of glycemic control. Arch Surg 138(1):34–40
Mullen JT, Moorman DW, Davenport DL (2009) The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 250(1):166–172
Rosemar A et al (2010) Effect of body mass index on groin hernia surgery. Ann Surg 252(2):397–401
Choban PS et al (1995) Increased incidence of nosocomial infections in obese surgical patients. Am Surg 61(11):1001–1005
Winfield RD et al (2016) Obesity and the risk for surgical site infection in abdominal surgery. Am Surg 82(4):331–336
Donohoe CL et al (2011) Perioperative evaluation of the obese patient. J Clin Anesth 23(7):575–586
Stenberg E et al (2014) Is glycosylated hemoglobin A1 c associated with increased risk for severe early postoperative complications in nondiabetics after laparoscopic gastric bypass? Surg Obes Relat Dis 10(5):801–805
Kwon S et al (2013) Importance of perioperative glycemic control in general surgery: a report from the Surgical Care and Outcomes Assessment Program. Ann Surg 257(1):8–14
Kiran RP et al (2013) The clinical significance of an elevated postoperative glucose value in nondiabetic patients after colorectal surgery: evidence for the need for tight glucose control? Ann Surg 258(4):599–604 discussion 604-5
Acknowledgments
The study was funded by a grant from Olle Engqvist research foundation.
Author’s contributions
Study conception and design—Gabriel Sandblom.
Acquisition of data—Gabriel Sandblom.
Analysis and interpretation of data—Ursula Dahlstrand, Ulf Gunnarsson, Gustaf Hellspong, Gabriel Sandblom.
Drafting of manuscript—Gustaf Hellspong, Gabriel Sandblom.
Critical revision of manuscript—Ursula Dahlstrand, Ulf Gunnarsson, Gustaf Hellspong, Gabriel Sandblom.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent
All patients registered in the Swedish Hernia Register have given oral consent to the registration.
Funding
The study was funded by a grant from Olle Engqvist research foundation.
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hellspong, G., Gunnarsson, U., Dahlstrand, U. et al. Diabetes as a risk factor in patients undergoing groin hernia surgery. Langenbecks Arch Surg 402, 219–225 (2017). https://doi.org/10.1007/s00423-016-1519-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-016-1519-8