Abstract
Zika virus (ZIKV) is an arbovirus transmitted mainly by mosquitos of Aedes species. The virus has emerged in recent years and spread throughout North and South Americas. The recent outbreak of ZIKV started in Brazil (2015) has resulted in infections surpassing a million mark. Contrary to the previous beliefs that Zika causes mildly symptomatic infections fever, headache, rash, arthralgia, and conjunctivitis, the recent outbreak associated ZIKV to serious neurological complications such as microcephaly, Guillain-Barré syndrome, and eye infections. The recent outbreak has resulted in an astonishing number of microcephaly cases in fetus and infants. Consequently, numerous studies were conducted using in vitro cell and in vivo animal models. These studies showed clear links between ZIKV infections and neurological abnormalities. Diagnosis methods based on nucleic acid and serological detection facilitated rapid and accurate identification of ZIKV infections. New transmission modalities such as sexual and transplacental transmission were uncovered. Given the seriousness of ZIKV infections, WHO declared the development of safe and effective vaccines and new antiviral drugs as an urgent global health priority. Rapid work in this direction has led to the identification of several vaccine and antiviral drug candidates. Here, we review the remarkable progress made in understanding the molecular links between ZIKV infections and neurological irregularities, new diagnosis methods, potential targets for antiviral drugs, and the current state of vaccine development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
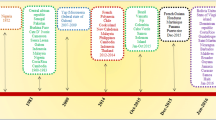
Zika virus (ZIKV) is an arbovirus (arthropod-borne) and belongs to Flavivirus genus within Flaviviridae family. Although first isolated in 1947 (Dick et al. 1952), it was not well studied until the recent outbreak in 2015. The massive outbreak in 2015 in Brazil has linked ZIKV infections with severe neurological complications such as microcephaly in the fetus and Guillain-Barré syndrome (GBS) in adults. Subsequently, World Health Organization (WHO) issued a public health emergency of international concern in 2016 (Gulland 2016; Heymann et al. 2016; WHO 2016a) and called for accelerated development of treatment strategies. A great emphasis was given to understanding the molecular links between ZIKV infections and neurological complications, mechanisms of transmission, rapid diagnostic methods, vaccine, and antiviral drug development. The current review article discusses the latest advancements in the ZIKV research (Fig. 1).
Schematic representation of ZIKV genome and its encoded proteins. a The 10,617 nucleotide ZIKV RNA encodes a polyprotein that gives three structural proteins envelope, premembrane/membrane, capsid protein and seven non-structural proteins NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5. b Structural proteins such as membrane and envelope proteins are displayed on the outer surface of the viral membrane and allow the lipid membrane to wrap around the nucleocapsid
Overview of ZIKV pandemic in North and South America
For more than 60 years, Zika infections were considered as mild infections since most ZIKV infections were either asymptomatic (~ 80%) or characterized by mild symptoms that were short-lived (Zammarchi et al. 2016). The symptoms resembled dengue (flavivirus) and chikungunya viral (alphavirus) infections and include acute fever, maculopapular rash, muscle aches, and eye pain. Until 2007, sporadic cases of ZIKV infections occurred in parts of Africa and Asia (Hayes 2009). From 2007, few outbreaks have been reported in Yap State, Federated States of Micronesia, Western Pacific, and South East Asia (Duffy et al. 2009; Musso et al. 2014b). In 2014, a massive outbreak in French Polynesia with 32,000 cases of infection and a 40-fold rise in GBS was reported (Cao-Lormeau et al. 2016; Mallet et al. 2015).
The first ever evidence of Zika infections in Americas was documented in February 2015 in Brazil’s northeastern state of Rio Grande do Norte (Zanluca et al. 2015). The patients reported maculopapular rash and intense pain much like chikungunya virus (CHIKV) infections. Although no deaths or severe complications were observed in these instances, Zika virus spread was predicted due to the naïve immunological status of the Brazilian population. By January 20, 2016, ZIKV infections spread to Puerto Rico (territory in the USA) and 19 other countries in South America (European Center for Disease Prevention and Control 2015; Pan American health Organization 2016). In Brazil alone, 500,000–1,500,000 suspected cases of Zika virus were confirmed by February 2016. In USA, four indigenous cases transmitted from local mosquitos were established in Florida in July 2016 (McCarthy 2016a). All the four cases in Florida were confined to a specific area in Miami because of an aggressive campaign conducted to prevent mosquito breeding and kill mosquito larvae. On the other hand, the situation in USA territory Puerto Rico reached to alarming levels with the total confirmed 5600 cases by July 2016, including 672 pregnant women (Adams et al. 2016). WHO reported a continuous vectorial transmission in 60 other countries including most of Central and South America, South East Asia, and Africa and hence declared ZIKV as a global public health emergency (European Center for Disease Prevention and Control 2016; WHO 2016e).
In addition to the rapid increase in Zika cases, the current outbreak was considered explosive due to its association with neurological irregularities. In the pregnant women, Zika infection has recently been associated with congenital birth defects. Brazilian Ministry of Health reported a 20-fold increase in patients with microcephaly in 2015 in comparison to historical statistics. The observation of high number of microcephaly cases in the 2015 outbreak may partly be attributed to the availability of more sensitive surveillance protocols and underdiagnosis bias in previous years (Schuler-Faccini et al. 2016; Victora et al. 2016). A recent study suggested that nearly one third of ZIKV-infected pregnant females develop neurological complications such as microcephaly, central nervous system alterations, and fetal cerebral calcifications (Brasil et al. 2016b). Risk of microcephaly was reported to be 1–13% during the first trimester and negligible during second and third trimesters (McCarthy 2016b). Zika virus infection is a pandemic in progress, and many important questions about its teratogenicity, links to microcephaly, and treatment strategies need answers. Yet, it reinforces the possibility that mild infectious agents can emerge as severe infections for human beings.
Virology of ZIKV
ZIKV is an 11 kb positive single-stranded RNA virus that belongs to Flavivirus genus. ZIKV is related to other flaviviruses, more closely with dengue virus (DENV), Japanese encephalitis virus (JEV), yellow fever virus (YFV), and distantly to West Nile virus (WNV). Two important lineages, African and Asian, were identified based on the phylogenetic analyses (Faye et al. 2014).
ZIKV genome consists of two non-coding regions and one coding region. The coding region encodes a polyprotein that makes three structural proteins (capsid, envelope, membrane precursor) and seven non-structural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5). Structure of ZIKV is similar to other flaviviruses, except at Asn180 glycosylation site in glycoproteins that make up the icosahedral shell. The glycosylated moiety at Asn180 was required for viral attachment of host cells and varies among ZIKV strains and flaviviruses (Sirohi et al. 2016). Like other flaviviruses, ZIKV may likely infect host cells by endocytosis after the interaction of virus particles with host cell surface receptors. Receptors such as C-type lectin, phosphatidylserine, T cell immunoglobin and mucin (TIM) and AXL, Tyro3, and Mertk (TAM) are identified as entry factors for various flaviviruses. In case of DENV, AXL receptor was considered as a major receptor for viral entry. AXL activates a cascade of events such as activation of AXL kinase, recruitment of interferon receptor (INFAR), inhibition of innate immune response, and replication of the virus inside the host cells. Role of AXL as a receptor required for the entry of ZIKV is contradictory since in vitro results support and most in vivo mice results question its role as a receptor mediating the viral entry (Hamel et al. 2015; Hastings et al. 2017; Nowakowski et al. 2016; Tabata et al. 2016; Wang et al. 2017; Wells et al. 2016).
ZIKV pathogenicity
ZIKV infections are associated with severe neurological manifestations such as microcephaly and Guillain-Barré syndrome. ZIKV infections are also being linked to other neurological disabilities such as meningoencephalitis, fetal cerebral calcification, central nervous system alterations, and myelitis. However, molecular evidences linking ZIKV infections to these pathological manifestations are largely unknown. Since the recent WHO declaration of ZIKV as a global health concern (Heymann et al. 2016), rapid improvements were made in understanding the molecular mechanisms of the ZIKV pathogenesis (Zhou et al. 2017).
ZIKV transmission
ZIKV transmission can be classified into vector-borne and non-vector borne. In vector-borne transmission, several species of Aedes mosquitos were reported. In non-vector borne human transmission, routes such as transplacental transmission, blood transfusion, and sexual transmission were reported (Besnard et al. 2014; Centers for Infectious Disease Research Policy 2016; Foy et al. 2011; Patino-Barbosa et al. 2015; Sharma and Lal 2017).
Mosquito-borne transmission
Transmission dynamics of ZIKV via mosquitoes is complex, mainly due to the involvement of several mosquito species in ZIKV maintenance. To date, ZIKV has been isolated from 17 Aedes mosquito species as well as Anopheles gambiae, Anopheles coustani, Culex perfuscus, and Mansonia uniformis mosquitoes (Ayres 2016; Saiz et al. 2016; Slavov et al. 2016). Among these several mosquito types, ZIKV transmission to humans has been reported only for female Aedes aegypti, Aedes albopictus, A. hensilli (responsible for Yap Island outbreak), and A. polynesiensis (responsible for French Polynesia outbreak) (Imperato 2016; Lazear and Diamond 2016). A. albopictus mosquitoes are suspected of broader transmission of virus due to their extensive geographic distribution in tropical, sub-tropical, and temperate regions (Thomas et al. 2012). In Americas, A. aegypti and A. albopictus are identified as the major vectors for human transmission (Petersen et al. 2016b). It is presumed that uninfected mosquitoes acquire ZIKV through infected humans, although further studies are needed to confirm whether the viral titer of infected humans are sufficient to infect mosquitoes (Grard et al. 2014). It was suggested that the incubation period for ZIKV in mosquitoes for viral transmission is ~ 10 days (Boorman and Porterfield 1956). An important strategy to prevent mosquito-borne transmission is avoidance of exposure to mosquitos. When possible, pregnant women should delay the travel to the areas of active ZIKV transmission. If travel is unavoidable, women are encouraged to use insect repellents such as DEET and permethrin.
Transplacental transmission
Accumulating evidences suggest that ZIKV is capable of crossing placenta to infect fetal nervous system. This transplacental transmission is supported by the detection of ZIKV RNA and antigens in amniotic fluid, placenta, and visualization of ZIKV in fetal brain tissues (Calvet et al. 2016b; Lazear and Diamond 2016; Petersen et al. 2016b). The mechanism used by ZIKV to cross placental barrier is yet to be known. However, many active studies are being carried to understand this mechanism. Pregnant mice when injected with ZIKV have shown poor intrauterine growth and poor fetal brain development (Microcephaly) suggesting that the virus can cross the placenta (Cugola et al. 2016; Li et al. 2016a, b; Miner et al. 2016a; Wu et al. 2016). In addition, immune-deficient mice injected with ZIKV showed viral particles and RNA in the fetal placenta (Miner et al. 2016a; Quicke et al. 2016). ZIKV isolates are capable of replicating in various cell lines including neuronal, placental, muscle, retinal, pulmonary, colonic, and hepatic cells. The ability of ZIKV isolates to grow in various cell lines explains that the virus can survive and move across cells (Chan et al. 2016). Accumulating evidence as shown above suggest the ZIKV movement across the placenta to cause neuronal tissue damage in infants.
Sexual transmission
ZIKV is also capable of trasmitting through sexual intercourse. Multiple cases of male to female transmission of ZIKV have been reported (Hills et al. 2016; Lazear and Diamond 2016; Mansuy et al. 2016; Moreira et al. 2017; Petersen et al. 2016a; Rowland et al. 2016; Venturi et al. 2016). Several case studies of ZIKV infection in the USA claimed sexual intercourse with infected male partners (returned from ZIKV endemic areas) as a causal factor for transmission to females (Foy et al. 2011). Observations such as replication of ZIKV in testicular lineage cell lines support the survival and prolonged shedding of virus from this anatomical site to spread the infection (Atkinson et al. 2016; D’Ortenzio et al. 2016; Foy et al. 2011; Lazear et al. 2016; Musso et al. 2015; Rossi et al. 2016). The female genital tract cell lines are also susceptible to ZIKV infections, suggesting a possible transmission of the virus from infected males to females through sexual intercourse. Studies using mouse models of vaginal ZIKV infection indicated that transcription factors IRF3 and 7 and type I interferon alpha receptor IFNAR may play a role in viral replication in these sites (Yockey et al. 2016). Recently in 2016, other transmission routes such as male-male and female to male were also reported, thereby raising concerns that ZIKV can spread widely (CDC Prevention Newsroom 2016; Davidson et al. 2016; Deckard et al. 2016; Santora 2016).
Transmission by breastfeeding and blood transfusion
Zika RNA and infective Zika viral particles have been detected in high loads in breast milk of infected mothers (Dupont-Rouzeyrol et al. 2016). ZIKV RNA was also detected in breast milk and serum of two mothers and the sera of their infants (Besnard et al. 2014). However, ZIKV replication was not found in Vero cells inoculated with breast milk. ZIKV infection was also not seen in infants despite the presence of detectable maternal viremia in four mothers, making the transmission via breast milk as inconclusive at the moment (Cavalcanti et al. 2017).
During ZIKV outbreak in French Polynesia, approximately 3% of blood donors were tested positive for ZIKV (CDC 2016; Musso et al. 2014a). The first confirmed case of blood transfusion-related ZIKV infection was reported in Brazil in 2016 (Motta et al. 2016) Subsequently, WHO issue strict guidelines for blood transfusions in areas where ZIKV infections are endemic (Imperato 2016). Until now, there are no reported cases of ZIKV infection due to blood transfusion in the USA; however, as a safety precaution, blood donors are being instructed to report any ZIKV symptoms during 2-week post blood donation.
ZIKV-associated neurological disorders
Microcephaly
Microcephaly is a rare neurological abnormality characterized by poor brain development in infants. Microcephaly infants develop smaller head compared to healthy infants of same age and sex. The ZIKV outbreak in Brazil in 2016 had received much attention because of the surge of ZIKV-associated microcephaly cases, suspecting a possible association (Brasil et al. 2016a, b; Duarte et al. 2017). Microcephaly was reported to occur either alone or as congenital syndrome and is characterized by intellectual disabilities, developmental delay, seizures, vision, and hearing problems in the affected children. Microcephaly can be diagnosed in utero or postnatally (Calvet et al. 2016a; Oliveira Melo et al. 2016). In February 2016, WHO declared a public health emergency due to clusters of association of microcephaly in areas affected by ZIKV infections (WHO 2016c).
In vitro models to understand ZIKV induced microcephaly
The molecular mechanisms underlying the microcephaly and brain damage in infants following ZIKV infection is under intense investigation. Early reports have drawn links between ZIKV infection and microcephaly based on observations on cell tropism of the virus in vitro. ZIKV was found to infect and reduce the cell viability of cultured neuronal progenitor cells and human cortical neurospheres as evidenced by the decrease in expression of cell cycle genes, upregulation of apoptosis, and dysregulation of neuronal cell proliferation (Tang et al. 2016; Cugola et al. 2016; Qian et al. 2016).
Several in vitro studies speculated AXL (a TAM family receptor) as a potential entry receptor for ZIKV. A close correlation of AXL expression and ZIKV tissue tropism made researchers highlight the role of AXL as an entry receptor for ZIKV (Nowakowski et al. 2016). It was suggested that ZIKV preferentially binds to AXL overexpressed cells such as radial glial cells, placental cells, and neural stem cells (astrocytes and neuron precursors) that form the cerebral cortex of the developing fetus brain (Nowakowski et al. 2016; Tabata et al. 2016). AXL expression is also found to be abundant in other anatomical sites such as stem cells of the retina, dermal fibroblasts, and cells of immune and reproductive tissues (Bauer et al. 2012; Graham et al. 2014; Hamel et al. 2015). Hamel et al. tested many receptors of flaviviruses and reported that AXL plays a major role in ZIKV infection of multiple human non-neural cell types (Hamel et al. 2015). Modulation of AXL response through incubation of host cells with AXL neutralizing antibodies, axl siRNA, and CRISPR/Cas9 axl gene deletion reduces the ZIKV infectivity (Hamel et al. 2015; Savidis et al. 2016). AXL was demonstrated to be essential for ZIKV infection of human endothelial cells (Liu et al. 2016). Using engineered AXL receptor and AXL inhibitor R428, Meertens et al. demonstrated that AXL downregulates innate immune signaling and thereby facilitates viral entry into human glial cells (Meertens et al. 2017). All these results strongly suggest that AXL receptor is crucial for ZIKV entry. However, some other in vitro studies on human neuronal progenitor cells called into question the role of AXL in ZIKV infection since inhibition of AXL was found to be insufficient to inhibit ZIKV entry or cell death of neural cells (Wells et al. 2016). In addition to AXL, glycosaminoglycans (GAGs) present in human placenta and porcine brains can bind to ZIKV envelope proteins with high affinity and can act as viral attachment factors (Kim et al. 2017).
Zika virus NS4A and NS4B proteins were found to play a crucial role in ZIKV pathogenesis. NS4A and NS4B proteins deregulate Akt-mTOR signaling in human fetal neural stem cells to inhibit neurogenesis and induce autophagy (Liang et al. 2016). After entry into the host cells, ZIKV replicates in neuronal progenitor cells without triggering the host intrinsic immune responses. Recent studies by Hanners et al. showed that ZIKV survives and replicates in primary human neural progenitors (hNPs) while causing cytopathic effects including hNP cell rounding, pyknosis, and activation of caspase 3 (Hanners et al. 2016). Despite the cytopathic effects, ZIKV infection triggered no significant immune response as observed by the lack of cytokine response. The virus continued to replicate in hNP cells for 28 days while showing only subpar immune responses.
In vitro 3D human organoid models that recapitulate the complex neurological regions of early human embryogenesis are also being used to investigate the association of ZIKV to microcephaly. These cerebral organoid models showed that the virus moves towards neuronal progenitor cells and activates innate immune receptor TLR3 to trigger apoptosis and deplete neuronal progenitor cells (Dang et al. 2016). The proliferative neural cell zones decrease along with disruption of cortical layers (Cugola et al. 2016; Qian et al. 2016). Overall, brain organoid models are very promising in vitro models to understand the molecular mechanisms of ZIKV infection since they contain more than one cell type and probably model cell-to-cell contact-dependent brain development stages. However, the major caveats of this approach are uneven exposure of virus to neural cells and a lack of immune cells to mirror the real in vivo setting.
In vivo mouse models to understand ZIKV induced microcephaly
In vivo models of ZIKV infection are essential to gain mechanistic insights on microcephaly. Many mice models including wild-type, engineered, and immunocompromised mice are being tested to establish links between maternal infection and microcephaly. Studies by Miner et al. suggested that mice fetal brain cells are vulnerable to viral infections irrespective of their maternal genotype. Zika viral infection of mice with baseline immune defects (lower circulating B cells but elevated circulating T cells) causes embryonic damage leading to cortical thinning, cortical malformations including neuronal cell apoptosis in newborns (Cugola et al. 2016). Mice lacking interferon alpha receptor (Ifnar1−/−) or wild-type mice with antibodies against interferon alpha receptors showed placental damage, brain malformation, and fetal death (Miner et al. 2016a) due to ZIKV infection. Other mice models with defective interferon signaling (A129, AG129, and TKO) also showed placental damage, vertical transmission of the virus from placental to fetus, and neural damage in the fetus (Aliota et al. 2016; Dowall et al. 2016; Koppolu et al. 2013; Lazear et al. 2016; Li et al. 2016b; Miner et al. 2016a; Rossi et al. 2016). Interestingly, wild-type C57BL/6 mice with no immune defects did not show any fetal damage when injected at higher dose intravenously but showed microcephaly with vaginal and intraperitoneal exposure (Cugola et al. 2016; Yockey et al. 2016).
To further understand the mechanism underlying microcephaly, Wu et al. have developed a mice model that recapitulated the human ZIKV infections (Nguyen et al. 2016). Direct injection of virus into the lateral ventricle of fetal mouse brain during cortical neurogenesis (embryonic day 13.5) has resulted in viral replication and infection in cerebral cortex. ZIKV virus crossed placental and replicated in radial glial cells of the developing fetus brain when injected into the abdominal cavity of pregnant mice. It was postulated that the placental damage during ZIKV infection can facilitate the entry of the virus into fetal neural cells.
Although most in vitro studies proclaimed that AXL as a major receptor for ZIKV entry and infection, in vivo mice studies contradicted those observations. Wang et al. showed that ZIKV is capable of successfully infecting AXL-deficient mice (Wang et al. 2017). In another study by Hasting et al., TAM family candidate receptors including AXL, Tyro3, and Mertk were found to be not essential for ZIKV infection, mother-to-fetus transmission, and ZIKV tropism in placenta and brain (Hastings et al. 2017). However, the same study showed that AXL could mediate ZIKV infection in vitro. In a similar study, Zika viral RNA was observed in the brain of AXL-deficient mice (Miner et al. 2016b). High level of ZIKV infection was also found in testis and epididymis of ZIKV-infected AXL-deficient mice (Govero et al. 2016). These observations imply that AXL may not be very important for infection in vivo. It is likely that ZIKV utilizes multiple attachment factors or receptors, and further work is required to elucidate the molecular mechanism of entry.
Guillain-Barré syndrome
GBS is an autoimmune demyelinating disorder that causes reduced signal transmissions, progressive muscle weakness, and paralysis. A significant number of GBS cases are found to have ZIKV infections in both recent outbreak in Americas and the previous outbreak in French Polynesia, suspecting a possible association (Araujo et al. 2016; Cao-Lormeau et al. 2016). GBS cases are increased by 20 to 40-fold during the ZIKV outbreak in French Polynesia () (Araujo et al. 2016; Bahia and Bahia 2015). Data released by WHO also showed a substantial increase in GBS cases in South America in 2016 (WHO 2016b, d).
In addition to ZIKV, infections by DENV and CHIKV can lead to GBS. Therefore, an accurate diagnosis of GBS causal agent is critical to choose an adequate treatment. GBD diagnosis is complicated due to overlapping clinical features of GBS with myelitis resulting from direct flaviviral infection of the spinal cord. Recently, a ZIKV-infected immunodeficient mice TKO (triple knockout of interferon regulatory factors 3, 5, 7) and Ifnar1−/− (interferon alpha receptor knockout) showed evidence of direct infection of the spinal cord and live virus in both brain and spinal cord, consistent with myelitis (Lazear et al. 2016). So, a correct distinction of GBS-induced paralysis from myelitis and proper diagnosis of the type of flavivirus causing the GBS are essential factors for choosing an effective treatment strategy (Araujo et al. 2016; Cao-Lormeau et al. 2016).
Other complications associated with ZIKV infections
Eye diseases
ZIKV causes mild eye infections in adults with symptoms such as conjunctivitis and uveitis in adults (Benzekri et al. 2017; Duffy et al. 2009; Furtado et al. 2016). However, ZIKV-related eye infections in infants are much severe and include blindness, optic neuritis, chorioretinal atrophy, bilateral iris coloboma, and intraretinal hemorrhages. ZIKV-related microcephaly case studies revealed ocular abnormalities in 10 out of 29 infants (de Paula Freitas et al. 2016). ZIKV is found to cause panuveitis in mice and sheds from tears (Miner et al. 2016b). The presence of ZIKV in eyes suggests that eyes may act as one of the reservoir hosts for ZIKV following the acute phase of infection.
Meningoencephalitis
ZIKV-related meningoencephalitis can occur rarely. To date, it was observed only in a single case of 81-year-old male returned from ZIKV endemic area (Mecharles et al. 2016). Brain infection resembling meningoencephalitis was seen in immunodeficient mice subjected to intravenous ZIKV injections (Fernandes et al. 2016). These shreds of evidence suggest a possible association of ZIKV infections to meningoencephalitis and thus merit further studies in this direction.
Possible reasons for emergence of ZIKV as neuropathogen
Despite being discovered over 50 years ago, ZIKV was not considered as a potential human neuropathogen until 2015. The possible reasons for the emergence of ZIKV as neuropathogen can be (a) emergence of more virulent strains, (b) adaptation of new routes of viral transmission, (c) genetic differences in populations making some groups more susceptible, and (d) under-diagnosis of ZIKV-associated neurological defects in previous outbreaks in Africa due to poor epidemiological data. Sequence analysis of all 41 known ZIKV RNA open reading frames belonging to different African, Asian, and Americas ZIKV strains indicated that ZIKV has undergone significant changes in both the nucleotide and protein sequences in the past 50 years (Wang et al. 2016). These changes might have made the virus more virulent in neural cells causing severe neurological complications. While emergence of new virulent strains remains a possibility, it is contradicted by the lack of conclusive evidence for differences between strains isolated from Africa and Americas regarding neural tropism or cell death, as shown in existing models (Bayer et al. 2016; Cugola et al. 2016; Lazear et al. 2016; Liang et al. 2016; Qian et al. 2016).
Another possibility could be viral adaptation of new routes of transmission. The only reported transmission route for the virus until a few years ago was vector transmission. Now potential new routes such as sexual and blood transmission have been identified and may have contributed to wider spread of the virus. However, the majority of the ZIKV infections even in the recent outbreak in North and South America are still through mosquitos and thus considered as a less distinct possibility. Susceptibility to ZIKV may be population specific, and genetic differences or prior exposure to other flaviviruses could contribute to increased susceptibility to neurological complications in one population over others. It has been evident that prior infection with one DENV serotype makes the individual more susceptible to other DENV serotypes. Thus, ZIKV may be more effective in causing microcephaly in persons that have been previously exposed to dengue or other flaviviruses. Experimental evidence for this phenomenon was found in in vitro experiments where exposure of DENV immune plasma and monoclonal antibodies caused a 12-fold increase in ZIKV infection (Dejnirattisai et al. 2016). Nonetheless, further understanding of cross-reactivity of ZIKV and other flaviviruses is needed to determine whether specific populations are prone to severe neurological consequences over others.
ZIKV diagnosis
An accurate and timely diagnosis of ZIKV infection is essential to choose correct treatment strategies. Clinical diagnosis of ZIKV is difficult because of its symptoms overlap with other arboviruses and cross-reactivity to other faviviral antibodies present in the serum at the time of infection. Current diagnosis of ZIKV infection includes reverse transcription polymerase chain reaction (RT-PCR) approach that detects virus-specific nucleic acids in the blood or urine samples. Additionally, serological approaches such as ELISA or immunofluorescence assay (IFA) that detects viral antigen-specific antibodies (IgG or IgM) in the patient’s serum are also being considered. However, diagnosis by serological approaches must be confirmed through virus neutralization assays and virus isolation from cell cultures. According to European Center for Disease Control and Prevention (ECDC), a Zika-confirmed case should require a positive identification of Zika viral RNA in RT-PCR, Zika antibodies in serum, confirmation of ZIKV in neutralization test, and isolation of ZIKV virus in cell cultures. A Zika case is considered as probable if only Zika-specific antibodies are found in serum with no further confirmatory tests for the presence of other distinguishing factors.
Nucleic acid screening
Molecular methods to detect ZIKV-specific nucleic acids by RT-PCR are preferred during the acute phase of ZIKV infection because of its high specificity and sensitivity. ZIKV DNA by RT-PCR can be detected up to 2 weeks of symptom onset in urine and saliva samples, and up to 2 months in blood samples. RT-PCR methods that detect either conserved regions of the viral genome or multiplex assays that allows simultaneous detection of ZIKV, DENV, and CHIKV have been developed (Corman et al. 2016; Faye et al. 2013; Faye et al. 2008; Lanciotti et al. 2008; Nicolini et al. 2017; Pyke et al. 2014; Tappe et al. 2014; Waggoner et al. 2016). Recently, a high-throughput and rapid “NASBA-CRISPR Cleavage (NASBACC) RT-PCR method” was developed. NASBA-CRISPR Cleavage (NASBACC) RT-PCR method leverages the sequence-specific nuclease activity of CRISPR/Cas9 and allows for strain differentiation at a single-base resolution in 4 h (Pardee et al. 2016). Other methods such as reverse transcription loop-mediated isothermal amplification (RT-LAMP) and EBOV POC test have allowed the detection of ZIKV rapidly in 40–90 min without the need for RNA extraction (Song et al. 2016; Zhang et al. 2017). A list of RT-PCR methods for diagnosis of ZIKV is shown in Table 1.
In addition to RT-PCR-based molecular assays, next-generation sequencing is also gaining popularity for ZIKV diagnosis (Calvet et al. 2016a; Faria et al. 2016; Mlakar et al. 2016; Sardi et al. 2016; Skredenske et al. 2013). With next-generation sequencing, full genome of the virus can be sequence for proper identification and characterization. Given the small genome size of ZIKV, complete genome sequencing can be done quickly. With the technical advances and reduction in the cost, sequencing can become a routine technology in the laboratories for the detection of ZIKV and other infectious diseases.
Serological approaches
At present, the diagnosis of ZIKV by serological techniques can be quite challenging because of cross-reactivity of ZIKV to sera of other flaviviruses especially when vaccinated or previously infected with other flaviviruses. Immunoassays such as ELISA and IFA detect IgG and IgM antibodies from serum and cerebrospinal fluid. ZIKV-specific antibodies are detectable in serum after 4 days of symptom onset and stay up to 2–12 weeks. Immunoassays detecting ZIKV NS1 antigen are preferred over whole virus or E protein antigens due to the high diversity and less cross-reactivity of NS-1 antigen (Huzly et al. 2016). A positive result in immunoassay is considered as a probable ZIKV case and needs confirmation by neutralization tests, seroconversion, or fourfold increase in ZIKV-specific antibodies in paired serum samples (Rabe et al. 2016).
The current serological diagnostic tests take 2–3 days for getting the results and are authorized to be conducted only in labs that are designated by Center for Disease Control and Prevention (CDC). To rapidly diagnose ZIKV infections within 4 h and to significantly advance the ZIKV testing to commercial and healthcare facility laboratories, a rapid diagnostic test “ZIKV DetectTM IgM Capture ELISA” is being developed (Abbasi 2016). The results from the test are designated as either presumptive Zika positive or possible Zika positive or presumptive another flavivirus positive. In case of patients with previous flavivirus infections, CDC recommends additional orthogonal testing for further confirmation. In addition, Food and Drug Administration (FDA) has issued Emergency Use Authorization (EUA) for different diagnostic methods for presumptive detection of anti-ZIKV IgM antibodies in human sera. A list of these FDA-recommended serological approaches is detailed in Table 1. Based on the current guidelines for ZIKV diagnosis, algorithms that detail the diagnosis approaches were also being developed to assist in proper laboratory diagnosis (Barzon et al. 2016).
Treatment options including vaccines and antiviral drug candidates
Vaccines and antiviral therapeutics to treat Zika infections are currently under trials and may take at least few more years to enter the market. Under this scenario, the best approach to control Zika infections relies on preventing the contact between the vector A. aegypti and humans (especially pregnant women). Avoiding travel to Zika endemic regions, utilizing insect repellents DEET, treat clothing with permethrin, and eliminating standing water to prevent mosquito egg laying and larval development are recommended choices to prevent the infections. Using genetically modified male mosquitoes that express a lethal dominant gene in larva leading to larval death, releasing A. aegypti infected with endosymbiotic bacteria such as Wolbachia that interfere with viral replication in mosquitoes, and use of lethal mosquito traps such as autocidal gravid ovitrap are also being implemented in smaller scale with moderate success (Barrera et al. 2014; Ritchie et al. 2015; Weaver et al. 2016; Wise de Valdez et al. 2011).
Vaccine candidates
The severity of current Zika outbreak and its possible link to microcephaly and other neurological disorders necessitated the urgent development of treatment strategies. Vaccines are currently available for other arthropod-borne flaviviruses such as West Nile virus (WNV), dengue virus (DENV), tick-borne encephalitis virus (TBEV), YFV, and JEV. Attempts to make a ZIKV vaccine took a rapid pace with the recent outbreak. Platforms exploited for ZIKV vaccine development include purified DNA vaccine, purified inactivated viral vaccines, live vectored vaccines, chimeric vaccine, and recombinant protein vaccines (see Table 2 for a list of ZIKV vaccine candidates).
A plasmid DNA vaccine and a purified inactivated virus (PIV) vaccine are being developed by Dan Borouch and his associates (Larocca et al. 2016). Plasmid DNA vaccine was constructed from Zika strain BeH815744 with gene encoding precursor transmembrane (prM) and envelope (E) proteins with the intent that these genes, when transferred to host, will produce proteins that are recognized by the host to develop antibodies against them. A single dose of this prM-E DNA vaccine produced a complete protection to Balb/c mice from subsequent ZIKA-BR (Brazil/ZKV2015) and ZIKA-PR (PR: Puerto Rico PRVABC59) virus challenge, as measured by the absence of detectable viremia, increased Zika-specific neutralizing antibody titers, and increased envelope-specific CD4 and CD8 responses. Passive protection was also observed due to adoptive transfer of IgG antibodies purified from the vaccinated mice even after depletion of CD4 and CD8 lymphocytes. A chimeric vaccine with DENV-2 prM-E genes also generated a robust antibody response and protected mice from subsequent ZIKV challenge (Xie et al. 2017). A purified inactivated virus (PIV) vaccine prepared from ZIKV strain PRVABC59 also demonstrated complete protection against ZIKV infection in mice. In another study, both plasmid prM-E DNA vaccine and PIV vaccine elicited neutralizing antibodies and provided complete protection to rhesus monkeys against ZIKV challenge (Abbink et al. 2016). A recombinant adenovirus serotype 52 vector vaccine expressing ZIKV pre-membrane and envelope proteins also elicited a similar response in rhesus monkeys (Abbink et al. 2016). Observations of robust protection with these vaccine candidates (PIV vaccine, DNA vaccine, and adenovirus serotype 52 vector vaccine) suggest a clear path forward for clinical testing of their efficacy in humans.
Group of researchers led by Dr. David Weiner (Wistar Institute, Philadelphia, USA) have also developed a DNA vaccine candidate expressing the precursor transmembrane (prM) and envelope (E) surface proteins and tested its efficacy in mice and in non-human primate models (Muthumani et al. 2016). The animals when introduced with the vaccine through electroporation, produced antigen-specific cellular and humoral responses, and neutralization activity. A single dose of vaccine elicited protection in immune-deficient mice (lacking interferon alpha and beta receptors) and prevented the viral pathology in brain tissues.
Another investigational vaccine VRC-ZKADNA085-00-VP is under development by National Institute of Allergy and Infectious Diseases (NIAID) at the National Institute of Health (NIH) (Abbasi 2016). The vaccine is also a DNA vaccine encoding the precursor transmembrane M (prM) and envelope (E) proteins from the H/PF/2013 strain of ZIKV. Based on the highly encouraging animal results (as mentioned by NIAID Director Anthony S. Fauci), NIAID is expeditiously performing phase I clinical trial (NCT02840487) in healthy human adults. The initial results of this phase I study intended to examine vaccine safety and ability to stimulate immune responses are encouraging. To further build on the promising phase I results, NIAID initiated a phase 2/2b study in March 2017. The phase 2/2b study consists of two parts. In the first part, 90 healthy men and non-pregnant women from ages 18–35 years will be enrolled from three sites in Houston, Miami, and San Juan (Puerto Rico) and injected with vaccine three times intramuscularly and followed for 32 weeks. In the second part, at least 2400 healthy men and non-pregnant women from ages 18–35 years will be enrolled from USA (Houston, Miami, and San Juan), Costa Rica, Peru, Peru, Brazil, Panama, and Mexico. Participants will be randomly assigned to the vaccine or placebo in three visits in a double-blind study and evaluated for 2 years. NIAID developed a similar DNA vaccine against West Nile virus NY99 strain which demonstrated both safety and efficacy of this type of vaccine and is optimistic of success of ZIKV clinical trials (Ledgerwood et al. 2011).
Other vaccine candidates that are in the early stages of development include an adenovirus serotype-5 vector vaccine (Ad5.ZIKV-Efl) that expresses envelope protein fused to T4 fibritin fold on trimerization domain (Efl) and a subunit recombinant envelope Efl vaccine delivered by carboxymethyl cellulose microneedle array (MNA-ZIKV-rEfl) (Kim et al. 2016). Both vaccine candidates induced ZIKV-specific antibodies and protected C57BL/6 mice. Evaluation of 7-day-old pups born to these mice challenged with lethal dose of intraperitoneal ZIKV injections showed a 100% protection from Ad5.ZIKV-Efl, and 50% protection from MNA-ZIKV-rEfl. Overall, the current anti-ZIKV vaccine strategies utilize a diverse range of molecular approaches targeting pre-membrane and envelope proteins. The success of these approaches would be critical for the fight against ZIKV.
Challenges in developing ZIKV vaccine
Developing a vaccine to treat ZIKV infection is the most effective public health strategy. However, the development of ZIKV vaccine can be challenging. A vaccine developed against one ZIKV serotype could worsen the infections of other serotypes or closely related viruses. This phenomenon is called antibody-dependent enhancement (ADE) and may happen when antibodies generated during a primary infection will not be of enough concentration or avidity to neutralize another serotype, instead causing enhanced infectivity of target cells through virus opsonization and Fc-receptor-mediated endocytosis. In previous studies with DENV (a close relative to ZIKV), antibody-dependent enhancement phenomenon was observed. Individuals who have antibodies against one DENV serotype from prior infection presented severe infections when infected with another DENV serotype than people who do not have antibodies. Recent observations suggested a similar phenomenon for ZIKV (Castanha et al. 2016; Dejnirattisai et al. 2016; Priyamvada et al. 2016; Singh et al. 2017; Stettler et al. 2016). For example, human anti-DENV immunosera and monoclonal antibodies with broad neutralizing activity showed cross-reactivity to ZIKV antigens with varying degrees of neutralization activity but enhanced ZIKV infection (Castanha et al. 2016). The presence of DENV immunosera and monoclonal antibodies enhanced the ZIKV infection by 12-fold in cultured cells (Dejnirattisai et al. 2016). This suggests that pre-existing antibodies to other flavivirus infections can increase the ZIKV infection severity. Nonetheless, antibodies to DENV EDE1 (envelope dimer epitope1) neutralized ZIKV showing that DENV antibodies can be protective in some ways. This implies that a thorough understanding of the interplay between ZIKV strains and other flaviviruses is essential for the design of vaccines for ZIKV.
Human serum antibodies for ZIKV infection
Monoclonal antibodies that can neutralize ZIKV can be used to treat ZIKV infections. In search of candidate therapeutic agents, a group of researchers led by Gopal Sapparapu isolated a panel of 29 antibodies from B cells of patients recovered from Zika infection and tested their immune specificity to envelope protein (ELISA binding assay), neutralizing activity (IC50), and envelope protein epitope recognition patterns (epitope mapping) (Sapparapu et al. 2016). Among the 29 antibodies, two inhibitory antibodies ZIKV-116 and ZIKV-117 showed strong neutralization activity and bound to ZIKV envelope protein at a lateral ridge of DIII (DIII-LR) and DII epitopes, respectively. Both ZIKV-116 and ZIKV-117 antibodies neutralized diverse ZIKV strains encompassing African and Asian-American lineages. ZIKV-117 antibody neutralized MR766 and Dakar 41519 (African), Malaysia P6740 and H/PF/2013 (Asian), Brazil Paraiba 2015 (American) strains and did not cross-react with other DENV and WNV infected cells. ZIKV-116 neutralized four of the five strains (except the original African strain MR766) but was reactive to some dengue-infected cells. Immunization of pregnant mice deficient in type-I interferon signaling with a single dose of ZIKV-117 antibody protected mice against lethal infection, decreased placental damage, and improved fetal recovery in both prophylactic and therapeutic settings.
ZIKV-117 represents the first medical intervention that prevented infections of diverse Zika virus strains in both adult mice and fetuses. ZIKV-117 was also the first antibody for which the epitopic interactions with envelope proteins are identified. The extent to which these results will translate into human protection needs further evaluation. Nonetheless, this gives us a possibility of protecting fetus by administering a natural serum-derived antibody to pregnant women. Regardless of ZIKV infection, women in ZIKV endemic areas can receive antibodies just before pregnancy and during pregnancy to protect the fetus from developing neurological abnormalities.
Antiviral drug candidates
Given the lack of specific knowledge on viral and host proteins essential for ZIKV infections, chemotherapeutic approaches for ZIKV antiviral drug development depend mostly on cell-based screening of pharmacologically active small molecules, and FDA-approved drugs (Table 3). These high-throughput drug repurposing screens were previously explored to develop antiviral drugs for DENV, CHIKV, and other infections (He et al. 2015; Johansen et al. 2015; Kouznetsova et al. 2014; Sun et al. 2014).
Xu et al. have screened ~ 6000 small molecules (including pharmacologically active compounds, approved drugs, and clinical trial active candidates) against ZIKV and identified candidates that inhibit ZIKV replication (antiviral) or suppress infection induced caspase-3 activity (neuroprotective) in many neural cell types (Xu et al. 2016). The identified candidates include a pan-caspase inhibitor emricasan, 10 cyclin-dependent kinase inhibitors (CDKis), and anthelmintic drug niclosamide that are previously approved by the FDA for worm infections. Emricasan has inhibited caspase-3 activity and protected human cortical progenitor cells in both monolayer and 3D organoid cultures. Cyclin-dependent kinase inhibitors were found to inhibit ZIKV replication indicating that ZIKV utilizes CDKs for replication. Combination treatments involving neuroprotective emricasan and antiviral CDK inhibitors showed an additive effect in inhibiting caspase-3 activity and preserving astrocyte viability. Niclosamide showed antiviral properties and inhibited ZIKV replication post-entry into neural cells. Studies prior to FDA approval of niclosamide against worm infections have shown that the drug niclosamide is very well tolerated and poses no risk to the fetus. Niclosamide is not mutagenic, teratogenic, or embryotoxic and can be potentially given to pregnant women.
Similar drug-repurposing screens on 774 FDA-approved drugs in human hepatoma cell line (HuH-7) have found ~ 20 drugs that reduce ZIKV infection (Barrows et al. 2016). The anti-ZIKV activity of these compounds was further validated in human cervical, placental, and neural stem cell lines, as well as primary human amnion cells. These drugs include established antiviral flavivirus drugs such as bortezomib and mycophenolic acid and drugs with previously unknown antiviral activity (e.g., daptomycin). Another screen of ~ 725 FDA-approved drugs in human hepatoma cells (HuH-7) has identified ~ 29 candidates with anti-ZIKV activity. Among which, five candidates lovastatin, 5-fluorouracil, 6-azauridine, kitasamycin, and palonosetron were found to have high anti-ZIKV activity (Pascoalino et al. 2016). All the five candidates belong to different classes, have different structures, and thus possibly have different mechanisms of blocking ZIKV infections. Other screens have identified several broad-spectrum antiviral compounds and pyrimidine synthesis inhibitors that suppress the ZIKV-induced cytopathic effects (Adcock et al. 2017). Another candidate, bromocriptine, had shown inhibitory effects on viral replication by interfering ZIKV NS2B-NS3 protein proteolytic activity (Chan et al. 2017). Overall, different screening studies provided a resource of small molecules that could be tested in animal and clinical models.
Studies have also identified candidates that target specific viral proteins such as viral RNA polymerases (De Clercq and Neyts 2009). Nucleoside analogs target viral RNA polymerases of hepatitis B, hepatitis C, herpes simplex virus, cytomegalovirus, and AIDS. Nucleoside analogs are well tolerated and target viral but not cellular polymerases to cause premature termination of viral replication. Nucleoside analogs, 2′-C-methylated nucleosides, have inhibited ZIKV replication in Vero cells and RNA-dependent RNA polymerase activity in vitro (Eyer et al. 2016; Lu et al. 2016). Sofosbuvir, an FDA-approved ribonucleotide analog (2′-F-2′-C-Me-UTP) targeting NS5 polymerase of hepatitis C virus, have inhibited replication of several ZIKV strains in the human tumor, fetal-derived neural cell lines, and mice models (Bullard-Feibelman et al. 2017). Sofosbuvir inhibited ZIKV RNA-dependent RNA polymerase activity with an IC50 as low as 0.38 μM (Sacramento et al. 2016). In vitro experiments using purified ZIKV NS5 polymerase suggested that sofosbuvir (2′-F-2′-C-Me-UTP) serves as a substrate for ZIKV NS5 polymerase and causes chain termination upon incorporation. Another ribonucleoside analog 2′-C-ethynyl-UTP was found to inhibit ZIKV NS5 polymerase activity (Lu et al. 2016), providing further proof of concept for using ribonucleotide analogs as an effective antiviral treatment strategy against ZIKV. In addition to the NS5 polymerase, Zika proteins NS4A and NS4B can be potential target candidates (Liang et al. 2016).
Very recently in July 2017, Cao et al. showed that an autophagy inhibitor hydrochloroquinone (HCQ) approved by FDA for treating patients with malaria during pregnancy was effective in limiting the maternal-fetal transmission of ZIKV in mice. HCQ-protected mice from placental and fetal ZIKV infections and ameliorated placental and fetal outcomes (Cao et al. 2017). Although the mice placenta is anatomically different from human placenta, the in vivo evidence of promising anti-Zika activity in a mouse model of pregnancy would provide the foundation for experiments in non-human primates and human clinical trials.
Conclusions and outstanding questions
Since the outbreak in Americas in early 2015 and subsequent WHO declaration of ZIKV as public health emergency of international concern in February 2016, a huge amount of data has been generated on ZIKV infections pertinent to ZIKV pathogenesis, transmission routes, diagnosis, and vaccines and antiviral development. In vivo and in vitro models now show clear links between ZIKV and neurological complications. ZIKV is found to be unique as no other mosquito-borne virus is ever found to be associated with congenital disabilities and transmit sexually. Although vast information was gained through clinical observation and basic research, significant knowledge gaps remain in the field. Our immediate focus should be on filling these gaps including (a) detailed molecular mechanism of ZIKV associated neuronal loss, (b) degree of population-specific vulnerability to ZIKV infection, (c) effects of antibody-mediated enhancement on vaccine development, (d) impact of ZIKV on growth and development of children born to infected Zika mothers but with no signs of neurologic defects at birth, and (e) effect of ZIKV on infants and toddlers with relatively plastic brains when a mosquito carrying ZIKV bites them. Our growing knowledge in understanding these challenges and experiences gained from research on similar flaviviruses would tremendously help in our effort to fight the disease. At this moment, it is profoundly uplifting to see neurobiology researchers, clinicians, vaccine, and drug development scientists working collaboratively to respond to this time-sensitive health emergency.
References
Abbasi J (2016) Zika vaccine enters clinical trials. JAMA 316:1249–1249
Abbink P, Larocca RA, De La Barrera RA, Bricault CA, Moseley ET, Boyd M, Kirilova M, Li Z, Ng'ang'a D, Nanayakkara O, Nityanandam R, Mercado NB, Borducchi EN, Agarwal A, Brinkman AL, Cabral C, Chandrashekar A, Giglio PB, Jetton D, Jimenez J, Lee BC, Mojta S, Molloy K, Shetty M, Neubauer GH, Stephenson KE, Peron JP, Zanotto PM, Misamore J, Finneyfrock B, Lewis MG, Alter G, Modjarrad K, Jarman RG, Eckels KH, Michael NL, Thomas SJ, Barouch DH (2016) Protective efficacy of multiple vaccine platforms against Zika virus challenge in rhesus monkeys. Science 353(6304):1129–1132. https://doi.org/10.1126/science.aah6157
Adams L, Bello-Pagan M, Lozier M, Ryff KR, Espinet C, Torres J, Perez-Padilla J, Febo MF, Dirlikov E, Martinez A, Munoz-Jordan J, Garcia M, Segarra MO, Malave G, Rivera A, Shapiro-Mendoza C, Rosinger A, Kuehnert MJ, Chung KW, Pate LL, Harris A, Hemme RR, Lenhart A, Aquino G, Zaki S, Read JS, Waterman SH, Alvarado LI, Alvarado-Ramy F, Valencia-Prado M, Thomas D, Sharp TM, Rivera-Garcia B (2016) Update: ongoing Zika virus transmission—Puerto Rico, November 1, 2015-July 7, 2016. MMWR Morb Mortal Wkly Rep 65(30):774–779. https://doi.org/10.15585/mmwr.mm6530e1
Adcock RS, Chu YK, Golden JE, Chung DH (2017) Evaluation of anti-Zika virus activities of broad-spectrum antivirals and NIH clinical collection compounds using a cell-based, high-throughput screen assay. Antivir Res 138:47–56. https://doi.org/10.1016/j.antiviral.2016.11.018
Aliota MT, Caine EA, Walker EC, Larkin KE, Camacho E, Osorio JE (2016) Characterization of lethal Zika virus infection in AG129 mice. PLoS Negl Trop Dis 10(4):e0004682. https://doi.org/10.1371/journal.pntd.0004682
Araujo AQ, Silva MT, Araujo AP (2016) Zika virus-associated neurological disorders: a review. Brain 139(8):2122–2130. https://doi.org/10.1093/brain/aww158
Atkinson B, Hearn P, Afrough B, Lumley S, Carter D, Aarons EJ, Simpson AJ, Brooks TJ, Hewson R (2016) Detection of Zika virus in semen. Emerg Infect Dis 22(5):940. https://doi.org/10.3201/eid2205.160107
Ayres CF (2016) Identification of Zika virus vectors and implications for control. Lancet Infect Dis 16(3):278–279. https://doi.org/10.1016/S1473-3099(16)00073-6
Bahia SDS, Bahia PN (2015) Dengue, Chikungunya e Zika. 6 deJulho de 2015
Barrera R, Amador M, Acevedo V, Caban B, Felix G, Mackay AJ (2014) Use of the CDC autocidal gravid ovitrap to control and prevent outbreaks of Aedes aegypti (Diptera: Culicidae). J Med Entomol 51(1):145–154. https://doi.org/10.1603/ME13096
Barrows NJ, Campos RK, Powell ST, Prasanth KR, Schott-Lerner G, Soto-Acosta R, Galarza-Munoz G, McGrath EL, Urrabaz-Garza R, Gao J, Wu P, Menon R, Saade G, Fernandez-Salas I, Rossi SL, Vasilakis N, Routh A, Bradrick SS, Garcia-Blanco MA (2016) A screen of FDA-approved drugs for inhibitors of Zika virus infection. Cell Host Microbe 20(2):259–270. https://doi.org/10.1016/j.chom.2016.07.004
Barzon L, Trevisan M, Sinigaglia A, Lavezzo E, Palu G (2016) Zika virus: from pathogenesis to disease control. FEMS Microbiol Lett 363
Bauer T, Zagórska A, Jurkin J, Yasmin N, Köffel R, Richter S, Gesslbauer B, Lemke G, Strobl H (2012) Identification of Axl as a downstream effector of TGF-β1 during Langerhans cell differentiation and epidermal homeostasis. J Exp Med 209(11):2033–2047. https://doi.org/10.1084/jem.20120493
Bayer A, Lennemann NJ, Ouyang Y, Bramley JC, Morosky S, Marques ET Jr, Cherry S, Sadovsky Y, Coyne CB (2016) Type III interferons produced by human placental trophoblasts confer protection against Zika virus infection. Cell Host Microbe 19(5):705–712. https://doi.org/10.1016/j.chom.2016.03.008
Benzekri R, Belfort R, Jr, Ventura CV, de Paula Freitas B, Maia M, Leite M, Labetoulle M, Rousseau A (2017) Ocular manifestations of Zika virus: what we do and do not know. J Fr Ophtalmol
Besnard M, Lastere S, Teissier A, Cao-Lormeau V, Musso D (2014) Evidence of perinatal transmission of Zika virus, French Polynesia, December 2013 and February 2014. Euro Surveill 19
Boorman JP, Porterfield JS (1956) A simple technique for infection of mosquitoes with viruses; transmission of Zika virus. Trans R Soc Trop Med Hyg 50(3):238–242. https://doi.org/10.1016/0035-9203(56)90029-3
Brasil P, Calvet GA, Siqueira AM, Wakimoto M, de Sequeira PC, Nobre A, Quintana Mde S, Mendonca MC, Lupi O, de Souza RV, Romero C, Zogbi H, Bressan Cda S, Alves SS, Lourenco-de-Oliveira R, Nogueira RM, Carvalho MS, de Filippis AM, Jaenisch T (2016a) Zika virus outbreak in Rio de Janeiro, Brazil: clinical characterization, epidemiological and virological aspects. PLoS Negl Trop Dis 10(4):e0004636. https://doi.org/10.1371/journal.pntd.0004636
Brasil P, Pereira JP Jr, Moreira ME, Ribeiro Nogueira RM, Damasceno L, Wakimoto M, Rabello RS, Valderramos SG, Halai UA, Salles TS, Zin AA, Horovitz D, Daltro P, Boechat M, Raja Gabaglia C, Carvalho de Sequeira P, Pilotto JH, Medialdea-Carrera R, Cotrim da Cunha D, Abreu de Carvalho LM, Pone M, Machado Siqueira A, Calvet GA, Rodrigues Baiao AE, Neves ES, Nassar de Carvalho PR, Hasue RH, Marschik PB, Einspieler C, Janzen C, Cherry JD, Bispo de Filippis AM, Nielsen-Saines K (2016b) Zika virus infection in pregnant women in Rio de Janeiro. N Engl J Med 375(24):2321–2334. https://doi.org/10.1056/NEJMoa1602412
Bullard-Feibelman KM, Govero J, Zhu Z, Salazar V, Veselinovic M, Diamond MS, Geiss BJ (2017) The FDA-approved drug sofosbuvir inhibits Zika virus infection. Antivir Res 137:134–140. https://doi.org/10.1016/j.antiviral.2016.11.023
Calvet G, Aguiar RS, Melo AS, Sampaio SA, de Filippis I, Fabri A, Araujo ES, de Sequeira PC, de Mendonca MC, de Oliveira L, Tschoeke DA, Schrago CG, Thompson FL, Brasil P, Dos Santos FB, Nogueira RM, Tanuri A, de Filippis AM (2016a) Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis 16(6):653–660. https://doi.org/10.1016/S1473-3099(16)00095-5
Calvet G, Aguiar RS, Melo ASO, Sampaio SA, de Filippis I, Fabri A, Araujo ESM, de Sequeira PC, de Mendonca MCL, de Oliveira L, Tschoeke DA, Schrago CG, Thompson FL, Brasil P, Dos Santos FB, Nogueira RMR, Tanuri A, de Filippis AMB (2016b) Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: a case study. Lancet Infect Dis 16(6):653–660. https://doi.org/10.1016/S1473-3099(16)00095-5
Cao B, Parnell LA, Diamond MS, Mysorekar IU (2017) Inhibition of autophagy limits vertical transmission of Zika virus in pregnant mice. J Exp Med 214(8):2303–2313. https://doi.org/10.1084/jem.20170957
Cao-Lormeau VM, Blake A, Mons S, Lastere S, Roche C, Vanhomwegen J, Dub T, Baudouin L, Teissier A, Larre P, Vial AL, Decam C, Choumet V, Halstead SK, Willison HJ, Musset L, Manuguerra JC, Despres P, Fournier E, Mallet HP, Musso D, Fontanet A, Neil J, Ghawche F (2016) Guillain-Barre syndrome outbreak associated with Zika virus infection in French Polynesia: a case-control study. Lancet 387(10027):1531–1539. https://doi.org/10.1016/S0140-6736(16)00562-6
Castanha PM, Nascimento EJ, Cynthia B, Cordeiro MT, de Carvalho OV, de Mendonca LR, Azevedo EA, Franca RF, Rafael D, Marques ET, Jr (2016) Dengue virus (DENV)-specific antibodies enhance Brazilian Zika virus (ZIKV) infection. J Infect Dis
Cavalcanti MG, Cabral-Castro MJ, Goncalves JL, Santana LS, Pimenta ES, Peralta JM (2017) Zika virus shedding in human milk during lactation. An unlikely source of infecton? Int J Infect Dis
CDCPreventionNewsroom (2016) First female-to-male sexual transmission of zika virus infection reported in New York City. Available online at: http://www.cdc.gov/media/releases/2016/s0715-zika-female-to-male.html
Centers for Disease Control and Prevention (CDC) (2016) About Zika virus disease. Available at http://www.cdc.gov/zika/about/
Centers for Infectious Disease Research Policy (2016) Brazil confirms blood-transfusion zika; PAHO calls for global support. Available online at: http://www.cidrap.umn.edu/news-perspective/2016/02/brazil-confirms-blood-transfusion-zika-paho-calls-global-support
Chan JF, Yip CC, Tsang JO, Tee KM, Cai JP, Chik KK, Zhu Z, Chan CC, Choi GK, Sridhar S, Zhang AJ, Lu G, Chiu K, Lo AC, Tsao SW, Kok KH, Jin DY, Chan KH, Yuen KY (2016) Differential cell line susceptibility to the emerging Zika virus: implications for disease pathogenesis, non-vector-borne human transmission and animal reservoirs. Emerg Microbes Infect 5(8):e93. https://doi.org/10.1038/emi.2016.99
Chan JF, Chik KK, Yuan S, Yip CC, Zhu Z, Tee KM, Tsang JO, Chan CC, Poon VK, Lu G, Zhang AJ, Lai KK, Chan KH, Kao RY, Yuen KY (2017) Novel antiviral activity and mechanism of bromocriptine as a Zika virus NS2B-NS3 protease inhibitor. Antiviral Res
Corman VM, Rasche A, Baronti C, Aldabbagh S, Cadar D, Reusken CBEM, Pas SD, Goorhuis A, Schinkel J, Molenkamp R, Kümmerer BM, Bleicker T, Brünink S, Eschbach-Bludau M, Eis-Hübinger AM, Koopmans MP, Schmidt-Chanasit J, Grobusch MP, de Lamballerie X, Drosten C, Drexler JF (2016) Clinical comparison, standardization and optimization of Zika virus molecular detection [submitted]. Bull World Health Organ 94(12):880–892. https://doi.org/10.2471/BLT.16.175950
Cugola FR, Fernandes IR, Russo FB, Freitas BC, Dias JL, Guimaraes KP, Benazzato C, Almeida N, Pignatari GC, Romero S, Polonio CM, Cunha I, Freitas CL, Brandao WN, Rossato C, Andrade DG, Faria Dde P, Garcez AT, Buchpigel CA, Braconi CT, Mendes E, Sall AA, Zanotto PM, Peron JP, Muotri AR, Beltrao-Braga PC (2016) The Brazilian Zika virus strain causes birth defects in experimental models. Nature 534(7606):267–271. https://doi.org/10.1038/nature18296
Dang J, Tiwari SK, Lichinchi G, Qin Y, Patil VS, Eroshkin AM, Rana TM (2016) Zika virus depletes neural progenitors in human cerebral organoids through activation of the innate immune receptor TLR3. Cell Stem Cell 19(2):258–265. https://doi.org/10.1016/j.stem.2016.04.014
Davidson A, Slavinski S, Komoto K, Rakeman J, Weiss D (2016) Suspected female-to-male sexual transmission of Zika virus—New York City, 2016. MMWR Morb Mortal Wkly Rep 65(28):716–717. https://doi.org/10.15585/mmwr.mm6528e2
De Clercq E, Neyts J (2009) Antiviral agents acting as DNA or RNA chain terminators. Handb Exp Pharmacol 53–84
Deckard DT, Chung WM, Brooks JT, Smith JC, Woldai S, Hennessey M, Kwit N, Mead P (2016) Male-to-male sexual transmission of Zika virus—Texas, January 2016. MMWR Morb Mortal Wkly Rep 65(14):372–374. https://doi.org/10.15585/mmwr.mm6514a3
Dejnirattisai W, Supasa P, Wongwiwat W, Rouvinski A, Barba-Spaeth G, Duangchinda T, Sakuntabhai A, Cao-Lormeau VM, Malasit P, Rey FA, Mongkolsapaya J, Screaton GR (2016) Dengue virus sero-cross-reactivity drives antibody-dependent enhancement of infection with zika virus. Nat Immunol 17(9):1102–1108. https://doi.org/10.1038/ni.3515
Dick GW, Kitchen SF, Haddow AJ (1952) Zika virus. I. Isolations and serological specificity. Trans R Soc Trop Med Hyg 46(5):509–520. https://doi.org/10.1016/0035-9203(52)90042-4
D'Ortenzio E, Matheron S, Yazdanpanah Y, de Lamballerie X, Hubert B, Piorkowski G, Maquart M, Descamps D, Damond F, Leparc-Goffart I (2016) Evidence of sexual transmission of Zika virus. N Engl J Med 374(22):2195–2198. https://doi.org/10.1056/NEJMc1604449
Dowall SD, Graham VA, Rayner E, Atkinson B, Hall G, Watson RJ, Bosworth A, Bonney LC, Kitchen S, Hewson R (2016) A susceptible mouse model for Zika virus infection. PLoS Negl Trop Dis 10(5):e0004658. https://doi.org/10.1371/journal.pntd.0004658
Duarte G, Moron AF, Timerman A, Fernandes CE, Mariani Neto C, Almeida Filho GL, Werner Junior H, Espirito Santo H, Steibel JAP, Bortoletti Filho J, Andrade JBB, Burla M, Silva de Sa MF, Busso NE, Giraldo PC, Moreira de Sa RA, Passini Junior R, Mattar R, Francisco RPV (2017) Zika virus infection in pregnant women and microcephaly. Rev Bras Ginecol Obstet 39(5):235–248. https://doi.org/10.1055/s-0037-1603450
Duffy MR, Chen TH, Hancock WT, Powers AM, Kool JL, Lanciotti RS, Pretrick M, Marfel M, Holzbauer S, Dubray C, Guillaumot L, Griggs A, Bel M, Lambert AJ, Laven J, Kosoy O, Panella A, Biggerstaff BJ, Fischer M, Hayes EB (2009) Zika virus outbreak on Yap Island, Federated States of Micronesia. N Engl J Med 360(24):2536–2543. https://doi.org/10.1056/NEJMoa0805715
Dupont-Rouzeyrol M, Biron A, O'Connor O, Huguon E, Descloux E (2016) Infectious Zika viral particles in breastmilk. Lancet 387(10023):1051. https://doi.org/10.1016/S0140-6736(16)00624-3
European Centre for Disease Prevention and Control (2015) Zika virus epidemic in the Americas: potential association with microcephaly and Guillain-Barré syndrome. Stockholm, Sweden: European Centre for Disease Prevention and Control. Available at http://ecdc.europa.eu/en/publications/Publications/zika-virus-americas-association-with-microcephaly-rapid-risk-assessment.pdf
European Centre for Disease Prevention and Control (2016) Zika virus disease epidemic. Rapid risk assessment. Seventh update. 8 July 2016. ECDC
Eyer L, Nencka R, Huvarova I, Palus M, Joao Alves M, Gould EA, De Clercq E, Ruzek D (2016) Nucleoside inhibitors of Zika virus. J Infect Dis 214(5):707–711. https://doi.org/10.1093/infdis/jiw226
Faria NR, Azevedo Rdo S, Kraemer MU, Souza R, Cunha MS, Hill SC, Theze J, Bonsall MB, Bowden TA, Rissanen I, Rocco IM, Nogueira JS, Maeda AY, Vasami FG, Macedo FL, Suzuki A, Rodrigues SG, Cruz AC, Nunes BT, Medeiros DB, Rodrigues DS, Nunes Queiroz AL, da Silva EV, Henriques DF, Travassos da Rosa ES, de Oliveira CS, Martins LC, Vasconcelos HB, Casseb LM, Simith Dde B, Messina JP, Abade L, Lourenco J, Carlos Junior Alcantara L, de Lima MM, Giovanetti M, Hay SI, de Oliveira RS, Lemos Pda S, de Oliveira LF, de Lima CP, da Silva SP, de Vasconcelos JM, Franco L, Cardoso JF, Vianez-Junior JL, Mir D, Bello G, Delatorre E, Khan K, Creatore M, Coelho GE, de Oliveira WK, Tesh R, Pybus OG, Nunes MR, Vasconcelos PF (2016) Zika virus in the Americas: early epidemiological and genetic findings. Science 352(6283):345–349. https://doi.org/10.1126/science.aaf5036
Faye O, Faye O, Dupressoir A, Weidmann M, Ndiaye M, Alpha Sall A (2008) One-step RT-PCR for detection of Zika virus. J Clin Virol 43(1):96–101. https://doi.org/10.1016/j.jcv.2008.05.005
Faye O, Faye O, Diallo D, Diallo M, Weidmann M, Sall AA (2013) Quantitative real-time PCR detection of Zika virus and evaluation with field-caught mosquitoes. Virol J 10(1):311. https://doi.org/10.1186/1743-422X-10-311
Faye O, Freire CC, Iamarino A, Faye O, de Oliveira JV, Diallo M, Zanotto PM, Sall AA (2014) Molecular evolution of Zika virus during its emergence in the 20(th) century. PLoS Negl Trop Dis 8(1):e2636. https://doi.org/10.1371/journal.pntd.0002636
Fernandes NC, Nogueira JS, Ressio RA, Cirqueira CS, Kimura LM, Fernandes KR, Cunha MS, Souza RP, Guerra JM (2016) Experimental Zika virus infection induces spinal cord injury and encephalitis in newborn Swiss mice. Exp Toxicol Pathol
Foy BD, Kobylinski KC, Chilson Foy JL, Blitvich BJ, Travassos da Rosa A, Haddow AD, Lanciotti RS, Tesh RB (2011) Probable non-vector-borne transmission of Zika virus, Colorado, USA. Emerg Infect Dis 17(5):880–882. https://doi.org/10.3201/eid1705.101939
Furtado JM, Esposito DL, Klein TM, Teixeira-Pinto T, da Fonseca BA (2016) Uveitis associated with Zika virus infection. N Engl J Med 375(4):394–396. https://doi.org/10.1056/NEJMc1603618
Govero J, Esakky P, Scheaffer SM, Fernandez E, Drury A, Platt DJ, Gorman MJ, Richner JM, Caine EA, Salazar V, Moley KH, Diamond MS (2016) Zika virus infection damages the testes in mice. Nature 540(7633):438–442. https://doi.org/10.1038/nature20556
Graham DK, DeRyckere D, Davies KD, Earp HS (2014) The TAM family: phosphatidylserine-sensing receptor tyrosine kinases gone awry in cancer. Nat Rev Cancer 14(12):769–785. https://doi.org/10.1038/nrc3847
Grard G, Caron M, Mombo IM, Nkoghe D, Mboui Ondo S, Jiolle D, Fontenille D, Paupy C, Leroy EM (2014) Zika virus in Gabon (Central Africa)—2007: a new threat from Aedes albopictus? PLoS Negl Trop Dis 8(2):e2681. https://doi.org/10.1371/journal.pntd.0002681
Gulland A (2016) Zika virus is a global public health emergency, declares WHO. BMJ 352:i657
Hamel R, Dejarnac O, Wichit S, Ekchariyawat P, Neyret A, Luplertlop N, Perera-Lecoin M, Surasombatpattana P, Talignani L, Thomas F, Cao-Lormeau VM, Choumet V, Briant L, Despres P, Amara A, Yssel H, Misse D (2015) Biology of Zika virus infection in human skin cells. J Virol 89(17):8880–8896. https://doi.org/10.1128/JVI.00354-15
Hanners NW, Eitson JL, Usui N, Richardson RB, Wexler EM, Konopka G, Schoggins JW (2016) Western Zika virus in human fetal neural progenitors persists long term with partial cytopathic and limited immunogenic effects. Cell Rep 15(11):2315–2322. https://doi.org/10.1016/j.celrep.2016.05.075
Hastings AK, Yockey LJ, Jagger BW, Hwang J, Uraki R, Gaitsch HF, Parnell LA, Cao B, Mysorekar IU, Rothlin CV, Fikrig E, Diamond MS, Iwasaki A (2017) TAM receptors are not required for Zika virus infection in mice. Cell Rep 19(3):558–568. https://doi.org/10.1016/j.celrep.2017.03.058
Hayes EB (2009) Zika virus outside Africa. Emerg Infect Dis 15(9):1347–1350. https://doi.org/10.3201/eid1509.090442
He S, Lin B, Chu V, Hu Z, Hu X, Xiao J, Wang AQ, Schweitzer CJ, Li Q, Imamura M, Hiraga N, Southall N, Ferrer M, Zheng W, Chayama K, Marugan JJ, Liang TJ (2015) Repurposing of the antihistamine chlorcyclizine and related compounds for treatment of hepatitis C virus infection. Sci Transl Med 7(282):282ra49. https://doi.org/10.1126/scitranslmed.3010286
Heymann DL, Hodgson A, Sall AA, Freedman DO, Staples JE, Althabe F, Baruah K, Mahmud G, Kandun N, Vasconcelos PF, Bino S, Menon KU (2016) Zika virus and microcephaly: why is this situation a PHEIC? Lancet 387(10020):719–721. https://doi.org/10.1016/S0140-6736(16)00320-2
Hills SL, Russell K, Hennessey M, Williams C, Oster AM, Fischer M, Mead P (2016) Transmission of Zika virus through sexual contact with travelers to areas of ongoing transmission—continental United States, 2016. MMWR Morb Mortal Wkly Rep 65(8):215–216. https://doi.org/10.15585/mmwr.mm6508e2
Huzly D, Hanselmann I, Schmidt-Chanasit J, Panning M (2016) High specificity of a novel Zika virus ELISA in European patients after exposure to different flaviviruses. Euro Surveill 21
Imperato PJ (2016) The convergence of a virus, mosquitoes, and human travel in globalizing the Zika epidemic. J Community Health 41(3):674–679. https://doi.org/10.1007/s10900-016-0177-7
Johansen LM, DeWald LE, Shoemaker CJ, Hoffstrom BG, Lear-Rooney CM, Stossel A, Nelson E, Delos SE, Simmons JA, Grenier JM, Pierce LT, Pajouhesh H, Lehar J, Hensley LE, Glass PJ, White JM, Olinger GG (2015) A screen of approved drugs and molecular probes identifies therapeutics with anti-Ebola virus activity. Sci Transl Med 7(290):290ra89. https://doi.org/10.1126/scitranslmed.aaa5597
Kim E, Erdos G, Huang S, Kenniston T, Falo LD Jr, Gambotto A (2016) Preventative vaccines for Zika virus outbreak: preliminary evaluation. EBioMedicine 13:315–320. https://doi.org/10.1016/j.ebiom.2016.09.028
Kim SY, Zhao J, Liu X, Fraser K, Lin L, Zhang X, Zhang F, Dordick JS, Linhardt RJ (2017) Interaction of zika virus envelope protein with glycosaminoglycans. Biochemistry
Koppolu V, Osaka I, Skredenske JM, Kettle B, Hefty PS, Li J, Egan SM (2013) Small-molecule inhibitor of the Shigella flexneri master virulence regulator VirF. Infect Immun 81(11):4220–4231. https://doi.org/10.1128/IAI.00919-13
Kouznetsova J, Sun W, Martinez-Romero C, Tawa G, Shinn P, Chen CZ, Schimmer A, Sanderson P, McKew JC, Zheng W, Garcia-Sastre A (2014) Identification of 53 compounds that block Ebola virus-like particle entry via a repurposing screen of approved drugs. Emerg Microbes Infect 3(12):e84. https://doi.org/10.1038/emi.2014.88
Lanciotti RS, Kosoy OL, Laven JJ, Velez JO, Lambert AJ, Johnson AJ, Stanfield SM, Duffy MR (2008) Genetic and serologic properties of Zika virus associated with an epidemic, Yap State, Micronesia, 2007. Emerg Infect Dis 14(8):1232–1239. https://doi.org/10.3201/eid1408.080287
Larocca RA, Abbink P, Peron JP, Zanotto PM, Iampietro MJ, Badamchi-Zadeh A, Boyd M, Ng'ang'a D, Kirilova M, Nityanandam R, Mercado NB, Li Z, Moseley ET, Bricault CA, Borducchi EN, Giglio PB, Jetton D, Neubauer G, Nkolola JP, Maxfield LF, De La Barrera RA, Jarman RG, Eckels KH, Michael NL, Thomas SJ, Barouch DH (2016) Vaccine protection against Zika virus from Brazil. Nature 536(7617):474–478. https://doi.org/10.1038/nature18952
Lazear HM, Diamond MS (2016) Zika virus: new clinical syndromes and its emergence in the western hemisphere. J Virol 90(10):4864–4875. https://doi.org/10.1128/JVI.00252-16
Lazear HM, Govero J, Smith AM, Platt DJ, Fernandez E, Miner JJ, Diamond MS (2016) A mouse model of Zika virus pathogenesis. Cell Host Microbe 19(5):720–730. https://doi.org/10.1016/j.chom.2016.03.010
Ledgerwood JE, Pierson TC, Hubka SA, Desai N, Rucker S, Gordon IJ, Enama ME, Nelson S, Nason M, Gu W, Bundrant N, Koup RA, Bailer RT, Mascola JR, Nabel GJ, Graham BS, Team VRCS (2011) A West Nile virus DNA vaccine utilizing a modified promoter induces neutralizing antibody in younger and older healthy adults in a phase I clinical trial. J Infect Dis 203(10):1396–1404. https://doi.org/10.1093/infdis/jir054
Li C, Xu D, Ye Q, Hong S, Jiang Y, Liu X, Zhang N, Shi L, Qin CF, Xu Z (2016a) Zika virus disrupts neural progenitor development and leads to microcephaly in mice. Cell Stem Cell 19(5):672. https://doi.org/10.1016/j.stem.2016.10.017
Li H, Saucedo-Cuevas L, Regla-Nava JA, Chai G, Sheets N, Tang W, Terskikh AV, Shresta S, Gleeson JG (2016b) Zika virus infects neural progenitors in the adult mouse brain and alters proliferation. Cell Stem Cell 19(5):593–598. https://doi.org/10.1016/j.stem.2016.08.005
Liang Q, Luo Z, Zeng J, Chen W, Foo SS, Lee SA, Ge J, Wang S, Goldman SA, Zlokovic BV, Zhao Z, Jung JU (2016) Zika virus NS4A and NS4B proteins deregulate Akt-mTOR signaling in human fetal neural stem cells to inhibit neurogenesis and induce autophagy. Cell Stem Cell 19(5):663–671. https://doi.org/10.1016/j.stem.2016.07.019
Liu S, DeLalio LJ, Isakson BE, Wang TT (2016) AXL-mediated productive infection of human endothelial cells by Zika virus. Circ Res 119(11):1183–1189. https://doi.org/10.1161/CIRCRESAHA.116.309866
Lu G, Bluemling GR, Collop P, Hager M, Kuiper D, Gurale BP, Painter GR, De La Rosa A, Kolykhalov AA (2016) Analysis of ribonucleotide 5′-triphosphate analogs as potential inhibitors of zika virus RNA-dependent RNA polymerase using non-radioactive polymerase assays. Antimicrob Agents Chemother
Mallet H, Vial A, Musso D (2015) Bilan de l'épidémie à virus Zika en Polynésie Française 2013–2014. Bull Inf Sanit Épidémiol Stat 2015
Mansuy JM, Dutertre M, Mengelle C, Fourcade C, Marchou B, Delobel P, Izopet J, Martin-Blondel G (2016) Zika virus: high infectious viral load in semen, a new sexually transmitted pathogen? Lancet Infect Dis 16(4):405. https://doi.org/10.1016/S1473-3099(16)00138-9
McCarthy M (2016a) Four in Florida are infected with Zika from local mosquitoes. BMJ 354:i4235
McCarthy M (2016b) Microcephaly risk with Zika infection is 1-13% in first trimester, study shows. BMJ 353:i3048
Mecharles S, Herrmann C, Poullain P, Tran TH, Deschamps N, Mathon G, Landais A, Breurec S, Lannuzel A (2016) Acute myelitis due to Zika virus infection. Lancet 387(10026):1481. https://doi.org/10.1016/S0140-6736(16)00644-9
Meertens L, Labeau A, Dejarnac O, Cipriani S, Sinigaglia L, Bonnet-Madin L, Le Charpentier T, Hafirassou ML, Zamborlini A, Cao-Lormeau VM, Coulpier M, Misse D, Jouvenet N, Tabibiazar R, Gressens P, Schwartz O, Amara A (2017) Axl mediates ZIKA virus entry in human glial cells and modulates innate immune responses. Cell Rep 18(2):324–333. https://doi.org/10.1016/j.celrep.2016.12.045
Miner JJ, Cao B, Govero J, Smith AM, Fernandez E, Cabrera OH, Garber C, Noll M, Klein RS, Noguchi KK, Mysorekar IU, Diamond MS (2016a) Zika virus infection during pregnancy in mice causes placental damage and fetal demise. Cell 165(5):1081–1091. https://doi.org/10.1016/j.cell.2016.05.008
Miner JJ, Sene A, Richner JM, Smith AM, Santeford A, Ban N, Weger-Lucarelli J, Manzella F, Ruckert C, Govero J, Noguchi KK, Ebel GD, Diamond MS, Apte RS (2016b) Zika virus infection in mice causes panuveitis with shedding of virus in tears. Cell Rep 16(12):3208–3218. https://doi.org/10.1016/j.celrep.2016.08.079
Mlakar J, Korva M, Tul N, Popovic M, Poljsak-Prijatelj M, Mraz J, Kolenc M, Resman Rus K, Vesnaver Vipotnik T, Fabjan Vodusek V, Vizjak A, Pizem J, Petrovec M, Avsic Zupanc T (2016) Zika virus associated with microcephaly. N Engl J Med 374(10):951–958. https://doi.org/10.1056/NEJMoa1600651
Moreira J, Peixoto TM, Machado de Siqueira A, Lamas CC (2017) Sexually acquired Zika virus: a systematic review. Clin Microbiol Infect
Motta IJ, Spencer BR, Cordeiro da Silva SG, Arruda MB, Dobbin JA, Gonzaga YB, Arcuri IP, Tavares RC, Atta EH, Fernandes RF, Costa DA, Ribeiro LJ, Limonte F, Higa LM, Voloch CM, Brindeiro RM, Tanuri A, Ferreira OC Jr (2016) Evidence for transmission of Zika virus by platelet transfusion. N Engl J Med 375(11):1101–1103. https://doi.org/10.1056/NEJMc1607262
Musso D, Nhan T, Robin E, Roche C, Bierlaire D, Zisou K, Shan Yan A, Cao-Lormeau VM, Broult J (2014a) Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Euro Surveill 19
Musso D, Nilles EJ, Cao-Lormeau VM (2014b) Rapid spread of emerging Zika virus in the Pacific area. Clin Microbiol Infect 20(10):O595–O596. https://doi.org/10.1111/1469-0691.12707
Musso D, Roche C, Robin E, Nhan T, Teissier A, Cao-Lormeau VM (2015) Potential sexual transmission of Zika virus. Emerg Infect Dis 21(2):359–361. https://doi.org/10.3201/eid2102.141363
Muthumani K, Griffin BD, Agarwal S, Kudchodkar SB, Reuschel EL, Choi H, Kraynyak KA, Duperret EK, Keaton AA, Chung C, Kim YK, Booth SA, Racine T, Yan J, Morrow MP, Jiang J, Lee B, Ramos S, Broderick KE, Reed CC, Khan AS, Humeau L, Ugen KE, Park YK, Maslow JN, Sardesai NY, Joseph Kim J, Kobinger GP, Weiner DB (2016) In vivo protection against ZIKV infection and pathogenesis through passive antibody transfer and active immunisation with a prMEnv DNA vaccine. Npj Vaccines 1(1):16021. https://doi.org/10.1038/npjvaccines.2016.21
Nguyen HN, Qian X, Song H, Ming GL (2016) Neural stem cells attacked by Zika virus. Cell Res 26(7):753–754. https://doi.org/10.1038/cr.2016.68
Nicolini AM, McCracken KE, Yoon JY (2017) Future developments in biosensors for field-ready Zika virus diagnostics. J Biol Eng 11(1):7. https://doi.org/10.1186/s13036-016-0046-z
Nowakowski TJ, Pollen AA, Di Lullo E, Sandoval-Espinosa C, Bershteyn M, Kriegstein AR (2016) Expression analysis highlights AXL as a candidate Zika virus entry receptor in neural stem cells. Cell Stem Cell 18(5):591–596. https://doi.org/10.1016/j.stem.2016.03.012
Oliveira Melo AS, Malinger G, Ximenes R, Szejnfeld PO, Alves Sampaio S, Bispo de Filippis AM (2016) Zika virus intrauterine infection causes fetal brain abnormality and microcephaly: tip of the iceberg? Ultrasound Obstet Gynecol 47(1):6–7. https://doi.org/10.1002/uog.15831
Pan American Health Organization (2016) Zika virus infection. Washington, DC: World Health Organization, Pan American Health Organization. http://www.paho.org/hq/index.php?option=com_topics&view=article&id=427&Itemid=41484&lang=en
Pardee K, Green AA, Takahashi MK, Braff D, Lambert G, Lee JW, Ferrante T, Ma D, Donghia N, Fan M, Daringer NM, Bosch I, Dudley DM, O'Connor DH, Gehrke L, Collins JJ (2016) Rapid, low-cost detection of Zika virus using programmable biomolecular components. Cell 165(5):1255–1266. https://doi.org/10.1016/j.cell.2016.04.059
Pascoalino BS, Courtemanche G, Cordeiro MT, Gil LH, Freitas-Junior L (2016) Zika antiviral chemotherapy: identification of drugs and promising starting points for drug discovery from an FDA-approved library. F1000Res 5:2523. https://doi.org/10.12688/f1000research.9648.1
Patino-Barbosa AM, Medina I, Gil-Restrepo AF, Rodriguez-Morales AJ (2015) Zika: another sexually transmitted infection? Sex Transm Infect 91(5):359. https://doi.org/10.1136/sextrans-2015-052189
de Paula Freitas B, de Oliveira Dias JR, Prazeres J, Sacramento GA, Ko AI, Maia M, Belfort R, Jr (2016) Ocular findings in infants with microcephaly associated with presumed zika virus congenital infection in Salvador, Brazil. JAMA Ophthalmol
Petersen EE, Polen KN, Meaney-Delman D, Ellington SR, Oduyebo T, Cohn A, Oster AM, Russell K, Kawwass JF, Karwowski MP, Powers AM, Bertolli J, Brooks JT, Kissin D, Villanueva J, Munoz-Jordan J, Kuehnert M, Olson CK, Honein MA, Rivera M, Jamieson DJ, Rasmussen SA (2016a) Update: interim guidance for health care providers caring for women of reproductive age with possible Zika virus exposure—United States, 2016. MMWR Morb Mortal Wkly Rep 65(12):315–322. https://doi.org/10.15585/mmwr.mm6512e2
Petersen LR, Jamieson DJ, Powers AM, Honein MA (2016b) Zika Virus. N Engl J Med 374(16):1552–1563. https://doi.org/10.1056/NEJMra1602113
Priyamvada L, Quicke KM, Hudson WH, Onlamoon N, Sewatanon J, Edupuganti S, Pattanapanyasat K, Chokephaibulkit K, Mulligan MJ, Wilson PC, Ahmed R, Suthar MS, Wrammert J (2016) Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc Natl Acad Sci U S A 113(28):7852–7857. https://doi.org/10.1073/pnas.1607931113
Pyke AT, Daly MT, Cameron JN, Moore PR, Taylor CT, Hewitson GR, Humphreys JL, Gair R (2014) Imported zika virus infection from the cook islands into australia, 2014. PLoS Curr 6
Qian X, Nguyen HN, Song MM, Hadiono C, Ogden SC, Hammack C, Yao B, Hamersky GR, Jacob F, Zhong C, Yoon KJ, Jeang W, Lin L, Li Y, Thakor J, Berg DA, Zhang C, Kang E, Chickering M, Nauen D, Ho CY, Wen Z, Christian KM, Shi PY, Maher BJ, Wu H, Jin P, Tang H, Song H, Ming GL (2016) Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell 165(5):1238–1254. https://doi.org/10.1016/j.cell.2016.04.032
Quicke KM, Bowen JR, Johnson EL, McDonald CE, Ma H, O'Neal JT, Rajakumar A, Wrammert J, Rimawi BH, Pulendran B, Schinazi RF, Chakraborty R, Suthar MS (2016) Zika virus infects human placental macrophages. Cell Host Microbe 20(1):83–90. https://doi.org/10.1016/j.chom.2016.05.015
Rabe IB, Staples JE, Villanueva J, Hummel KB, Johnson JA, Rose L, Mts HS, Wasley A, Fischer M, Powers AM (2016) Interim guidance for interpretation of Zika virus antibody test results. MMWR Morb Mortal Wkly Rep 65(21):543–546. https://doi.org/10.15585/mmwr.mm6521e1
Ritchie SA, Townsend M, Paton CJ, Callahan AG, Hoffmann AA (2015) Application of wMelPop Wolbachia strain to crash local populations of Aedes aegypti. PLoS Negl Trop Dis 9(7):e0003930. https://doi.org/10.1371/journal.pntd.0003930
Rossi SL, Tesh RB, Azar SR, Muruato AE, Hanley KA, Auguste AJ, Langsjoen RM, Paessler S, Vasilakis N, Weaver SC (2016) Characterization of a novel murine model to study Zika virus. Am J Trop Med Hyg 94(6):1362–1369. https://doi.org/10.4269/ajtmh.16-0111
Rowland A, Washington CI, Sheffield JS, Pardo-Villamizar CA, Segars JH (2016) Zika virus infection in semen: a call to action and research. J Assist Reprod Genet 33(4):435–437. https://doi.org/10.1007/s10815-016-0684-6
Sacramento CQ, de Melo GR, Rocha N, Hoelz LVB, Mesquita M, de Freitas CS, Fintelman-Rodrigues N, Marttorelli A, Ferreira AC, Barbosa-Lima G, Bastos MM, de Mello Volotao E, Tschoeke DA, Leomil L, Bozza FA, Bozza PT, Boechat N, Thompson FL, de Filippis AM, Bruning K, Souza T (2016) The clinically approved antiviral drug sofosbuvir impairs Brazilian zika virus replication. bioRxiv:061671
Saiz JC, Vazquez-Calvo A, Blazquez AB, Merino-Ramos T, Escribano-Romero E, Martin-Acebes MA (2016) Zika virus: the latest newcomer. Front Microbiol 7:496
Santora M (2016) Twist in Zika outbreak: New York case shows women can spread it to men. Available online at: http://www.nytimes.com/2016/07/16/nyregion/zika-virus-female-to-male-sexual-transmission.html?_r=0
Sapparapu G, Fernandez E, Kose N, Bin C, Fox JM, Bombardi RG, Zhao H, Nelson CA, Bryan AL, Barnes T, Davidson E, Mysorekar IU, Fremont DH, Doranz BJ, Diamond MS, Crowe JE (2016) Neutralizing human antibodies prevent Zika virus replication and fetal disease in mice. Nature 540(7633):443–447. https://doi.org/10.1038/nature20564
Sardi SI, Somasekar S, Naccache SN, Bandeira AC, Tauro LB, Campos GS, Chiu CY (2016) Coinfections of Zika and chikungunya viruses in Bahia, Brazil, identified by metagenomic next-generation sequencing. J Clin Microbiol 54(9):2348–2353. https://doi.org/10.1128/JCM.00877-16
Savidis G, McDougall WM, Meraner P, Perreira JM, Portmann JM, Trincucci G, John SP, Aker AM, Renzette N, Robbins DR, Guo Z, Green S, Kowalik TF, Brass AL (2016) Identification of Zika virus and dengue virus dependency factors using functional genomics. Cell Rep 16(1):232–246. https://doi.org/10.1016/j.celrep.2016.06.028
Schuler-Faccini L, Ribeiro EM, Feitosa IM, Horovitz DD, Cavalcanti DP, Pessoa A, Doriqui MJ, Neri JI, Neto JM, Wanderley HY, Cernach M, El-Husny AS, Pone MV, Serao CL, Sanseverino MT, Brazilian Medical Genetics Society-Zika Embryopathy Task F (2016) Possible association between Zika virus infection and microcephaly—Brazil, 2015. MMWR Morb Mortal Wkly Rep 65(3):59–62. https://doi.org/10.15585/mmwr.mm6503e2
Sharma A, Lal SK (2017) Zika virus: transmission, detection, control, and prevention. Front Microbiol 8:110
Singh MV, Weber EA, Singh VB, Stirpe NE, Maggirwar SB (2017) Preventive and therapeutic challenges in combating Zika virus infection: are we getting any closer? J Neurovirol
Sirohi D, Chen Z, Sun L, Klose T, Pierson TC, Rossmann MG, Kuhn RJ (2016) The 3.8 a resolution cryo-EM structure of Zika virus. Science 352(6284):467–470. https://doi.org/10.1126/science.aaf5316
Skredenske JM, Koppolu V, Kolin A, Deng J, Kettle B, Taylor B, Egan SM (2013) Identification of a small-molecule inhibitor of bacterial AraC family activators. J Biomol Screen 18(5):588–598. https://doi.org/10.1177/1087057112474690
Slavov SN, Otaguiri KK, Kashima S, Covas DT (2016) Overview of Zika virus (ZIKV) infection in regards to the Brazilian epidemic. Braz J Med Biol Res 49:e5420
Song J, Mauk MG, Hackett BA, Cherry S, Bau HH, Liu C (2016) Instrument-free point-of-care molecular detection of Zika virus. Anal Chem 88(14):7289–7294. https://doi.org/10.1021/acs.analchem.6b01632
Stettler K, Beltramello M, Espinosa DA, Graham V, Cassotta A, Bianchi S, Vanzetta F, Minola A, Jaconi S, Mele F, Foglierini M, Pedotti M, Simonelli L, Dowall S, Atkinson B, Percivalle E, Simmons CP, Varani L, Blum J, Baldanti F, Cameroni E, Hewson R, Harris E, Lanzavecchia A, Sallusto F, Corti D (2016) Specificity, cross-reactivity, and function of antibodies elicited by Zika virus infection. Science 353(6301):823–826. https://doi.org/10.1126/science.aaf8505
Sun W, Tanaka TQ, Magle CT, Huang W, Southall N, Huang R, Dehdashti SJ, McKew JC, Williamson KC, Zheng W (2014) Chemical signatures and new drug targets for gametocytocidal drug development. Sci Rep 4:3743
Tabata T, Petitt M, Puerta-Guardo H, Michlmayr D, Wang C, Fang-Hoover J, Harris E, Pereira L (2016) Zika virus targets different primary human placental cells, suggesting two routes for vertical transmission. Cell Host Microbe 20(2):155–166. https://doi.org/10.1016/j.chom.2016.07.002
Tang H, Hammack C, Ogden SC, Wen Z, Qian X, Li Y, Yao B, Shin J, Zhang F, Lee EM, Christian KM, Didier RA, Jin P, Song H, Ming GL (2016) Zika virus infects human cortical neural progenitors and attenuates their growth. Cell Stem Cell 18(5):587–590. https://doi.org/10.1016/j.stem.2016.02.016
Tappe D, Rissland J, Gabriel M, Emmerich P, Gunther S, Held G, Smola S, Schmidt-Chanasit J (2014) First case of laboratory-confirmed Zika virus infection imported into Europe, November 2013. Euro Surveill 19
Thomas SM, Obermayr U, Fischer D, Kreyling J, Beierkuhnlein C (2012) Low-temperature threshold for egg survival of a post-diapause and non-diapause European aedine strain, Aedes albopictus (Diptera: Culicidae). Parasit Vectors 5(1):100. https://doi.org/10.1186/1756-3305-5-100
Venturi G, Zammarchi L, Fortuna C, Remoli ME, Benedetti E, Fiorentini C, Trotta M, Rizzo C, Mantella A, Rezza G, Bartoloni A (2016) An autochthonous case of Zika due to possible sexual transmission, Florence, Italy, 2014. Euro Surveill 21
Victora CG, Schuler-Faccini L, Matijasevich A, Ribeiro E, Pessoa A, Barros FC (2016) Microcephaly in Brazil: how to interpret reported numbers? Lancet 387(10019):621–624. https://doi.org/10.1016/S0140-6736(16)00273-7
Waggoner JJ, Gresh L, Mohamed-Hadley A, Ballesteros G, Davila MJ, Tellez Y, Sahoo MK, Balmaseda A, Harris E, Pinsky BA (2016) Single-reaction multiplex reverse transcription PCR for detection of Zika, chikungunya, and dengue viruses. Emerg Infect Dis 22(7):1295–1297. https://doi.org/10.3201/eid2207.160326
Wang L, Valderramos SG, Wu A, Ouyang S, Li C, Brasil P, Bonaldo M, Coates T, Nielsen-Saines K, Jiang T, Aliyari R, Cheng G (2016) From mosquitos to humans: genetic evolution of Zika virus. Cell Host Microbe 19(5):561–565. https://doi.org/10.1016/j.chom.2016.04.006
Wang Z-Y, Wang Z, Zhen Z-D, Feng K-H, Guo J, Gao N, Fan D-Y, Han D-S, Wang P-G, An J (2017) Axl is not an indispensable factor for Zika virus infection in mice. J Gen Virol 98(8):2061–2068. https://doi.org/10.1099/jgv.0.000886
Weaver SC, Costa F, Garcia-Blanco MA, Ko AI, Ribeiro GS, Saade G, Shi PY, Vasilakis N (2016) Zika virus: history, emergence, biology, and prospects for control. Antivir Res 130:69–80. https://doi.org/10.1016/j.antiviral.2016.03.010
Wells MF, Salick MR, Wiskow O, Ho DJ, Worringer KA, Ihry RJ, Kommineni S, Bilican B, Klim JR, Hill EJ, Kane LT, Ye C, Kaykas A, Eggan K (2016) Genetic ablation of AXL does not protect human neural progenitor cells and cerebral organoids from Zika virus infection. Cell Stem Cell 19(6):703–708. https://doi.org/10.1016/j.stem.2016.11.011
WHO (2016a) Disease outbreak news: Zika virus infection-Dominican Republic. 27 January 2016 [Internet]. Geneve: WHO; 2016
WHO (2016b) Emergencies preparedness, response. Guillain-Barré syndrome –Colombia and Venezuela. Available at http://www.who.int/csr/don/12-february-2016-gbs-colombia-venezuela/en/4 (19 February 2016, date last accessed)
WHO (2016c) WHO statement on the first meeting of the International Health Regulations (2005) (IHR 2005) emergency committee on Zika virus and observed increase in neurological disorders and neonatal malformations. Available at http://www.who.int/mediacentre/news/statements/2016/1st-emergency-committee-zika/en/4 (13 February 2016, date last accessed)
WHO (2016d) Zika situation report. Neurological syndrome and congenital abnormalities. Available at http://www.who.int/mediacentre/news/statements/2016/emergency-committee-zika-microcephaly/en/4 (13 February 2016, date last accessed)
WHO (2016e) Situation report. Zika virus, Microcephaly, Guillain Barré Syndrome, May 26
Wise de Valdez MR, Nimmo D, Betz J, Gong HF, James AA, Alphey L, Black WCT (2011) Genetic elimination of dengue vector mosquitoes. Proc Natl Acad Sci U S A 108(12):4772–4775. https://doi.org/10.1073/pnas.1019295108
Wu KY, Zuo GL, Li XF, Ye Q, Deng YQ, Huang XY, Cao WC, Qin CF, Luo ZG (2016) Vertical transmission of Zika virus targeting the radial glial cells affects cortex development of offspring mice. Cell Res 26(6):645–654. https://doi.org/10.1038/cr.2016.58
Xie X, Yang Y, Muruato AE, Zou J, Shan C, Nunes BT, Medeiros DB, Vasconcelos PF, Weaver SC, Rossi SL, Shi PY (2017) Understanding Zika virus stability and developing a chimeric vaccine through functional analysis. MBio 8
Xu M, Lee EM, Wen Z, Cheng Y, Huang WK, Qian X, Tcw J, Kouznetsova J, Ogden SC, Hammack C, Jacob F, Nguyen HN, Itkin M, Hanna C, Shinn P, Allen C, Michael SG, Simeonov A, Huang W, Christian KM, Goate A, Brennand KJ, Huang R, Xia M, Ming GL, Zheng W, Song H, Tang H (2016) Identification of small-molecule inhibitors of Zika virus infection and induced neural cell death via a drug repurposing screen. Nat Med 22(10):1101–1107. https://doi.org/10.1038/nm.4184
Yockey LJ, Varela L, Rakib T, Khoury-Hanold W, Fink SL, Stutz B, Szigeti-Buck K, Van den Pol A, Lindenbach BD, Horvath TL, Iwasaki A (2016) Vaginal exposure to Zika virus during pregnancy leads to fetal brain infection. Cell 166(5):1247–1256 e4. https://doi.org/10.1016/j.cell.2016.08.004
Zammarchi L, Spinicci M, Bartoloni A (2016) Zika virus: a review from the virus basics to proposed management strategies. Mediterr J Hematol Infect Dis 8:e2016056
Zanluca C, Melo VC, Mosimann AL, Santos GI, Santos CN, Luz K (2015) First report of autochthonous transmission of Zika virus in Brazil. Mem Inst Oswaldo Cruz 110(4):569–572. https://doi.org/10.1590/0074-02760150192
Zhang XA, Li S, Ching J, Feng HY, Yang K, Dolinger DL, Zhang LD, Zhang PH, Liu W, Cao WC (2017) A sensitive and specific point-of-care detection assay for Zaire Ebola virus. Emerg Microbes Infect 6(1):e5. https://doi.org/10.1038/emi.2016.134
Zhou K, Wang L, Yu D, Huang H, Ji H, Mo X (2017) Molecular and cellular insights into Zika virus-related neuropathies. J Neuro-Oncol 23:341–346
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors are full-time employees of MedImmune, Gaithersburg, USA.
Rights and permissions
About this article
Cite this article
Koppolu, V., Shantha Raju, T. Zika virus outbreak: a review of neurological complications, diagnosis, and treatment options. J. Neurovirol. 24, 255–272 (2018). https://doi.org/10.1007/s13365-018-0614-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13365-018-0614-8