Abstract
Purpose
Inflammation is thought to be a vital element in the etiology of cancer-related fatigue (CRF), and circulating blood cell parameters could be important markers of inflammatory response. However, the associations of several major blood cell counts and their derived inflammatory indices with CRF are not well described. The present study aimed to establish whether a relationship exists between the counts of three white blood cell (WBC) types, platelets, and CRF and investigate whether several systemic inflammatory indices were associated with CRF in patients with breast cancer (BC).
Methods
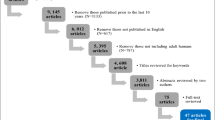
A cross-sectional survey was conducted with a sample of 824 patients with BC undergoing chemotherapy. The cancer fatigue scale was administered to assess CRF. Hematological indicators, including neutrophils, lymphocytes, monocytes, and platelets, were retrieved from routine blood test. Network analyses were used to examine the associations among them.
Results
Among 824 participants, the mean score of CRF was (27 ± 10), ranging from 0 to 57. The results of network models indicated that physical fatigue was negatively linked to lymphocyte counts (weight = − 0.161), and affective fatigue was positively associated with neutrophil counts (weight = 0.070). Additionally, physical fatigue was positively linked to the platelet-to-lymphocyte ratio (PLR) (weight = 0.049).
Conclusion
There were preliminary associations of counts of three WBC types, platelet counts, and systemic inflammatory indices, with distinct dimensions of CRF in patients with BC. Findings provide empirical support for the cellular basis of fatigue-associated inflammatory states.




Similar content being viewed by others
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA Cancer J Clin 71: 209–249
Wijnhoven LMA, Custers JAE, Kwakkenbos L, Prins JB (2022) Trajectories of adjustment disorder symptoms in post-treatment breast cancer survivors. Support Care Cancer 30:3521–3530
Ehrenstein JK, van Zon SKR, Duijts SFA, Stewart RE, Almansa J, Amick BC 3rd, Schagen SB, Bültmann U (2023) Trajectories of cognitive symptoms and associated factors in cancer survivors after return to work: an 18-month longitudinal cohort study. J Cancer Surviv 17:290–299
Bower JE, Wiley J, Petersen L, Irwin MR, Cole SW, Ganz PA (2018) Fatigue after breast cancer treatment: biobehavioral predictors of fatigue trajectories. Health Psychol 37:1025–1034
Bower JE, Ganz PA, Irwin MR, Cole SW, Garet D, Petersen L, Asher A, Hurvitz SA, Crespi CM (2021) Do all patients with cancer experience fatigue? A longitudinal study of fatigue trajectories in women with breast cancer. Cancer 127:1334–1344
Abrahams HJG, Gielissen MFM, Schmits IC, Verhagen C, Rovers MM, Knoop H (2016) Risk factors, prevalence, and course of severe fatigue after breast cancer treatment: a meta-analysis involving 12 327 breast cancer survivors. Ann Oncol 27:965–974
Ruiz-Casado A, Álvarez-Bustos A, de Pedro CG, Méndez-Otero M, Romero-Elías M (2021) Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer 21:10–25
Groenvold M, Petersen MA, Idler E, Bjorner JB, Fayers PM, Mouridsen HT (2007) Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat 105:209–219
Thornton LM, Andersen BL, Carson WE (2007) Elevated cell counts, cortisol and fatigue precede breast cancer recurrence: a controlled, Prospective Study. Annal Behav Med 33:S17–S17
Abrahams HJG, Gielissen MFM, Verhagen C, Knoop H (2018) The relationship of fatigue in breast cancer survivors with quality of life and factors to address in psychological interventions: a systematic review. Clin Psychol Rev 63:1–11
Liu L, Mills PJ, Rissling M, Fiorentino L, Natarajan L, Dimsdale JE, Sadler GR, Parker BA, Ancoli-Israel S (2012) Fatigue and sleep quality are associated with changes in inflammatory markers in breast cancer patients undergoing chemotherapy. Brain Behav Immun 26:706–713
Pertl MM, Hevey D, Boyle NT, Hughes MM, Collier S, O’Dwyer AM, Harkin A, Kennedy MJ, Connor TJ (2013) C-reactive protein predicts fatigue independently of depression in breast cancer patients prior to chemotherapy. Brain Behav Immun 34:108–119
Xiao C, Miller AH, Felger J, Mister D, Liu T, Torres MA (2017) Depressive symptoms and inflammation are independent risk factors of fatigue in breast cancer survivors. Psychol Med 47:1733–1743
Maurer T, Jaskulski S, Behrens S, Jung AY, Obi N, Johnson T, Becher H, Chang-Claude J (2021) Tired of feeling tired – the role of circulating inflammatory biomarkers and long-term cancer related fatigue in breast cancer survivors. The Breast 56:103–109
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, Zhang X, Wang WM, Qiu SJ, Zhou J, Fan J (2014) Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res 20:6212–6222
Fest J, Ruiter R, Ikram MA, Voortman T, van Eijck CHJ, Stricker BH (2018) Reference values for white blood-cell-based inflammatory markers in the Rotterdam Study: a population-based prospective cohort study. Sci Rep 8:10566
Ye Z, Hu T, Wang J, Xiao R, Liao X, Liu M, Sun Z (2022) Systemic immune-inflammation index as a potential biomarker of cardiovascular diseases: a systematic review and meta-analysis. Front Cardiovasc Med 9:933913
Liew PX, Kubes P (2019) The neutrophil’s role during health and disease. Physiol Rev 99:1223–1248
Yang R, Chang Q, Meng X, Gao N, Wang W (2018) Prognostic value of systemic immune-inflammation index in cancer: a meta-analysis J. Cancer 9:3295–3302
Nøst TH, Alcala K, Urbarova I, Byrne KS, Guida F, Sandanger TM, Johansson M (2021) Systemic inflammation markers and cancer incidence in the UK Biobank. Eur J Epidemiol 36:841–848
Rimando J, Campbell J, Kim JH, Tang SC, Kim S (2016) The pretreatment neutrophil/lymphocyte ratio is associated with all-cause mortality in black and white patients with non-metastatic breast cancer. Front Oncol 6:81
Lusho S, Durando X, Mouret-Reynier MA, Kossai M, Lacrampe N, Molnar I, Penault-Llorca F, Radosevic-Robin N, Abrial C (2021) Platelet-to-lymphocyte ratio is associated with favorable response to neoadjuvant chemotherapy in triple negative breast cancer: a study on 120 patients. Front Oncol 11:678315
Park B, Lee HS, Lee JW, Park S (2019) Association of white blood cell count with breast cancer burden varies according to menopausal status, body mass index, and hormone receptor status: a case-control study. Sci Rep 9:5762
Akinbami A, Popoola A, Adediran A, Dosunmu A, Oshinaike O, Adebola P, Ajibola S (2013) Full blood count pattern of pre-chemotherapy breast cancer patients in Lagos, Nigeria Caspian. J Intern Med 4:574–579
Alencar MVOB, Machado KC, Ali ES, Mishra SK, Gomes LF, Sobral ALP, e Sousa JMC, de Souza GF, Melo-Cavalcante AAC, da Silva J (2018) Assessment of chemotherapy on various biochemical markers in breast cancer patients. J Cell Biochem 119:2923–2928
Mehreen L, Khanam A (2005) Evaluation of toxicities induced by chemotherapy in breast cancer patients. Biomed Pharmacother 59:524–527
Avlund K, Hokland M, Mehlsen MY, Thomsen DK, Viidik A, Ekmann A, Zachariae R (2012) Differential associations between white blood cell counts and fatigue in young and older adults. Aging Clin Exp Res 24:439–447
Gerber LH, Stout N, McGarvey C, Soballe P, Shieh CY, Diao G, Springer BA, Pfalzer LA (2011) Factors predicting clinically significant fatigue in women following treatment for primary breast cancer. Support Care Cancer 19:1581–1591
Raison CL, Lin J-MS, Reeves WC (2009) Association of peripheral inflammatory markers with chronic fatigue in a population-based sample. Brain Behav Immun 23:327–337
Hersh EM, Bodey GP (1970) Leukocytic mechanisms in inflammation. Annu Rev Med 21:105-+
Belok SH, Bosch NA, Klings ES, Walkey AJ (2021) Evaluation of leukopenia during sepsis as a marker of sepsis-defining organ dysfunction. PLoS One 16:e0252206
Kennedy G, Norris G, Spence V, McLaren M, Belch JJF (2006) Is chronic fatigue syndrome associated with platelet activation? Blood Coag Fibrinol 17:89–92
LaRosa DF, Orange JS (2008) 1. Lymphocytes. J Allergy Clin Immunol 121:S364–S369
Qi Q, Zhuang L, Shen Y, Geng Y, Yu S, Chen H, Liu L, Meng Z, Wang P, Chen Z (2016) A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 122:2158–2167
Huang L, Chen C, Yang L, Wan R, Hu G (2019) Neutrophil-to-lymphocyte ratio can specifically predict the severity of hypertriglyceridemia-induced acute pancreatitis compared with white blood cell. J Clin Lab Anal 33:e22839
Song M, Graubard BI, Rabkin CS, Engels EA (2021) Neutrophil-to-lymphocyte ratio and mortality in the United States general population. Sci Rep 11:464
Hua Y, Sun JY, Lou YX, Sun W, Kong XQ (2023) Monocyte-to-lymphocyte ratio predicts mortality and cardiovascular mortality in the general population. Int J Cardio 379:118–126
Zhu ML, Chen L, Kong XY, Wang XY, Li XR, Fang Y, Wang J (2022) The systemic immune-inflammation index is an independent predictor of survival in breast cancer patients. Cancer Manag Res 14:775–820
Chen L, Kong X, Yan C, Fang Y, Wang J (2020) The research progress on the prognostic value of the common hematological parameters in peripheral venous blood in breast cancer. Oncotargets Ther 13:1397–1412
Savioli F, Morrow ES, Dolan RD, Romics L, Lannigan A, Edwards J, McMillan DC (2022) Prognostic role of preoperative circulating systemic inflammatory response markers in primary breast cancer: meta-analysis. Br J Surg 109:1206–1215
Hemond CC, Glanz BI, Bakshi R, Chitnis T, Healy BC (2019) The neutrophil-to-lymphocyte and monocyte-to-lymphocyte ratios are independently associated with neurological disability and brain atrophy in multiple sclerosis. BMC Neurol 19:23
Valentine RJ, Woods JA, McAuley E, Dantzer R, Evans EM (2011) The associations of adiposity, physical activity and inflammation with fatigue in older adults. Brain Behav Immun 25:1482–1490
Okuyama T, Akechi T, Kugaya A, Okamura H, Shima Y, Maruguchi M, Hosaka T, Uchitomi Y (2000) Development and validation of the cancer fatigue scale: a brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J Pain Symptom Manage 19:5–14
Okuyama T, Wang XS, Akechi T, Mendoza TR, Hosaka T, Cleeland CS, Uchitomi Y (2003) Validation study of the Japanese version of the brief fatigue inventory. J Pain Symptom Manage 25:106–117
Zou G, Li Y, Xu R, Li P (2018) Resilience and positive affect contribute to lower cancer-related fatigue among Chinese patients with gastric cancer. J Clin Nurs 27:e1412–e1418
Shun SC, Beck SL, Pett MA, Berry PH (2006) Psychometric testing of three Chinese fatigue instruments in Taiwan. J Pain Symptom Manage 32:155–167
Zhang F, Ding Y, Han L (2011) Reliability and validity of the Chinese version of Cancer Fatigue Scale. Chin Ment Health J 25:810–813
Djordjevic D, Rondovic G, Surbatovic M, Stanojevic I, Udovicic I, Andjelic T, Zeba S, Milosavljevic S, Stankovic N, Abazovic D, Jevdjic J, Vojvodic D (2018) Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically ill and injured patients: which ratio to choose to predict outcome and nature of bacteremia? Mediators Inflamm 2018:3758068
Shi X, Li H, Xu Y, Nyalali AMK, Li F (2022) The prognostic value of the preoperative inflammatory index on the survival of glioblastoma patients. Neurol Sci 43:5523–5531
Haslbeck JMB, Waldorp LJ (2020) mgm: estimating time-varying mixed graphical models in high-dimensional data. J Stat Software 93:1–46
Epskamp S, Fried EI (2018) A tutorial on regularized partial correlation networks. Psychol Methods 23:617–634
Haslbeck JMB, Waldorp LJ (2018) How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods 50:853–861
Jones PJ, Ma R, McNally RJ (2021) Bridge centrality: a network approach to understanding comorbidity Multivariate. Behav Res 56:353–367
Robinaugh DJ, Millner AJ, McNally RJ (2016) Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol 125:747–757
Epskamp S, Borsboom D, Fried EI (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 50:195–212
Bower JE, Ganz PA, Aziz N, Fahey JL (2002) Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med 64:604–611
Wratten C, Kilmurray J, Nash S, Seldon M, Hamilton CS, O’Brien PC, Denham JW (2004) Fatigue during breast radiotherapy and its relationship to biological factors. Int J Radiat Oncol Biol Phys 59:160–167
Dan J, Tan J, Huang J, Zhang X, Guo Y, Huang Y, Yang J (2020) The dynamic change of neutrophil to lymphocyte ratio is predictive of pathological complete response after neoadjuvant chemotherapy in breast cancer patients. Breast Cancer 27:982–988
Chou M-L, Babamale AO, Walker TL, Cognasse F, Blum D, Burnouf T (2023) Blood-brain crosstalk: the roles of neutrophils, platelets, and neutrophil extracellular traps in neuropathologies. Trends Neurosci 46:764–779
Bower JE, Lamkin DM (2013) Inflammation and cancer-related fatigue: mechanisms, contributing factors, and treatment implications. Brain Behav Immun 30:S48–S57
Kono SA, Heasley LE, Doebele RC, Camidge DR (2012) Adding to the mix: fibroblast growth factor and platelet-derived growth factor receptor pathways as targets in non-small cell lung cancer. Curr Cancer Drug Targets 12:107–123
Leblanc R, Lee SC, David M, Bordet JC, Norman DD, Patil R, Miller D, Sahay D, Ribeiro J, Clézardin P, Tigyi GJ, Peyruchaud O (2014) Interaction of platelet-derived autotaxin with tumor integrin αVβ3 controls metastasis of breast cancer cells to bone. Blood 124:3141–3150
Cuello-López J, Fidalgo-Zapata A, López-Agudelo L, Vásquez-Trespalacios E (2018) Platelet-to-lymphocyte ratio as a predictive factor of complete pathologic response to neoadjuvant chemotherapy in breast cancer. PLoS One 13:e0207224
Asano Y, Kashiwagi S, Onoda N, Noda S, Kawajiri H, Takashima T, Ohsawa M, Kitagawa S, Hirakawa K (2016) Platelet-lymphocyte ratio as a useful predictor of the therapeutic effect of neoadjuvant chemotherapy in breast cancer. PLoS One 11:e0153459
Turkmen K, Erdur FM, Ozcicek F, Ozcicek A, Akbas EM, Ozbicer A, Demirtas L, Turk S, Tonbul HZ (2013) Platelet-to-lymphocyte ratio better predicts inflammation than neutrophil-to-lymphocyte ratio in end-stage renal disease patients. Hemodial Int 17:391–396
Acknowledgements
We are thankful for the generous contributions of the research participants and the staffs who assisted with data collection during the study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82272923).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Guopeng Li: conceptualization, data acquisition, and writing–original draft. Di Zhao: data collection, and review and editing. Rui Qin: data collection and statistical analysis. Xiangyu Zhao: statistical analysis and review and editing. Zhijun Huo: conceptualization, methodology, project administration, and review and editing. Ping Li: supervision, funding acquisition, writing–original draft, and review and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the University Human Research Ethics Committee (Approval No. 2020-R-053).
Informed consent
Informed consent was obtained from all participants involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, G., Zhao, D., Qin, R. et al. Associations of three differential white blood cell counts, platelet counts, and their derived inflammatory indices with cancer-related fatigue in patients with breast cancer undergoing chemotherapy. Support Care Cancer 32, 486 (2024). https://doi.org/10.1007/s00520-024-08700-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-08700-2