Summary
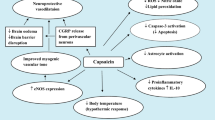
Capsaicin, the most pungent ingredient in red peppers, has been used for centuries to remedy pain. Recently, its role has come under reinvestigation due to evidence that the drug acts selectively on a subpopulation of primary sensory neurons with a nociceptive function. These neurons, besides generating pain sensations, participate through an antidromic activation in the process known as neurogenic inflammation. The first exposure to capsaicin intensely activates these neurons in both senses (orthodromic: pain sensation; antidromic: local reddening, oedema etc.). After the first exposure, the neurons become insensitive to all further stimulation (including capsaicin itself). This evidence led to the proposal of capsaicin as a prototype of an agent producing selective analgesia. This perspective is radically different from previous ‘folk medicine’ cures, where the drug was used as a counter-irritating agent (i.e. for muscular pain). The new concept requires that capsaicin be repeatedly applied on the painful area to obtain the desensitisation of the sensory neurons. Following this idea, capsaicin has been used successfully in controlling pain in postherpetic neuralgia, diabetic neuropathy and other conditions of neuropathic pain. Furthermore, evidence indicates that capsaicin could also control the pain of osteoarthritis. Finally, repeated applications of the drug to the nasal mucosa result in the prevention of cluster headache attacks. On the basis of this evidence, capsaicin appears to be a promising prototype for obtaining selective analgesia in localised pain syndromes.
Similar content being viewed by others
References
Hua XY, Saria A, Gamse R, et al. Multiple tachykinins (neurokinin A, neuropeptide Y, and substance P) in capsaicin-sensitive neurons in guinea-pig. Regul Pept 1985; 133: 1–19
Burgess PR, Perl PR. Myelinated afferent fibres responding specifically to noxious stimulation of the skin. J Physiol (Lond) 1967; 190: 541–62
Szolcziany J. Antidromic vasodilation and neurogenic inflammation. Agents Actions 1988; 23: 4–11
Lembeck F. Sir Thomas Lewis’s nocifensor system, histamine and substance P containing primary afferent nerves. Trends Neurol Sci 1983; 6: 106–8
Jancso G, Kiraly E, Jancso-Gabor A. Pharmacologically induced selective degeneration of chemosensensitive primary sensory neurons. Nature 1977; 270: 741–3
Jancso G, Kiraly E, Jancso-Gabor A, et al. Direct evidence for an axonal site of action of capsaicin. Naunyn Schmiedebergs Arch Pharmacol 1980; 313: 91–4
Nagy I, Maggi CA, Dray A, et al. The role of neurokinin and N-methyl-D aspartate receptors in synaptic transmission form capsaicin-sensitive primary afferent in the rat spinal cord in vitro. Neuroscience 1993; 52: 1029–37
Maggi CA, Santicioli P, Geppetti P, et al. Simultaneous release of substance P and calcitonin gene-related peptide (CGRP)-like immunoreactivity from isolated muscle of the guinea pig urinary bladder. Neurosci Lett 1988; 87: 163–7
Maggi CA, Santicioli P, Geppetti P, et al. Regional differences in the motor response to capsaicin of the guinea-pig urinary bladder: relative role of pre and postjunctional factors related to neuropeptide-containing sensory nerves. Neuroscience 1988; 31: 375–82
Geppetti P, Tramontana M, Evangelista S, et al. Differential effect on neuropeptide release of different concentrations of hydrogen ions on afferent and intrinsic neurons of the rat stomach. Gastroenterology 1991; 101: 1505–11
Jancso N. Desensitization with capsaicin and related acylamides as a tool for studying the function of pain receptors. In: Lin Kill D Armstrong, Pardo EG, editors. Pharmacology of pain. Vol. 9. Oxford: Pergamon Press, 1968: 33
Szallasi A, Blumberg PM. Specific binding of resinoferatoxin, an ultrapotent capsaicin analog, by dorsal root ganglion membranes. Brain Res 1990; 524: 106–11
Szallasi A, Blumberg PM. Mechanisms and therapeutic potential of vanilloids (capsaicin-like molecules). Adv Pharmacol 1993; 24: 123–55
Holtzer P, Bucsics A, Lembeck F. Distribution of (capsaicin-sensitive nerve fibres containing immunoreactive substance P) in cutaneous and visceral tissues of the rat. Neurosci Lett 1982; 31: 253–7
Szallasi A. The vanilloid (capsaicin) receptor: receptor type and species differences. Gen Pharmacol 1994, 25: 223–43
Buck S, Burks T. The neuropharmacology of capsaicin: review of some recent observations. Pharmacol Rev 1986; 38: 179–216
Buck S, Miller MS, Burks TF. Depletion of primary afferent substance Pby capsaicin without altered thermal sensitivity in rats. Brain Res 1982; 233: 216–20
P Geppetti, BM Fusco, M Alessandri, et al. Kallidin applied to the human nasal mucosa produces algesic response not blocked by capsaicin desensitization. Regul Pept 1991; 33: 321–9
Simone D, Ochoa J. Early and late effects of prolonged topical capsaicin on cutaneous sensibility and neurogenic vasodilation in humans. Pain 1991; 47: 285–94
Carpenter SE, Lynn B. Vascular and sensory responses of human skin to mild injury after topical treatment with capsaicin. Br J Pharmacol 1981; 33: 755–8
Geppetti P, Fusco BM, Marabini S, et al. Secretion, pain and sneezing induced by application of capsaicin to the nasal mucosa in man. Br J Pharmacol 1987; 93: 509–14
Jancso G, Lynn B. Possible use of capsaicin in pain therapy. Clin J Pain 1987; 3: 123–6
Lynn B. Actions on nociceptive C-fibers and therapeutical potential. Pain 1990; 41: 61–9
Sjolund BH, Erickson MBE. Stimulation techniques in the management of pain. In: Kosterlitz H, Terenius L, editors. Pain and society. London: Verlac Chemie, 1980: 415
Bernstein JE, Bickers DR, Dahl MV, et al. Treatment of chronic postherpetic neuralgia with topical capsaicin. J Am Acad Dermatol 1987; 17: 93–6
Watson CPN, Evans RJ, Watt VR. Post-herpetic neuralgia and topical capsaicin. Pain 1988; 33: 333–40
Watson CPN, Evans RJ, Watt VR. The post mastectomy pain syndrome and the effect of topical capsaicin. Pain 1989; 38: 177–86
Ross DR, Varipapa RJ. Treatment of painful diabetic neuropathy with topical capsaicin, N Engl J Med 1989; 321: 474–5
Capsaicin Study Group. Treatment of painful diabetic neuropathy with topical capsaicin. Arch Intern Med 1991; 151: 2225–9
Fusco BM, Alessandri M. Effect of topical application of capsaicin in trigeminal neuralgia. Anesth Analg 1992; 74: 375–7
Deal CL, Schnitzer TJ, Lipstein E, et al. Treatment of arthritis with topical capsaicin: a double blind trial. Clin Ther 1991; 13: 383–95
Cheshire WP, Snyder CR. Treatment of reflex sympathetic dystrophy with topical capsaicin. Case report. Pain 1990; 42: 307–11
Wallengren J. Treatment of notalgia paresthetica with topical capsaicin. J Am Acad Dermatol 1990; 24: 286–8
Wallengren J, Klinker M. Successful treatment of notalgia paresthetica with topical capsaicin vehicle. Controlled, double blind, crossover study. J Am Acad Dermatol 1995; 32: 287–9
Morgelander JC, Hurwitz BJ, Massy W. Capsaicin for the treatment of pain in Guillain-Barré syndrome. Ann Neurol 1990; 28: 199
Fusco BM, Marabini S, Maggi CA, et al. Preventative effect of repeated nasal applications of capsaicin in cluster headache. Pain 1994; 59: 321–5
Berger A, Henderson M, Nadoolman W, et al. Oral capsaicin provides temporary relief for oral mucositis pain secondary to chemotherapy/radiation therapy. J Pain Symptom Manage 1995; 10(3): 243–8
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fusco, B.M., Giacovazzo, M. Peppers and Pain. Drugs 53, 909–914 (1997). https://doi.org/10.2165/00003495-199753060-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199753060-00001