Abstract
Background
Clinical trials are currently ongoing to determine the safety and efficacy of active surveillance (AS) versus usual care (surgical and radiation treatment) for women with ductal carcinoma in situ (DCIS). This study aimed to determine upgrade rates of DCIS at needle biopsy to invasive carcinoma at surgery among women who meet the eligibility criteria for AS trials.
Methods
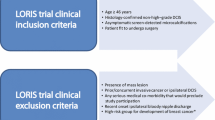
A retrospective review was performed of consecutive women at an academic medical center with a diagnosis of DCIS at needle biopsy from 2007 to 2016. Medical records were reviewed for mode of presentation, imaging findings, biopsy pathology results, and surgical outcomes. Each patient with DCIS was evaluated for AS trial eligibility based on published criteria for the COMET, LORD, and LORIS trials.
Results
During a 10-year period, DCIS was diagnosed in 858 women (mean age 58 years; range 28–89 years). Of the 858 women, 498 (58%) were eligible for the COMET trial, 101 (11.8%) for the LORD trial, and 343 (40%) for the LORIS trial. The rates of upgrade to invasive carcinoma were 12% (60/498) for the COMET trial, 5% (5/101) for the LORD trial, and 11.1% (38/343) for the LORIS trial. The invasive carcinomas ranged from 0.2 to 20 mm, and all were node-negative.
Conclusions
Women who meet the eligibility criteria for DCIS AS trials remain at risk for occult invasive carcinoma at presentation, with upgrade rates ranging from 5 to 12%. These findings suggest that more precise criteria are needed to ensure that women with invasive carcinoma are excluded from AS trials.
Similar content being viewed by others
References
Yamada T, Mori N, Watanabe M, et al. Radiologic-pathologic correlation of ductal carcinoma in situ. Radiographics. 2010;30:1183–98. https://doi.org/10.1148/rg.305095073.
Mitchell KB, Kuerer H. Ductal carcinoma in situ: treatment update and current trends. Curr Oncol Rep. 2015;17:48. https://doi.org/10.1007/s11912-015-0473-x.
Pang JM, Gorringe KL, Fox SB. Ductal carcinoma in situ: update on risk assessment and management. Histopathology. 2016;68:96–109. https://doi.org/10.1111/his.12796.
Rosso KJ, Weiss A, Thompson AM. Are there alternative strategies for the local management of ductal carcinoma in situ? Surg Oncol Clin North Am. 2018;27:69–80. https://doi.org/10.1016/j.soc.2017.08.002.
Bruce J, Thornton AJ, Scott NW, et al. Chronic preoperative pain and psychological robustness predict acute postoperative pain outcomes after surgery for breast cancer. Br J Cancer. 2012;107:937–46. https://doi.org/10.1038/bjc.2012.341.
Miller ME, Muhsen S, Olcese C, et al. Contralateral breast cancer risk in women with ductal carcinoma in situ: is it high enough to justify bilateral mastectomy? Ann Surg Oncol. 2017;24:2889–97. https://doi.org/10.1245/s10434-017-5931-2.
Elshof LE, Tryfonidis K, Slaets L, et al. Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ: the LORD study. Eur J Cancer. 2015;51:1497–510. https://doi.org/10.1016/j.ejca.2015.05.008.
Francis A, Thomas J, Fallowfield L, et al. Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer. 2015;51:2296–303. https://doi.org/10.1016/j.ejca.2015.07.017.
Hwang ES, Hyslop T, Lynch T, et al. The COMET (Comparison of Operative versus Monitoring and Endocrine Therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open. 2019;9:e026797. https://doi.org/10.1136/bmjopen-2018-026797.
Grimm LJ, Shelley Hwang E. Active surveillance for DCIS: the importance of selection criteria and monitoring. Ann Surg Oncol. 2016;23:4134–6. https://doi.org/10.1245/s10434-016-5596-2.
Brennan ME, Turner RM, Ciatto S, et al. Ductal carcinoma in situ at core-needle biopsy: meta-analysis of underestimation and predictors of invasive breast cancer. Radiology. 2011;260:119–28. https://doi.org/10.1148/radiol.11102368.
Brem RF, Schoonjans JM, Goodman SN, et al. Nonpalpable breast cancer: percutaneous diagnosis with 11- and 8-gauge stereotactic vacuum-assisted biopsy devices. Radiology. 2001;219:793–6. https://doi.org/10.1148/radiology.219.3.r01jn34793.
Jackman RJ, Burbank F, Parker SH, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001;218:497–502. https://doi.org/10.1148/radiology.218.2.r01fe35497.
Wahedna Y, Evans AJ, Pinder SE, et al. Mammographic size of ductal carcinoma in situ does not predict the presence of an invasive focus. Eur J Cancer. 2001;37:459–62. https://doi.org/10.1016/s0959-8049(00)00397-x.
Goyal A, Douglas-Jones A, Monypenny I, et al. Is there a role of sentinel lymph node biopsy in ductal carcinoma in situ? Analysis of 587 cases. Breast Cancer Res Treat. 2006;98:311–4. https://doi.org/10.1007/s10549-006-9167-2.
Houssami N, Ciatto S, Ellis I, Ambrogetti D. Underestimation of malignancy of breast core-needle biopsy: concepts and precise overall and category-specific estimates. Cancer. 2007;109:487–95. https://doi.org/10.1002/cncr.22435.
Houssami N, Ambrogetti D, Marinovich ML, et al. Accuracy of a preoperative model for predicting invasive breast cancer in women with ductal carcinoma in situ on vacuum-assisted core needle biopsy. Ann Surg Oncol. 2011;18:1364–71. https://doi.org/10.1245/s10434-010-1438-9.
Kim J, Han W, Lee JW, et al. Factors associated with upstaging from ductal carcinoma in situ following core needle biopsy to invasive cancer in subsequent surgical excision. Breast. 2012;21:641–5. https://doi.org/10.1016/j.breast.2012.06.012.
Trentin C, Dominelli V, Maisonneuve P, et al. Predictors of invasive breast cancer and lymph node involvement in ductal carcinoma in situ initially diagnosed by vacuum-assisted breast biopsy: experience of 733 cases. Breast. 2012;21:635–40. https://doi.org/10.1016/j.breast.2012.06.009.
Schulz S, Sinn P, Golatta M, et al. Prediction of underestimated invasiveness in patients with ductal carcinoma in situ of the breast on percutaneous biopsy as rationale for recommending concurrent sentinel lymph node biopsy. Breast. 2013;22:537–42. https://doi.org/10.1016/j.breast.2012.11.002.
Parikh U, Chhor CM, Mercado CL. Ductal carcinoma in situ: the whole truth. AJR Am J Roentgenol. 2018;210:246–55. https://doi.org/10.2214/ajr.17.18778.
Lamb LR, Lehman CD, Oseni TO, Bahl M. Ductal carcinoma in situ (DCIS) at breast MRI: predictors of upgrade to invasive carcinoma. Acad Radiol. 2019. Epub ahead of print. https://doi.org/10.1016/j.acra.2019.09.025.
Grimm LJ, Ryser MD, Partridge AH, et al. Surgical upstaging rates for vacuum-assisted biopsy-proven DCIS: implications for active surveillance trials. Ann Surg Oncol. 2017;24:3534–40. https://doi.org/10.1245/s10434-017-6018-9.
Elmore JG, Longton GM, Carney PA, et al. Diagnostic concordance among pathologists interpreting breast biopsy specimens. JAMA. 2015;313:1122–32. https://doi.org/10.1001/jama.2015.1405.
Pilewskie M, Stempel M, Rosenfeld H, et al. Do LORIS trial eligibility criteria identify a ductal carcinoma in situ patient population at low risk of upgrade to invasive carcinoma? Ann Surg Oncol. 2016;23:3487–93. https://doi.org/10.1245/s10434-016-5268-2.
Soumian S, Verghese ET, Booth M, et al. Concordance between vacuum-assisted biopsy and postoperative histology: implications for the proposed Low-Risk DCIS Trial (LORIS). Eur J Surg Oncol. 2013;39:1337–40. https://doi.org/10.1016/j.ejso.2013.09.028.
Podoll MB, Reisenbichler ES, Roland L, et al. Feasibility of the less-is-more approach in treating low-risk ductal carcinoma in situ diagnosed on core needle biopsy: ten-year review of ductal carcinoma in situ upgraded to invasion at surgery. Arch Pathol Lab Med. 2018;142:1120–6. https://doi.org/10.5858/arpa.2017-0268-oa.
Ryser MD, Worni M, Turner EL, et al. Outcomes of active surveillance for ductal carcinoma in situ: a computational risk analysis. J Natl Cancer Inst. 2015;108. https://doi.org/10.1093/jnci/djv372.
Shi B, Grimm LJ, Mazurowski MA, et al. Can occult invasive disease in ductal carcinoma in situ be predicted using computer-extracted mammographic features? Acad Radiol. 2017;24:1139–47. https://doi.org/10.1016/j.acra.2017.03.013.
Lin CY, Mooney K, Choy W, et al. Will oncotype DX DCIS testing guide therapy? A single-institution correlation of oncotype DX DCIS results with histopathologic findings and clinical management decisions. Mod Pathol. 2018;31:562–8. https://doi.org/10.1038/modpathol.2017.172.
Shi B, Grimm LJ, Mazurowski MA, et al. Prediction of occult invasive disease in ductal carcinoma in situ using deep learning features. J Am Coll Radiol. 2018;15(3 Pt B):527–34. https://doi.org/10.1016/j.jacr.2017.11.036.
Lehman CD, Gatsonis C, Romanoff J, et al. Association of magnetic resonance imaging and a 12-gene expression assay with breast ductal carcinoma in situ treatment. JAMA Oncol. 2019;5:1036–42. https://doi.org/10.1001/jamaoncol.2018.6269.
Zhu Z, Harowicz M, Zhang J, et al. Deep learning analysis of breast MRIs for prediction of occult invasive disease in ductal carcinoma in situ. Comput Biol Med. 2019;115:103498. https://doi.org/10.1016/j.compbiomed.2019.103498.
Acknowledgement
This work was supported by the Agfa HealthCare/Radiological Society of North America (RSNA) Research Scholar Grant (Principal Investigator (PI): Dr. Manisha Bahl) and the Electronic Space Systems Corporation (ESSCO)-MGH Breast Cancer Research Fund (PI: Dr. Manisha Bahl and Dr. Tawakalitu O. Oseni).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Constance D. Lehman has served as an advisory board member for GE Healthcare, and her institution has received research support from GE Healthcare. Tawakalitu O. Oseni, Barbara L. Smith, Charmi A. Vijapura, Niveditha Pinnamaneni, and Manisha Bahl declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Oseni, T.O., Smith, B.L., Lehman, C.D. et al. Do Eligibility Criteria for Ductal Carcinoma In Situ (DCIS) Active Surveillance Trials Identify Patients at Low Risk for Upgrade to Invasive Carcinoma?. Ann Surg Oncol 27, 4459–4465 (2020). https://doi.org/10.1245/s10434-020-08576-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08576-6