Abstract
Background: Most melanoma patients with a positive sentinel lymph node dissection (SLND) undergo a completion lymph node dissection (CLND) that does not yield additional positive nonsentinel lymph nodes (NSLN). This study was designed to determine if NSLN status can be predicted using patient, primary tumor, and sentinel lymph node (SLN) characteristics.
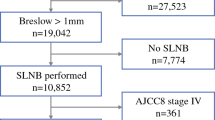
Methods: The study population includes melanoma patients who had a positive SLND and subsequently underwent CLND retrieved from our prospective institutional melanoma database. The primary tumor and SLN pathologies were prospectively determined. An Size/Ulceration (SU) score was derived by assigning 1 point for primary tumor ulceration and 1 point for SLN tumor size >2 mm.
Results: Ninety-eight patients had a positive SLND and underwent CLND. Sixteen of these patients had a positive NSLN. On univariate analysis, primary tumor characteristics (thickness, ulceration, no regression), SLN metastasis characteristics (size >2 mm, location nonsubcapsular), and SU score were all significantly associated with positive NSLN status. However, on multivariate analysis, only the SU score was a significant independent predictor of NSLN status. No patient with an SU score of 0 had a positive NSLN.
Conclusions: The SU score is predictive of NSLN status in patients with a positive SLND. Patients with an SU score of 0 are very unlikely to have positive NSLNs at CLND.
Similar content being viewed by others
REFERENCES
Gershenwald JE, Colome MI, Lee JE, et al. Patterns of recurrence following a negative sentinel lymph node biopsy in 243 patients with stage I or II melanoma. J Clin Oncol 1998; 16: 2253–60.
Morton DL, Wen DR, Foshag LJ, Essner R, Cochran A. Intraoperative lymphatic mapping and selective cervical lymphadenectomy for early-stage melanomas of the head and neck. J Clin Oncol 1993; 11: 1751–6.
Reintgen D, Cruse CW, Wells K, et al. The orderly progression of melanoma nodal metastases. Ann Surg 1994; 220: 759–67.
Krag DN, Meijer SJ, Weaver DL, et al. Minimal-access surgery for staging of malignant melanoma. Arch Surg 1995; 130: 654–8.
Gershenwald JE, Thompson W, Mansfield PF, et al. Multi-institutional melanoma lymphatic mapping experience: the prognostic value of sentinel lymph node status in 612 stage I or II melanoma patients. J Clin Oncol 1999; 17: 976–83.
Cascinelli N, Belli F, Santinami M, et al. Sentinel lymph node biopsy in cutaneous melanoma: the WHO Melanoma Program experience. Ann Surg Oncol 2000; 7: 469–74.
Albertini JJ, Cruse CW, Rapaport D, et al. Intraoperative radio-lympho-scintigraphy improves sentinel lymph node identification for patients with melanoma. Ann Surg 1996; 223: 217–24.
Thompson JF, McCarthy WH, Bosch CM, et al. Sentinel lymph node status as an indicator of the presence of metastatic melanoma in regional lymph nodes. Melanoma Res 1995; 5: 255–60.
Kelley MC, Ollila DW, Morton DL. Lymphatic mapping and sentinel lymphadenectomy for melanoma. Semin Surg Oncol 1998; 14: 283–90.
McMasters KM, Reintgen DS, Ross MI, et al. Sentinel lymph node biopsy for melanoma: controversy despite widespread agreement. J Clin Oncol 2001; 19: 2851–5.
Houghton A, Coit D, Bloomer W, et al. NCCN melanoma practice guidelines. National Comprehensive Cancer Network. Oncology (Huntingt) 1998; 12: 153–77.
Balch CM, Soong S, Ross MI, et al. Long-term results of a multi-institutional randomized trial comparing prognostic factors and surgical results for intermediate thickness melanomas (1.0 to 4.0 mm). Intergroup Melanoma Surgical Trial. Ann Surg Oncol 2000; 7: 87–97.
Cascinelli N, Morabito A, Santinami M, MacKie RM, Belli F. Immediate or delayed dissection of regional nodes in patients with melanoma of the trunk: a randomised trial. WHO Melanoma Programme. Lancet 1998; 351: 793–6.
Morton DL, Wen DR, Wong JH, et al. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 1992; 127: 392–9.
Sabel MS, Gibbs JF, Cheney R, McKinley BP, Lee JS, Kraybill WG. Evolution of sentinel lymph node biopsy for melanoma at a National Cancer Institute-designated cancer center. Surgery 2000; 128: 556–63.
Wagner JD, Gordon MS, Chuang TY, et al. Predicting sentinel and residual lymph node basin disease after sentinel lymph node biopsy for melanoma. Cancer 2000; 89: 453–62.
Morton DL, Thompson JF, Essner R, et al. Validation of the accuracy of intraoperative lymphatic mapping and sentinel lymphadenectomy for early-stage melanoma: a multicenter trial. Multicenter Selective Lymphadenectomy Trial Group. Ann Surg 1999; 230: 453–63.
Bilchik AJ, Giuliano A, Essner R, et al. Universal application of intraoperative lymphatic mapping and sentinel lymphadenectomy in solid neoplasms. Cancer J Sci Am 1998; 4: 351–8.
Haddad FF, Stall A, Messina J, et al. The progression of melanoma nodal metastasis is dependent on tumor thickness of the primary lesion. Ann Surg Oncol 1999; 6: 144–9.
Starz H, Balda BR, Kramer KU, Buchels H, Wang H. A micromorphometry-based concept for routine classification of sentinel lymph node metastases and its clinical relevance for patients with melanoma. Cancer 2001; 91: 2110–21.
Reeves ME, Coit DG. Melanoma. A multidisciplinary approach for the general surgeon. Surg Clin North Am 2000; 80: 581–601.
Coit DG. How we do it: the Memorial Sloan-Kettering Cancer Center approach to sentinel lymph node biopsy. In: Cody HS, ed. Sentinel Lymph Node Biopsy. London: Martin Dunitz, Ltd., 2002: 135–42.
Clopper CJ, Pearson ES. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 1934; 26: 404.
McMasters KM, Edwards MJ, Ross MI, et al. Frequency of non-sentinel lymph node metastasis in melanoma. SSO 54th Annual Cancer Symposium 2001; 54: 16.
Wrightson WR, Wong SL, Edwards MJ, et al. Reverse transcriptase-polymerase chain reaction (RT-PCR) analysis of nonsentinel nodes following completion lymphadenectomy for melanoma. J Surg Res 2001; 98: 47–51.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reeves, M.E., Delgado, R., Busam, K.J. et al. Prediction of Nonsentinel Lymph Node Status in Melanoma. Ann Surg Oncol 10, 27–31 (2003). https://doi.org/10.1245/ASO.2003.03.020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1245/ASO.2003.03.020