Abstract
BACKGROUND:
Obesity is a common health problem that requires a long-term care approach. We systematically reviewed long-term (≥2 y) studies investigating dietary/lifestyle, pharmacologic, and surgical weight loss methods to assess (1) weight loss efficacy, defined by absolute weight loss and the proportion of subjects with ≥5% weight loss, (2) effects of weight loss on cardiovascular risk factors, and (3) applicability of findings from studies to everyday clinical practice.
METHODS:
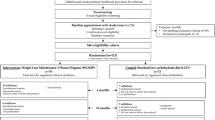
The MEDLINE, HealthSTAR, and the Cochrane Controlled Trials databases were searched for studies investigating the long-term efficacy of weight loss methods in overweight and obese adults. Data were extracted for (i) weight loss after 1 y (pharmacologic studies only), 2 y, 3 y, and 4 y, (ii) proportion of subjects with ≥5% weight loss at the end of follow-up, and (iii) changes (end-of follow-up minus baseline values) in blood lipids, fasting blood glucose, and systolic and diastolic blood pressure.
RESULTS:
Dietary/lifestyle therapy provides <5 kg weight loss after 2–4 y, pharmacologic therapy provides 5–10 kg weight loss after 1–2 y, and surgical therapy provides 25–75 kg weight loss after 2–4 y. Weight loss of ≥5% baseline weight is not consistently associated with improvements in cardiovascular risk factors and these benefits appear to be intervention specific and occur mainly in people with concomitant cardiovascular risk factors. Weight loss studies have methodologic limitations that restrict the applicability of findings to unselected obese people assessed in everyday clinical practice. These limitations include an inadequate study duration, large proportions of subjects lost to follow-up, a lack of an appropriate usual care group, and a lack of reporting of outcomes in high-risk subgroups.
CONCLUSIONS:
Dietary/lifestyle and pharmacologic weight loss interventions provide modest weight loss, and may improve markers of cardiovascular risk factors although these benefits occur mainly in patients with cardiovascular risks. Studies investigating weight loss have methodologic limitations that restrict the applicability of findings to obese patients assessed in clinical practice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Mokdad AH, Serdula MK, Dietz WH, Bowman BA, Marks JS, Koplan JP . The spread of the obesity epidemic in the United States, 1991–1998. JAMA 1999; 282: 1519–1522.
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the Evidence Report. Obes Res 1998; 6 (Suppl 2): 51S–209S.
World Health Organization Consultation on Obesity. Global prevalence and secular trends in obesity. In: Obesity: preventing and managing the global epidemic. World Health Organization: Geneva, Switzerland; 1998. pp 17–40.
Rabkin SW, Chen Y, Leiter L, Liu L, Reeder BA, the Canadian Heart Health Surveys Research Group. Risk factor correlates of body mass index. Can Med Assoc J 1997; 157 (Suppl 1): S26–S31.
Pi-Sunyer FX . Medical hazards of obesity. Ann Intern Med 1993; 119: 655–660.
Bianchini F, Kaaks R, Vainio H . Overweight, obesity, and cancer risk. Lancet Oncol 2002; 3: 565–574.
National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med 2000; 160: 898–904.
Flegal KM, Carroll MD, Ogden CL, Johnson CL . Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002; 288: 1723–1727.
National Center for Health Statistics. Prevalence of overweight and obesity among adults: United States, 1999. Hyatsville, MD. National Center for Health Statistics, Health E-Stats, 2000. Available at http://www.cdc.gov/nchs/products/pubs/hestats/obese/obse99.htm . Accessed June 1, 2002.
Katzmarzyk PT . The Canadian obesity epidemic, 1985–1998. Can Med Assoc J 2002; 166: 1039–1040.
Seidell JC . The epidemiology of obesity. In: Björntorp P (ed). International textbook of obesity. John Wiley & Sons Ltd: Chichester; 2001. pp 23–29.
Martorell R, Kettel-Khan L, Hughes ML, Grummer-Strawn LM . Obesity in women from developing countries. Eur J Clin Nutr 2000; 54: 247–252.
Jeffcoate W . Obesity is a disease: food for thought. Lancet 1998; 351: 903–904.
Rippe JM, Crossley S, Ringer R . Obesity as a chronic disease: modern medical and lifestyle management. J Am Diet Assoc 1998; 98 (Suppl 2): 9S–15S.
Rössner S . Long-term intervention strategies in obesity treatment. Int J Obes Relat Metab Disord 1995; 19: S29–S33.
Björntorp P . Obesity. Lancet 1997; 350: 423–426.
Atkinson RL . A 33-year old woman with morbid obesity. JAMA 2000; 283: 3236–3243.
Walker AR . Obesity: a time bomb to be defused. Lancet 1998; 352: 912.
Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Executive summary of the clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. Arch Intern Med 1998; 158: 1855–1867.
Douketis JD, Feightner JW, Attia J, Feldman WF, with the Canadian Task Force on Preventive Health Care. Periodic Health Examination, 1999 update: detection, prevention, and treatment of obesity. Can Med Assoc J 1999; 160: 513–524.
Oster G, Thompson D, Edelsberg J, Bird AP, Colditz GA . Lifetime effect and economic benefits of weight loss among obese persons. Am J Public Health 1999; 89: 1536–1542.
Blackburn G . Effect of degree of weight loss on health benefits. Obes Res 1995; 3 (Suppl 2): 211S–216S.
Hypertension Prevention Trial Research Group. The hypertension prevention trial: three year effects of dietary changes on blood pressure. Arch Intern Med 1990; 150: 153–162.
Goldstein DJ . Beneficial effects of modest weight loss. Int J Obes Relat Metab Disord 1992; 16: 397–415.
Dattilo AM, Kris-Etherton PM . Effects of weight reduction on blood lipids and lipoproteins: a meta-analysis. Am J Clin Nutr 1992; 56: 320–328.
Wing R, Jeffery RW . Effect of modest weight loss on changes in cardiovascular risk factors: are there differences between men and women or between weight loss and maintenance? Int J Obes Relat Metab Disord 1995; 19: 67–73.
Williamson DF, Thompson TJ, Thun M, Flanders D, Pamuk E, Byers T . Intentional weight loss and mortality among overweight individuals with diabetes. Diabetes Care 2000; 23: 1499–1504.
Anderson JW, Konz EC . Obesity and disease management: effects of weight loss on comorbid conditions. Obes Res 2001; 9 (Suppl 4): 326S–334S.
Singh RB, Rastogi SS, Verma R, Laxmi B, Singh R, Ghosh S, Niaz MA . Randomized controlled trial of cardioprotective diet in patients with recent acute myocardial infarction: results of one year follow-up. BMJ 1992; 304: 1015–1019.
Glazer G . Long-term pharmacotherapy of obesity 2000. A review of efficacy and safety. Arch Intern Med 2001; 161: 1814–1824.
Moher D, Fortin P, Jadad AR, Juni P, Klassen T, Le Lorier J, Liberati A, Linde K, Penna A . Completeness of reporting of trials published in languages other than English: implications for conduct and reporting of systematic reviews. Lancet 1996; 347: 907–908.
McManus RJ, Wilson S, Delaney BC, Fitzmaurice DA, Hyde CJ, Tobias RS, Jowett S, Hobb FD . Review of the usefulness of contacting other experts when conducting a literature search for systematic reviews. BMJ 1998; 317: 1562–1563.
Moher D, Cook DJ, Eastwood S, Oklin I, Rennie D, Stroup DF, for the QUORUM Group. Lancet 1999; 354: 1896–1900.
Wathen N, Walton R, Fear J . Process manual for producing and disseminating CTF reviews. Canadian Task Force on Preventive Health Care; May 2002.
The Direct Thrombin Inhibitor Trialists' Collaborative Group. Direct thrombin inhibitors in acute coronary syndromes: principal results of a meta-analysis based on individual patient data. Lancet 2002; 359: 294–302.
Scheen AJ, Lefebre PJ . Pharmacological treatment of obesity: present status. Int J Obes Relat Metab Disord 1999; 23 (Suppl 1): 47–53.
Khan LK, Serdula MK, Bowman BA, Williamson DF . Use of prescription weight loss pills among U.S. adults in 1996–1998. Ann Intern Med 2001; 134: 282–286.
Fleiss JL . Statistical methods for rates and proportions. John Wiley & Sons: New York; 1973. pp 43–47.
Pedersen T, Olsson A, Faergeman O, Kjekshus J, Wedel H, Berg K, Wilhelmsen L, Haghfelt T, Thorgeirsson G, Pyorala K, Miettinen T, Christophersen B, Tobert JA, Musliner TA, Cook TJ . Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandanavian Simvastatin Survival Study (4S). Circulation 1998; 97: 1453–1460.
Collins R, MacMahon S . Blood pressure, antihypertensive drug treatment on vascular disease: reappraisal of the evidence in 1994. J Vasc Med Biol 1994; 50: 272–298.
Coutinho M, Gerstein HC, Wang Y, Yusuf S . The relationship between glucose and incident cardiovascular events. A metaregression analysis of published data from 20 studies of 95 783 individuals followed for 12.4 years. Diabetes Care 1999; 22: 1385–1387.
DerSimonian R, Laird NM . Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188.
Adams SO, Grady KE, Lund AK, Mukaida C, Wolk CH . Weight loss: long-term results in an ambulatory setting. J Am Diet Assoc 1983; 83: 306–310.
Kramer FM, Jeffrey RW, Forster JL, Snell MK . Long-term follow-up of behavioral treatment for obesity: patterns of weight regain among men and women. Int J Obes Relat Metab Disord 1989; 13: 123–136.
Anderson JW, Hamilton CC, Crown-Weber E, Riddlemoser M, Gustafson NJ . Safety and effectiveness of a multidisciplinary very-low calorie diet program for selected obese individuals. J Am Diet Assoc 1991; 91: 1582–1584.
Fitzwater SL, Weinsier RL, Wooldridge NH, Birch R, Liu C, Bartolucci AA . Evaluation of long-term weight changes after a multidisciplinary weight control program. J Am Diet Assoc 1991; 91: 421–426.
Eriksson KF, Lindgärde F . Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. Diabetologia 1991; 34: 891–898.
Elmer PJ, Grimm R, Laing B, Grandits G, Svendsen K, Van Heel N, Betz E, Raines J, Link M, Stamler J . Lifestyle intervention: results of the Treatment of Mild Hypertension Study (TOMHS). Prev Med 1995; 24: 378–388.
Skender ML, Goodrick GK, Del Junco D, Reeves RS, Darnell L, Gotto AM, Foreyt JP . Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc 1996; 96: 342–346.
Torgerson JS, Lissner L, Lindroos AK, Kruijer H, Sjöstrom L . VLCD plus dietary and behavioural support versus support alone in the treatment of severe obesity. A randomised two-year clinical trial. Intl J Obes Relat Metab Disord 1997; 21: 987–994.
The Trials of Hypertension Prevention Collaborative Research Group. Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. Arch Intern Med 1997; 157: 657–667.
Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, Milas NC, Mattfeldt-Berman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, Cohen J . Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, Phase II. Ann Intern Med 2001; 134: 1–11.
Jones DW, Miller ME, Wofford MR, Anderson Jr DC, Cameron ME, Wiloughby DL, Adair CT, King NS . The effect of weight loss intervention on antihypertensive medication requirements in the Hypertension Optimal Treatment (HOT) Study. Am J Hypertens 1999; 12: 1175–1180.
Ditschuneit HH, Flechtner-Mors M, Johnson TD, Adler G . Metabolic and weight-loss effects of a long-term dietary intervention in obese patients. Am J Clin Nutr 1999; 69: 198–204.
Flechtner-Mors M, Ditscchuneit HH, Johnson TD, Suchard MA, Adler G . Metabolic and weight loss effects of long-term dietary intervention in obese patients: four-year results. Obes Res 2000; 8: 399–402.
Tuomilehto J, Lindström J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M . Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Stamler R, Stamler J, Grimm R, Gosch FC, Elmer P, Dyer A, Berman R, Fishman J, Van Heel N, Civinelli J, McDonald A . Nutritional therapy for high blood pressure. Final report of a four-year randomized controlled trial—The Hypertension Control Program. JAMA 1987; 257: 1484–1491.
King AC, Frey-Hewitt B, Dreon DM, Wood PD . Diet vs exercise in weight maintenance. The effects of minimal intervention strategies on long-term outcome in men. Arch Intern Med 1989; 149: 2741–2746.
Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W . Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care 1998; 21: 350–359.
Hollander PA, Elbein SC, Hirsch IB, Kelley D, McGill J, Taylor T, Weiss SR, Crockett SE, Kaplan RA, Comstock J, Lucas CP, Lodewick PA, Canovatchel W, Chung J, Hauptman J . Role of orlistat in the treatment of obese patients with type 2 diabetes. Diabetes Care 1998; 21: 1288–1294.
Sjöström L, Rissanen A, Andersen T, Boldrin M, Golay A, Koppeschaar HP, Krempf M . Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. Lancet 1998; 352: 167–173.
Davidson MH, Hauptman J, DiGirolamo M, Foreyt JP, Halsted CH, Heber D, Heimburger DC, Lucas CP, Robbins DC, Chung J, Heymsfield SB . Weight controlled and risk factor reduction in obese subjects treated for 2 years with orlistat. A randomized controlled trial. JAMA 1999; 281: 235–242.
Lindgärde F, on behalf of the Orlistat Swedish Multimorbidity Study Group. The effect of orlistat on body weight and coronary heart disease risk profile in obese patients: The Swedish Multimorbidity Study. J Intern Med 2000; 248: 245–254.
Finer N, James WPT, Kopelman PG, Lean MEJ, Williams G . One-year treatment of obesity: a randomized, double-blind, placebo-controlled, multicentre study of orlistat, a gastrointestinal lipase inhibitor. Intl J Obes Relat Metab Disord 2000; 24: 306–313.
Rössner S, Sjöström L, Noack R, Meinders AE, Noseda G, on behalf of the European Orlistat Obesity Study Group. Weight loss, weight maintenance, and improved cardiovascular risk factors after 2 years treatment with orlistat for obesity. Obes Res 2000; 8: 49–61.
Hauptman J, Lucas C, Boldrin MN, Collins H, for the Orlistat Primary Care Study Group, Segal KR . Orlistat in the long-term treatment of obesity in primary care settings. Arch Fam Med 2000; 9: 160–167.
Kelley DE, Bray GA, Pi-Sunyer FX, Klein S, Hill J, Miles J, Hollander P . Clinical efficacy of orlistat therapy in overweight and obese patients with insulin-treated type 2 diabetes. Diabetes Care 2002; 25: 1033–1041.
Miles JM, Leiter L, Hollander P, Wadden T, Anderson JW, Doyle M, Foreyt J, Aronne L, Klein S . Effect of orlistat in overweight and obese patients with type 2 diabetes treated with metformin. Diabetes Care 2002; 25: 1123–1128.
Broom I, Wilding J, Stott P, Myers N . Randomised trial of the effects of orlistat on body weight and cardiovascular disease risk profile in obese patients: UK multimorbidity study. Int J Clin Pract 2002; 56: 494–499.
Bakris G, Calhoun D, Hellman C, Dolker, Kingma I, on behalf of the orlistat and resistant hypertension investigators. Orlistat improves blood pressure control in obese subjects with treated but inadequately controlled hypertension. J Hypertens 2002; 20: 2257–2267.
Hanefeld M, Sache G . The effects of orlistat on body weight and glycaemic control in overweight patients with type 2 diabetes: a randomized placebo-controlled trial. Diabetes Obes Metabol 2002; 4: 415–423.
James WPT, Astrup A, Finer N, Hilsted J, Kopelman P, Rossner S, Saris WH, Van Gaal LF . Effect of sibutramine on weight maintenance after weight loss: a randomised trial. Lancet 2000; 356: 2119–2125.
McMahon FG, Fujioka K, Singh BN, Mendel CM, Rowe E, Rolston K, Johnson F, Mooradian AD . Efficacy and safety of sibutramine in obese white and African American patients with hypertension. A 1-year, double-blind, placebo-controlled, multicenter trial. Arch Intern Med 2000; 160: 2185–2191.
Smith IG, on behalf of the members of the Sibutramine Clinical Study 1047 Team, Goulder MA . Randomized placebo-controlled trial of long-term treatment with sibutramine in mild to moderate obesity. J Fam Pract 2001; 50: 505–512.
McMahon FG, Weinstein SP, Rowe E, Ernst KR, Johnson F, Fujioka K, the Sibutramine in Hypertension Clinical Study Group. Sibutramine is safe and effective for weight loss in obese patients whose hypertension is well controlled with angiotensin-converting enzyme inhibitors. J Hum Hypertens 2002; 16: 5–11.
McNulty SJ, Ur E, Williams G, for the Multicenter Siburtamine Study Group. A randomized trial of sibutramine in the management of obese type 2 diabetic patients treated with metformin. Diabetes Care 2003; 26: 125–131.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Charles MA, Morange P, Eschwège E, Andre P, Vague P, Juhan-Vague I . Effect of weight change and metformin on fibrinolysis and the von Willebrand factor in obese nondiabetic subjects. The BIGPRO1 Study. Diabetes Care 1998; 21: 1967–1972.
Lechner GW, Elliot DW . Comparison of weight loss after gastric exclusion and partitioning. Arch Surg 1983; 118: 685–692.
Capella JF, Capella RF . The weight reduction operation of choice: vertical banded gastroplasty or gastric bypass? Am J Surg 1996; 171: 74–79.
Sapala JA, Wood MH, Sapala MA, Flake Jr TM . Marginal ulcer after gastric bypass: a prospective 3-year study of 173 patients. Obes Surg 1998; 8: 505–516.
Sjöstrom CD, Lissner L, Wedel H, Sjöström L . Reduction in incidence of diabetes, hypertension and lipid disturbances after intentional weight loss induced by bariatric surgery: the SOS Intervention Study. Obes Res 1999; 7: 477–484.
Torgerson JS, Sjöström L . The Swedish Obese Subjects (SOS) Study—rationale and results. Int J Obes Relat Metab Disord 2001; 25 (Suppl 1): S2–S4.
Sjöström CD, Peltonen M, Wedel H, Sjöström L . Differential long-term effects of intentional weight loss on diabetes and hypertension. Hypertension 2000; 36: 20–25.
Løvig T, Haffner JFW, Kaaresen R, Nygaard K, Stadaas JO . Gastric banding for morbid obesity: five years follow-up. Int J Obes Relat Metab Disord 1993; 17: 453–457.
Sugerman HJ, Londrey GL, Kellum JM, Wolf L, Liszka T, Engle KM, Birkenhauer R, Starkey JV . Weight loss with vertical banded gastroplasty and Roux-Y gastric bypass for morbid obesity with selective versus random assignment. Am J Surg 1989; 157: 93–102.
Hall JC, Watts JM, O'Brien PE, Dunstan RE, Walsh JF, Slavotinek AH, Elmslie RG . Gastric surgery for morbid obesity. The Adelaide Study. Ann Surg 1990; 4: 419–427.
Brolin RE, Bradley LJ, Wilson AC, Cody RP . Lipid risk profile and weight stability after gastric restrictive operations for morbid obesity. J Gastrointest Surg 2000; 4: 464–469.
Pontiroli AE, Pizzocri P, Librenti MC, Vedani P, Marchi M, Cucchi E, Orena C, Paganelli M, Giacomelli M, Ferla G, Folli F . Laparoscopic adjustable banding for the treatment of morbid (grade 3) obesity and its metabolic complications: a three-year study. J Clin Endocrinol Metab 2002; 87: 3361–3555.
Fanghanel G, Cortinas L, Sanchez-Reyes L, Berber A . Second phase of a double-blind study clinical trial on sibutramine for the treatment of patients suffering essential obesity: 6 months after treatment cross-over. Int J Obes Relat Metab Disord 2001; 25: 741–747.
Williamson DF . Pharmacotherapy for obesity. JAMA 1999; 281: 278–280.
Balsiger BM, Murr MM, Poggio JL, Sarr MG . Bariatric surgery. Surgery for weight control in patients with morbid obesity. Med Clin N Am 2000; 84: 477–489.
Sugerman HJ . Bariatric surgery for severe obesity. J Assoc Acad Minor Phys 2001; 12: 129–136.
Azagara JS, Goergen M, Ansay J, De Simone P, Vanhaverbeek M, Devuyst L, Squelaert J . Laparoscopic gastric reduction surgery. Preliminary results of a randomized, prospective trial of laparoscopic vs open vertical banded gastroplasty. Surg Endosc 1999; 13: 555–558.
Westling A, Gustavsson S . Laparoscopic vs open Roux-en-Y gastric bypass: a prospective, randomized trial. Obes Surg 2001; 11: 284–292.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Health C . Prospective study of intentional weight loss and mortality in never-smoking overweight US white women aged 40–64 years. Am J Epidemiol 1995; 141: 1128–1141.
Williamson DF, Pamuk E, Thun M, Flanders D, Byers T, Health C . Prospective study of intentional weight loss and mortality in overweight white men aged 40–64 years. Am J Epidemiol 1999; 149: 491–503.
Denke MA . Cholesterol-lowering diets. A review of the evidence. Arch Intern Med 1995; 155: 17–26.
Knopp RH, Walden CE, Retzlaff BM, McCann BS, Dowdy AA, Albers JJ, Gey GO, Cooper MN . Long-term cholesterol-lowering effects of 4 fat-restricted diets in hypercholesterolemic and combined hyperlipidemic men. The Dietary Alternatives Study. JAMA 1997; 278: 1509–1515.
Blood Pressure Lowering Trialists' Collaboration. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Lancet 2000; 355: 1955–1964.
Anonymous. Intensive blood-glucose control with sulfonylureas or insulin compared with conventional treatment and risk of cardiovascular complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 1998; 352: 837–853.
ACP Journal Club: purpose and procedures. Available at http://www.acpjc.org/shared/purpose and procedure.htm Accessed December 2003.
Yanovski SZ, Yanovski JA . Obesity. N Engl J Med 2002; 346: 591–602.
National Task Force on the Prevention and Treatment of Obesity. Very-low calorie diets. JAMA 1993; 270: 967–974.
Goldstein DJ, Potvin JH . Long-term weight loss: the effect of pharmacologic agents. Am J Clin Nutr 1994; 60: 647–657.
Monteforte MJ, Turkelson CM . Bariatric surgery for morbid obesity. Obes Surg 2000; 10: 391–401.
Astrup, Grunwald GK, Melanson EL, Saris WHM, Hill JO . The role of low-fat diets in body weight control: a meta-analysis of ad libitum dietary intervention studies. Int J Obes Relat Metab Disord 2000; 24: 1545–1552.
Mulrow CD, Chiquette E, Angel L, Cornell J, Summerbell C, Anagnostelis B, Grimm Jr R, Brand MB . Dieting to reduce body weight for controlling hypertension in adults. The Cochrane Library Issue 1 2002.
Miller WC, Koceja DM, Hamilton EJ . A meta-analysis of the past 25 years of weight loss research using diet, exercise or diet plus exercise intervention. Int J Obes Relat Metab Disord 1997; 21: 941–947.
Zavoral JH . Treatment with orlistat reduces cardiovascular risk in obese patients. J Hypertens 1998; 16: 2013–2017.
Garrow JS, Summerbell CD . Meta-analysis: effect of exercise, with or without dieting, on the body composition of overweight subjects. Eur J Clin Nutr 1995; 49: 1–10.
Ebrahim S, Smith GD . Lowering blood pressure: a systematic review of sustained effects of non-pharmacological interventions. J Public Health Med 1998; 20: 441–448.
Arteburn D, Noel PH . Effects of drug treatment for obesity in adults. Clin Evid 2001; 412–419.
Anderson JW, Konz EC, Frederich RC, Wood CL . Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 2001; 74: 579–584.
Clegg A, Colquitt J, Sidhu M, Walker A . Clinical and cost effectiveness of surgery for morbid obesity: a systematic review and economic evaluation. Int J Obes Relat Metab Disord 2003; 27: 1167–1177.
Padwal R, Li SK, Lau DCW . Long-term pharmacotherapy for overweight and obesity: a systematic review and meta-analysis of randomized controlled trials. Int J Obes Relat Metab Disord 2003; 12: 1437–1446.
Fogelholm M, Kukkonen-Harjula K . Does physical activity prevent weight gain —a systematic review. Obes Rev 2000; 1: 95–111.
Poirier P, Despres JP . Exercise in weight management of obesity. Cardiol Clin 2001; 19: 459–470.
Acknowledgements
We thank Drs Arya Sharma, Hertzel Gerstein, and Anna Sawka for their helpful reviews of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Appendix A1 Criteria for grading the internal validity of individual studies
Appendix A1 Criteria for grading the internal validity of individual studies
(Adapted from the Process Manual for Producing and Disseminating CTF Reviews, Canadian Task Force on Preventive Health Care (May 2002 draft), and from the United States Preventive Services Task Force Methods Manual (August 2000 draft).
Design-specific criteria and quality category definitions
Presented below are a set of minimal criteria for each study design and then a general definition of three categories: ‘good’, ‘fair’, and ‘poor’ based on those criteria. These specifications are not meant to be rigid rules, but rather are intended to be general guidelines, and individual exceptions, when explicitly explained and justified, can be made. In general,
-
a ‘good’ study is one that meets all criteria well
-
a ‘fair’ study is one that does not meet (or it is not clear that it meets) at least one criterion but has no known ‘fatal flaw’
Randomized controlled trials and cohort studies
Criteria:
-
Initial assembly of comparable groups.For randomized controlled trials (RCTs): adequate randomization, including first concealment and whether potential confounders were distributed equally among groups
-
For cohort studies: consideration of potential confounders with either restriction or measurement for adjustment in the analysis; consideration of inception cohorts
-
Maintenance of comparable groups (includes attrition, crossovers, adherence, contamination)
-
Important differential loss to follow-up or overall high loss to follow-up
-
Measurements: equal, reliable, and valid (includes masking of outcome assessment)
-
Clear definition of interventions
-
All important outcomes considered
-
Analysis: adjustment for potential confounders for cohort studies, or intention to treat analysis for RCTs.
Definition of ratings based on above criteria
Good: Meets all criteria. Comparable groups are assembled initially and maintained throughout the study (follow-up at least 80%); reliable and valid measurement instruments are used and applied equally to the groups; interventions are spelled out clearly; all important outcomes are considered; and appropriate attention to confounders in analysis. In addition, for RCTs, intention to treat analysis is used.
Fair: Studies will be graded ‘fair’ if any or all of the following problems occur, without the fatal flaws noted in the ‘poor’ category below: generally, comparable groups are assembled initially but question remains whether some (although not major) differences occurred with follow-up; measurement instruments are acceptable (although not the best) and generally applied equally; some but not all important outcomes are considered; and some but not all potential confounders are accounted for. Intention to treat analysis is carried out for RCTs.
Poor: Studies will be graded ‘poor’ if any of the following fatal flaws exists: groups assembled initially are not close to being comparable or maintained throughout the study; unreliable or invalid measurement instruments are used or not applied at all equally among groups (including not masking outcome assessment); and key confounders are given little or no attention. For RCTs, intention to treat analysis is lacking.
Rights and permissions
About this article
Cite this article
Douketis, J., Macie, C., Thabane, L. et al. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J Obes 29, 1153–1167 (2005). https://doi.org/10.1038/sj.ijo.0802982
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802982
Keywords
This article is cited by
-
Proprietary alpha-amylase inhibitor formulation from white kidney bean (Phaseolus vulgaris L.) promotes weight and fat loss: a 12-week, double-blind, placebo-controlled, randomized trial
Scientific Reports (2024)
-
Association between long-term weight loss and obesity-related complications defined by Edmonton obesity staging system: analysis from the NHANES (2011–2018)
European Journal of Clinical Nutrition (2024)
-
Bilateral Subdiaphragmatic Vagal Nerve Stimulation Using a Novel Waveform Decreases Body Weight, Food Consumption, Adiposity, and Activity in Obesity-Prone Rats
Obesity Surgery (2024)
-
Weight Regain After Bariatric Surgery: Scope of the Problem, Causes, Prevention, and Treatment
Current Diabetes Reports (2023)
-
The inverted U-shaped relationship between weight loss percentage and cardiovascular health scores
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2023)