Abstract
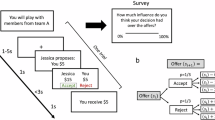
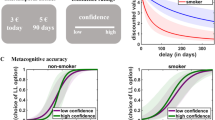
Beliefs have a powerful influence on our behavior, yet their neural mechanisms remain elusive. Here we investigate whether beliefs could impact brain activities in a way akin to pharmacological dose-dependent effects. Nicotine-dependent humans were told that nicotine strength in an electronic cigarette was either ‘low’, ‘medium’ or ‘high’, while nicotine content was held constant. After vaping, participants underwent functional neuroimaging and performed a decision-making task known to engage neural circuits affected by nicotine. Beliefs about nicotine strength induced dose-dependent responses in the thalamus, a key binding site for nicotine, but not in other brain regions such as the striatum. Nicotine-related beliefs also parametrically modulated the connectivity between the thalamus and ventromedial prefrontal cortex, a region important for decision-making. These findings reveal a high level of precision in the way beliefs influence the brain, offering mechanistic insights into humans’ heterogeneous responses to drugs and a pivotal role of beliefs in addiction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$79.00 per year
only $6.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data supporting the findings of this study are deposited at https://osf.io/3hq6s/.
Code availability
The scripts used for data acquisition and analysis are available at https://osf.io/3hq6s/. Analyses were conducted using open software and toolboxes available online as described in Methods (SPM: www.fil.ion.ucl.ac.uk/spm/software/spm12; R Studio: https://www.rstudio.com/products/rstudio/download/#download; Lead-DBS: https://www.lead-dbs.org/download/; MRIcroGL: https://www.nitrc.org/projects/mricrogl/).
References
Posner, M. I., Petersen, S. E., Fox, P. T. & Raichle, M. E. Localization of cognitive operations in the human brain. Science 240, 1627–1631 (1988).
Gu, X., FitzGerald, T. H. B. & Friston, K. J. Modeling subjective belief states in computational psychiatry: interoceptive inference as a candidate framework. Psychopharmacology (Berl.) 236, 2405–2412 (2019).
Goldstein, R. Z. et al. The neurocircuitry of impaired insight in drug addiction. Trends Cogn. Sci. 13, 372–380 (2009).
Volkow, N. D. & Baler, R. Beliefs modulate the effects of drugs on the human brain. Proc. Natl Acad. Sci. USA 112, 2301–2302 (2015).
Kirsch, I. Response expectancy as a determinant of experience and behavior. Am. Psychol. 40, 1189–1202 (1985).
Tallarida, R. J. Drug Synergism and Dose–Effect Data Analysis (CRC Press, 2000).
Abdel-Rahman, S. M. & Kauffman, R. E. The integration of pharmacokinetics and pharmacodynamics: understanding dose-response. Annu. Rev. Pharmacol. Toxicol. 44, 111–136 (2004).
Davis, J. M. & Chen, N. Dose response and dose equivalence of antipsychotics. J. Clin. Psychopharmacol. 24, 192–208 (2004).
Benowitz, N. L., Jacob, P. & Herrera, B. Nicotine intake and dose response when smoking reduced-nicotine content cigarettes. Clin. Pharmacol. Ther. 80, 703–714 (2006).
Bisby, J. A., Leitz, J. R., Morgan, C. J. A. & Curran, H. V. Decreases in recollective experience following acute alcohol: a dose–response study. Psychopharmacology (Berl). 208, 67–74 (2010).
Curran, V. H., Brignell, C., Fletcher, S., Middleton, P. & Henry, J. Cognitive and subjective dose–response effects of acute oral Δ9-tetrahydrocannabinol (THC) in infrequent cannabis users. Psychopharmacology (Berl.) 164, 61–70 (2002).
Mayberg, H. S. et al. The functional neuroanatomy of the placebo effect. Am. J. Psychiatry 159, 728–737 (2002).
Wager, T. D. et al. Placebo-induced changes in fMRI in the anticipation and experience of pain. Science 303, 1162–1167 (2004).
Benedetti, F., Mayberg, H. S., Wager, T. D., Stohler, C. S. & Zubieta, J. K. Neurobiological mechanisms of the placebo effect. J. Neurosci. 25, 10390–10402 (2005).
Price, D. D., Finniss, D. G. & Benedetti, F. A comprehensive review of the placebo effect: recent advances and current thought. Annu. Rev. Psychol. 59, 565–590 (2008).
Zilcha-Mano, S., Brown, P. J., Roose, S. P., Cappetta, K. & Rutherford, B. R. Optimizing patient expectancy in the pharmacologic treatment of major depressive disorder. Psychol. Med. 49, 2414–2420 (2019).
Rutherford, B., Sneed, J., Devanand, D., Eisenstadt, R. & Roose, S. Antidepressant study design affects patient expectancy: a pilot study. Psychol. Med. 40, 781–788 (2010).
Gu, X. et al. Belief about nicotine selectively modulates value and reward prediction error signals in smokers. Proc. Natl Acad. Sci. USA 112, 2539–2544 (2015).
Gu, X. et al. Belief about nicotine modulates subjective craving and insula activity in deprived smokers. Front. Psychiatry 7, 126 (2016).
Russell, M. A. H. Nicotine intake and its regulation. J. Psychosom. Res. 24, 253–264 (1980).
Giovino, G. A., Henningfield, J. E., Tomar, S. L., Escobedo, L. G. & Slade, J. Epidemiology of tobacco use and dependence. Epidemiol. Rev. 17, 48–65 (1995).
Juliano, L. M., Fucito, L. M. & Harrell, P. T. The influence of nicotine dose and nicotine dose expectancy on the cognitive and subjective effects of cigarette smoking. Exp. Clin. Psychopharmacol. 19, 105–115 (2011).
Kelemen, W. L. & Kaighobadi, F. Expectancy and pharmacology influence the subjective effects of nicotine in a balanced-placebo design. Exp. Clin. Psychopharmacol. 15, 93–101 (2007).
Watkins, S. S., Koob, G. F. & Markou, A. Neural mechanisms underlying nicotine addiction: acute positive reinforcement and withdrawal. Nicotine Tob. Res. 2, 19–37 (2000).
Huang, A. S., Mitchell, J. A., Haber, S. N., Alia-Klein, N. & Goldstein, R. Z. The thalamus in drug addiction: from rodents to humans. Philos. Trans. R. Soc. 373, 20170028 (2018).
Haber, S. N. & Knutson, B. The reward circuit: linking primate anatomy and human imaging. Neuropsychopharmacol. Rep. 35, 4–26 (2010).
Shohamy, D. Learning and motivation in the human striatum. Curr. Opin. Neurobiol. 21, 408–414 (2011).
Shine, J. M., Lewis, L. D., Garrett, D. D. & Hwang, K. The impact of the human thalamus on brain-wide information processing. Nat. Rev. Neurosci. https://doi.org/10.1038/s41583-023-00701-0 (2023).
Brody, A. L. et al. Cigarette smoking saturates brain alpha 4 beta 2 nicotinic acetylcholine receptors. Arch. Gen. Psychiatry 63, 907–915 (2006).
Mukhin, A. G. et al. Greater nicotinic acetylcholine receptor density in smokers than in nonsmokers: a PET study with 2-18F-FA-85380. J. Nucl. Med. 49, 1628–1635 (2008).
Gotti, C. et al. Nicotinic acetylcholine receptors in the mesolimbic pathway: primary role of ventral tegmental area α6β2* receptors in mediating systemic nicotine effects on dopamine release, locomotion, and reinforcement. J. Neurosci. 30, 5311–5325 (2010).
Brody, A. L. et al. Brain nicotinic acetylcholine receptor occupancy: effect of smoking a denicotinized cigarette. Int. J. Neuropsychopharmacol. https://doi.org/10.1017/S146114570800922X (2009).
Brody, A. L. et al. Effect of secondhand smoke on occupancy of nicotinic acetylcholine receptors in brain. Arch. Gen. Psychiatry 68, 953–960 (2011).
Spurden, D. P. et al. Nicotinic receptor distribution in the human thalamus: autoradiographical localization of [3H]nicotine and [125I]α-bungarotoxin binding. J. Chem. Neuroanat. 13, 105–113 (1997).
Rubboli, F. et al. Distribution of nicotinic receptors in the human hippocampus and thalamus. Eur. J. of Neurosci. 6, 1596–1604 (1994).
Paterson, D. & Nordberg, A. Neuronal nicotinic receptors in the human brain. Prog. Neurobiol. 61, 75–111 (2000).
Picard, F. et al. High density of nicotinic receptors in the cingulo-insular network. Neuroimage 79, 42–51 (2013).
Shepherd, G. M. G. & Yamawaki, N. Untangling the cortico-thalamo-cortical loop: cellular pieces of a knotty circuit puzzle. Nat. Rev. Neurosci. 22, 389–406 (2021).
Garibotto, V., Wissmeyer, M., Giavri, Z., Ratib, O. & Picard, F. Nicotinic acetylcholine receptor density in the ‘higher-order’ thalamus projecting to the prefrontal cortex in humans: a PET study. Mol. Imaging Biol. 22, 417–424 (2020).
de Kloet, S. F. et al. Bi-directional regulation of cognitive control by distinct prefrontal cortical output neurons to thalamus and striatum. Nat. Commun. 12, 1994 (2021).
Steward, T. et al. A thalamo-centric neural signature for restructuring negative self-beliefs. Mol. Psychiatry 27, 1611–1617 (2022).
Schuck, N. W., Cai, M. B., Wilson, R. C. & Niv, Y. Human orbitofrontal cortex represents a cognitive map of state space. Neuron. 91, 1402–1412 (2016).
Moneta, N., Garvert, M. M., Heekeren, H. R. & Schuck, N. W. Task state representations in vmPFC mediate relevant and irrelevant value signals and their behavioral influence. Nat. Commun. 14, 3156 (2023).
Petersen, G. O., Leite, C. E., Chatkin, J. M. & Thiesen, F. V. Cotinine as a biomarker of tobacco exposure: development of a HPLC method and comparison of matrices. J. Sep. Sci. 33, 516–521 (2010).
Duehlmeyer, L., Parsons, N., Malpas, C. B. & Hester, R. Functional connectivity during feedback learning in smokers. Addict. Biol. 27, e13109 (2022).
Lohrenz, T., McCabe, K., Camerer, C. F. & Montague, P. R. Neural signature of fictive learning signals in a sequential investment task. Proc. Natl Acad. Sci. USA 104, 9493–9498 (2007).
Chiu, P. H., Lohrenz, T. M. & Montague, P. R. Smokers’ brains compute, but ignore, a fictive error signal in a sequential investment task. Nat. Neurosci. 11, 514–520 (2008).
Maldjian, J. A., Laurienti, P. J., Kraft, R. A. & Burdette, J. H. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 19, 1233–1239 (2003).
Su, J. H. et al. Thalamus Optimized Multi Atlas Segmentation (THOMAS): fast, fully automated segmentation of thalamic nuclei from structural MRI. Neuroimage 194, 272–282 (2019).
Zander, T. O., Kothe, C., Jatzev, S. & Gaertner, M. in Brain–Computer Interfaces: Applying our Minds to Human–Computer Interaction (eds. Tan, D. S. & Nijholt, A.) 181–199 (Springer, 2010).
Mandelkow, H., De Zwart, J. A. & Duyn, J. H. Linear discriminant analysis achieves high classification accuracy for the BOLD fMRI response to naturalistic movie stimuli. Front. Hum. Neurosci. 10, 1–12 (2016).
Friston, K. J. et al. Psychophysiological and modulatory interactions in neuroimaging. Neuroimage 6, 218–229 (1997).
Rouault, M. & Fleming, S. M. Formation of global self-beliefs in the human brain. Proc. Natl Acad. Sci. USA 117, 27268–27276 (2020).
Rushworth, M. F. S. & Behrens, T. E. J. Choice, uncertainty and value in prefrontal and cingulate cortex. Nat. Neurosci. 11, 389–397 (2008).
Niv, Y. Learning task-state representations. Nat. Neurosci. 22, 1544–1553 (2019).
Adem, A. et al. Distribution of nicotinic receptors in human thalamus as visualized by 3H-nicotine and 3H-acetylcholine receptor autoradiography. J. Neural Transm. 73, 77–83 (1988).
Wong, D. F. et al. PET imaging of high-affinity a4b2 nicotinic acetylcholine receptors in humans with 18F-AZAN, a radioligand with optimal brain kinetics. J. Nucl. Med. 54, 1308–1314 (2013).
Lawrence, N. S., Ross, T. J. & Stein, E. A. Cognitive mechanisms of nicotine on visual attention. Neuron. 36, 539–548 (2002).
Stein, E. A. et al. Nicotine-induced limbic cortical activation in the human brain: a functional MRI study. Am. J. Psychiatry 155, 1009–1015 (1998).
Kumari, V. et al. Cognitive effects of nicotine in humans: an fMRI study. Neuroimage 19, 1002–1013 (2003).
Levy, D. J. & Glimcher, P. W. The root of all value: a neural common currency for choice. Curr. Opin. Neurobiol. 22, 1027–1038 (2012).
Barbalat, G., Bazargani, N. & Blakemore, S.-J. The influence of prior expectations on emotional face perception in adolescence. Cereb. Cortex 23, 1542–1551 (2012).
Perkins, K. A. et al. Effects of central and peripheral nicotinic blockade on human nicotine discrimination. Psychopharmacology (Berl.) 142, 158–164 (1999).
Perkins, K. A., Herb, T. & Karelitz, J. L. Discrimination of nicotine content in electronic cigarettes. Addict. Behav. 91, 106–111 (2019).
Franklin, T. R. et al. Limbic activation to cigarette smoking cues independent of nicotine withdrawal: a perfusion fMRI study. Neuropsychopharmacol. Rep. 32, 2301–2309 (2007).
Engelmann, J. M. et al. Neural substrates of smoking cue reactivity: a meta-analysis of fMRI studies. NeuroImage https://doi.org/10.1016/j.neuroimage.2011.12.024 (2012).
McClernon, F. J., Kozink, R. V. & Rose, J. E. Individual differences in nicotine dependence, withdrawal symptoms, and sex predict transient fMRI-BOLD responses to smoking cues. Neuropsychopharmacol. Rep. 33, 2148–2157 (2008).
Wilson, S. J., Sayette, M. A., Delgado, M. R. & Fiez, J. A. Instructed smoking expectancy modulates cue-elicited neural activity: a preliminary study. Nicotine Tob. Res. 7, 637–645 (2005).
McBride, D., Barrett, S. P., Kelly, J. T., Aw, A. & Dagher, A. Effects of expectancy and abstinence on the neural response to smoking cues in cigarette smokers: an fMRI study. Neuropsychopharmacol. Rep. 31, 2728–2738 (2006).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control 22, Suppl 1:i14–i17 (2013).
Nakamura, Y. et al. Investigating dose-dependent effects of placebo analgesia: a psychophysiological approach. Pain 153, 227–237 (2012).
Geuter, S., Eippert, F., Hindi Attar, C. & Büchel, C. Cortical and subcortical responses to high and low effective placebo treatments. Neuroimage 67, 227–236 (2013).
Cui, Y. et al. The impact of nicotine dose and instructed dose on smokers’ implicit attitudes to smoking cues: an ERP study. Psychol. Addict. Behav. 33, 710–720 (2019).
de Wit, H., Uhlenhuth, E. H. & Johanson, C. E. Individual differences in the reinforcing and subjective effects of amphetamine and diazepam. Drug Alcohol Depend. 16, 341–360 (1986).
Scott, D. J. et al. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron 55, 325–336 (2007).
SPM12 algorithms. Univeristy College London http://fil.ion.ucl.ac.uk/spm (2014).
Mazaika P. K., Whitfield-Gabrieli, S. Reiss, A. & Glover, G. Artifact repair for fMRI data from high motion clinical subjects. Hum. Brain Mapp. 47, 70238-1 (2007).
Woo, C.-W., Krishnan, A. & Wager, T. D. Cluster-extent based thresholding in fMRI analyses: pitfalls and recommendations. Neuroimage 91, 412–419 (2014).
Lieberman, M. D. & Cunningham, W. A. Type I and type II error concerns in fMRI research: re-balancing the scale. Soc. Cogn. Affect. Neurosci. 4, 423–428 (2009).
Acknowledgements
This work was supported by National Institute on Drug Abuse grant R01DA043695 (X.G.), National Institute on Drug Abuse grant R21DA049243 (X.G.) and University of Texas, Dallas internal funding (X.G.). The funders had no role in study design, data collection, data analysis or manuscript preparation. We thank staff members at the University of Texas Southwestern Imaging Center for their assistance with scanning, J. Jung and M. Labinski for their help with developing the fMRI task and J. Maclin for her help with participant recruitment. We also thank L. Berner for her advice on the statistical analysis, and D. Schiller and P. Kenny for their helpful discussions and comments on an earlier version of this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: X.G. Methodology: O.P, A.S., N.B., W.C.P. and X.G. Investigation: M.H., S.N. and A.K. Visualization: O.P. Funding acquisition: X.G. Project administration: M.H. and X.G. Supervision: X.G. Writing—original draft: O.P., W.C.P., V.G.F. and X.G. Writing—review and editing: O.P., V.G.F. and X.G.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Mental Health thanks Cynthia Conklin, Qinghua He and Nicholas Parsons for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary text, Figs. 1–9 and Tables 1 and 2.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Perl, O., Shuster, A., Heflin, M. et al. Nicotine-related beliefs induce dose-dependent responses in the human brain. Nat. Mental Health 2, 177–188 (2024). https://doi.org/10.1038/s44220-023-00188-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44220-023-00188-9