Abstract
Long noncoding RNAs (lncRNAs) play a significant role in the occurrence and development of malignant tumours. However, ceRNAs, which are significantly associated with the prognosis of breast cancer (BC), need to be further investigated. Therefore, the current study aimed to investigate the effect of the lncRNA DDX11-AS1 on BC progression. Bioinformatics analysis via a public microarray revealed that DDX11-AS1 was upregulated in BC. The above findings were verified via RT‒qPCR analysis of BC tissues. Additionally, our study revealed that the expression levels of DDX11-AS1 increased with increasing pathological grade and lymph node metastasis. Furthermore, DDX11-AS1 knockdown markedly inhibited the proliferation, migration and invasion abilities of BC cells. Mechanistically, DDX11-AS1 could prevent the degradation of MTDH in BC via competitively binding with miR-30c-5p, which could act as a tumour promoter factor. Additionally, miR-30c-5p was downregulated and MTDH was upregulated in BC cells and tissues. The promoting effect of DDX11-AS1 on BC cells was enhanced by miR-30c-5p silencing and reduced by treatment with MTDH inhibitors. Collectively, the above results suggest that the DDX11-AS1/miR-30c-5p/MTDH axis could be associated with the progression of BC and that DDX11-AS1 could be a potential biomarker and therapeutic target for BC.
Similar content being viewed by others
Introduction
In 2023, the incidence rate of breast cancer (BC) among women surpassed that of lung cancer, with BC becoming the most common malignancy among women worldwide. Breast cancer in women has high incidence and mortality rates and ranks second among female malignancies, second only to lung cancer1. Due to its high heterogeneity in terms of morphology and genetics, BC is characterized by enhanced metastatic potential, easy relapse and high drug resistance. Although treatment approaches continue to improve, recurrence and metastasis still occur and several patients may develop these conditions as the disease progresses2. Previous studies have shown that noncoding RNAs can act as ceRNAs to regulate the occurrence and progression of human breast cancer, potentially serving as novel therapeutic targets3,4.
Long noncoding RNAs (lncRNAs), which have no protein coding potential, are RNAs that are > 200 nucleotides in length5. LncRNAs are involved in various biological processes, such as mRNA degradation, gene imprinting, splicing regulation, chromatin remodelling and cell cycle regulation6, particularly in cancer7. The competing endogenous RNA (ceRNA) hypothesis suggests that lncRNAs, which act as endogenous RNAs, can competitively promote mRNA expression by binding to particular microRNAs (miRs)8. This is also known as the miRNA sponge effect9,10. A previous study indicated that ceRNAs may be involved in the initiation and development of BC11,12. However, ceRNAs, which are significantly associated with the prognosis of BC, need to be further investigated. The lncRNA DDX11-AS1, also known as cohesion regulator noncoding RNA, is involved in several types of cancer, including hepatocarcinoma, lung cancer, colorectal carcinoma, renal carcinoma and bladder cancer13,14,15, and it functions primarily as a ceRNA to regulate gene expression. Another study revealed that DDX11-AS1 was associated with the resistance of BC cells to chemotherapy16,17. Nevertheless, the detailed molecular mechanism underlying the function of DDX11-AS1 as a ceRNA in BC oncogenesis remains unknown. MiR-30c-5p has been found to be abnormally expressed as a ceRNA in gastric cancer, bladder cancer, and other malignancies18,19. Additionally, some studies have reported aberrant miR-30c-5p expression in breast cancer20,21. Therefore, our research focused on DDX11-AS1 as a ceRNA sponge that adsorbs miR-30c-5p to promote breast cancer progression.
Metadherin (MTDH) is also known as astrocyte elevated gene-1 (AEG-1) and is lysine rich. MTDH is highly expressed in numerous cancer types and plays a pivotal role in promoting tumour proliferation, migration, and invasion, as well as enhancing cell survival; facilitating escape from apoptosis, angiogenesis, and metastasis; and conferring resistance to chemotherapy22,23,24,25,26. Previous clinical studies have shown that elevated expression of MTDH is associated with poorer prognosis in BC patients, and cellular assays have revealed that MTDH can promote BC progression and paclitaxel resistance through activation of the NF-κB pathway27,28. Our research revealed that MTDH can act as a target gene of miR-30c-5p in BC.
In this study, the expression levels of DDX11-AS1 in BC were analysed via a public microarray. Furthermore, the effects of DDX11-AS1, which acts as a ceRNA through the miR-30c-5p/metadherin (MTDH)axis, on BC carcinogenesis were also investigated. In our study, we found that the overexpression of MTDH could activate the NF-κB pathway by increasing p65 phosphorylation (p-p65) and causing the nuclear translocation of p65. The results of this study emphasize that DDX11-AS1, as a potential ceRNA, could become a new therapeutic target for BC.
Materials and methods
Patients and specimens. BC tissues (n = 36) and matched adjacent normal breast tissues (> 5 cm away from the tumour location) were obtained from 36 patients who underwent surgery at The Fourth Hospital of Hebei Medical University (Shijiazhuang, China) between September and December 2022. None of the recruited participants had accepted any therapy prior to surgery. Informed consent was obtained from all patients. The tissue samples harvested in the present study were stored at -80 ˚C in a refrigerator. The study was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University. The clinicopathological characteristics of the patients are listed in Table 1.
Bioinformatics analysis. The Gene Expression Omnibus (GEO) datasets, GSE156229 and GSE45666 (http://www.ncbi.nlm.nih.gov/geo/), and The Cancer Genome Atlas (TCGA; http://cancergenome.nih.gov/) database were used to analyse the differential expression of lncRNAs or miRNAs between BC and normal matched tissues.
RNA extraction and reverse transcription‒quantitative PCR (RT‒qPCR). A TRIzol® reagent (Takara Bio, Inc.) was used to extract total RNA from cells and tissues, according to the manufacturer’s instructions. The RNA quality and concentration were measured via the A260/A280 ratio on a microplate reader (Thermo Fisher Scientific, Inc.). A total of 2 µg of RNA was reverse-transcribed into complementary DNA via the Transcriptor First Strand cDNA Synthesis Kit (Tiangen Biotech Co., Ltd.) under the following thermocycling conditions: 42 °C for 15 min and 95 °C for 3 min. qPCR was performed with the GoTaq® Real-Time PCR System (Applied Biosystems; Thermo Fisher Scientific, Inc.). The relative expression levels were measured via the 2−ΔΔCqmethod29. Human GAPDH and U6 served as internal reference genes to calculate the relative expression of lncRNAs and miRNAs, respectively. The sequences of primers used are listed in Table S2.
Subcellular fractionation. To determine the cellular localization of the lncRNA DDX11-AS1, RNA from cytoplasmic and nuclear fractions was isolated and purified via a the Cytoplasmic and Nuclear RNA Purification Kit (Norgen Biotek Corp.), according to the manufacturer’s instructions. RT was performed using the extracted RNAs and the expression levels of the lncRNA DDX11-AS1 were detected via RT‒qPCR. U6 and GAPDH were used as nuclear and cytoplasmic control genes, respectively.
Cell culture. The human breast epithelial MCF10A cell line and the BC cell lines, BT549(ER:-, PR:-, HER2:-), MCF-7(ER:+, PR:+, HER2:-), MDA-MB-453(ER:-, PR:-, HER2:-), MDA-MB-231(ER:-, PR:-, HER2:-), and SK-BR3(ER:-, PR:-, HER2:+) were originally purchased from Procell Life Science & Technology Co., Ltd. MCF-7 and MDA-MB-231 cells were cultured in RPMI-1640 medium (Invitrogen; Thermo Fisher Scientific, Inc.), while BT549 and MDA-MB-453 cells were cultured in DMEM (Invitrogen; Thermo Fisher Scientific, Inc.). Both media were supplemented with 10% foetal bovine serum (FBS; Biological Industries Israel Beit-Haemek Ltd.) and antibiotics (Beijing Solarbio Science & Technology Co., Ltd.). The SK-BR3 cell line was maintained in McCoy’s 5 A medium containing 10% FBS (both from Procell Life Science & Technology Co., Ltd.), whereas the MCF10A cells were cultured in a special medium (Procell Life Science & Technology Co., Ltd.). All the cell lines were cultured at 37˚ C in an incubator with 5% CO2.
Cell transfection. The small interfering RNA targeting DDX11-AS (si-DDX11-AS) and the pcDNA-DDX11-AS1 overexpression plasmid were purchased from Shanghai Jikai Gene Chemical Technology Co., Ltd. The corresponding empty pcDNA vector and siRNA were used as negative controls (NCs). The miR-30c-5p inhibitor, miR-NC inhibitor, miR-30c-5p mimics, miR-NC mimics and the MTDH overexpression and knockdown plasmids and their corresponding NCs were also synthesized by Shanghai Jikai Gene Chemical Technology Co., Ltd. The indicated sequences are listed in Table S1. MDA-MB-231 or SK-BR3 cells were transfected with the above plasmids via the FuGENE® HD Transfection Reagent (Promega Corporation), according to the manufacturer’s protocol. The transfection efficiency was measured by RT‒qPCR. Following transfection for 48–72 h, subsequent experiments were carried out.
Cell Counting Kit 8 (CCK-8) assay. BC cells were seeded into 96-well plates at a density of ~ 2 × 103 cells/well and transfected for 24 h. Each group of cells was set up with six compound pores and tested. Cell proliferation was assessed via a CCK-8 assay according to the manufacturer’s instructions. Briefly, the following experimental steps were repeated at 0, 24, 48, 72 and 96 h. Each well was supplemented with 10 µl of CCK-8 reagent (Wuhan Boster Biological Technology, Ltd.) and the plates were then incubated for 2 h in a humidified incubator with 5% CO2 at 37 °C. The absorbance at a wavelength of 450 nm was measured in each well using the Tecan Infinite F50 microplate reader (Tecan Group, Ltd.).
Colony formation assay. Transfected cells (2 × 103 cells/well) were inoculated into 6-well plates and incubated with 10% FBS for 14 days. Then, the colonies were fixed with 4% paraformaldehyde for 15 min and stained with crystal violet dye (Beijing Solarbio Science & Technology Co., Ltd.) for 30 min. Colonies consisting of ≥ 50 cells were counted and analysed via ImageJ software (NIH).
Transwell invasion and migration assays. A Transwell chamber (pore size: 8 μm; Corning; Corning, Inc.) was coated with 20 µl of Matrigel (1 mg/ml; Beijing Solarbio Science & Technology Co., Ltd.) according to the manufacturer’s instructions. For the migration (without Matrigel) and invasion (with Matrigel; Millipore Sigma) assays, 4 × 104 BC cells were seeded into the upper chamber of the Transwell insert in 200 µl of FBS-free medium. The lower chamber was supplemented with 600 µl of 10% FBS medium as a chemoattractant. Following incubation at 37 °C for the indicated time points, noninvading cells were removed via a cotton swab. The cells adhering to the bottom surface of the membrane were fixed with 4% paraformaldehyde for 20 min and stained with crystal violet for 20 min. The stained cells were counted via ImageJ software (NIH).Five representative areas were counted per transwell, and the mean cell number per field of view was calculated for each transwell.
Wound healing assay. Transfected cells were cultured in 6-well plates until they reached 100% confluence. The cell monolayer was subsequently scraped linearly via a 10-µl pipette tip prior to rinsing away any isolated cells with PBS. The remaining cells were subsequently cultured in FBS-free medium after which artificial wound closure was observed. Images of the migrated cells were captured at 0, 24–48 h. The width of the wound area was measured via ImageJ software (NIH plugin: Background Correction; Colour Profile). The mobility ratio was determined via the following formula: Mobility=(scratch width at 0 h-scratch width at 24–48 h)/scratch width at 0 h × 100%.
Luciferase reporter assay. The wild type (WT) and mutant (MUT) lncRNA DDX11-AS1 sequences and the 3’-untranslated regions (3’-UTRs) of WT or MUT MTDH encompassing the miR-30c-5p binding sites were inserted into the pmirGLO luciferase vector (Shanghai GenePharma Co., Ltd.). HEK293T cells were cotransfected with miR-30c-5p or miR-NC mimics and luciferase reporter plasmids for 48 h at 37 °C via the FuGENE® HD Transfection Reagent (Promega Corporation). The cells were harvested and the luciferase activity was measured via a dual-luciferase reporter gene assay kit (Shanghai GenePharma Co., Ltd.), according to the manufacturer’s instructions.
Western blot analysis. Cell lysis and protein separation were carried out via RIPA lysis buffer (Beijing Solarbio Science & Technology Co., Ltd.) supplemented with protease and phosphatase inhibitor intact tablets (Beijing Solarbio Science & Technology Co., Ltd.). The Nuclear and Cytoplasmic Protein Extraction Kit (Beyotime Biotech, Inc.) was used to extract cytoplasmic and nuclear proteins, respectively, according to the manufacturer’s instructions. The protein concentration was measured via a BCA protein assay kit (Wuhan Boster Biological Technology, Ltd.). Total proteins were separated by 10% SDS‒PAGE and then electrotransferred onto PVDF membranes. Following blocking with 5% skim milk powder for 2 h at room temperature, the PVDF membranes were then incubated with primary antibodies against MTDH (dilution, 1:1000; rabbit; cat. no. 13860-1-AP), IκBα (dilution, 1:1000; rabbit; cat. no. 10268-1-AP), phosphorylation of IκBα (p-IκBα) (dilution, 1:5000; rabbit; cat. no. 82349-1-RR), p65 (dilution, 1:2000; rabbit; cat. no.10745-1-AP), p-p65 (dilution, 1:2000; rabbit; cat. no.82335-1-RR), Lamin B1 (dilution, 1:1000; rabbit; cat. no.12987-1-AP), and GAPDH (dilution, 1:10000; rabbit; cat. no.10494-1-AP; all from Proteintech Group, Inc.) at 4 °C overnight. The following day, the membranes were washed three times with TBS-Tween for 10 min and were then incubated with the corresponding secondary antibodies (dilution, 1:10000; anti-rabbit; cat. no. ZJ2020-R; from Bioworld Technology, Inc.) at room temperature for 2 h. Finally, the protein bands were visualized via a ChemiDoc XRS imaging system (Bio-Rad Laboratories) with an ECL solution.
Statistical analysis. All the statistical analyses were performed via SPSS 26.0 (IBM Corp.) and GraphPad Prism 8 (GraphPad Software, Inc.) software. All measured data are expressed as the mean ± standard deviation (SD). The differences among multiple groups were compared by one-way ANOVA and Tukey’s post hoc test or the χ2 test. Pearson correlation analysis was carried out to assess the association between DDX11-AS1 and miR-30c-5p in cell lines. All experiments were performed in at least three independent replicates. P < 0.05 was considered to indicate a statistically significant difference.
Results
DDX11-AS1 is upregulated in BC
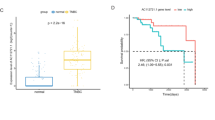
To predict the key lncRNAs, involved in BC progression, the public microarray GEO dataset GSE156229 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE156229), which contains the differential lncRNA expression profiles between tumour and normal tissues from patients with BC was analysed (fold change, ≥ 2 and P < 0.05; Fig. 1A). The analysis revealed that the lncRNA DDX11-AS1 was significantly differentially expressed in BC tissues. RNA-seq data from a BC cohort in the TCGA database also revealed that DDX11-AS1 expression was higher in BC tissues than in normal breast tissues, suggesting that DDX11-AS1 could promote the progression of BC (P < 0.001; Fig. 1B). In addition, RT‒qPCR analysis showed that DDX11-AS1 was notably upregulated in BC tissues derived from 36 patients with BC compared with normal tissues (P < 0.001; Fig. 1D). The clinicopathological characteristics of patients with BC are listed in Table 1. Furthermore, higher DDX11-AS1 expression levels were associated with high pathological grading and lymph node metastasis in patients with BC (P < 0.001; Fig. 1E and F). Moreover, compared with those in MCF10A normal breast epithelial cells, DDX11-AS1 expression levels were significantly greater in the BT549, MDA-MB-231, MCF7, MDA-MB-453 and SK-BR3 BC cell lines. The results revealed that the highest expression was in SK-BR3 cell line and slightly lower expression was in BT549 and MDA-MB-231 cells, but the difference was not significant (P < 0.05; Fig. 1C). We selected the SK-BR3 and MDA-MB-231 cell lines for subsequent validation. The MDA-MB-231 cell line was selected for overexpression because its endogenous expression level was lower than that of other cell lines, and the SK-BR3 cell line was selected for knockdown because it presented the highest expression. Collectively, the above findings indicate that the DDX11-AS1 expression levels are increased in BC tissues and BC cell lines, and that DDX11-AS1 may play a carcinogenic role in BC progression.
DDX11-AS1 expression was increased in BC tissues and cell lines. (A) Differential lncRNAs with a fold change ≥ 2 and p < 0.05 between BC samples and normal samples in the public GSE156229 dataset. (B) The expression of DDX11-AS1 in BC and normal tissues in the TCGA database. (C) DDX11-AS1 expression analysis in five BC cell lines and normal MCF-10 A cells; n = 3. (D) RT‒PCR analysis was performed to detect the expression of DDX11-AS1 in tumour and normal tissues from 36 BC patients; n = 3. (E) Differential expression of DDX11-AS1 across BC tissues with different pathological grades; n = 3. (F) Differential expression of DDX11-AS1 with or without lymph node metastasis in BC tissues; n = 3. *p < 0.05, **p < 0.01, ***p < 0.001.
DDX11-AS1 promotes BC cell proliferation, colony formation, migration and invasion
To evaluate the specific effects of DDX11-AS1 on BC, MDA-MB-231 cells were transfected with a pcDNA3.1 overexpression plasmid containing the DDX11-AS1 sequence. In addition, SK-BR3 cells were transfected with siRNA clones targeting DDX11-AS1 (si-DDX11-AS1-1,2,3). RT‒qPCR analysis revealed that DDX11-AS1 was successfully upregulated in MDA-MB-231 cells but downregulated in SK-BR3 cells (P < 0.05; Fig. 2A and C). Since si-DDX11-AS1-2 exhibited the most potent silencing activity, this siRNA clone was used for subsequent functional experiments. Therefore, CCK-8 assays demonstrated that SK-BR3 cell transfection with si-DDX11-AS1-2 significantly inhibited cell proliferation, whereas DDX11-AS1 overexpression in MDA-MB-231 cells had the opposite effect (P < 0.05; Fig. 2B and D). Consistently, colony formation assays further verified that DDX11-AS1 knockdown significantly inhibited SK-BR3 BC cell proliferation, whereas DDX11-AS1 overexpression significantly promoted the colony formation ability of MDA-MB-231 cells (P < 0.001; Fig. 2E-F). Furthermore, wound healing and Transwell assays were performed to assess the effects of DDX11-AS1 on the invasion and migration abilities of BC cells. The results revealed that DDX11-AS1 overexpression in MDA-MB-231 cells promoted cell invasion and migration, whereas SK-BR3 cell transfection with si-DDX11-AS1-2 yielded the opposite results (P < 0.001; Fig. 2G-J).
DDX11-AS1 knockdown inhibited BC cell proliferation in vitro. si-DDX11-AS1 or si-NC was transfected into SK-BR3 cells, and DDX11-AS1 or pcDNA3.1 was introduced into MDA-MB-231 cells. (A) Transfection efficiency of DDX11-AS1 in MDA-MB-231 cells, as determined via qRT‒PCR; n = 3. (B) Cell proliferation of MDA-MB-231 cells after transfection, as determined by a CCK-8 assay; n = 3. (C) Transfection efficiency of si-DDX11-AS1 in SK-BR3 cells; n = 3. (D) SK-BR3 cell proliferation was assessed via a CCK-8 assay after transfection; n = 3. (E-F) Cell proliferation of MDA-MB-231 and SK-BR3 cells, as determined by a colony formation assay; n = 6. (G-H)Cell migration was assessed via wound healing assays after the transfection of MDA-MB-231 and SK-BR3 cells. Scale bar, 200 μm; n = 6. (I-J) Cell invasion and migration abilities were evaluated by transwell assays in each group. Scale bar, 200 μm; n = 6. *p < 0.05, **p < 0.01, ***p < 0.001.
DDX11-AS1 sponges miR-30c-5p in BC cells
It is widely accepted that the functions and mechanisms of lncRNAs are associated with their particular cellular localization30. Therefore, a subcellular distribution assay was performed to verify the subcellular localization of DDX11-AS1 in BC cells. DDX11-AS1 was detected in both the nuclear and cytoplasmic fractions of MDA-MB-231 and SK-BR3 cells (P < 0.05; Fig. 3A and B). It was therefore hypothesized that DDX11-AS1 could act as a ceRNA to sponge miRNAs. To further verify the mechanism underlying the effect of DDX11-AS1 on BC, the expression profile of miRNAs was analysed via the GEO GSE45666 database (fold change, ≤-2 and P < 0.05; Fig. 3C). Additionally, the StarBase V3.0 database predicted that DDX11-AS1 contains binding sites for both miR-30c-5p and miR-30e-5p. In addition, bioinformatics analysis revealed that miR-30c-5p was significantly downregulated in the GEO GSE45666 dataset. However, the expression levels of miR-30e-5p were greater (P < 0.05; Fig. 3D and E). Additionally, the expression levels of miR-30c-5p were lower in BC tissues than in normal tissues. The above finding was consistent with that observed in the GEO dataset (P < 0.001; Fig. 3F). To verify the results of the bioinformatics analysis, DDX11-AS1 was silenced in SK-BR3 cells and overexpressed in MDA-MB-231 cells. RT‒qPCR analysis revealed that miR-30c-5p was upregulated in DDX11-AS1-depleted BC cells and downregulated in DDX11-AS1 overexpressing BC cells (P < 0.05; Fig. 3G-H). These findings verified that miR-30c-5p could be a potential target of DDX11-AS1 (Fig. 3I). Subsequently, dual-luciferase reporter gene assays were performed in 293T cells to confirm whether DDX11-AS1 could sponge miR-30c-5p. Therefore, the luciferase activity of the DDX11-AS1-WT reporter plasmid was significantly reduced in cells cotransfected with miR-30c-5p mimics, whereas this inhibition was eliminated when the binding site of miR-30c-5p in the DDX11-AS1 sequence was mutated (P < 0.001; Fig. 3J). These results verified that DDX11-AS1 could sponge miR-30c-5p to inhibit its expression.
DDX11-AS1 interacted with miR-30c-5p to inhibit its expression. (A-B) The expression level of DDX11-AS1 in the subcellular fractions of MDA-MB-231 and SK-BR3 cells was detected via qRT‒PCR. U6 and GAPDH were used as nuclear and cytoplasmic markers, respectively; n = 6. (C) Differentially expressed miRNAs with a fold change ≤-2 and p < 0.05 between BC samples and normal samples in the GEO GSE45666 database. (D-E) The expression of miR-30c-5p and miR-30e-5p in BC and normal tissues in the GEO GSE45666 database. (F) RT‒qPCR analysis of the expression of miR-30c-5p in tumour and normal tissues from 15 BC patients. (G-H) Effects of si-DDX11-AS1 and OE-DDX11-AS1 on the expression of miR-30c-5p in SK-BR3 and MDA-MB-231 cells. DDX11-AS1 and miR-30c-5p were negatively correlated; n = 6. (I) Predicted binding sites on DDX11-AS1 that sponge miR-30c-5p. (J) Dual-luciferase reporter assays in HEK293T cells were carried out to investigate the interaction between miR-30c-5p and DDX11-AS1; n = 3. *p < 0.05, **p < 0.01, ***p < 0.001.
miR-30c-5p silencing abolishes the suppressive effect of DDX11-AS1 knockdown on BC cells
Subsequently, rescue experiments were carried out to further investigate whether DDX11-AS1 could promote the progression of BC by regulating miR-30c-5p. CCK-8 and colony formation assays demonstrated that miR-30c-5p silencing partially reversed the inhibitory effect of DDX11-AS1-2 silencing on cell proliferation, whereas miR-30c-5p overexpression rescued the effect of DDX11-AS1 overexpression (P < 0.01; Fig. 4A-F). Additionally, the wound healing assays produced the same results (P < 0.001; Fig. 4G-H). In general, the above findings suggest that miR-30c-5p could be an inhibitory target of DDX11-AS1 in BC.
DDX11-AS1 sponges miR-30c-5p in BC. Si-DDX11-AS1 or si-NC and the miR-30c-5p or NC inhibitor were cotransfected into SK-BR3 cells, and DDX11-AS1 or pcDNA3.1 and the miR-30c-5p or NC mimic were introduced into MDA-MB-231 cells. (A-F)CCK-8 assay and colony formation assay for SK-BR3 and MDA-MB-231 cells after cotransfection; n = 12. (G-H) Cell migration was assessed via wound healing assays after cotransfection. Scale bar, 200 μm; n = 6. *p < 0.05, **p < 0.01, ***p < 0.001. OE-lnc: Overexpression of DDX11-AS1, miR mimic: miR-30c-5p mimic, NC-inh: NC-inhibitor, si-lnc: si-DDX11-AS1, miR inh: miR-30c-5p inhibitor.
DDX11-AS1 sponges miR-30c-5p to regulate the expression of MTDH in BC cells
Bioinformatics analysis via the miRDB, miRWalk, miRanda and TargetScan databases revealed that MTDH could be a potential target of miR-30c-5p (Fig. 5A). Furthermore, the analysis revealed that MTDH expression was positively and negatively associated with that of DDX11-AS1 and miR-30c-5p, respectively (P < 0.01; Fig. 5C and D). In addition, the TargetScan database predicted that MTDH encompassed a sequence complementary to miR-30c-5p. This result suggested that MTDH could act as a potential target of miR-30c-5p and was therefore selected for further investigation. Therefore, luciferase assays revealed that miR-30c-5p overexpression reduced the luciferase activity of the WT MTDH reporter plasmid, but not that of the MUT reporter plasmid, further confirming that MTDH was a direct target of miR-30c-5p (P < 0.001; Fig. 5B and E). The effect of DDX11-AS1 on the protein expression levels of MTDH was then assessed via Western blot analysis. The results demonstrated that the protein expression levels of MTDH were significantly increased by DDX11-AS1 overexpression and miR-30c-5p knockdown, but were reduced by DDX11-AS1 knockdown and miR-30c-5p overexpression.(P < 0.05; Fig. 5F-G). These results revealed that the DDX11-AS1/miR-30c-5p/MTDH axis promotes the progression of BC (Fig. 5H).
MTDH is a direct target of miR-30c-5p (A) Venn diagram showing the putative target genes of miR-30c-5p identified by miRWalk, miRDB, TargetScan, and miRanda. (B) Predicted binding sites and potential mutation sequences of the miR-30c-5p binding sites in MTDH. (C-D) Effects of si-DDX11-AS1 and the miR-30c-5p inhibitor on the expression of MTDH in SK-BR3 cells; n = 6. (E) Luciferase activity of WT or MUT luciferase plasmids after transfection with miR-30c-5p mimics in HEK293T cells; n = 3. (F-G) Western blot assays were used to determine the MTDH expression level in MDA-MB-231 and SK-BR3 cells cotransfected with DDX11-AS1 and the miR-30c-5p mimic or with si-DDX11-AS1 and the miR-30c-5p inhibitor, and the original blots are presented in Figure S2; n = 6. (H) A schematic model of how the DDX11-AS1/miR-30c-5p/MTDH axis promotes the progression of BC by regulating the activation of the NF-κB signalling pathway. *p < 0.05, **p < 0.01, ***p < 0.001. OE-lnc: Overexpression of DDX11-AS1, si-lnc: si-DDX11-AS1, miR mimic: miR-30c-5p mimic, NC-inh: NC-inhibitor, miR inh: miR-30c-5p inhibitor, BC: breast cancer.
The DDX11-AS1/miR-30c-5p/MTDH axis promotes the progression of BC by regulating the activation of the NF-κB signalling pathway
To determine the role of the DDX11-AS1/miR-30c-5p/MTDH axis in BC, MDA-MB-231 cells were cotransfected with miR-30c-5p mimics with or without an MTDH overexpression plasmid. In addition, SK-BR3 cells were transfected with a miR-30c-5p inhibitor with or without a siRNA clone targeting MTDH. The transfection efficiency was determined by RT‒qPCR (P < 0.001; Fig. 6A and C). The results showed that miR-30c-5p overexpression inhibited BC cell proliferation and this effect was reversed by MTDH overexpression. In contrast, the transfection of SK-BR3 cells with miR-30c-5p inhibitors significantly promoted cell proliferation, which was attenuated by MTDH knockdown (P < 0.01; Fig. 6B and D, E and F). Furthermore, miR-30c-5p overexpression attenuated BC cell migration and invasion, whereas miR-30c-5p knockdown enhanced these processes. These effects were abolished by MTDH overexpression or knockdown (P < 0.001; Fig. 6G-H). In addition, Western blot analysis demonstrated that the overexpression of MTDH promoted iκBα degradation, increased p-p65 levels to activate the NF-κB pathway, and caused the nuclear translocation of p65, whereas the knockdown of MTDH had the opposite effect. (P < 0.01; Fig. 6I, J and Fig. S1). The above data suggested that DDX11-AS1 promoted BC by regulating MTDH through competitively binding to miR-30c-5p in vitro.
The DDX11-AS1/miR-30c-5p/MTDH axis promotes progression in BC cells. Si-MTDH or si-NC and the miR-30c-5p or NC inhibitor were cotransfected into SK-BR3 cells, and MTDH or the empty vector and the miR-30c-5p or NC mimic were introduced into MDA-MB-231 cells. (A) The expression levels of miR-30c-5p in MDA-MB-231 cells were determined via qRT‒PCR; n = 3. (B) CCK-8 assay for MDA-MB-231 cells after cotransfection; n = 3. (C)The expression levels of miR-30c-5p in SK-BR3 cells were determined via qRT‒PCR; n = 3. (D) CCK-8 assay in SK-BR3 cells after cotransfection; n = 3. (E-F) The effects of the cotransfection of miR-30c-5p and MTDH on cell proliferation were examined via a colony formation assay; n = 6. (G-H) Cell invasion and migration abilities were evaluated by transwell assays in each group. Scale bar, 200 μm; n = 6. (I-J) Western blot analysis of the protein expression levels of p65, p-p65, IκBα, p-IκBα, N-p65, C-p65, and MTDH after transfection; the original blots are presented in Figure S3-4 and Figure S5-6; n = 6. *p < 0.05, **p < 0.01, ***p < 0.001. miR mimic: miR-30c-5p mimic; NC-inh: NC-inhibitor; si-lnc: si-DDX11-AS1; miR-inh: miR-30c-5p inhibitor. p-p65: p65 phosphorylation, p-IκBα: phosphorylation of IκBα, C-p65: cytoplasmic p65, N-p65: nuclear p65.
Discussion
LncRNAs, noncoding RNAs, are involved in a range of biological functions related to carcinogenesis and have therefore received increasing attention31,32. Accumulating evidence has indicated that lncRNAs located in the cytoplasm serve as ceRNAs to protect target mRNAs from repression, while they are involved in gene regulation at the posttranscriptional level8,17. The significant role of lncRNAs as ceRNAs has been previously verified in BC11,33,34. Previous studies on DDX11-AS1 in breast cancer have demonstrated that its expression is upregulated in BC cell lines as well as in drug-resistant cell lines16,17. However, in the present study, we examined the relative expression level of DDX11-AS1 in paired BC tissues and normal tissues and confirmed that its expression is significantly upregulated in BC tissues. Moreover, the DDX11-AS1 expression level increased with increasing pathological stage and lymph node metastasis, suggesting that DDX11-AS1 is associated with poor prognosis in BC patients. Functional studies demonstrated that DDX11-AS1 overexpression facilitated the proliferation, invasion and migration of BC cells in vitro, and these findings further reinforce the potential role of DDX11-AS1 in breast cancer development and progression. When investigating the role of DDX11-AS1 in other cancers, we found that it functions primarily as a ceRNA to regulate gene expression13,14,15. In the present study, subcellular distribution assays also revealed that DDX11-AS1 was expressed in the cytoplasm of BC cells, suggesting that it could act as a ceRNA to sponge miRNAs.
Previous studies have demonstrated that miR-30c-5p can inhibit the progression of different types of cancer, such as oral squamous cell carcinoma, gastric cancer and clear cell renal cell carcinoma35,36,37. Pei et al20. reported that miR-30c-5p could restrain tumour metastasis and BC cell migration by targeting coactosin-like protein 1. Furthermore, Yen et al21. demonstrated that isolinderalactone inhibited the STAT3 signalling pathway by regulating suppressor of cytokine signalling 3 and miR-30c in BC. Herein, bioinformatics analysis via the StarBase V3.0 database predicted that miR-30c-5p encompassed a complementary sequence of DDX11-AS1. This finding was further verified by dual-luciferase reporter assays. Additionally, the results revealed that DDX11-AS1 was upregulated and that miR-30c-5p was downregulated in BC tissues, further suggesting that DDX11-AS1 expression was negatively associated with that of miR-30c-5p. Therefore, miR-30c-5p overexpression could partially reverse the promotive effect of DDX11-AS1 on the behaviour of BC cells. Overall, the results suggested that DDX11-AS1 could sponge miR-30c-5p to inhibit its expression.
MTDH is ubiquitously expressed in almost all human tissues at variable levels, while its expression levels are dramatically increased in cancer22. One study revealed that the abundance of MTDH was positively associated with advanced clinical stages, clinicopathological features, distant metastasis and poor survival in patients with BC38. MTDH expression in cancer cells can be modulated through a miRNA-mediated posttranslational process39. For example, miR-375 can attenuate the growth of hepatocellular carcinoma by downregulating MTDH40. In the present study, dual-luciferase reporter assays combined with bioinformatics analysis indicated that MTDH could be a direct target of miR-30c-5p. In addition, DDX11-AS1 positively regulates MTDH expression in BC. Furthermore, the effects of the DDX11-AS1/miR-30c-5p/MTDH axis on the progression of BC were verified via in vitro rescue experiments, and our results revealed that the overexpression of MTDH could activate the NF-κB pathway by increasing p-p65 levels and causing the nuclear translocation of p65, which is consistent with the findings of previous studies41. Previous studies have shown that MTDH and NF-κB are involved in paclitaxel and doxorubicin drug resistance and that MTDH overexpression may mediate trastuzumab resistance by increasing p65 nuclear translocation22,27,41,42. Additionally, DDX11-AS1 was upregulated in drug-resistant BC cell lines, suggesting that DDX11-AS1 could be involved in the resistance of BC cells to paclitaxel, doxorubicin and trastuzumab through the MTDH/NF-κB axis16,17,41. It was therefore hypothesized that the DDX11-AS1/miR-30c-5p/MTDH axis could play a key role in the chemoresistance of BC cells. However, our study was challenged by the limited availability of specimens, precluding a definitive validation of the correlation between DDX11-AS1 and BC patient prognosis and drug resistance. Furthermore, our research did not proceed to functional validation at the animal level. These limitations also serve as directions for our future research.
In conclusion, the present study confirmed that DDX11-AS1 acted as a tumour promoter factor in BC by acting as a ceRNA. As a sponge of miR-30c-5p, DDX11-AS1 weakened its inhibitory effect on MTDH and promoted cell proliferation, migration, invasion and activation of the NF-κB signalling pathway in BC. Overall, the present study suggested that the DDX11-AS1/miR-30c-5p/MTDH axis could be a potential target in BC therapy.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. Ca-Cancer J. Clin. 73, 17–48 (2023).
Saad, E. D., Katz, A. & Buyse, M. Overall survival and post-progression survival in advanced breast cancer: a review of recent randomized clinical trials. J. Clin. Oncol. 28, 1958–1962 (2010).
Liu, P. et al. The FUS/circEZH2/KLF5/ feedback loop contributes to CXCR4-induced liver metastasis of breast cancer by enhancing epithelial-mesenchymal transition. Mol. Cancer. 21, 198 (2022).
Zeng, Y. et al. Hsa_circ_0060467 promotes breast cancer liver metastasis by complexing with eIF4A3 and sponging miR-1205. Cell. Death Discov. 9, 153 (2023).
Chen, Z. et al. Long non-coding RNA SNHG20 promotes non-small cell lung cancer cell proliferation and migration by epigenetically silencing of P21 expression. Cell. Death Dis. 8, e3092 (2017).
Li, D. et al. Identification of a novel human long non-coding RNA that regulates hepatic lipid metabolism by inhibiting SREBP-1c. Int. J. Biol. Sci. 13, 349–357 (2017).
Prensner, J. R. & Chinnaiyan, A. M. The emergence of lncRNAs in cancer biology. Cancer Discov. 1, 391–407 (2011).
Salmena, L., Poliseno, L., Tay, Y., Kats, L. & Pandolfi, P. P. A ceRNA hypothesis: the rosetta stone of a hidden RNA language? Cell. 146, 353–358 (2011).
Paraskevopoulou, M. D. & Hatzigeorgiou, A. G. Analyzing MiRNA-LncRNA interactions. Methods Mol. Biol. 1402, 271–286 (2016).
An, Y., Furber, K. L. & Ji, S. Pseudogenes regulate parental gene expression via ceRNA network. J. Cell. Mol. Med. 21, 185–192 (2017).
Liang, Y. et al. LncRNA BCRT1 promotes breast cancer progression by targeting miR-1303/PTBP3 axis. Mol. Cancer. 19, 85 (2020).
Gao, J. et al. Inhibition of ZEB1-AS1 confers cisplatin sensitivity in breast cancer by promoting microRNA-129-5p-dependent ZEB1 downregulation. Cancer Cell. Int. 20, 90 (2020).
Wan, T. et al. LncRNA DDX11-AS1 accelerates hepatocellular carcinoma progression via the miR-195-5p/MACC1 pathway. Ann. Hepatol. 20, 100258 (2021).
Liu, J., Yang, X., Gao, S., Wen, M. & Yu Qiong DDX11-AS1 modulates DNA damage repair to enhance paclitaxel resistance of lung adenocarcinoma cells. Pharmacogenomics. 24, 163–172 (2023).
Marchese, F. P. et al. A long noncoding RNA regulates sister chromatid cohesion. Mol. Cell. 63, 397–407 (2016).
Si, X. et al. DDX11-AS1 promotes Chemoresistance through LIN28A-Mediated ATG12 mRNA stabilization in breast Cancer. PHARMACOLOGY. 108, 61–73 (2023).
Liang, M., Zhu, B., Wang, M. & Jin, J. Knockdown of long noncoding RNA DDX11AS1 inhibits the proliferation, migration and paclitaxel resistance of breast cancer cells by upregulating microRNA-497 expression. Mol. Med. Rep. 25, 123 (2022).
Xiang, W. & Zhang, B. LncRNA DLEU2 contributes to Taxol resistance of gastric cancer cells through regulating the miR-30c-5p-LDHA axis. J. Chemother. 36, 49–60 (2024).
Chen, X. et al. PRMT5 circular RNA promotes metastasis of Urothelial Carcinoma of the bladder through sponging miR-30c to induce epithelial-mesenchymal T ransition. Clin. Cancer Res. 24, 6319–6330 (2018).
Pei, B. Al Downregulation of microRNA-30c-5p was responsible for cell migration and tumor metastasis via COTL1-mediated microfilament arrangement in breast cancer. Gland Surg. 9, 747–758 (2020).
Yen, M. C. et al. Isolinderalactone enhances the inhibition of SOCS3 on STAT3 activity by decreasing miR-30c in breast cancer. Oncol. Rep. 35, 1356–1364 (2016).
Kang, D. C. et al. Cloning and characterization of HIV-1-inducible astrocyte elevated gene-1, AEG-1. Gene 353, 8–15 (2005).
Song, Z., Wang, Y., Li, C., Zhang, D. & Wang, X. Molecular modification of Metadherin/MTDH impacts the sensitivity of breast Cancer to Doxorubicin. Plos One. 10, e0127599 (2015).
Blanco, M. A. et al. Identification of staphylococcal nuclease domain-containing 1 (SND1) as a metadherin-interacting protein with metastasis-promoting functions. J. Biol. Chem. 286, 19982–19992 (2011).
Lee, S. G., Kang, D. C., DeSalle, R., Sarkar, D. & Fisher, P. B. AEG-1/MTDH/LYRIC, the beginning: initial cloning, structure, expression profile, and regulation of expression. Adv. Cancer Res. 120, 1–38 (2013).
Yoo, B. K. et al. Astrocyte elevated gene-1 (AEG-1): a multifunctional regulator of normal and abnormal physiology. Pharmacol. Ther. 130, 1–8 (2011).
Yang, L. et al. Efficient and tumor-specific knockdown of MTDH gene attenuates paclitaxel resistance of breast cancer cells both in vivo and in vitro. Breast Cancer Res. 20, 113 (2018).
Li, J. et al. Astrocyte elevated gene-1 is a novel prognostic marker for breast cancer progression and overall patient survival. Clin. Cancer Res. 14, 3319–3326 (2008).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2(– Delta Delta C(T)) method. Methods. 25, 402–408 (2001).
Zhang, K. et al. The ways of action of long non-coding RNAs in cytoplasm and nucleus. Gene. 547, 1–9 (2014).
Sun, M., Nie, F., Wang, Z. & De, W. Involvement of lncRNA dysregulation in gastric cancer. Histol. Histopathol. 31, 33–39 (2016).
Cen, S. Z. et al. The role of AFAP1-AS1 in mitotic catastrophe and metastasis of triple-negative breast cancer cells by activating the PLK1 signaling pathway. Oncol. Res. 31, 375–388 (2023).
Feng, J. et al. Cross-talk between the ER pathway and the lncRNA MAFG-AS1/miR-339-5p/ CDK2 axis promotes progression of ER + breast cancer and confers tamoxifen resistance. Aging (Albany NY). 12, 20658–20683 (2020).
Mao, Q. et al. Long non coding RNA NRON inhibited breast cancer development through regulating miR-302b/SRSF2 axis. Am. J. Transl Res. 12, 4683–4692 (2020).
Mehterov, N. et al. Salivary miR-30c-5p as potential biomarker for detection of oral squamous cell carcinoma. Biomedicines. 9, 1079 (2021).
Cao, J., Li, G., Han, M., Xu, H. & Huang, K. MiR-30c-5p suppresses migration, invasion and epithelial to mesenchymal transition of gastric cancer via targeting MTA1. Biomed. Pharmacother. 93, 554–560 (2017).
Outeiro-Pinho, G. et al. Epigenetically-regulated miR-30a/c-5p directly target TWF1 and hamper ccRCC cell aggressiveness. Transl Res. 249, 110–127 (2022).
Wan, L. & Kang, Y. Pleiotropic roles of AEG-1/MTDH/LYRIC in breast cancer. Adv. Cancer Res. 120, 113–134 (2013).
Khan, M. & Sarkar, D. The scope of astrocyte elevated Gene-1/Metad-herin (AEG-1/MTDH) in Cancer Clinicopathology: a review. Genes (Basel). 12, 308 (2021).
He, X. et al. MicroRNA-375 targets AEG-1 in hepatocellular carcinoma and suppresses liver cancer cell growth in vitro and in vivo. Oncogene. 31, 3357–3369 (2012).
Du, C. et al. MTDH mediates trastuzumab resistance in HER2 positive breast cancer by decreasing PTEN expression through an NF-κB-dependent pathway. BMC Cancer. 14, 869 (2014).
Abdin, S. M., Tolba, M. F., Zaher, D. M. & Omar, H. A. Nuclear factor-κB signaling inhibitors revert multidrug-resistance in breast cancer cells. Chem-biol Interact. 340, 109450 (2021).
Funding
This study was supported by the Provincial Health Commission of Hebei Province (grant no. 20230485), the Natural Science Foundation of Hebei Province (grant no. H2020206365 and H2021206071), the S&T Program of Hebei Province (grant no. 236Z7719G), the Special Fund for Clinical Research of the Wu Jieping Medical Foundation (grant no. 320.6750.2020/07/17) and the Bethune Cancer Basic Research Program (grant no. BCF-NH-ZL-20201119-013).
Author information
Authors and Affiliations
Contributions
ZCS conceived, designed and oversaw the study. SL collected the clinical specimens and data. YTL and MSZ conducted the experiments. LY, BX and LXY analysed and interpreted the data. YTL wrote the manuscript. ZCS critically revised the manuscript for significant intellectual content. XLL and HJZ confirmed the authenticity of all the raw data. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Fourth Hospital of Hebei Medical University (approval no. 2021KY056) and all studies were conducted in accordance with relevant guidelines. All patients agreed and provided signed informed consent. The present study was conducted in accordance with the principles described in the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Y., Zhou, M., Yang, L. et al. LncRNA DDX11-AS1 promotes breast cancer progression by targeting the miR-30c-5p/MTDH axis. Sci Rep 14, 26745 (2024). https://doi.org/10.1038/s41598-024-78413-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-78413-3