Abstract
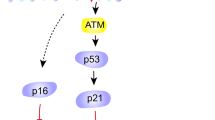
Physical function declines in old age, portending disability, increased health expenditures, and mortality. Cellular senescence, leading to tissue dysfunction, may contribute to these consequences of aging, but whether senescence can directly drive age-related pathology and be therapeutically targeted is still unclear. Here we demonstrate that transplanting relatively small numbers of senescent cells into young mice is sufficient to cause persistent physical dysfunction, as well as to spread cellular senescence to host tissues. Transplanting even fewer senescent cells had the same effect in older recipients and was accompanied by reduced survival, indicating the potency of senescent cells in shortening health- and lifespan. The senolytic cocktail, dasatinib plus quercetin, which causes selective elimination of senescent cells, decreased the number of naturally occurring senescent cells and their secretion of frailty-related proinflammatory cytokines in explants of human adipose tissue. Moreover, intermittent oral administration of senolytics to both senescent cell–transplanted young mice and naturally aged mice alleviated physical dysfunction and increased post-treatment survival by 36% while reducing mortality hazard to 65%. Our study provides proof-of-concept evidence that senescent cells can cause physical dysfunction and decreased survival even in young mice, while senolytics can enhance remaining health- and lifespan in old mice.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Crimmins, E. M. Lifespan and healthspan: past, present, and promise. Gerontologist 55, 901–911 (2015).
Fries, J. F. Aging, natural death, and the compression of morbidity. N. Engl. J. Med. 303, 130–135 (1980).
Michaud, M. et al. Proinflammatory cytokines, aging, and age-related diseases. J. Am. Med. Dir. Assoc. 14, 877–882 (2013).
Fried, L. P. et al. Frailty in older adults: evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146–M156 (2001).
Collard, R. M., Boter, H., Schoevers, R. A. & Oude Voshaar, R. C. Prevalence of frailty in community-dwelling older persons: a systematic review. J. Am. Geriatr. Soc. 60, 1487–1492 (2012).
Song, X., Mitnitski, A. & Rockwood, K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J. Am. Geriatr. Soc. 58, 681–687 (2010).
Xue, Q. L. The frailty syndrome: definition and natural history. Clin. Geriatr. Med. 27, 1–15 (2011).
Tchkonia, T., Zhu, Y., van Deursen, J., Campisi, J. & Kirkland, J. L. Cellular senescence and the senescent secretory phenotype: therapeutic opportunities. J. Clin. Invest. 123, 966–972 (2013).
Campisi, J. & d’Adda di Fagagna, F. Cellular senescence: when bad things happen to good cells. Nat. Rev. Mol. Cell Biol. 8, 729–740 (2007).
Wiley, C. D. et al. Mitochondrial dysfunction induces senescence with a distinct secretory phenotype. Cell Metab. 23, 303–314 (2016).
Wang, C. et al. DNA damage response and cellular senescence in tissues of aging mice. Aging Cell 8, 311–323 (2009).
Zhu, Y., Armstrong, J. L., Tchkonia, T. & Kirkland, J. L. Cellular senescence and the senescent secretory phenotype in age-related chronic diseases. Curr. Opin. Clin. Nutr. Metab. Care 17, 324–328 (2014).
Coppé, J. P. et al. Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS Biol. 6, 2853–2868 (2008).
Xu, M. et al. JAK inhibition alleviates the cellular senescence–associated secretory phenotype and frailty in old age. Proc. Natl. Acad. Sci. USA 112, E6301–E6310 (2015).
Xu, M. et al. Targeting senescent cells enhances adipogenesis and metabolic function in old age. eLife 4, e12997 (2015).
Xu, M. et al. transplanted senescent cells induce an osteoarthritis-like condition in mice. J. Gerontol. A Biol. Sci. Med. Sci. 72, 780–785 (2017).
Palmer, A. K. et al. cellular senescence in type 2 diabetes: a therapeutic opportunity. Diabetes 64, 2289–2298 (2015).
Chang, J. et al. Clearance of senescent cells by ABT263 rejuvenates aged hematopoietic stem cells in mice. Nat. Med. 22, 78–83 (2016).
Childs, B. G. et al. Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science 354, 472–477 (2016).
Baker, D. J. et al. Naturally occurring p16Ink4a-positive cells shorten healthy lifespan. Nature 530, 184–189 (2016).
Xu, M., Tchkonia, T. & Kirkland, J. L. Perspective: targeting the JAK/STAT pathway to fight age-related dysfunction. Pharmacol. Res. 111, 152–154 (2016).
Bitto, A. et al. Transient rapamycin treatment can increase lifespan and healthspan in middle-aged mice. eLife 5, e16351 (2016).
Tchkonia, T. et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. 17, 644–656 (2013).
Farr, J. N. et al. Identification of senescent cells in the bone microenvironment. J. Bone Miner. Res. 31, 1920–1929 (2016).
Schafer, M. J. et al. Cellular senescence mediates fibrotic pulmonary disease. Nat. Commun. 8, 14532 (2017).
Ryan, J. M., Barry, F. P., Murphy, J. M. & Mahon, B. P. Mesenchymal stem cells avoid allogeneic rejection. J. Inflamm. (Lond.) 2, 8 (2005).
Tchkonia, T. et al. Fat tissue, aging, and cellular senescence. Aging Cell 9, 667–684 (2010).
Acosta, J. C. et al. A complex secretory program orchestrated by the inflammasome controls paracrine senescence. Nat. Cell Biol. 15, 978–990 (2013).
Nelson, G. et al. A senescent cell bystander effect: senescence-induced senescence. Aging Cell 11, 345–349 (2012).
Hewitt, G. et al. Telomeres are favoured targets of a persistent DNA damage response in ageing and stress-induced senescence. Nat. Commun. 3, 708 (2012).
Walston, J. et al. The physical and biological characterization of a frail mouse model. J. Gerontol. A Biol. Sci. Med. Sci. 63, 391–398 (2008).
Schafer, M. J. et al. Exercise prevents diet-induced cellular senescence in adipose tissue. Diabetes 65, 1606–1615 (2016).
Mosier, D. E., Stell, K. L., Gulizia, R. J., Torbett, B. E. & Gilmore, G. L. Homozygous scid/scid;beige/beige mice have low levels of spontaneous or neonatal T cell-induced B cell generation. J. Exp. Med. 177, 191–194 (1993).
Kirkland, J. L. & Tchkonia, T. Cellular senescence: a translational perspective. EBioMedicine 21, 21–28 (2017).
Zhu, Y. et al. The Achilles’ heel of senescent cells: from transcriptome to senolytic drugs. Aging Cell 14, 644–658 (2015).
Stern, J. H., Rutkowski, J. M. & Scherer, P. E. Adiponectin, leptin, and fatty acids in the maintenance of metabolic homeostasis through adipose tissue crosstalk. Cell Metab. 23, 770–784 (2016).
Farmer, S. R. Transcriptional control of adipocyte formation. Cell Metab. 4, 263–273 (2006).
Reuben, D. B., Judd-Hamilton, L., Harris, T. B. & Seeman, T. E. The associations between physical activity and inflammatory markers in high-functioning older persons: MacArthur Studies of Successful Aging. J. Am. Geriatr. Soc. 51, 1125–1130 (2003).
Cohen, H. J., Pieper, C. F., Harris, T., Rao, K. M. & Currie, M. S. The association of plasma IL-6 levels with functional disability in community-dwelling elderly. J. Gerontol. A Biol. Sci. Med. Sci. 52, M201–M208 (1997).
Beyer, I. et al. Inflammation-related muscle weakness and fatigue in geriatric patients. Exp. Gerontol. 47, 52–59 (2012).
Lu, Y. et al. Inflammatory and immune markers associated with physical frailty syndrome: findings from Singapore longitudinal aging studies. Oncotarget 7, 28783–28795 (2016).
Kao, T. W. et al. Examining how p16INK4a expression levels are linked to handgrip strength in the elderly. Sci. Rep. 6, 31905 (2016).
Justice, J. N. et al. Cellular senescence biomarker p16INK4a+ cell burden in thigh adipose is associated with poor physical function in older women. J. Gerontol. A Biol. Sci. Med. Sci. 73, 939–945 (2017).
Christopher, L. J. et al. Metabolism and disposition of dasatinib after oral administration to humans. Drug Metab. Dispos. 36, 1357–1364 (2008).
Graefe, E. U. et al. Pharmacokinetics and bioavailability of quercetin glycosides in humans. J. Clin. Pharmacol. 41, 492–499 (2001).
Roos, C. M. et al. Chronic senolytic treatment alleviates established vasomotor dysfunction in aged or atherosclerotic mice. Aging Cell 15, 973–977 (2016).
Farr, J. N. et al. Targeting cellular senescence prevents age-related bone loss in mice. Nat. Med. 23, 1072–1079 (2017).
Ogrodnik, M. et al. Cellular senescence drives age-dependent hepatic steatosis. Nat. Commun. 8, 15691 (2017).
Baker, D. J. et al. Clearance of p16Ink4a-positive senescent cells delays ageing-associated disorders. Nature 479, 232–236 (2011).
Srinivas-Shankar, U. & Wu, F. C. Frailty and muscle function: role for testosterone? Front. Horm. Res. 37, 133–149 (2009).
Hall, B. M. et al. p16Ink4a and senescence-associated β-galactosidase can be induced in macrophages as part of a reversible response to physiological stimuli. Aging (Albany NY) 9, 1867 (2017).
Helman, A. et al. p16Ink4a-induced senescence of pancreatic beta cells enhances insulin secretion. Nat. Med. 22, 412–420 (2016).
Costa, L. G., Garrick, J. M., Roquè, P. J. & Pellacani, C. Mechanisms of neuroprotection by quercetin: counteracting oxidative stress and more. Oxid. Med. Cell. Longev. 2016, 2986796 (2016).
Montani, D. et al. Pulmonary arterial hypertension in patients treated by dasatinib. Circulation 125, 2128–2137 (2012).
Kirkland, J. L., Tchkonia, T., Zhu, Y., Niedernhofer, L. J. & Robbins, P. D. The clinical potential of senolytic drugs. J. Am. Geriatr. Soc. 65, 2297–2301 (2017).
Kane, A. E. et al. Animal models of frailty: current applications in clinical research. Clin. Interv. Aging 11, 1519–1529 (2016).
Ness, K. K. et al. Frailty in childhood cancer survivors. Cancer 121, 1540–1547 (2015).
Pajvani, U. B. et al. Fat apoptosis through targeted activation of caspase 8: a new mouse model of inducible and reversible lipoatrophy. Nat. Med. 11, 797–803 (2005).
Miller, R. A. et al. An aging interventions testing program: study design and interim report. Aging Cell 6, 565–575 (2007).
Ikeno, Y. et al. Housing density does not influence the longevity effect of calorie restriction. J. Gerontol. A Biol. Sci. Med. Sci. 60, 1510–1517 (2005).
Tchkonia, T. et al. Increased TNFα and CCAAT/enhancer-binding protein homologous protein with aging predispose preadipocytes to resist adipogenesis. Am. J. Physiol. Endocrinol. Metab. 293, E1810–E1819 (2007).
Jurk, D. et al. Chronic inflammation induces telomere dysfunction and accelerates ageing in mice. Nat. Commun. 2, 4172 (2014).
Xu, J. Preparation, culture, and immortalization of mouse embryonic fibroblasts. Curr. Protoc. Mol. Biol. 70, 28.1.1–28.1.8 (2005).
Acknowledgements
The authors are grateful to J. L. Armstrong and L. Thesing for administrative assistance, M. Mahlman for obtaining human adipose tissue samples, Z. Aversa for help with muscle analysis, the Pathology Research Core Lab at Mayo Clinic–Rochester for histology studies, and C. Guo for overall support. This work was supported by the Connor Group (J.L.K.) and Robert J. and Theresa W. Ryan (J.L.K.); the National Institutes of Health (NIH) grants AG13925 (J.L.K.), AG49182 (J.L.K), DK50456 (Adipocyte Subcore, J.L.K.), AG46061 (A.K.P.), AG004875 (S.K.), AG048792 (S.K.), AR070241 (J.N.F.), AR070281 (M.M.W.), AG13319 (Y.I. and G.B.H.), AG050886 (D.B.A.), AG043376 (P.D.R., and L.J.N.), AG056278 (P.D.R. and L.J.N.), and AG044376 (L.J.N.); a Glenn/American Federation for Aging Research (AFAR) BIG Award (J.L.K.); the Glenn Foundation (L.J.N.); and the Ted Nash Long Life and Noaber Foundations (J.L.K.). M.X. received the Glenn/AFAR Postdoctoral Fellowship for Translational Research on Aging and an Irene Diamond Fund/AFAR Postdoctoral Transition Award in Aging.
Author information
Authors and Affiliations
Contributions
M.X., T.T., and J.L.K. conceived and designed the study. M.X. performed and analyzed most of the transplanted mouse experiments and human adipose tissue explant experiments. N.G. and T.T. contributed to the human adipose tissue explant experiments. J.N.F., D.G.F., J.L.O., and S.K. contributed to the study of aged mice treated with senolytics. A.K.P. contributed to the bioluminescence studies. M.B.O. and D.J. contributed to ear fibroblast isolation. T.P., M.X., T.T., and C.L.I. performed the survival experiments using senolytics in aged mice. B.M.W., M.M.W., C.M.H., N.K.L., H.C., V.D.G., X.H., S.J.W., K.O.J., M.W., L.G.P.L., G.C.V., P.D.R., L.J.N., and J.D.M. contributed to the mouse studies. R.J.S. contributed to androgen measurement. D.B.A. and K.E. contributed to lifespan analysis. G.B.H. and Y.I. contributed to mouse pathology analysis. M.X. and J.L.K. wrote the manuscript with input from all coauthors. J.L.K., M.X., and T.T. oversaw all experimental design, data analyses, and manuscript preparation.
Corresponding authors
Ethics declarations
Competing interests
J.L.K, T.T., M.X., T.P., N.G., and A.K.P. have a financial interest related to this research. Patents on senolytic drugs (PCT/US2016/041646, filed at the US Patent Office) are held by Mayo Clinic. This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and was conducted in compliance with Mayo Clinic Conflict of Interest policies. None of the other authors has a relevant financial conflict of interest.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15
Supplementary Dataset
Raw Data
Rights and permissions
About this article
Cite this article
Xu, M., Pirtskhalava, T., Farr, J.N. et al. Senolytics improve physical function and increase lifespan in old age. Nat Med 24, 1246–1256 (2018). https://doi.org/10.1038/s41591-018-0092-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-018-0092-9
This article is cited by
-
SenPred: a single-cell RNA sequencing-based machine learning pipeline to classify deeply senescent dermal fibroblast cells for the detection of an in vivo senescent cell burden
Genome Medicine (2025)
-
Senescence as a therapeutic target in cancer and age-related diseases
Nature Reviews Drug Discovery (2025)
-
Enhancing immunity during ageing by targeting interactions within the tissue environment
Nature Reviews Drug Discovery (2025)
-
Lung endothelial cell senescence impairs barrier function and promotes neutrophil adhesion and migration
GeroScience (2025)
-
Cellular Senescence Contributes to Colonic Barrier Integrity Impairment Induced by Toxoplasma gondii Infection
Inflammation (2025)