Abstract
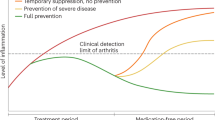
Cure is the aspirational aim for the treatment of all diseases, including chronic inflammatory conditions such as rheumatoid arthritis (RA); however, it has only been during the twenty-first century that remission, let alone cure, has been a regularly achievable target in RA. Little research has been carried out on how to cure RA, and the term ‘cure’ still requires definition for this disease. Even now, achieving a cure seems to be a rare occurrence among individuals with RA. Therefore, this Review is aimed at addressing the obstacles to the achievement of cure in RA. The differences between remission and cure in RA are first defined, followed by a discussion of the underlying factors (referred to as drivers) that prevent the achievement of cure in RA by triggering sustained immune activation and effector cytokine production. Such drivers include adaptive immune system activation, mesenchymal tissue priming and so-called ‘remote’ (non-immune and non-articular) factors. Strategies to target these drivers are also presented, with an emphasis on the development of strategies that could complement currently used cytokine inhibition and thereby improve the likelihood of curing RA.
Key points
-
The term cure indicates the principle absence of disease, whereas remission indicates that disease is still present but is adequately controlled by therapy.
-
Although effector cytokines involved in rheumatoid arthritis (RA) are well-defined and can be effectively neutralized by current treatment modalities, cure is still rare.
-
Underlying disease mechanisms (referred to as drivers) are thought to continuously promote effector cytokine production and thereby prevent cure of RA.
-
Aberrant T cell activation related to autoimmunity, microenvironmental changes associated with local mesenchymal cell priming and so-called ‘remote’ factors such as intestinal barrier function all serve as drivers of RA.
-
To attain cure of RA as an ultimate treatment goal, strategies need to be developed to therapeutically tackle drivers of RA and enable a sustained interruption of the disease process.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Felson, D. T. Defining remission in rheumatoid arthritis. Ann. Rheum. Dis 71 (Suppl. 2), i86–i88 (2012).
McInnes, I. B. & Schett, G. Pathogenetic insights from the treatment of rheumatoid arthritis. Lancet 389, 2328–2337 (2017).
Aga, A. B. et al. Time trends in disease activity, response and remission rates in rheumatoid arthritis during the past decade: results from the NOR-DMARD study 2000-2010. Ann. Rheum. Dis. 74, 381–388 (2015).
Fransen, J., Creemers, M. & Van Riel, P. Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology 43, 1252–1255 (2004).
Smolen, J. S. et al. A simplified disease activity index for rheumatoid arthritis for use in clinical practice. Rheumatology 42, 244–257 (2003).
Aletaha, D. et al. Remission and active disease in rheumatoid arthritis: defining criteria for disease activity states. Arthritis Rheum. 52, 2625–2636 (2005).
Felson, D. T. et al. American College of Rheumatology/European League Against Rheumatism provisional definition of remission in rheumatoid arthritis for clinical trials. Ann. Rheum. Dis. 70, 404–413 (2011).
Hughes, C. D. et al. Intensive therapy and remissions in rheumatoid arthritis: a systematic review. BMC Musculoskelet. Disord. 19, 389 (2018).
Bijlsma, J. W. J. et al. Early rheumatoid arthritis treated with tocilizumab, methotrexate, or their combination (U-Act-Early): a multicentre, randomised, double-blind, double-dummy, strategy trial. Lancet 388, 343–355 (2016).
Schett, G. et al. Tapering biologic and conventional DMARD therapy in rheumatoid arthritis: current evidence and future directions. Ann. Rheum. Dis. 75, 1428–1437 (2016).
Olsen, C. L. et al. Predictors of fatigue in rheumatoid arthritis patients in remission or in a low disease activity state. Arthritis Care Res. 68, 1043–1048 (2016).
Verstappen, M. DMARD-free remission as novel treatment target in rheumatoid arthritis: a systematic literature review of achievability and sustainability. RMD Open 6, e001220 (2020).
Ajeganova, S. & Huizinga, T. Sustained remission in rheumatoid arthritis: latest evidence and clinical considerations. Ther. Adv. Musculoskelet. Dis. 9, 249–262 (2017).
Akdemir, G. et al. Clinical and radiological outcomes of 5-year drug-free remission-steered treatment in patients with early arthritis: IMPROVED study. Ann. Rheum. Dis. 77, 111–118 (2018).
van Gaalen, F. A. et al. Autoantibodies to cyclic citrullinated peptides predict progression to rheumatoid arthritis in patients with undifferentiated arthritis: a prospective cohort study. Arthritis Rheum. 50, 709–715 (2004).
Sokolove, J. et al. Autoantibody epitope spreading in the pre-clinical phase predicts progression to rheumatoid arthritis. PLoS One 7, e35296 (2012).
Simon, D. et al. Micro-structural bone changes are associated with broad-spectrum autoimmunity and predict the onset of rheumatoid arthritis. Arthritis Rheum. https://doi.org/10.1002/art.41229 (2020).
Figueiredo, C. P. et al. Anti-modified protein antibody response pattern influences the risk for disease relapse in patients with rheumatoid arthritis tapering disease modifying anti-rheumatic drugs. Ann. Rheum. Dis. 76, 399–407 (2017).
Stahl, E. A. et al. Genome-wide association study meta-analysis identifies seven new rheumatoid arthritis risk loci. Nat. Genet. 42, 508–514 (2010).
Makrygiannakis, D. et al. Smoking increases peptidylarginine deiminase 2 enzyme expression in human lungs and increases citrullination in BAL cells. Ann. Rheum. Dis. 67, 1488–1492 (2008).
Van den Broek, M. et al. Discontinuation of infliximab and potential predictors of persistent low disease activity in patients with early rheumatoid arthritis and disease activity score-steered therapy: subanalysis of the BeSt study. Ann. Rheum. Dis. 70, 1389–1394 (2011).
Tjin, C. C. et al. Synthesis and biological evaluation of an indazole-based selective protein arginine deiminase 4 (PAD4) inhibitor. ACS Med. Chem. Lett. 9, 1013–1018 (2018).
Burgoyne, C. H. et al. Abnormal T cell differentiation persists in patients with rheumatoid arthritis in clinical remission and predicts relapse. Ann. Rheum. Dis. 67, 750–757 (2008).
Lawson, C. A. et al. Early rheumatoid arthritis is associated with a deficit in the CD4+ CD25high regulatory T cell population in peripheral blood. Rheumatology 45, 1210–1217 (2006).
van Roon, J. A. et al. Numbers of CD25+Foxp3+ T cells that lack the IL-7 receptor are increased intra-articularly and have impaired suppressive function in RA patients. Rheumatology 49, 2084–2089 (2010).
Dominguez-Villar, M. & Hafler, D. A. Regulatory T cells in autoimmune disease. Nat. Immunol. 19, 665–673 (2018).
Komatsu, N. et al. Pathogenic conversion of Foxp3+ T cells into TH17 cells in autoimmune arthritis. Nat. Med. 20, 62–68 (2014).
Nguyen, D. X. et al. Regulatory T cells as a biomarker for response to adalimumab in rheumatoid arthritis. J. Allergy Clin. Immunol. 142, 978–980 (2018).
Buckner, J. H. Mechanisms of impaired regulation by CD4+CD25+FOXP3+ regulatory T cells in human autoimmune diseases. Nat. Rev. Immunol. 10, 849–859 (2010).
Van Amelsfort, J. M. R. et al. Proinflammatory mediator-induced reversal of CD4+CD25+regulatory T cell-mediated suppression in rheumatoid arthritis. Arthritis Rheum. 56, 732–742 (2007).
Flores-Borja, F. et al. Defects in CTLA-4 are associated with abnormal regulatory T cell function in rheumatoid arthritis. Proc. Natl Acad. Sci. USA 105, 19396–19401 (2008).
Chemin, K., Gerstner, C. & Malmström, V. Effector functions of CD4+T cells at the site of local autoimmune inflammation-lessons from rheumatoid arthritis. Front. Immunol. 10, 353 (2019).
Yang, X. Z. et al. Restoring oxidant signaling suppresses proarthritogenic T cell effector functions in rheumatoid arthritis. Sci. Transl Med. 8, 331ra38 (2016).
Rosenzwajg, M. et al. Immunological and clinical effects of low-dose interleukin-2 across 11 autoimmune diseases in a single, open clinical trial. Ann. Rheum. Dis. 78, 209–217 (2019).
Hao, H. et al. Conversion of T follicular helper cells to T follicular regulatory cells through transcriptional regulation in systemic lupus erythematosus. Arthritis Rheumatol. https://doi.org/10.1002/art.41457 (2020).
Crotty, S. T follicular helper cell biology: a decade of discovery and diseases. Immunity 50, 1133–1148 (2019).
Wunderlich, C. et al. Effects of DMARDs on citrullinated peptide autoantibody levels in RA patients — a longitudinal analysis. Semin. Arthritis Rheum. 46, 709–714 (2017).
Rao, D. A. et al. Pathologically expanded peripheral T helper cell subset drives B cells in rheumatoid arthritis. Nature 542, 110–114 (2017).
Scott, I. C. et al. The protective effect of alcohol on developing rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology 52, 856–867 (2013).
Azizov, V. et al. Ethanol consumption inhibits the development of autoimmunity by blocking IL-21 secretion in TFH cells. Nat. Commun. 11, 1998 (2020).
Iwata, S. et al. Activation of Syk in peripheral blood B cells in patients with rheumatoid arthritis: a potential target for abatacept therapy. Arthritis Rheumatol. 67, 63–73 (2015).
Bozec, A. et al. Abatacept blocks anti-citrullinated protein antibody and rheumatoid factor mediated cytokine production in human macrophages in IDO-dependent manner. Arthritis Res. Ther. 20, 24 (2018).
Jansen, D. et al. Conversion to seronegative status after abatacept treatment in patients with early and poor prognostic rheumatoid arthritis is associated with better radiographic outcomes and sustained remission: post hoc analysis of the AGREE study. RMD Open 4, e000564 (2018).
Emery, P. et al. Evaluating drug-free remission with abatacept in early rheumatoid arthritis: results from the phase 3b, multicentre, randomised, active-controlled AVERT study of 24 months, with a 12-month, double-blind treatment period. Ann. Rheum. Dis. 74, 19–26 (2015).
Gerlag, D. M. et al. Effects of B-cell directed therapy on the preclinical stage of rheumatoid arthritis: the PRAIRI study. Ann. Rheum. Dis. 78, 179–185 (2019).
Hartkamp, L. M. et al. Btk inhibition suppresses agonist-induced human macrophage activation and inflammatory gene expression in RA synovial tissue explants. Ann. Rheum. Dis. 74, 1603–1611 (2015).
Clavel, C., Ceccato, L., Anquetil, F., Serre, G. & Sebbag, M. Among human macrophages polarised to different phenotypes, the M-CSF-oriented cells present the highest pro-inflammatory response to the rheumatoid arthritis-specific immune complexes containing ACPA. Ann. Rheum. Dis. 75, 2184–2191 (2016).
Nimmerjahn, F. & Ravetch, J. V. Fcγ receptors as regulators of immune responses. Nat. Rev. Immunol. 8, 34–47 (2008).
Pfeifle, R. et al. Regulation of autoantibody activity by the IL-23-TH17 axis determines the onset of autoimmune disease. Nat. Immunol. 18, 104–113 (2017).
Engdahl, C. et al. Estrogen induces St6gal1 expression and increases IgG sialylation in mice and patients with rheumatoid arthritis: a potential explanation for the increased risk of rheumatoid arthritis in postmenopausal women. Arthritis Res. Ther. 20, 84 (2018).
De Moel, E. C. et al. Baseline autoantibody profile in rheumatoid arthritis is associated with early treatment response but not long-term outcomes. Arthritis Res. Ther. 20, 33 (2018).
Culemann, S. et al. Locally renewing resident synovial macrophages provide a protective barrier for the joint. Nature 572, 670–675 (2019).
Filková, M. et al. Association of circulating miR-223 and miR-16 with disease activity in patients with early rheumatoid arthritis. Ann. Rheum. Dis. 73, 1898–1904 (2014).
Alivernini, S. et al. Distinct synovial tissue macrophage subsets regulate inflammation and remission in rheumatoid arthritis. Nat. Med. 26, 1295–1306 (2020).
Croft, A. P. et al. Distinct fibroblast subsets drive inflammation and damage in arthritis. Nature 570, 246–251 (2019).
Ai, R. et al. Comprehensive epigenetic landscape of rheumatoid arthritis fibroblast-like synoviocytes. Nat. Commun. 9, 1921 (2018).
Karouzakis, E. et al. Epigenome analysis reveals TBX5 as a novel transcription factor involved in the activation of rheumatoid arthritis synovial fibroblasts. J. Immunol. 193, 4945–4951 (2014).
Kurowska-Stolarska, M. et al. MicroRNA-155 as a proinflammatory regulator in clinical and experimental arthritis. Proc. Natl Acad. Sci. USA 108, 11193–11198 (2011).
Karouzakis, E. et al. Analysis of early changes in DNA methylation in synovial fibroblasts of RA patients before diagnosis. Sci. Rep. 8, 7370 (2018).
Ai, R. et al. DNA methylome signature in synoviocytes from patients with early rheumatoid arthritis compared to synoviocytes from patients with longstanding rheumatoid arthritis. Arthritis Rheumatol. 67, 1978–1980 (2015).
Whitaker, J. W. et al. Integrative omics analysis of rheumatoid arthritis identifies non-obvious therapeutic targets. PLoS One 10, e0124254 (2015).
Suraweera, A., O’Byrne, K. J. & Richard, D. J. Combination therapy with histone deacetylase inhibitors (HDACi) for the treatment of cancer: achieving the full therapeutic potential of HDACi. Front. Oncol. 8, 92 (2018).
Frank-Bertoncelj, M. et al. Epigenetically-driven anatomical diversity of synovial fibroblasts guides joint-specific fibroblast functions. Nat. Commun. 8, 14852 (2017).
Zhang, H. J. et al. LncRNA HOTAIR alleviates rheumatoid arthritis by targeting miR-138 and inactivating NF-κB pathway. Int. Immunopharmacol. 50, 283–290 (2017).
Hu, X. et al. Silencing of long non-coding RNA HOTTIP reduces inflammation in rheumatoid arthritis by demethylation of SFRP1. Mol. Ther. Nucleic Acids 19, 468–481 (2020).
Scher, J. U. et al. Expansion of intestinal Prevotella copri correlates with enhanced susceptibility to arthritis. eLife 2, e01202 (2013).
Alpizar-Rodriguez, D. et al. Prevotella copri in individuals at risk for rheumatoid arthritis. Ann. Rheum. Dis. 78, 590–593 (2019).
Tajik, N. et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat. Commun. 11, 1995 (2020).
Edwards, R. R. et al. Enhanced reactivity to pain in patients with rheumatoid arthritis. Arthritis Res. Ther. 11, R61 (2009).
Yılmaz, V., Umay, E., Gündoğdu, İ., Karaahmet, Z. Ö. & Öztürk, A. E. Rheumatoid arthritis: are psychological factors effective in disease flare? Eur. J. Rheumatol. 4, 127–132 (2017).
Evers, A. W. et al. Does stress affect the joints? Daily stressors stress vulnerability, immune and HPA axis activity, and short-term disease and symptom fluctuations in rheumatoid arthritis. Ann. Rheum. Dis. 73, 1683–1688 (2014).
Kolmus, K., Tavernier, J. & Gerlo, S. β2-Adrenergic receptors in immunity and inflammation: stressing NF-κB. Brain Behav. Immun. 4, 297–310 (2015).
del Rey, A. et al. Disrupted brain-immune system-joint communication during experimental arthritis. Arthritis Rheum. 58, 3090–3099 (2008).
Harre, U. et al. Glycosylation of immunoglobulin G determines osteoclast differentiation and bone loss. Nat. Commun. 6, 6651 (2015).
Radbruch, A. et al. Competence and competition: the challenge of becoming a long-lived plasma cell. Nat. Rev. Immunol. 6, 741–750 (2006).
Stanway, J. A. & Isaacs, J. D. Tolerance-inducing medicines in autoimmunity: rheumatology and beyond. Lancet Rheumatol. 9, 565–575 (2020).
Herold, K. C. et al. An anti-CD3 antibody, teplizumab, in relatives at risk for type 1 diabetes. N. Engl. J. Med. 381, 603–613 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02778906 (2020).
Bio Med Central. ISRCTN Registry https://doi.org/10.1186/ISRCTN46017566 (2020).
Iqbal, K. & Isaacs, J. Potential pharmacologic targets for the prevention of rheumatoid arthritis. Clin. Ther. 41, 1312–1322 (2019).
Mrsny, R. J. et al. A key claudin extracellular loop domain is critical for epithelial barrier integrity. Am. J. Pathol. 172, 905–915 (2008).
Pastori, C. et al. The Bromodomain protein BRD4 controls HOTAIR, a long noncoding RNA essential for glioblastoma proliferation. Proc. Natl Acad. Sci. USA 112, 8326–8331 (2015).
Cochran, A. G. et al. Bromodomains: a new target class for drug development. Nat. Rev. Drug Discov. 18, 609–628 (2019).
Lindner, T. et al. Targeting of activated fibroblasts for imaging and therapy. EJNMMI Radiopharm. Chem. 4, 16 (2019).
Jia, W. et al. Histone demethylase JMJD3 regulates fibroblast-like synoviocyte-mediated proliferation and joint destruction in rheumatoid arthritis. FASEB J. 32, 4031–4042 (2018).
Zhou, S. et al. In vivo therapeutic success of microRNA‐155 antagomir in a mouse model of lupus alveolar hemorrhage. Arthritis Rheumatol. 68, 953–964 (2016).
Häger, J. et al. The role of dietary fiber in rheumatoid arthritis patients: a feasibility study. Nutrients 11, E2392 (2019).
Bosmann, M. et al. Anti-inflammatory effects of β2 adrenergic receptor agonists in experimental acute lung injury. FASEB J. 26, 2137–2144 (2012).
Hadi, T. et al. Beta3 adrenergic receptor stimulation in human macrophages inhibits NADPHoxidase activity and induces catalase expression via PPARγ activation. BBA Mol. Cell Res. 1864, 1769–1784 (2017).
Koopman, F. A. et al. Vagus nerve stimulation inhibits cytokine production and attenuates disease severity in rheumatoid arthritis. Proc. Natl Acad. Sci. USA 113, 8284–8289 (2016).
Van der Woude, D., Young, A. & Jayakumar, K. Prevalence of and predictive factors for sustained disease-modifying antirheumatic drug-free remission in rheumatoid arthritis: results from two large early arthritis cohorts. Arthritis Rheum. 60, 2262–2271 (2009).
Baker, K. F. et al. Predicting drug-free remission in rheumatoid arthritis: a prospective interventional cohort study. J. Autoimmun. 105, 102298 (2019).
Jones, G. W. et al. Interleukin-27 inhibits ectopic lymphoid-like structure development in early inflammatory arthritis. J. Exp. Med. 212, 1793–1802 (2015).
Teitsma, X. M. et al. Baseline metabolic profiles of early rheumatoid arthritis patients achieving sustained drug-free remission after initiating treat-to-target tocilizumab, methotrexate, or the combination: insights from systems biology. Arthritis Res. Ther. 20, 230 (2018).
Acknowledgements
The work of G.S. is supported by the German Research Council (DFG: SPP1468-IMMUNOBONE; CRC1181), the German Ministry of Science and Education (project MASCARA), the European Union (ERC Synergy grant 4DnanoSCOPE) and EU/EFPIA Innovative Medicines Initiative 2 (project RTCure). The work of J.D.I. is supported by the Research into Inflammatory Arthritis Centre Versus Arthritis, the National Institute for Health Research Newcastle Biomedical Research Centre, a partnership between Newcastle Hospitals NHS Foundation Trust and Newcastle University, and the EU/EFPIA Innovative Medicines Initiative 2 (project RTCure).
Author information
Authors and Affiliations
Contributions
All authors researched data for the article and provided substantial contributions to discussions of content. G.S. and J.D.I. wrote the article. G.S. and Y.T. reviewed or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Disclaimer
The views expressed are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Peer review information
Nature Reviews Rheumatology thanks H. Xu and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schett, G., Tanaka, Y. & Isaacs, J.D. Why remission is not enough: underlying disease mechanisms in RA that prevent cure. Nat Rev Rheumatol 17, 135–144 (2021). https://doi.org/10.1038/s41584-020-00543-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41584-020-00543-5