Abstract
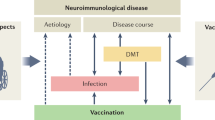
Vaccines protect against many infectious diseases, including some that can directly or indirectly cause nervous system damage. Serious neurological consequences of immunization are typically extremely rare, although they have the potential to jeopardize vaccination programmes, as demonstrated most recently during the COVID-19 pandemic. Neurologists have an important role in identifying safety signals at population and individual patient levels, as well as providing advice on the benefit–risk profile of vaccination in cohorts of patients with diverse neurological conditions. This article reviews the links between vaccination and neurological disease and considers how emerging signals can be evaluated and their mechanistic basis identified. We review examples of neurotropic infections with live attenuated vaccines, as well as neuroimmunological and neurovascular sequelae of other types of vaccines. We emphasize that such risks are typically dwarfed by neurological complications associated with natural infection and discuss how the risks can be further mitigated. The COVID-19 pandemic has highlighted the need to rapidly identify and minimize neurological risks of vaccination, and we review the structures that need to be developed to protect public health against these risks in the future.
Key points
-
Vaccines have a key public health role in protecting populations against infectious diseases, including neurological diseases caused by infections.
-
Serious neurological complications of vaccination are extremely rare, but when they do occur they have the potential to jeopardize vaccination programmes.
-
Live attenuated vaccines, such as the yellow fever and poliomyelitis vaccines, carry a very small risk of neurotropic infections; vaccine-specific and recipient-specific factors can predispose to these complications.
-
Very rare neurological complications of vaccination include neuroimmunological conditions such as Guillain–Barré syndrome, acute disseminated encephalomyelitis and narcolepsy, and neurovascular conditions such as cerebral venous sinus thrombosis and stroke.
-
Apart from live vaccines in immunosuppressed individuals and the yellow fever vaccine in people with myasthenia gravis, vaccination is typically safe in individuals with neurological disease, with strongly positive benefit–risk profiles.
-
Recent advances in data linkage have allowed monitoring of the neurological safety profile of vaccines as they are rolled out, almost in real time, and have enabled these risks to be weighed against the risks of infection in unvaccinated individuals.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
World Health Organization. Child mortality and causes of death. WHO, https://www.who.int/gho/child_health/mortality/mortality_under_five_text/en/ (2020).
Pollard, A. J. & Bijker, E. M. A guide to vaccinology: from basic principles to new developments. Nat. Rev. Immunol. 21, 83–100 (2021).
Cao-Lormeau, V. M. et al. Guillain–Barré syndrome outbreak associated with Zika virus infection in French Polynesia: a case–control study. Lancet 387, 1531–1539 (2016).
Patone, M. et al. Neurological complications after first dose of COVID-19 vaccines and SARS-CoV-2 infection. Nat. Med. 27, 2144–2153 (2021).
& Barwick Eidex, R. Yellow Fever Vaccine Safety Working Group. History of thymoma and yellow fever vaccination.Lancet 364, 936 (2004).
Nath, A. Neurologic complications with vaccines: what we know, what we don’t, and what we should do. Neurology 101, 621–626 (2023).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383, 2603–2615 (2020).
Perry, R. J. et al. Cerebral venous thrombosis after vaccination against COVID-19 in the UK: a multicentre cohort study. Lancet 398, 1147–1156 (2021).
Godlee, F., Smith, J. & Marcovitch, H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 342, c7452 (2011).
Waugh, C. J., Willocks, L. J., Templeton, K. & Stevenson, J. Recurrent outbreaks of mumps in Lothian and the impact of waning immunity. Epidemiol. Infect. 148, e131 (2020).
Baker, J. P. The pertussis vaccine controversy in Great Britain, 1974–1986. Vaccine 21, 4003–4010 (2003).
Larson, H. J., Gakidou, E. & Murray, C. J. L. The vaccine-hesitant moment. N. Engl. J. Med. 387, 58–65 (2022).
Knipe, D. M., Levy, O., Fitzgerald, K. A. & Muhlberger, E. Ensuring vaccine safety. Science 370, 1274–1275 (2020).
Folegatti, P. M. et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet 396, 467–478 (2020).
Ramasamy, M. N. et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 396, 1979–1993 (2021).
Jackson, L. A. et al. An mRNA vaccine against SARS-CoV-2 — preliminary report. N. Engl. J. Med. 383, 1920–1931 (2020).
Voysey, M. et al. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet 397, 99–111 (2021).
Scully, M. et al. Pathologic antibodies to platelet factor 4 after ChAdOx1 nCoV-19 vaccination. N. Engl. J. Med. 384, 2202–2211 (2021).
Candore, G. et al. Comparison of statistical signal detection methods within and across spontaneous reporting databases. Drug. Saf. 38, 577–587 (2015).
Lazarus, R. et al. Safety and immunogenicity of concomitant administration of COVID-19 vaccines (ChAdOx1 or BNT162b2) with seasonal influenza vaccines in adults in the UK (ComFluCOV): a multicentre, randomised, controlled, phase 4 trial. Lancet 398, 2277–2287 (2021).
Verani, J. R. et al. Case–control vaccine effectiveness studies: preparation, design, and enrollment of cases and controls. Vaccine 35, 3295–3302 (2017).
Farrington, P. The self-controlled case series method and covid-19. BMJ 377, o625 (2022).
Minor, P. D. Live attenuated vaccines: historical successes and current challenges. Virology 479–480, 379–392 (2015).
Norrby, E. Yellow fever and Max Theiler: the only Nobel Prize for a virus vaccine. J. Exp. Med. 204, 2779–2784 (2007).
Baicus, A. History of polio vaccination. World J. Virol. 1, 108–114 (2012).
Mangtani, P. et al. Protection by BCG vaccine against tuberculosis: a systematic review of randomized controlled trials. Clin. Infect. Dis. 58, 470–480 (2014).
Poyhonen, L., Bustamante, J., Casanova, J. L., Jouanguy, E. & Zhang, Q. Life-threatening infections due to live-attenuated vaccines: early manifestations of inborn errors of immunity. J. Clin. Immunol. 39, 376–390 (2019).
Reno, E. et al. Prevention of yellow fever in travellers: an update. Lancet Infect. Dis. 20, e129–e137 (2020).
Garske, T. et al. Yellow Fever in Africa: estimating the burden of disease and impact of mass vaccination from outbreak and serological data. PLoS Med. 11, e1001638 (2014).
Gianchecchi, E., Cianchi, V., Torelli, A. & Montomoli, E. Yellow fever: origin, epidemiology, preventive strategies and future prospects. Vaccines 10, 372 (2022).
Staples, J. E., Gershman, M., Fischer, M. & Centers for Disease Control and Prevention. Yellow fever vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 59, 1–27 (2010).
de Abreu, A. J. L., Cavalcante, J. R., de Araujo Lagos, L. W., Caetano, R. & Braga, J. U. A systematic review and a meta-analysis of the yellow fever vaccine in the elderly population. Vaccines 10, 711 (2022).
Kitchener, S. Viscerotropic and neurotropic disease following vaccination with the 17D yellow fever vaccine, ARILVAX®. Vaccine 22, 2103–2105 (2004).
McMahon, A. W. et al. Neurologic disease associated with 17D-204 yellow fever vaccination: a report of 15 cases. Vaccine 25, 1727–1734 (2007).
Cohen, M. et al. Case report: yellow fever vaccine-associated neurotropic disease and associated MRI, EEG, and CSF findings. Front. Neurol. 12, 779014 (2021).
Kengsakul, K., Sathirapongsasuti, K. & Punyagupta, S. Fatal myeloencephalitis following yellow fever vaccination in a case with HIV infection. J. Med. Assoc. Thai. 85, 131–134 (2002).
Ribeiro, A. F. et al. Neurologic disease after yellow fever vaccination, Sao Paulo, Brazil, 2017–2018. Emerg. Infect. Dis. 27, 1577–1587 (2021).
Guedes, B. F. et al. Potential autoimmune encephalitis following yellow fever vaccination: a report of three cases. J. Neuroimmunol. 355, 577548 (2021).
Frierson, J. G. The yellow fever vaccine: a history. Yale J. Biol. Med. 83, 77–85 (2010).
DeSilva, M. et al. Notes from the field: fatal yellow fever vaccine-associated viscerotropic disease — Oregon, September 2014. MMWR Morb. Mortal. Wkly Rep. 64, 279–281 (2015).
Wolfe, G. I., Kaminski, H. J. & Cutter, G. R. Randomized trial of thymectomy in myasthenia gravis. N. Engl. J. Med. 375, 2006–2007 (2016).
Bastard, P. et al. Auto-antibodies to type I IFNs can underlie adverse reactions to yellow fever live attenuated vaccine. J. Exp. Med. 218, e20202486 (2021).
History of Polio. Global Eradication Polio Initiative. https://polioeradication.org/polio-today/history-of-polio/ (2019).
Cooper, L. V. et al. Risk factors for the spread of vaccine-derived type 2 polioviruses after global withdrawal of trivalent oral poliovirus vaccine and the effects of outbreak responses with monovalent vaccine: a retrospective analysis of surveillance data for 51 countries in Africa. Lancet Infect. Dis. 22, 284–294 (2022).
Hill, M., Bandyopadhyay, A. S. & Pollard, A. J. Emergence of vaccine-derived poliovirus in high-income settings in the absence of oral polio vaccine use. Lancet 400, 713–715 (2022).
Macklin, G. R. et al. Enabling accelerated vaccine roll-out for Public Health Emergencies of International Concern (PHEICs): novel oral polio vaccine type 2 (nOPV2) experience. Vaccine 41, A122–A127 (2023).
Platt, L. R., Estivariz, C. F. & Sutter, R. W. Vaccine-associated paralytic poliomyelitis: a review of the epidemiology and estimation of the global burden. J. Infect. Dis. 210, S380–S389 (2014).
Shaghaghi, M. et al. Combined immunodeficiency presenting with vaccine-associated paralytic poliomyelitis: a case report and narrative review of literature. Immunol. Invest. 43, 292–298 (2014).
Jafari, H. et al. Polio eradication. Efficacy of inactivated poliovirus vaccine in India. Science 345, 922–925 (2014).
Yeh, M. T. et al. Engineering the live-attenuated polio vaccine to prevent reversion to virulence. Cell Host Microbe 27, 736–751.e8 (2020).
Zaman, K. et al. Evaluation of the safety, immunogenicity, and faecal shedding of novel oral polio vaccine type 2 in healthy newborn infants in Bangladesh: a randomised, controlled, phase 2 clinical trial. Lancet 401, 131–139 (2023).
Wahid, R. et al. Assessment of genetic changes and neurovirulence of shed Sabin and novel type 2 oral polio vaccine viruses. npj Vaccines 6, 94 (2021).
Hubschen, J. M., Gouandjika-Vasilache, I. & Dina, J. Measles. Lancet 399, 678–690 (2022).
Bellini, W. J. et al. Subacute sclerosing panencephalitis: more cases of this fatal disease are prevented by measles immunization than was previously recognized. J. Infect. Dis. 192, 1686–1693 (2005).
Ferren, M., Horvat, B. & Mathieu, C. Measles encephalitis: towards new therapeutics. Viruses 11, 1017 (2019).
Costales, C. et al. Vaccine-associated measles encephalitis in immunocompromised child, California, USA. Emerg. Infect. Dis. 28, 906–908 (2022).
Moens, L. et al. A novel kindred with inherited STAT2 deficiency and severe viral illness. J. Allergy Clin. Immunol. 139, 1995–1997.e9 (2017).
van den Berg, B. et al. Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat. Rev. Neurol. 10, 469–482 (2014).
Leonhard, S. E. et al. An international perspective on preceding infections in Guillain–Barré syndrome: the IGOS-1000 cohort. Neurology 99, e1299–e1313 (2022).
Pritchard, J. & Hughes, R. A. Guillain–Barré syndrome. Lancet 363, 2186–2188 (2004).
Drenthen, J. et al. Guillain–Barré syndrome subtypes related to Campylobacter infection. J. Neurol. Neurosurg. Psychiatry 82, 300–305 (2011).
Hurwitz, E. S., Schonberger, L. B., Nelson, D. B. & Holman, R. C. Guillain–Barré syndrome and the 1978–1979 influenza vaccine. N. Engl. J. Med. 304, 1557–1561 (1981).
Kurland, L. T., Wiederholt, W. C., Kirkpatrick, J. W., Potter, H. G. & Armstrong, P. Swine influenza vaccine and Guillain–Barré syndrome. Epidemic or artifact? Arch. Neurol. 42, 1089–1090 (1985).
Martin Arias, L. H., Sanz, R., Sainz, M., Treceno, C. & Carvajal, A. Guillain–Barré syndrome and influenza vaccines: a meta-analysis. Vaccine 33, 3773–3778 (2015).
Boender, T. S., Bartmeyer, B., Coole, L., Wichmann, O. & Harder, T. Risk of Guillain–Barré syndrome after vaccination against human papillomavirus: a systematic review and meta-analysis, 1 January 2000 to 4 April 2020. Eur. Surveill. 27, 2001619 (2022).
Goud, R. et al. Risk of Guillain–Barré syndrome following recombinant zoster vaccine in Medicare beneficiaries. JAMA Intern. Med. 181, 1623–1630 (2021).
Melgar, M. et al. Use of respiratory syncytial virus vaccines in older adults: recommendations of the Advisory Committee on Immunization Practices — United States, 2023. Am. J. Transpl. 23, 1631–1640 (2023).
Keh, R. Y. S. et al. COVID-19 vaccination and Guillain–Barré syndrome: analyses using the National Immunoglobulin Database. Brain 146, 739–748 (2023).
Anjum, Z. et al. Guillain–Barré syndrome after mRNA-1273 (Moderna) COVID-19 vaccination: a case report. Clin. Case Rep. 10, e05733 (2022).
Abara, W. E. et al. Reports of Guillain–Barré syndrome after COVID-19 vaccination in the United States. JAMA Netw. Open 6, e2253845 (2023).
McNeil, M. M. et al. Adverse events following adenovirus type 4 and type 7 vaccine, live, oral in the Vaccine Adverse Event Reporting System (VAERS), United States, October 2011–July 2018. Vaccine 37, 6760–6767 (2019).
Jacobs, B. C. et al. The spectrum of antecedent infections in Guillain–Barré syndrome: a case–control study. Neurology 51, 1110–1115 (1998).
Allen, C. M. et al. Guillain–Barré syndrome variant occurring after SARS-CoV-2 vaccination. Ann. Neurol. 90, 315–318 (2021).
Maramattom, B. V. et al. Guillain–Barré syndrome following ChAdOx1-S/nCoV-19 vaccine. Ann. Neurol. 90, 312–314 (2021).
Shoamanesh, A. & Traboulsee, A. Acute disseminated encephalomyelitis following influenza vaccination. Vaccine 29, 8182–8185 (2011).
Baxter, R. et al. Acute demyelinating events following vaccines: a case-centered analysis. Clin. Infect. Dis. 63, 1456–1462 (2016).
Constantinescu, C. S., Farooqi, N., O’Brien, K. & Gran, B. Experimental autoimmune encephalomyelitis (EAE) as a model for multiple sclerosis (MS). Br. J. Pharmacol. 164, 1079–1106 (2011).
Plesner, A. M., Arlien-Soborg, P. & Herning, M. Neurological complications and Japanese encephalitis vaccination. Lancet 348, 202–203 (1996).
Ohtaki, E., Matsuishi, T., Hirano, Y. & Maekawa, K. Acute disseminated encephalomyelitis after treatment with Japanese B encephalitis vaccine (Nakayama-Yoken and Beijing strains). J. Neurol. Neurosurg. Psychiatry 59, 316–317 (1995).
Francis, A., Palace, J. & Fugger, L. MOG antibody-associated disease after vaccination with ChAdOx1 nCoV-19. Lancet Neurol. 21, 217–218 (2022).
Francis, A. G. et al. Acute inflammatory diseases of the central nervous system after SARS-CoV-2 vaccination. Neurol. Neuroimmunol. Neuroinflamm. 10, e200063 (2023).
Rinaldi, V., Bellucci, G., Romano, A., Bozzao, A. & Salvetti, M. ADEM after ChAdOx1 nCoV-19 vaccine: a case report. Mult. Scler. 28, 1151–1154 (2022).
Copland, E. Safety outcomes following COVID-19 vaccination and infection in 5.1 million children in England. Nat. Commun. 15, 3822 (2024).
Miller, E. et al. Risk of narcolepsy in children and young people receiving AS03 adjuvanted pandemic A/H1N1 2009 influenza vaccine: retrospective analysis. BMJ 346, f794 (2013).
Kornum, B. R. et al. Narcolepsy. Nat. Rev. Dis. Prim. 3, 16100 (2017).
Nohynek, H. et al. AS03 adjuvanted AH1N1 vaccine associated with an abrupt increase in the incidence of childhood narcolepsy in Finland. PLoS ONE 7, e33536 (2012).
Ahmed, S. S. et al. Antibodies to influenza nucleoprotein cross-react with human hypocretin receptor 2. Sci. Transl. Med. 7, 294ra105 (2015).
Hallberg, P. et al. Pandemrix-induced narcolepsy is associated with genes related to immunity and neuronal survival. eBioMedicine 40, 595–604 (2019).
Bomfim, I. L. et al. The immunogenetics of narcolepsy associated with A(H1N1)pdm09 vaccination (Pandemrix) supports a potent gene–environment interaction. Genes Immun. 18, 75–81 (2017).
Hippisley-Cox, J. et al. Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ 374, n1931 (2021).
Malas, M. B. et al. Thromboembolism risk of COVID-19 is high and associated with a higher risk of mortality: a systematic review and meta-analysis. eClinicalMedicine 29, 100639 (2020).
Schultz, N. H. et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N. Engl. J. Med. 384, 2124–2130 (2021).
Kelton, J. G., Arnold, D. M. & Nazy, I. Lessons from vaccine-induced immune thrombotic thrombocytopenia. Nat. Rev. Immunol. 21, 753–755 (2021).
Kanack, A. J. et al. Monoclonal and oligoclonal anti-platelet factor 4 antibodies mediate VITT. Blood 140, 73–77 (2022).
Pavord, S. et al. Vaccine induced immune thrombocytopenia and thrombosis: summary of NICE guidance. BMJ 375, n2195 (2021).
Kanack, A. J. et al. Persistence of Ad26.COV2.S-associated vaccine-induced immune thrombotic thrombocytopenia (VITT) and specific detection of VITT antibodies. Am. J. Hematol. 97, 519–526 (2022).
Marks, P. Joint CDC and FDA Statement on Johnson & Johnson COVID-19 Vaccine. FDA https://www.fda.gov/news-events/press-announcements/joint-cdc-and-fda-statement-johnson-johnson-covid-19-vaccine (2021).
Vaxzevria (previously COVID-19 Vaccine AstraZeneca). European Medicines Agency https://www.ema.europa.eu/en/medicines/human/EPAR/vaxzevria-previously-covid-19-vaccine-astrazeneca (2024).
Sahin, U., Kariko, K. & Tureci, O. mRNA-based therapeutics — developing a new class of drugs. Nat. Rev. Drug Discov. 13, 759–780 (2014).
Martinon, F. et al. Induction of virus-specific cytotoxic T lymphocytes in vivo by liposome-entrapped mRNA. Eur. J. Immunol. 23, 1719–1722 (1993).
Chaudhary, N., Weissman, D. & Whitehead, K. A. mRNA vaccines for infectious diseases: principles, delivery and clinical translation. Nat. Rev. Drug Discov. 20, 817–838 (2021).
Patone, M. et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat. Med. 28, 410–422 (2022).
Patone, M. et al. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation 146, 743–754 (2022).
Ihle-Hansen, H. et al. Stroke after SARS-CoV-2 mRNA vaccine: a nationwide registry study. Stroke 54, e190–e193 (2023).
Stefanou, M. I. et al. Acute arterial ischemic stroke following COVID-19 vaccination: a systematic review and meta-analysis. Neurology 99, e1465–e1474 (2022).
Lu, Y. et al. Stroke risk after COVID-19 bivalent vaccination among US older adults. JAMA 331, 938–950 (2024).
Rakusa, M. et al. COVID-19 vaccination hesitancy among people with chronic neurological disorders: a position paper. Eur. J. Neurol. 29, 2163–2172 (2022).
Farez, M. F. & Correale, J. Yellow fever vaccination and increased relapse rate in travelers with multiple sclerosis. Arch. Neurol. 68, 1267–1271 (2011).
Huttner, A. et al. Risk of MS relapse after yellow fever vaccination: a self-controlled case series. Neurol. Neuroimmunol. Neuroinflamm. 7, e726 (2020).
Papeix, C. et al. Multiple sclerosis: is there a risk of worsening after yellow fever vaccination? Mult. Scler. 27, 2280–2283 (2021).
Labani, A. et al. Incidence of multiple sclerosis relapses and pseudo-relapses following COVID-19 vaccination. Mult. Scler. Relat. Disord. 77, 104865 (2023).
Langer-Gould, A. et al. Vaccines and the risk of multiple sclerosis and other central nervous system demyelinating diseases. JAMA Neurol. 71, 1506–1513 (2014).
Frahm, N. et al. SARS-CoV-2 vaccination in patients with multiple sclerosis in Germany and the United Kingdom: gender-specific results from a longitudinal observational study. Lancet Reg. Health Eur. 22, 100502 (2022).
Willison, A. G. et al. SARS-CoV-2 vaccination and neuroimmunological disease: a review. JAMA Neurol. 81, 179–186 (2024).
Wu, X., Wang, L., Shen, L. & Tang, K. Response of COVID-19 vaccination in multiple sclerosis patients following disease-modifying therapies: a meta-analysis. eBioMedicine 81, 104102 (2022).
Winkelmann, A., Loebermann, M., Barnett, M., Hartung, H. P. & Zettl, U. K. Vaccination and immunotherapies in neuroimmunological diseases. Nat. Rev. Neurol. 18, 289–306 (2022).
Baxter, R. et al. Recurrent Guillain–Barré syndrome following vaccination. Clin. Infect. Dis. 54, 800–804 (2012).
Baars, A. E. et al. SARS-CoV-2 vaccination safety in Guillain–Barré syndrome, chronic inflammatory demyelinating polyneuropathy, and multifocal motor neuropathy. Neurology 100, e182–e191 (2023).
Grohskopf, L. A. et al. Prevention and control of seasonal influenza with vaccines: recommendations of the advisory committee on immunization practices — United States, 2022–23 Influenza Season. MMWR Recomm. Rep. 71, 1–28 (2022).
Zinman, L. et al. Safety of influenza vaccination in patients with myasthenia gravis: a population-based study. Muscle Nerve 40, 947–951 (2009).
Sansone, G. & Bonifati, D. M. Vaccines and myasthenia gravis: a comprehensive review and retrospective study of SARS-CoV-2 vaccination in a large cohort of myasthenic patients. J. Neurol. 269, 3965–3981 (2022).
Pang, E. W., Lawn, N. D., Chan, J., Lee, J. & Dunne, J. W. COVID-19 vaccination-related exacerbation of seizures in persons with epilepsy. Epilepsy Behav. 138, 109024 (2023).
Clayton, L. M. et al. The impact of SARS-CoV-2 vaccination in Dravet syndrome: a UK survey. Epilepsy Behav. 124, 108258 (2021).
von Wrede, R., Pukropski, J., Moskau-Hartmann, S., Surges, R. & Baumgartner, T. COVID-19 vaccination in patients with epilepsy: first experiences in a German tertiary epilepsy center. Epilepsy Behav. 122, 108160 (2021).
Edwards, K. M. & Griffin, M. R. Postmarketing vaccine safety assessments: important work in progress. JAMA 331, 915–917 (2024).
Herati, R. S. & Wherry, E. J. What is the predictive value of animal models for vaccine efficacy in humans? Consideration of strategies to improve the value of animal models. Cold Spring Harb. Perspect. Biol. 10, a031583 (2018).
Gonsalvez, D. G. et al. A simple approach to induce experimental autoimmune neuritis in C57BL/6 mice for functional and neuropathological assessments. J. Vis. Exp. 129, 56455 (2017).
Libbey, J. E. & Fujinami, R. S. Experimental autoimmune encephalomyelitis as a testing paradigm for adjuvants and vaccines. Vaccine 29, 3356–3362 (2011).
Vuorela, A. et al. Enhanced influenza A H1N1 T cell epitope recognition and cross-reactivity to protein-O-mannosyltransferase 1 in Pandemrix-associated narcolepsy type 1. Nat. Commun. 12, 2283 (2021).
Top, K. A. et al. Advancing the science of vaccine safety during the coronavirus disease 2019 (COVID-19) pandemic and beyond: launching an international network of special immunization services. Clin. Infect. Dis. 75, S11–S17 (2022).
Collection: Immunisation Against Infectious Disease. GOV.UK. https://www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book (2024).
Wei, J. et al. Antibody responses to SARS-CoV-2 vaccines in 45,965 adults from the general population of the United Kingdom. Nat. Microbiol. 6, 1140–1149 (2021).
Acknowledgements
D.P.J.H. is supported by a Wellcome Trust Senior Research Fellowship (215621/Z/19/Z) and the Medical Research Foundation, and his research is supported by the UK Dementia Research Institute (Medical Research Council). L.H. is supported by the National Institute for Health and Care Research (NIHR) Oxford Health Biomedical Research Centre, UK. L.T. is supported by the NIHR Health Protection Research Unit (HPRU) in Emerging and Zoonotic Infections (NIHR200907) at the University of Liverpool, UK in partnership with the UK Health Security Agency (UK HSA), in collaboration with Liverpool School of Tropical Medicine and the University of Oxford. L.T. is based at the University of Liverpool. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, the Department of Health or the UK HSA.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of the article.
Corresponding author
Ethics declarations
Competing interests
L.T. has received consulting fees from the UK Medicines and Healthcare products Regulatory Agency (MHRA); consulting fees from AstraZeneca and Synairgen, paid to the University of Liverpool, UK; speakers’ fees from Eisai; and support for conference attendance from AstraZeneca. L.T. was a member of the MHRA yellow fever vaccine safety expert working group. D.P.J.H. is a Commissioner for the UK Government Commission for Human Medicines. L.H. and M.N.R. declare no competing interests.
Peer review
Peer review information
Nature Reviews Neurology thanks A. Nath and S. Meuth for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Adverse Events Following Immunization (AEFI): https://www.who.int/publications/m/item/reporting-form-aefi
Vaccine Adverse Event Reporting System (VAERS): https://vaers.hhs.gov/
Vaccine Damage Payment Scheme: https://www.gov.uk/vaccine-damage-payment
Yellow Card: https://yellowcard.mhra.gov.uk/
Glossary
- Bayesian analysis
-
Modelling method that incorporates prior data to infer the probability of a given hypothesis.
- Embryonated chicken eggs
-
Fertilized chicken eggs that have been allowed to develop into embryos over 5–12 days and are used for viral cell culture.
- Seed lot system
-
A manufacturing technique in which batches of vaccine are made using a standardized master cell and/or virus stock.
- Time-invariant confounding
-
A confounder that remains constant across the duration of the study period (for example, sex or ethnicity).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Handunnetthi, L., Ramasamy, M.N., Turtle, L. et al. Identifying and reducing risks of neurological complications associated with vaccination. Nat Rev Neurol 20, 541–554 (2024). https://doi.org/10.1038/s41582-024-01000-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41582-024-01000-7