Abstract
Endocannabinoid signaling is implicated in an array of psychopathologies ranging from anxiety to psychosis and addiction. In recent years, radiotracers targeting the endocannabinoid system have been used in positron emission tomography (PET) studies to determine whether individuals with psychiatric disorders display altered endocannabinoid signaling. We comprehensively reviewed PET studies examining differences in endocannabinoid signaling between individuals with psychiatric illness and healthy controls. Published studies evaluated individuals with five psychiatric disorders: cannabis use disorder, alcohol use disorder, schizophrenia, post-traumatic stress disorder, and eating disorders. Most studies employed radiotracers targeting cannabinoid receptor 1 (CB1). Cannabis users consistently demonstrated decreased CB1 binding compared to controls, with normalization following short periods of abstinence. Findings in those with alcohol use disorder and schizophrenia were less consistent, with some studies demonstrating increased CB1 binding and others demonstrating decreased CB1 binding. Evidence of aberrant CB1 binding was also found in individuals with anorexia nervosa and post-traumatic stress disorder, but limited data have been published to date. Thus, existing evidence suggests that alterations in endocannabinoid signaling are present in a range of psychiatric disorders. Although recent efforts have largely focused on evaluating CB1 binding, the synthesis of new radiotracers targeting enzymes involved in endocannabinoid degradation, such as fatty acid amide hydrolase, will allow for other facets of endocannabinoid signaling to be evaluated in future studies.
Similar content being viewed by others
Introduction
The endocannabinoid system is one of the most widely distributed neurotransmitter systems in the human brain [1, 2]. Cannabinoid receptor 1 (CB1), the main receptor involved in central endocannabinoid signaling, modulates synaptic circuits that play a prominent role in psychopathology. For example, in the basolateral amygdala, CB1 activation facilitates the extinction of aversive memories by inducing long-term depression of GABAergic synapses [3]. In the medial prefrontal cortex, CB1 receptors regulate stress reactivity by terminating stress-induced corticosterone release [4]. In the ventral striatum and midbrain, CB1 activation is thought to be responsible for cannabis’ rewarding properties [5], and blockade of the CB1 receptor leads to reductions in self-administration of cannabis and other drugs of abuse [6], possibly by decreasing drug-induced dopamine release [7, 8]. Given the diverse role of endocannabinoid signaling in these and other brain regions, the endocannabinoid system had been proposed as a pharmacological target for a range of psychiatric disorders, including mood disorders [9], anxiety disorders [10], and substance use disorders [11]. However, there is limited knowledge as to whether these disorders are associated with altered endocannabinoid signaling in humans.
To better determine whether psychiatric disorders are associated with endocannabinoid signaling abnormalities in the brain, we comprehensively reviewed human positron emission tomography (PET) studies employing radiotracers targeting the endocannabinoid system. We specifically selected studies that compared individuals with psychiatric disorders to healthy controls. If differences were present, we sought to determine whether these differences were global or regional. A literature search found relevant studies for five psychiatric disorders: cannabis use disorder, alcohol use disorder, schizophrenia, post-traumatic stress disorder (PTSD), and eating disorders (for details regarding the search strategy, see Supplemental methods). Studies investigating patients with neurological or neurodegenerative diseases, including temporal lobe epilepsy [12], migraine [13], Alzheimer’s disease [14], and Parkinson’s disease [15], were excluded from our review. Important details from each study, including the sex distribution of the sample, sample size, and method used to estimate receptor availability, are displayed in the accompanying tables.
Radiotracers targeting the endocannabinoid system
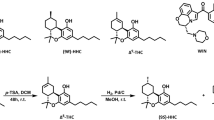
Three radiotracers have been used to probe the CB1 receptor in human PET studies of psychiatric disorders: [18F]MK-9470, [18F]FMPEP-d2, and [11C]OMAR (Table 1) [16, 17]. These tracers are used to provide an index of CB1 receptor availability, though PET cannot generally distinguish whether altered radiotracer binding is due to changes in receptor density, occupancy, or affinity [18]. Although binding potential (BPND) is commonly used as a measure of receptor availability in PET studies, its estimation often requires a reference region devoid of receptors [18]. For CB1, there is no suitable reference region; therefore, researchers have used other estimates of receptor binding, such as volume of distribution (VT) and modified standardized uptake values (mSUV). Unfortunately, these estimates can be affected by nonspecific binding (i.e., binding of the radioligand to molecules other than CB1), which represents a significant methodological limitation. Other radiotracer-related issues may also confound results. For example, radioactivity has been shown to accumulate in the skull during [18F]FMPEP-d2 scans due to in vivo defluorination and bone uptake of 18F-fluoride ions. This may, in turn, affect measurements in the adjacent cortex [19]. Despite these limitations, PET imaging using all three radiotracers has shown good test–retest reliability [19,20,21]. Furthermore, in healthy subjects, higher CB1 binding has been found in the basal ganglia, cerebral cortex, and hippocampus relative to the pons and white matter [22, 23], which is in accordance with the distribution of CB1 receptors observed in postmortem studies [2].
Endocannabinoid signaling is primarily terminated by the enzymes fatty acid amide hydrolase (FAAH) and monoacylglycerol lipase (MAGL), which metabolize the endogenous cannabinoids anandamide and 2-arachidonoylglycerol (2-AG), respectively. [11C]CURB is the only radiotracer that has been used to probe FAAH activity in human PET studies of individuals with psychiatric disorders (Table 1). [11C]CURB is an irreversible FAAH inhibitor that shows high brain uptake in rodents, with highest uptake levels in the cortex and cerebellum [24]. As with radiotracers targeting CB1, imaging with [11C]CURB has been demonstrated to have good test–retest reliability [25]. There are several lines of evidence suggesting that [11C]CURB provides an index of FAAH activity. First, individuals with the FAAH C385A polymorphism (rs324420), which reduces FAAH expression and activity [26, 27], have reduced [11C]CURB binding [28]. Second, oral administration of a FAAH inhibitor greatly reduces [11C]CURB binding in humans [25]. At the present time, no radiotracers targeting MAGL have been used in human studies.
PET studies of substance use disorders
Cannabis use disorder
Cannabis contains multiple compounds that bind directly to central CB1 receptors; therefore, cannabis users are an ideal sample for PET studies of the endocannabinoid system. The endocannabinoid system is also a promising target for the treatment of cannabis use disorder. Agonists of the CB1 receptor, such as dronabinol, nabilone, and nabiximols, have been used to successfully treat cannabis withdrawal [29,30,31,32]. Whether CB1 agonists or antagonists are useful in relapse prevention is less clear. Clinical trials testing dronabinol and nabiximols for cannabis use disorder have failed to show increased abstinence rates [33,34,35]. There is some evidence from the non-human primate literature that CB1 antagonists could be useful for this indication [36, 37], although these compounds have never been tested for relapse prevention in humans. Given the lack of effective pharmacotherapies for this disorder [38], a better understanding of cannnabis’ effect on central endocannabinoid signaling could help guide the development of novel pharmacological treatment strategies.
Human PET studies have found that chronic cannabis use is associated with decreased CB1 availability (Table 2) [39,40,41]. The preponderance of evidence indicates that cannabis-induced reductions in CB1 availability are global [40, 41], although one study found that reductions were mostly restricted to cortical regions [39]. These changes may be responsible for the symptoms of cannabis withdrawal, as CB1 availability on day 2 of abstinence was negatively correlated with withdrawal severity (Spearman’s Rho = −0.67) [40]. CB1 availability appears to normalize rapidly after a period of abstinence [39, 40], indicating that cannabis-induced alterations in endocannabinoid signaling may be reversible. However, these findings require replication in female samples, as there were only two female cannabis-using subjects across all three studies.
The effect of chronic cannabis use on FAAH binding has also been examined in humans [42]. In accordance with the CB1 receptor findings, chronic cannabis users demonstrated global reductions in FAAH binding. Strong negative correlations were found between FAAH binding and delta-9-tetrahydrocannabinol (Δ9-THC) metabolite concentrations in blood and urine, suggesting that these reductions are directly related to Δ9-THC exposure. The observed findings were contrary to the authors’ hypothesis; FAAH was expected to be upregulated to compensate for high levels of exogenous CB1 stimulation. However, chronic Δ9-THC use may also lead to reduced anandamide synthesis which, in turn, could lead to decreased FAAH synthesis or activity. Indeed, there is evidence that cerebrospinal fluid levels of anandamide are reduced following heavy cannabis exposure [43], but whether these reductions are secondary to decreased anandamide synthesis or other mechanisms remains unclear.
Alcohol use disorder
There is evidence that altered endocannabinoid signaling affects human alcohol consumption. Individuals of European ancestry with the FAAH C385A polymorphism have a higher probability of being diagnosed with alcohol dependence [44]. Furthermore, dependent individuals with this polymorphism consume more alcohol, have higher Alcohol Use Disorders Identification Test (AUDIT) scores, and are more likely to meet criteria for severe dependence [44]. This accords with extensive rodent literature showing that increasing CB1 signaling induces alcohol consumption [45], whereas CB1 blockade reduces alcohol intake [46,47,48]. On the other hand, clinical studies testing rimonabant, an inverse agonist of the CB1 receptor, have not shown any efficacy in reducing alcohol consumption or relapse [49, 50]. Human PET studies could help clarify whether individuals at risk for alcoholism have aberrant endocannabinoid signaling and could also prove useful to elucidate whether acute and chronic consumption alter endocannabinoid metabolism and CB1 receptor density.
Three PET studies have examined whether alcohol dependence is associated with CB1 availability in males (Table 2). A small preliminary study comparing alcohol-dependent males to healthy male controls found increased CB1 receptor availability in dependent individuals [51]. Subsequent larger studies have not supported this finding. These studies found global reductions in CB1 availability in alcohol-dependent individuals versus controls, which persisted after a period of abstinence [52, 53]. The second of these studies also tested the effects of acute intravenous ethanol administration on CB1 availability in healthy males [53]. Interestingly, as opposed to the decreased CB1 availability observed with chronic ethanol use, acute administration was associated with global increases in CB1 availability. The reason that acute and chronic ethanol consumption appear to have opposing effects remains to be determined. Follow-up studies should also evaluate whether alcohol use affects endocannabinoid signaling in females.
PET studies of other psychiatric disorders
Schizophrenia
The endocannabinoid system may be involved in the etiology of psychotic disorders. For example, there is evidence that cannabis use has dose-dependent psychotogenic effects, as both higher levels of cannabis use [54] and use of cannabis with higher concentrations of Δ9-THC [55] are associated with a greater likelihood of developing psychosis. In individuals with schizophrenia, cannabis abuse has been associated with relapse of psychotic symptoms [56] and higher rates of hospitalization [57]. The link between Δ9-THC use and psychosis has also been demonstrated more directly in human laboratory studies. Intravenous administration of Δ9-THC in healthy subjects dose-dependently increases both psychotic symptoms [58] and an electroencephalography measure of cortical noise associated with psychosis [59]. Interestingly, there is growing evidence that cannabidiol, a negative allosteric modulator of the CB1 receptor [60], reduces psychotic symptoms in patients with schizophrenia, both as a monotherapy [61] and as an adjunctive treatment [62]. On the other hand, a clinical trial found that blockade of CB1 was ineffective at reducing psychotic symptoms in individuals with schizophrenia and schizoaffective disorder [63], suggesting the possibility that cannabidiol may exert its antipsychotic effects through other molecular targets.
Three human PET studies have assessed CB1 receptor binding in individuals with schizophrenia. The first study found higher [11C]OMAR binding in individuals with schizophrenia than in healthy controls, which only reached statistical significance in the pons [22]. This study had several limitations. First, all subjects with schizophrenia were undergoing treatment with atypical antipsychotics (either risperidone or olanzapine); therefore, any differences in radiotracer binding could have been secondary to medication effects rather than underlying pathophysiology. Second, the schizophrenia group’s mean age was 8.6 years older than the control group, and CB1 binding was negatively correlated with age in this study. A much larger study overcame these issues by examining [18F]MK-9470 binding in medicated and unmedicated individuals with schizophrenia and age-matched controls [64]. Global increases in CB1 receptor availability were observed in both schizophrenia groups. However, in contrast to earlier findings, a third study employing [11C]OMAR found global reductions in CB1 receptor availability in both medicated and unmedicated patients with schizophrenia [65], raising questions about whether endocannabinoid signaling is increased or decreased in this disorder.
Another question raised by these studies is whether antipsychotic treatment alters CB1 availability. Ceccarini et al. [64] compared CB1 availability in medicated and unmedicated patients with schizophrenia and found that the medicated group had CB1 availability closer to that of controls, suggesting that antipsychotic treatment may normalize CB1 availability. In concordance with this finding, Ranganathan et al. [65] also found that antipsychotic treatment tended to normalize CB1 availability. Normalization of CB1 availability could be secondary to the pharmacological effects of antipsychotics, such as D2 receptor antagonism, or may be a sign of clinical response to treatment. Several lines of evidence suggest that the latter may be the case. First, Ranganathan et al. [65] found that antipsychotic dose was not correlated with CB1 availability, suggesting that increased D2 antagonism does not reduce CB1 availability. Second, all three studies demonstrated correlations between CB1 availability and symptom severity measures [22, 64, 65], although there was disagreement as to which symptoms correlated best with CB1 availability. Third, individuals with schizophrenia have higher circulating and cerebrospinal levels of anandamide than healthy controls [66, 67], but circulating levels return to normal following clinical remission [66]. Thus, these findings provide preliminary evidence that CB1 receptor availability and circulating levels of endocannabinoids may have some utility as a biomarker for clinical response in individuals with schizophrenia.
Post-traumatic stress disorder
Endocannabinoid signaling may modulate anxiety and stress responses in humans. For example, subjecting healthy subjects to experimental stress induction paradigms leads to increases in circulating cannabinoid levels [68, 69], which may buffer human stress responses. In support of this, individuals carrying a FAAH polymorphism that decreases anandamide metabolism demonstrate more rapid fear extinction [26, 70] and a reduced amygdala response to fearful faces [71]. Interestingly, acute stress-induced increases in circulating endocannabinoid concentrations have not been observed in subjects with comorbid PTSD and alcohol dependence [72], indicating potential aberrancies in endocannabinoid-related stress regulation in these subjects.
Several studies have found reductions in circulating endocannabinoid levels in individuals with PTSD [73, 74], although one study demonstrated lower circulating levels of anandamide but not 2-AG [74], whereas another demonstrated lower levels of 2-AG but not anandamide [73]. Hair samples derived from individuals with PTSD also contain lower levels of endocannabinoids compared to controls [75]. Only one human PET study has examined central CB1 binding in PTSD. This study compared untreated individuals with PTSD to trauma-exposed and healthy controls and found global increases in CB1 binding in the PTSD group compared to both control groups [74] (Table 3). This increase in CB1 binding could represent upregulated receptor levels secondary to depressed endocannabinoid levels. In support of this, [11C]OMAR binding was found to correlate negatively with circulating anandamide levels, although the strength of this correlation was modest (r = −0.27). In a subsample of this study (n = 20), both decreased circulating anandamide levels and elevated CB1 receptor availability in the amygdala were associated with increased attentional bias to threat using a dot-probe task [76]. These studies provide preliminary evidence that the endocannabinoid system is involved in PTSD symptomatology.
Since endocannabinoids appear to influence stress and anxiety, cannabinoid receptor agonists have been proposed as a potential treatment for PTSD. One small randomized placebo-controlled crossover trial indicated that nabilone, a synthetic analog of Δ9-THC, reduced PTSD symptoms in male military personnel compared to placebo [77]. Despite the lack of randomized trials investigating cannabis use for this indication, some states allow the use of medical marijuana to treat PTSD [78, 79]. This is concerning given that individuals with PTSD have a substantially increased likelihood of being diagnosed with cannabis use disorder [80]. Further research is needed to clarify whether medical marijuana use for PTSD treatment is causing more benefit than harm.
Eating disorders
Exogenous cannabinoids have long been known to influence appetite and food intake. Whereas cannabis intoxication increases appetite [81], cannabis withdrawal is associated with decreased caloric intake and weight loss [31]. Dronabinol, an encapsulated form of oral Δ9-THC which was the first Food and Drug Administration (FDA)-approved cannabinoid, received its initial indication as an appetite stimulant for individuals with AIDS who had experienced anorexia and weight loss [82]. Despite the appetite-stimulating effects of acute Δ9-THC intoxication, chronic Δ9-THC use may actually be protective against obesity [83]. These putative anti-obesity effects remain poorly understood, although several central and peripheral mechanisms have been proposed [84, 85]. Like their exogenous counterparts, endogenous cannabinoids may also regulate appetite and food intake. Presenting food to normal weight and obese individuals has been shown to increase circulating anandamide [86]; levels of anandamide gradually decrease following food consumption or intravenous glucose administration [86, 87]. Multiple studies also suggest that exercise increases circulating anandamide levels [88, 89], suggesting that anandamide may stimulate appetite following energy utilization. The endocannabinoid system therefore represents a viable pharmacological target for disordered eating.
Clinical trials have investigated medications that block the CB1 receptor as a treatment for obesity. Four large randomized trials found that rimonabant, an inverse agonist of the CB1 receptor, led to weight loss and improvement of cardiometabolic risk factors when compared to placebo [90,91,92,93]. Rimonabant was approved by the European Medicine Agency as a treatment for obesity in 2006 [94]. However, regulatory approval was subsequently withdrawn when rimonabant was discovered to increase anxious and depressive symptomatology [95, 96], which may have led to the higher rate of suicide attempts and completions observed in a large trial investigating the use of rimonabant to prevent cardiovascular death in high-risk patients [97]. Given that blocking CB1 receptors decreases food intake, it would stand to reason that decreased CB1 signaling may be present in individuals who restrict their caloric intake. Indeed, there is evidence that individuals with anorexia nervosa do not exhibit normal endocannabinoid responses to food consumption [98].
Human PET studies have examined CB1 availability in individuals with disordered eating (Table 3). One study, using [18F]MK-9470, found that CB1 availability was globally increased in subjects with anorexia nervosa compared to both healthy controls and subjects with bulimia nervosa [99]. The bulimia nervosa group also had global increases in CB1 availability compared to healthy controls, although the difference did not reach statistical significance. Another study examined CB1 availability in functional dyspepsia, a disorder that is not included in the Diagnostic and Statistical Manual of Mental Disorders (DSM), in which patients have abdominal pain with no obvious organic etiology on diagnostic testing [100]. This study also found increased CB1 availability in cases versus controls, which persisted when subjects were re-scanned 3 years later [101]. An analysis pooling data from both studies, which also included an additional group of individuals with obesity, found a negative association between radiotracer binding and body mass index (BMI) [102], replicating an association observed in some [39] but not all [40, 51, 74] CB1 PET studies. This association raises the possibility that the fluctuations in BMI associated with disordered eating may explain the observed alterations in radiotracer binding, suggesting that altered CB1 availability may be a result of disordered eating rather than a causal factor. Prospective studies of subjects with anorexia and bulimia may help resolve this issue.
Discussion
Human PET studies have examined CB1 availability in several psychiatric conditions. Of these, studies comparing cannabis users to healthy controls have the most consistent findings. All three published studies demonstrated reduced CB1 availability in cannabis users, likely due to receptor downregulation following heavy cannabis exposure. This parallels studies of stimulant users, which suggest that chronic dopamine exposure leads to reductions in D2/D3 receptor availability [103]. As with stimulant users [104], a period of abstinence from cannabis use seems to normalize receptor availability [39, 40]. Studies investigating CB1 availability in individuals with alcohol use disorder and schizophrenia have been less consistent, with some studies reporting increased availability and others reporting decreased availability. Preliminary results in samples with PTSD and anorexia nervosa indicate altered endocannabinoid signaling, but other common psychiatric disorders such as major depressive disorder have yet to be studied. Across disorders, differences in CB1 availability tend to be global rather than regional, with radioligand binding showing strong correlations across brain regions.
Several factors could explain the discrepant results observed in the schizophrenia and alcohol use disorder studies. One possibility is that the use of different radiotracers influenced findings [105]. Indeed, several PET studies using [11C]OMAR, a reversible radiotracer, have yielded different results from those using the irreversible radiotracers [18F]MK-9470 and [18F]FMPEP-d2 [51,52,53, 64, 65]. On the other hand, two studies using [11C]OMAR to compare patients with schizophrenia to healthy controls reported results in the opposite direction [22, 65], which makes this hypothesis seem somewhat less plausible. Genetic factors may also affect CB1 availability. There is evidence that a variant of the CB1 gene (rs2023239) alters radiotracer binding, but only one study controlled for this polymorphism [52]. Furthermore, there is preliminary evidence of lower CB1 availability in healthy subjects of Indian ancestry compared to those of European and African ancestry [39]. A recent analysis of raclopride studies demonstrated significant differences in binding based on ancestry [106]; thus, ancestry may deserve greater consideration in human PET studies than previously assumed. Other confounding factors could include length of illness and symptom severity, which were correlated with CB1 availability in some studies (Supplemental Tables 1 and 2). Future studies should attempt to parse out the effects of each of these variables.
Tobacco use represents another potential confound, as subjects with psychiatric disorders tended to smoke at much higher rates than controls across studies (Supplemental Tables 1 and 2). A published abstract directly comparing CB1 availability in smokers and non-smokers using [18F]FMPEP-d2 found that smokers had significantly lower CB1 availability throughout the brain [107]. However, this contrasts with supplementary analyses performed in several published studies, which found that smoking status was not associated with CB1 availability in individuals with comorbid psychopathology [39, 41, 52, 53, 64, 74]. Only one supplementary analysis suggested a main effect of comorbid tobacco use, indicating that smokers with schizophrenia had higher CB1 availability than non-smokers with schizophrenia, although this was only significant at a trend level (P = 0.096) [65]. Thus, the preponderance of evidence suggests that comorbid tobacco use has no effect on CB1 availability in patients with psychiatric disorders. However, these supplementary analyses were often limited to a subgroup of cases who smoked and were potentially underpowered to detect main effects of tobacco use. Additional studies should be conducted to assess CB1 availability in smokers and non-smokers with and without psychiatric comorbidities in order to resolve this issue.
Most human PET studies evaluating the endocannabinoid system have focused on CB1. Less is known about whether psychiatric disorders are associated with alterations in other molecules involved in endocannabinoid signaling, such as FAAH, MAGL, and CB2. To date, only one published PET study has probed for abnormalities in endocannabinoid degradation in a clinical sample, employing [11C]CURB to measure FAAH activity in cannabis users [42]. This tracer should be used in other clinical populations with hypothesized aberrancies in endocannabinoid signaling, including samples with schizophrenia and PTSD. The development of radiotracers targeting MAGL [108] ensures that there will also be new studies evaluating the role of 2-AG in these disorders. CB2 receptors represent another target of potential interest. Although they are mainly expressed on peripheral immune cells, there is preclinical evidence that they are also expressed in the brain [109, 110], where they may affect addictive and schizophrenia-related behaviors [110,111,112]. Several attempts have been made to develop CB2 radiotracers, but these ligands have been unsuitable for clinical imaging studies due to high non-specific binding and unfavorable pharmacokinetic properties [113]. Hopefully, the synthesis of new tracers for these targets will allow for a greater understanding of all aspects of endocannabinoid signaling rather than focusing exclusively on CB1.
At the present time, we only possess a rudimentary understanding of endocannabinoid signaling in humans. The PET studies summarized in this review represent an initial attempt at characterizing alterations in endocannabinoid signaling in psychiatric disorders. Subsequent PET studies should be complemented by studies measuring circulating and cerebrospinal endocannabinoid levels and postmortem studies employing autoradiography and immunohistochemistry in individuals with and without disease. Furthermore, both in vitro and animal studies will be necessary to clarify how receptor downregulation or upregulation and changes in enzymatic activity affect cellular signaling and contribute to the behavioral phenotypes observed in these disorders. This work will hopefully lead to a greater understanding of endocannabinoid signaling in human psychopathology.
References
Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77:299–318.
Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci U S A. 1990;87:1932–6.
Marsicano G, Wotjak CT, Azad SC, Bisogno T, Rammes G, Cascio MG, et al. The endogenous cannabinoid system controls extinction of aversive memories. Nature. 2002;418:530–4.
Hill MN, McLaughlin RJ, Pan B, Fitzgerald ML, Roberts CJ, Lee TT, et al. Recruitment of prefrontal cortical endocannabinoid signaling by glucocorticoids contributes to termination of the stress response. J Neurosci. 2011;31:10506–15.
Zangen A, Solinas M, Ikemoto S, Goldberg SR, Wise RA. Two brain sites for cannabinoid reward. J Neurosci. 2006;26:4901–7.
Le Foll B, Goldberg SR. Cannabinoid CB1 receptor antagonists as promising new medications for drug dependence. J Pharmacol Exp Ther. 2005;312:875–83.
Hungund BL, Szakall I, Adam A, Basavarajappa BS, Vadasz C. Cannabinoid CB1 receptor knockout mice exhibit markedly reduced voluntary alcohol consumption and lack alcohol-induced dopamine release in the nucleus accumbens. J Neurochem. 2003;84:698–704.
Cohen C, Perrault G, Voltz C, Steinberg R, Soubrie P. SR141716, a central cannabinoid (CB(1)) receptor antagonist, blocks the motivational and dopamine-releasing effects of nicotine in rats. Behav Pharmacol. 2002;13:451–63.
Hillard CJ, Liu QS. Endocannabinoid signaling in the etiology and treatment of major depressive illness. Curr Pharm Des. 2014;20:3795–811.
Patel S, Hill MN, Cheer JF, Wotjak CT, Holmes A. The endocannabinoid system as a target for novel anxiolytic drugs. Neurosci Biobehav Rev. 2017;76:56–66.
Sloan ME, Gowin JL, Ramchandani VA, Hurd YL, Le Foll B. The endocannabinoid system as a target for addiction treatment: Trials and tribulations. Neuropharmacology. 2017;124:73–83.
Goffin K, Van Paesschen W, Van Laere K. In vivo activation of endocannabinoid system in temporal lobe epilepsy with hippocampal sclerosis. Brain. 2011;134:1033–40.
Van der Schueren BJ, Van Laere K, Gerard N, Bormans G, De Hoon JN. Interictal type 1 cannabinoid receptor binding is increased in female migraine patients. Headache. 2012;52:433–40.
Ahmad R, Goffin K, Van den Stock J, De Winter FL, Cleeren E, Bormans G, et al. In vivo type 1 cannabinoid receptor availability in Alzheimer’s disease. Eur Neuropsychopharmacol. 2014;24:242–50.
Van Laere K, Casteels C, Lunskens S, Goffin K, Grachev ID, Bormans G, et al. Regional changes in type 1 cannabinoid receptor availability in Parkinson’s disease in vivo. Neurobiol Aging. 2012;33:e1–8.
Horti AG, Van Laere K. Development of radioligands for in vivo imaging of type 1 cannabinoid receptors (CB1) in human brain. Curr Pharm Des. 2008;14:3363–83.
Hirvonen J. In vivo imaging of the cannabinoid CB1 receptor with positron emission tomography. Clin Pharmacol Ther. 2015;97:565–7.
Heurling K, Leuzy A, Jonasson M, Frick A, Zimmer ER, Nordberg A, et al. Quantitative positron emission tomography in brain research. Brain Res. 2017;1670:220–34.
Terry GE, Hirvonen J, Liow JS, Zoghbi SS, Gladding R, Tauscher JT, et al. Imaging and quantitation of cannabinoid CB1 receptors in human and monkey brains using (18)F-labeled inverse agonist radioligands. J Nucl Med. 2010;51:112–20.
Burns HD, Van Laere K, Sanabria-Bohorquez S, Hamill TG, Bormans G, Eng WS, et al. [18F]MK-9470, a positron emission tomography (PET) tracer for in vivo human PET brain imaging of the cannabinoid-1 receptor. Proc Natl Acad Sci U S A. 2007;104:9800–5.
Normandin MD, Zheng MQ, Lin KS, Mason NS, Lin SF, Ropchan J, et al. Imaging the cannabinoid CB1 receptor in humans with [11C]OMAR: assessment of kinetic analysis methods, test-retest reproducibility, and gender differences. J Cereb Blood Flow Metab. 2015;35:1313–22.
Wong DF, Kuwabara H, Horti AG, Raymont V, Brasic J, Guevara M, et al. Quantification of cerebral cannabinoid receptors subtype 1 (CB1) in healthy subjects and schizophrenia by the novel PET radioligand [11C]OMAR. Neuroimage. 2010;52:1505–13.
Terry GE, Liow JS, Zoghbi SS, Hirvonen J, Farris AG, Lerner A, et al. Quantitation of cannabinoid CB1 receptors in healthy human brain using positron emission tomography and an inverse agonist radioligand. Neuroimage. 2009;48:362–70.
Wilson AA, Garcia A, Parkes J, Houle S, Tong J, Vasdev N. [11C]CURB: evaluation of a novel radiotracer for imaging fatty acid amide hydrolase by positron emission tomography. Nucl Med Biol. 2011;38:247–53.
Boileau I, Rusjan PM, Williams B, Mansouri E, Mizrahi R, De Luca V, et al. Blocking of fatty acid amide hydrolase activity with PF-04457845 in human brain: a positron emission tomography study with the novel radioligand [(11)C]CURB. J Cereb Blood Flow Metab. 2015;35:1827–35.
Dincheva I, Drysdale AT, Hartley CA, Johnson DC, Jing D, King EC, et al. FAAH genetic variation enhances fronto-amygdala function in mouse and human. Nat Commun. 2015;6:6395.
Chiang KP, Gerber AL, Sipe JC, Cravatt BF. Reduced cellular expression and activity of the P129T mutant of human fatty acid amide hydrolase: evidence for a link between defects in the endocannabinoid system and problem drug use. Hum Mol Genet. 2004;13:2113–9.
Boileau I, Tyndale RF, Williams B, Mansouri E, Westwood DJ, Le Foll B, et al. The fatty acid amide hydrolase C385A variant affects brain binding of the positron emission tomography tracer [11C]CURB. J Cereb Blood Flow Metab. 2015;35:1237–40.
Vandrey R, Stitzer ML, Mintzer MZ, Huestis MA, Murray JA, Lee D. The dose effects of short-term dronabinol (oral THC) maintenance in daily cannabis users. Drug Alcohol Depend. 2013;128:64–70.
Trigo JM, Lagzdins D, Rehm J, Selby P, Gamaleddin I, Fischer B, et al. Effects of fixed or self-titrated dosages of Sativex on cannabis withdrawal and cravings. Drug Alcohol Depend. 2016;161:298–306.
Haney M, Cooper ZD, Bedi G, Vosburg SK, Comer SD, Foltin RW. Nabilone decreases marijuana withdrawal and a laboratory measure of marijuana relapse. Neuropsychopharmacology. 2013;38:1557–65.
Allsop DJ, Copeland J, Lintzeris N, Dunlop AJ, Montebello M, Sadler C, et al. Nabiximols as an agonist replacement therapy during cannabis withdrawal: a randomized clinical trial. JAMA Psychiatry. 2014;71:281–91.
Levin FR, Mariani JJ, Brooks DJ, Pavlicova M, Cheng W, Nunes EV. Dronabinol for the treatment of cannabis dependence: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2011;116:142–50.
Levin FR, Mariani JJ, Pavlicova M, Brooks D, Glass A, Mahony A, et al. Dronabinol and lofexidine for cannabis use disorder: a randomized, double-blind, placebo-controlled trial. Drug Alcohol Depend. 2016;159:53–60.
Trigo JM, Soliman A, Quilty LC, Fischer B, Rehm J, Selby P, et al. Nabiximols combined with motivational enhancement/cognitive behavioral therapy for the treatment of cannabis dependence: a pilot randomized clinical trial. PLoS ONE. 2018;13:e0190768.
Schindler CW, Redhi GH, Vemuri K, Makriyannis A, Le Foll B, Bergman J, et al. Blockade of nicotine and cannabinoid reinforcement and relapse by a cannabinoid CB1-receptor neutral antagonist AM4113 and inverse agonist rimonabant in squirrel monkeys. Neuropsychopharmacology. 2016;41:2283–93.
Justinova Z, Munzar P, Panlilio LV, Yasar S, Redhi GH, Tanda G, et al. Blockade of THC-seeking behavior and relapse in monkeys by the cannabinoid CB(1)-receptor antagonist rimonabant. Neuropsychopharmacology. 2008;33:2870–7.
Marshall K,Gowing L,Ali R,Le Foll B. Pharmacotherapies for cannabis dependence. Cochrane Database Syst Rev. 2014;(12): CD008940.
Hirvonen J, Goodwin RS, Li CT, Terry GE, Zoghbi SS, Morse C, et al. Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers. Mol Psychiatry. 2012;17:642–9.
D’Souza DC, Cortes-Briones JA, Ranganathan M, Thurnauer H, Creatura G, Surti T, et al. Rapid changes in CB1 receptor availability in cannabis dependent males after abstinence from cannabis. Biol Psychiatry Cogn Neurosci Neuroimaging. 2016;1:60–7.
Ceccarini J, Kuepper R, Kemels D, van Os J, Henquet C, Van Laere K. [18F]MK-9470 PET measurement of cannabinoid CB1 receptor availability in chronic cannabis users. Addict Biol. 2015;20:357–67.
Boileau I, Mansouri E, Williams B, Le Foll B, Rusjan P, Mizrahi R, et al. Fatty acid amide hydrolase binding in brain of cannabis users: imaging with the novel radiotracer [(11)C]CURB. Biol Psychiatry. 2016;80:691–701.
Morgan CJ, Page E, Schaefer C, Chatten K, Manocha A, Gulati S, et al. Cerebrospinal fluid anandamide levels, cannabis use and psychotic-like symptoms. Br J Psychiatry. 2013;202:381–2.
Sloan ME, Gowin JL, Yan J, Schwandt ML, Spagnolo PA, Sun H, et al. Severity of alcohol dependence is associated with the fatty acid amide hydrolase Pro129Thr missense variant. Addict Biol.2018;23:474–84.
Colombo G, Serra S, Brunetti G, Gomez R, Melis S, Vacca G, et al. Stimulation of voluntary ethanol intake by cannabinoid receptor agonists in ethanol-preferring sP rats. Psychopharmacology (Berl). 2002;159:181–7.
Colombo G, Agabio R, Fa M, Guano L, Lobina C, Loche A, et al. Reduction of voluntary ethanol intake in ethanol-preferring sP rats by the cannabinoid antagonist SR-141716. Alcohol Alcohol. 1998;33:126–30.
Arnone M, Maruani J, Chaperon F, Thiebot MH, Poncelet M, Soubrie P, et al. Selective inhibition of sucrose and ethanol intake by SR 141716, an antagonist of central cannabinoid (CB1) receptors. Psychopharmacology (Berl). 1997;132:104–6.
Femenia T, Garcia-Gutierrez MS, Manzanares J. CB1 receptor blockade decreases ethanol intake and associated neurochemical changes in fawn-hooded rats. Alcohol Clin Exp Res. 2010;34:131–41.
George DT, Herion DW, Jones CL, Phillips MJ, Hersh J, Hill D, et al. Rimonabant (SR141716) has no effect on alcohol self-administration or endocrine measures in nontreatment-seeking heavy alcohol drinkers. Psychopharmacology (Berl). 2010;208:37–44.
Soyka M, Koller G, Schmidt P, Lesch OM, Leweke M, Fehr C, et al. Cannabinoid receptor 1 blocker rimonabant (SR 141716) for treatment of alcohol dependence: results from a placebo-controlled, double-blind trial. J Clin Psychopharmacol. 2008;28:317–24.
Neumeister A, Normandin MD, Murrough JW, Henry S, Bailey CR, Luckenbaugh DA, et al. Positron emission tomography shows elevated cannabinoid CB1 receptor binding in men with alcohol dependence. Alcohol Clin Exp Res. 2012;36:2104–9.
Hirvonen J, Zanotti-Fregonara P, Umhau JC, George DT, Rallis-Frutos D, Lyoo CH, et al. Reduced cannabinoid CB1 receptor binding in alcohol dependence measured with positron emission tomography. Mol Psychiatry. 2013;18:916–21.
Ceccarini J, Hompes T, Verhaeghen A, Casteels C, Peuskens H, Bormans G, et al. Changes in cerebral CB1 receptor availability after acute and chronic alcohol abuse and monitored abstinence. J Neurosci. 2014;34:2822–31.
Marconi A, Di Forti M, Lewis CM, Murray RM, Vassos E. Meta-analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull. 2016;42:1262–9.
Di Forti M, Marconi A, Carra E, Fraietta S, Trotta A, Bonomo M, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. Lancet. Psychiatry. 2015;2:233–8.
Linszen DH, Dingemans PM, Lenior ME. Cannabis abuse and the course of recent-onset schizophrenic disorders. Arch Gen Psychiatry. 1994;51:273–9.
Manrique-Garcia E, Zammit S, Dalman C, Hemmingsson T, Andreasson S, Allebeck P. Prognosis of schizophrenia in persons with and without a history of cannabis use. Psychol Med. 2014;44:2513–21.
D’Souza DC, Perry E, MacDougall L, Ammerman Y, Cooper T, Wu YT, et al. The psychotomimetic effects of intravenous delta-9-tetrahydrocannabinol in healthy individuals: implications for psychosis. Neuropsychopharmacology. 2004;29:1558–72.
Cortes-Briones JA, Cahill JD, Skosnik PD, Mathalon DH, Williams A, Sewell RA, et al. The psychosis-like effects of Delta(9)-tetrahydrocannabinol are associated with increased cortical noise in healthy humans. Biol Psychiatry. 2015;78:805–13.
Laprairie RB, Bagher AM, Kelly ME, Denovan-Wright EM. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br J Pharmacol. 2015;172:4790–805.
Leweke FM, Piomelli D, Pahlisch F, Muhl D, Gerth CW, Hoyer C, et al. Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl Psychiatry. 2012;2:e94.
McGuire P, Robson P, Cubala WJ, Vasile D, Morrison PD, Barron R, et al. Cannabidiol (CBD) as an adjunctive therapy in schizophrenia: a multicenter randomized controlled trial.Am J Psychiatry. 2018;175:225–31.
Meltzer HY, Arvanitis L, Bauer D, Rein W. Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry. 2004;161:975–84.
Ceccarini J, De Hert M, Van Winkel R, Peuskens J, Bormans G, Kranaster L, et al. Increased ventral striatal CB1 receptor binding is related to negative symptoms in drug-free patients with schizophrenia. Neuroimage. 2013;79:304–12.
Ranganathan M, Cortes-Briones J, Radhakrishnan R, Thurnauer H, Planeta B, Skosnik P, et al. Reduced brain cannabinoid receptor availability in schizophrenia. Biol Psychiatry. 2016;79:997–1005.
De Marchi N, De Petrocellis L, Orlando P, Daniele F, Fezza F, Di Marzo V. Endocannabinoid signalling in the blood of patients with schizophrenia. Lipids Health Dis. 2003;2:5.
Leweke FM, Giuffrida A, Wurster U, Emrich HM, Piomelli D. Elevated endogenous cannabinoids in schizophrenia. Neuroreport. 1999;10:1665–9.
Dlugos A, Childs E, Stuhr KL, Hillard CJ, de Wit H. Acute stress increases circulating anandamide and other N-acylethanolamines in healthy humans. Neuropsychopharmacology. 2012;37:2416–27.
Hill MN, Miller GE, Carrier EJ, Gorzalka BB, Hillard CJ. Circulating endocannabinoids and N-acyl ethanolamines are differentially regulated in major depression and following exposure to social stress. Psychoneuroendocrinology. 2009;34:1257–62.
Gunduz-Cinar O, MacPherson KP, Cinar R, Gamble-George J, Sugden K, Williams B, et al. Convergent translational evidence of a role for anandamide in amygdala-mediated fear extinction, threat processing and stress-reactivity. Mol Psychiatry. 2013;18:813–23.
Hariri AR, Gorka A, Hyde LW, Kimak M, Halder I, Ducci F, et al. Divergent effects of genetic variation in endocannabinoid signaling on human threat- and reward-related brain function. Biol Psychiatry. 2009;66:9–16.
Spagnolo PA, Ramchandani VA, Schwandt ML, Kwako LE, George DT, Mayo LM, et al. FAAH gene variation moderates stress response and symptom severity in patients with posttraumatic stress disorder and comorbid alcohol dependence. Alcohol Clin Exp Res. 2016;40:2426–34.
Hill MN, Bierer LM, Makotkine I, Golier JA, Galea S, McEwen BS, et al. Reductions in circulating endocannabinoid levels in individuals with post-traumatic stress disorder following exposure to the World Trade Center attacks. Psychoneuroendocrinology. 2013;38:2952–61.
Neumeister A, Normandin MD, Pietrzak RH, Piomelli D, Zheng MQ, Gujarro-Anton A, et al. Elevated brain cannabinoid CB1 receptor availability in post-traumatic 5stress disorder: a positron emission tomography study. Mol Psychiatry. 2013;18:1034–40.
Wilker S, Pfeiffer A, Elbert T, Ovuga E, Karabatsiakis A, Krumbholz A, et al. Endocannabinoid concentrations in hair are associated with PTSD symptom severity. Psychoneuroendocrinology. 2016;67:198–206.
Pietrzak RH, Huang Y, Corsi-Travali S, Zheng MQ, Lin SF, Henry S, et al. Cannabinoid type 1 receptor availability in the amygdala mediates threat processing in trauma survivors. Neuropsychopharmacology. 2014;39:2519–28.
Jetly R, Heber A, Fraser G, Boisvert D. The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: A preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology. 2015;51:585–8.
D’Souza DC, Ranganathan M. Medical marijuana: is the cart before the horse? JAMA. 2015;313:2431–2.
Steenkamp MM, Blessing EM, Galatzer-Levy IR, Hollahan LC, Anderson WT. Marijuana and other cannabinoids as a treatment for posttraumatic stress disorder: a literature review. Depress Anxiety. 2017;34:207–16.
Hasin DS, Kerridge BT, Saha TD, Huang B, Pickering R, Smith SM, et al. Prevalence and correlates of DSM-5 cannabis use disorder, 2012-2013: findings from the National Epidemiologic Survey on alcohol and related conditions-iii. Am J Psychiatry. 2016;173:588–99.
Haney M, Ward AS, Comer SD, Foltin RW, Fischman MW. Abstinence symptoms following smoked marijuana in humans. Psychopharmacology (Berl). 1999;141:395–404.
FDA. MARINOL (dronabinol) capsules, for oral use. 2017.
Le Strat Y, Le Foll B. Obesity and cannabis use: results from 2 representative national surveys. Am J Epidemiol. 2011;174:929–33.
Cluny NL, Keenan CM, Reimer RA, Le Foll B, Sharkey KA. Prevention of diet-induced obesity effects on body weight and gut microbiota in mice treated chronically with delta9-tetrahydrocannabinol. PLoS ONE. 2015;10:e0144270.
Le Foll B, Trigo JM, Sharkey KA, Le Strat Y. Cannabis and delta9-tetrahydrocannabinol (THC) for weight loss? Med Hypotheses. 2013;80:564–7.
Gatta-Cherifi B, Matias I, Vallee M, Tabarin A, Marsicano G, Piazza PV, et al. Simultaneous postprandial deregulation of the orexigenic endocannabinoid anandamide and the anorexigenic peptide YY in obesity. Int J Obes (Lond). 2012;36:880–5.
Di Marzo V, Verrijken A, Hakkarainen A, Petrosino S, Mertens I, Lundbom N, et al. Role of insulin as a negative regulator of plasma endocannabinoid levels in obese and nonobese subjects. Eur J Endocrinol. 2009;161:715–22.
Heyman E, Gamelin FX, Goekint M, Piscitelli F, Roelands B, Leclair E, et al. Intense exercise increases circulating endocannabinoid and BDNF levels in humans--possible implications for reward and depression. Psychoneuroendocrinology. 2012;37:844–51.
Koltyn KF, Brellenthin AG, Cook DB, Sehgal N, Hillard C. Mechanisms of exercise-induced hypoalgesia. J Pain. 2014;15:1294–304.
Despres JP, Golay A, Sjostrom L. Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med. 2005;353:2121–34.
Scheen AJ, Finer N, Hollander P, Jensen MD, Van Gaal LF, Group, R-DS. Efficacy and tolerability of rimonabant in overweight or obese patients with type 2 diabetes: a randomised controlled study. Lancet. 2006;368:1660–72.
Van Gaal LF, Rissanen AM, Scheen AJ, Ziegler O, Rossner S. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet. 2005;365:1389–97.
Pi-Sunyer FX, Aronne LJ, Heshmati HM, Devin J, Rosenstock J, Group, R-NAS. Effect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trial. JAMA. 2006;295:761–75.
EMA. EUROPEAN PUBLIC ASSESSMENT REPORT (EPAR) ACOMPLIA: EPAR summary for the public. London: European Medicines Agency; 2007.
Rucker D, Padwal R, Li SK, Curioni C, Lau DC. Long term pharmacotherapy for obesity and overweight: updated meta-analysis. BMJ. 2007;335:1194–9.
Christensen R, Kristensen PK, Bartels EM, Bliddal H, Astrup A. Efficacy and safety of the weight-loss drug rimonabant: a meta-analysis of randomised trials. Lancet. 2007;370:1706–13.
Topol EJ, Bousser MG, Fox KA, Creager MA, Despres JP, Easton JD, et al. Rimonabant for prevention of cardiovascular events (CRESCENDO): a randomised, multicentre, placebo-controlled trial. Lancet. 2010;376:517–23.
Monteleone AM, Di Marzo V, Aveta T, Piscitelli F, Dalle Grave R, Scognamiglio P, et al. Deranged endocannabinoid responses to hedonic eating in underweight and recently weight-restored patients with anorexia nervosa. Am J Clin Nutr. 2015;101:262–9.
Gerard N, Pieters G, Goffin K, Bormans G, Van Laere K. Brain type 1 cannabinoid receptor availability in patients with anorexia and bulimia nervosa. Biol Psychiatry. 2011;70:777–84.
Brun R, Kuo B. Functional dyspepsia. Ther Adv Gastroenterol. 2010;3:145–64.
Ly HG, Ceccarini J, Weltens N, Bormans G, Van Laere K, Tack J, et al. Increased cerebral cannabinoid-1 receptor availability is a stable feature of functional dyspepsia: a [F]MK-9470 PET study. Psychother Psychosom. 2015;84:149–58.
Ceccarini J, Weltens N, Ly HG, Tack J, Van Oudenhove L, Van Laere K. Association between cerebral cannabinoid 1 receptor availability and body mass index in patients with food intake disorders and healthy subjects: a [(18)F]MK-9470 PET study. Transl Psychiatry. 2016;6:e853.
Ashok AH, Mizuno Y, Volkow ND, Howes OD. Association of stimulant use with dopaminergic alterations in users of cocaine, amphetamine, or methamphetamine: a systematic review and Meta-analysis. JAMA Psychiatry. 2017;74:511–9.
Volkow ND, Fowler JS, Wolf AP, Schlyer D, Shiue CY, Alpert R, et al. Effects of chronic cocaine abuse on postsynaptic dopamine receptors. Am J Psychiatry. 1990;147:719–24.
Mihov Y. Positron emission tomography studies on cannabinoid receptor type 1 in Schizophrenia. Biol Psychiatry. 2016;79:e97–9.
Wiers CE, Towb PC, Hodgkinson CA, Shen PH, Freeman C, Miller G, Lindgren E, Shokri-Kojori E, Demiral ŞB, Kim SW, Tomasi D. Association of genetic ancestry with striatal dopamine D2/D3 receptor availability. Molecular psychiatry. 2017 Nov 7. https://doi.org/10.1038/mp.2017.208. [Epub ahead of print]
Hirvonen J, Zanotti-Fregonara P, Gorelick D, Rallis-Frutos D, Morse C, Zoghbi S, et al. Decreased brain cannabinoid CB1 receptor binding in tobacco smokers examined with positron emission tomography. J Nucl Med. 2014;55:84.
Wang C, Placzek MS, Van de Bittner GC, Schroeder FA, Hooker JM. A novel radiotracer for imaging monoacylglycerol lipase in the brain using positron emission tomography. ACS Chem Neurosci. 2016;7:484–9.
Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, Mackie K, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310:329–32.
Zhang HY, Gao M, Liu QR, Bi GH, Li X, Yang HJ, et al. Cannabinoid CB2 receptors modulate midbrain dopamine neuronal activity and dopamine-related behavior in mice. Proc Natl Acad Sci Usa. 2014;111:E5007–15.
Xi ZX, Peng XQ, Li X, Song R, Zhang HY, Liu QR, et al. Brain cannabinoid CB(2) receptors modulate cocaine’s actions in mice. Nat Neurosci. 2011;14:1160–6.
Ortega-Alvaro A, Aracil-Fernandez A, Garcia-Gutierrez MS, Navarrete F, Manzanares J. Deletion of CB2 cannabinoid receptor induces schizophrenia-related behaviors in mice. Neuropsychopharmacology. 2011;36:1489–504.
Spinelli F, Mu L, Ametamey SM. Radioligands for positron emission tomography imaging of cannabinoid type 2 receptor. J Label Comp Radiopharm. 2018;61:299–308.
Acknowledgements
This study was supported by the NIAAA Division of Intramural Clinical and Biological Research (Z1A AA000466).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Sloan, M.E., Grant, C.W., Gowin, J.L. et al. Endocannabinoid signaling in psychiatric disorders: a review of positron emission tomography studies. Acta Pharmacol Sin 40, 342–350 (2019). https://doi.org/10.1038/s41401-018-0081-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-018-0081-z