Abstract
Background
Obesity is the result of energy intake (EI) chronically exceeding energy expenditure. However, the potential metabolic factors, including insulin resistance, remain unclear. This study longitudinally investigated factors associated with changes in body weight.
Subjects
A cohort of 707 adults without diabetes were investigated at the 4-year follow-up visit. The habitual intake of energy and macronutrients during the past 12 months was assessed using a validated Food Frequency Questionnaire for the local population. Homeostatic model assessment of β-cell function and insulin resistance (HOMA-IR) was used as a surrogate measure of insulin resistance. Additionally, PNPLA3 was genotyped.
Results
Eighty-seven participants were weight gainers (G; cutoff value = 5 kg), and 620 were non-gainers (NG). Initial anthropometric (G vs. NG: age, 44 ± 13 vs 51 ± 13 years, P < 0.001; body mass index, 27.8 ± 6.5 vs 28.1 ± 5.1 kg/m2, P = ns; body weight, 76.7 ± 22.1 vs 74.2 ± 14.7 kg, P = ns; final body weight, 86.3 ± 23.7 vs 72.9 ± 14.2 kg, P < 0.001) and diet characteristics, as well as insulin concentrations and HOMA-IR values, were similar in both groups. Four years later, G showed significantly increased EI, insulin concentrations, and HOMA-IR values. G had a higher prevalence of the PNPLA3 CG and GG alleles than NG (P < 0.05). The presence of G was independently associated with age (OR = 1.031), EI change (OR = 2.257), and unfavorable alleles of PNPLA3 gene (OR = 1.700). Final body mass index, waist circumference, and EI were independently associated with final HOMA-IR (P < 0.001).
Conclusions
EI is associated with body weight gain, and genetic factors may influence the energy balance. Insulin resistance is a consequence of weight gain, suggesting a possible intracellular protective mechanism against substrate overflow.
Clinical trial registration
ISRCTN15840340.
Similar content being viewed by others
Introduction
Obesity is an increasingly widespread condition worldwide, with an actual prevalence of over 800 million adults and a predicted prevalence of 1.5 billion people by 2035 [1]. Although it is commonly accepted that obesity is the result of an unhealthy lifestyle, with energy intake chronically exceeding energy expenditure, the roles of other potentially contributing metabolic factors remain clarified [2]. An extensively investigated but still unresolved question concerns the possibility that insulin resistance and hyperinsulinemia, in addition to being caused by obesity, primarily contribute to the development of obesity itself [3,4,5]. In fact, as insulin induces liposynthesis and influences appetite and energy expenditure, it was also proposed that hyperinsulinemia and insulin resistance may primarily induce weight gain [6]. However, clinical epidemiological studies in adult cohorts are inconclusive about this possibility [7, 8]. In addition, studies involving pediatric cohorts have shown contradictory results. In a longitudinal study involving children, Sedaka et al. [9] failed to observe a predictive relationship between insulin, the homeostatic model assessment of β-cell function and insulin resistance (HOMA-IR), and body weight gain. However, a similar study by Labayen et al. [10] demonstrated that insulin resistance in childhood may predict subsequent total and central adiposity gains during adolescence. Insulin resistance associated with obesity is also a common basis of metabolic Syndrome, a clinical condition to which much attention is paid, as it can evolve with the development of type 2 diabetes, hypertension, hypertriglyceridemia, low serum concentrations of high-density lipoprotein-cholesterol (HDL-C), liver steatosis, and atherosclerosis. Therefore, insulin resistance is often considered a clinical problem to address not only favorable lifestyle changes but also pharmacological treatments, as biguanides are the most commonly used drugs [11]. Therefore, ascertaining the longitudinal direction of the association between insulin resistance/hyperinsulinemia and obesity is important because it may contribute to addressing more appropriate strategies, such as prevention-as-treatment, to counteract obesity and its complications.
In this study, we aimed to longitudinally investigate the factors associated with a 4-year body weight change, including serum insulin concentration and HOMA-IR, as a surrogate measure of insulin resistance, in a comprehensive general population cohort.
Subjects and methods
Participants
The Nutrition, Cardiovascular Wellness, and Diabetes (ABCD) Project (ISRCTN15840340) is a longitudinal observational single-center study of a cohort representative of the general population living in Palermo, the largest city in Sicily (Italy), with 674,742 inhabitants in 2011. The ABCD_1 study cohort was recruited in 2011 as previously described [12]. The inclusion criteria were participants aged >18 years and residing in Palermo. The demographic characteristics of the ABCD cohort were similar to, if not overlapping with, those of the general population of the same age range (18–90 years) as presented elsewhere [13]. At the conclusion of their participation in the ABCD_1 study, all participants were interviewed briefly by one of the investigators. During this interview, they received a written report detailing the results of the investigations conducted. This report also highlighted any identified clinical issues and health risk factors. An analysis of eating habits was conducted, and recommendations were provided to improve one’s dietary choices and potentially increase levels of physical activity. The report, along with its associated recommendations, was forwarded to the participants’ doctors. The original cohort was recontacted (telephone, e-mail, letter) in 2015, and those who agreed to participate in the study were re-examined between March 21 and July 31 at the Metabolism and Clinical Nutrition Laboratory of the Department of Internal Medicine at the University of Palermo. Demographic characteristics of the ABCD_2 cohort were not significantly different from those of the ABCD_1 cohort, as reported previously [14]. For this study, individuals with a known diabetes diagnosis were excluded from calculations.
The institutional Ethics Committee (“Palermo 1,” Policlinico “P. Giaccone” University Hospital, 11/03/2014, ref: 3/2015) approved the study protocol, and each participant signed an approved informed consent form.
The habitual intake of energy and macronutrients during the past 12 months was assessed using a previously validated medium-length Food Frequency Questionnaire for the local population as described elsewhere [15]. Adherence to the Mediterranean Diet was assessed by using the MEDI-LITE questionnaire [16].
Habitual physical activity level was investigated using a specific questionnaire for the local population that describes 4 levels of physical activity progressively increasing from 1 to 4 [14].
Participants underwent blood sampling for the assessment of blood chemistry and hormonal parameters. For each participant, a blood sample was frozen and stored at −80 °C for subsequent measurements. Type 2 diabetes and pre-diabetes were defined according to the most recent consensus statements [17].
Measurements
Height and body weight were measured with the participants lightly dressed and without shoes (SECA; Birmingham, UK). Body mass index (BMI) was calculated as body weight (kg)/height2 (m2). Participants with a BMI <25 kg/m2 were categorized as normal-weight, while those with a BMI ≥25 kg/m2 were classified as overweight/obese [18]. Body circumference was measured at the umbilicus (waist circumference) and at the most prominent buttock level (hip circumference) and was used as an indirect index of body fat distribution. Systolic and diastolic arterial blood pressure (two measurements obtained at 5-min intervals in a seated position) and heart rate (Omron M6; Omron Healthcare Co., Matsusaka, Mie, Japan) were measured by physicians or dietitians, according to standardized procedures. Body composition in terms of fat mass (FM) and fat-free mass (FFM) was estimated using Bioelectrical Impedance Analysis (BIA; BIA-101 Anniversary; Akern, Firenze, Italy) following the manufacturer’s equations, as previously described [19].
Laboratory analysis
Fasting plasma glucose, total cholesterol, HDL-C, triglyceride, uric acid, and creatinine levels were measured using standard clinical chemistry methods (Glucosio HK UV; Colesterolo totale Mod P/D; Colesterolo HDL gen 3 mod P/917; Trigliceridi; Acido urico MOD P/917; Creatinina enzimatica; Roche Diagnostics, Monza, Italy). Basal insulin concentrations (Elecsys insulina; Roche Diagnostics; Monza, Italy), high-sensitivity C-reactive protein (hs-CRP; B-analyst hs-CRP; Menarini Diagnostics; Florence, Italy), and glycated hemoglobin (HbA1c; B-analyst HbA1c; Menarini Diagnostics; Florence, Italy) levels were also measured. Low-density lipoprotein-cholesterol serum concentration was calculated using Friedewald’s formula [20]; glomerular filtration rate (eGFR) was estimated based on the CKD-EPI equation [21], and HOMA-IR was calculated as described by Matthews et al. [22]. DNA was purified using a QIAmp blood Mini Kit (Qiagen, Hilden, Germany), and DNA samples were quantified using spectrophotometry. Genotyping for patatin-like phospholipase domain containing 3 (PNPLA3) (rs738409) and transmembrane 6 superfamily 2 (TM6SF2) (rs58542926) was performed using the TaqMan SNP genotyping allelic discrimination method (Applied Biosystems, Foster City, CA, USA).
Statistical analysis
Data are reported as the means ± SD for continuous variables and as percentages for categorical variables. A body weight increase of <3 kg in 10 years is commonly considered physiological in adults [23]. Therefore, based on the body weight change from 2011 to 2015, an arbitrary cutoff value of 5 kg was utilized to distinguish individuals who gained weight (weight gainers, G) from those who did not gain weight (weight non-gainers, NG). Furthermore, it was demonstrated that a body weight gain of 5 kg had a significant impact on different aspects of health [24]. The Student’s t test for unpaired data was used to compare continuous variables between groups. The changes in variables between ABCD_1 and ABCD_2 were assessed using paired sample Student’s t tests. Differences in categorical variables were analyzed using the χ2 test. Pearson’s correlation coefficients were calculated to explore the associations between continuous variables. The absolute differences (Δ = value measured in ABCD_2 – value measured in ABCD_1) between the continuous variables of interest were categorized as 0 (Δ≤0) or 1 (Δ > 0). Multiple logistic binary regression analysis was used to predict the outcomes (body weight change and HOMA-I). Statistical significance was set at P value < 0.05. All analyses were performed using the Systat software (Windows version 13.0; San Jose, CA, USA).
Results
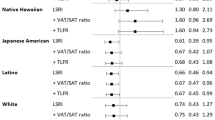
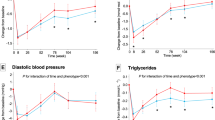
A total of 1139 participants of the ABCD_1 study were selected, and 707 of them were included after the ABCD_2 re-evaluation. The participant selection flowchart is shown in Fig. 1. According to body weight change (cutoff, 5 kg), 87 participants were classified as G and 620 as NG. At the end of follow-up, 186 participants (26.3%) had body weight stable ( ± 1 kg). Body weight change distribution is reported in the Appendix (Supplemental Fig. A). The physical and clinical characteristics of the two groups are shown in Tables 1 and 2, and the dietary data are reported in Table 3. In particular, the reported prevalence of type 2 diabetes in at least one first or second-degree family member was not significantly different between G and NG (58.2% vs. 51.8%; χ2 = 2.99; P = 0.22). The two groups were comparable in terms of sex distribution and drug use; however, G were significantly younger than NG. Initial body weight and BMI were similar in both groups; nevertheless, 4 years later, G exhibited an average body weight gain of ~10 kg, while NG slightly but significantly decreased their body weight. The initial habitual energy intake was similar in both groups; however, 4 years later, the G group exhibited significantly higher habitual energy intake than the NG group. The correlation between body weight change and habitual energy intake is presented in the Appendix (Supplemental Fig. B). Dietary habits changed in both groups, as demonstrated by a reduction in the habitual intake of fats and an increase in carbohydrate intake. The MEDI-Lite score increased significantly in the NG group and remained unchanged in the G group. The physical activity level was not significantly different between G and NG (data not shown). The correlation between body weight change and HOMA-IR is presented in the Appendix (Supplemental Fig. C). The basal insulin serum concentrations and the HOMA-IR markedly increased in the G group, which also exhibited a higher prevalence of the alleles CG and GG (CG + GG, 56.1 vs. 43.0%; P < 0.05) of the PNAPL3 gene than the NG group. The change (Δ) in body weight was correlated with Δ insulin concentrations (r = 0.36; P < 0.001), Δ HOMA-IR (r = 0.32; P < 0.001), Δ MED-LITE score (r = −0.08; P < 0.05), Δ habitual energy intake (r = 0.17; P < 0.001), Δ glycemic index of diet (r = 0.08; P < 0.05), Δ glycemic load of diet (r = 0.14; P < 0.001), age (r = −0.19; P < 0.001). The multivariate logistic analysis demonstrated that becoming a body weight gainer (0 = not; 1 = yes) was independently associated with age, energy intake change (0 = \(\le \,\) kcal/day; 1 = > 0 kcal/day) and carrying the CG or GG alleles of the PNAPL3 gene (0 = not; 1 = yes) (Table 4).
The final HOMA-IR value was correlated with final values of age (r = 0.17; P < 0.001), sex (male = 0, female = 1; r = −0.11; P < 0.005), BMI (r = 0.49; P < 0.001), waist circumference (r = 0.51; P < 0.001), waist-to-hip ratio (r = 0.40; P < 0.001), FFM-kg (r = 0.28; P < 0.001), FM% (r = 0.30; P < 0.001), energy intake (r = 0.11; P < 0.005). No significant correlation was observed with MEDI-LITE score (r = −0.05, P = 0.17), PNPLA3 CG + GG alleles (0=not, 1=yes; r = 0.07, P = 0.09), glycemic index (r = −0.02, P = 0.62), and glucose load (r = 0.06, P = 0.10). Multiple stepwise regression analysis demonstrated that only the final BMI (P < 0.001), waist circumference (P < 0.001), and energy intake (P < 0.05) were independently correlated with HOMA-IR according to the following equation:
HOMA-IR = −3.13 + (0.067 × BMI) + (0.033 × waist circumference) + (0.0001 × energy intake), R2 = 0.31 (P < 0.001).
Discussion
In this study, G comprised ~12% of the initial cohort; they experienced a significant increase in body weight, ~10 kg more than the NG. The G and NG groups had comparable initial body weights, BMI, body fat distributions (Table 1), and habitual energy intakes. However, as expected, 4 years later, G significantly increased their energy intake, which was higher than that of NG (Table 3), thus confirming that energy intake is the main critical factor influencing energy balance and body weight change. In general, participants in the ABCD study improved their dietary choices following initial, albeit generic, nutritional suggestions provided during the ABCD_1 study. Therefore, the macronutrient composition of the habitual diet was similar in both groups. Four years later, both groups significantly reduced their habitual fat intake and increased their carbohydrate intake (protein intake remained unchanged). However, only NG significantly reduced the glycemic index of the diet and improved adherence to the Mediterranean diet, as indicated by the MEDI-Lite score. These data also suggest that individualized prevention campaigns promoting healthy lifestyles are effective. By addressing clinical issues, providing strategies, and offering personalized suggestions, they can guide lifestyle changes in a nonintensive manner.
We previously investigated this cohort for variants in the PNPLA3 and TM6SF2 genes to identify people at a higher risk of liver steatosis (PNPLA3) and fibrosis (TM6SF2), a condition frequently associated with obesity, diabetes, and metabolic syndrome [25]. Interestingly, in this study, the G group had a significantly higher prevalence of the CG and GG variants of PNPLA3 gene than that of the NG group. Multivariate analysis revealed that the change in body weight, such as in G, was independently associated with age, changes in energy intake, and the presence of the CG or GG alleles of the PNPLA3 gene. Consistent with our findings, Cinque et al. [26] investigated liver steatosis in a small cohort of individuals during the COVID-19 lockdown and found that the PNPLA3 G allele was independently associated with body weight gain. However, to the best of our knowledge, this is the first report of an independent association between these alleles and body weight gain or obesity in a general population cohort. This association does not appear to be related to chance, as it may have a congruent biological explanation. Indeed, PNPLA3 is expressed in response to feeding and is involved in lipid autophagy (lipophagy), particularly in the liver, and to a lesser extent in adipose tissue, especially when there is an excess of dietary fatty acids [27,28,29]. Therefore, a defective protein may not ensure an efficient mechanism of autophagy that protects liver cells from excessive fat accumulation. Hence, we hypothesized that PNPLA3 might contribute to the destruction of a small but significant amount of dietary-derived fats introduced in excess, thus contributing to mitigating a positive energy balance and consequent body weight gain. If we postulate that autophagy mechanisms can eliminate as little as 5 g (or even less) of fatty acids daily, it could potentially prevent around 2.0–2.5 kg of body weight gain per year. This aligns with the amount of weight gained over 4 years by the participants in the G group of our study. However, it is essential to emphasize that this is merely a hypothesis that requires further investigation and remains speculative at this stage.
The relationship between insulin resistance (IR) and obesity has not yet been elucidated. However, our study clearly demonstrates that IR does not precede weight gain; rather, it is a consequence of weight gain. In fact, initially, the G and NG groups had the same anthropometric characteristics and did not have different values of both serum insulin concentrations and HOMA-IR. However, 4 years later, insulin levels as HOMA-IR increased significantly in the G group, which exhibited values higher than those in the NG group. As expected, the final HOMA-IR independently correlated with measures of adiposity (BMI) of central fat distribution, such as waist circumference, and, interestingly, with the amount of habitual energy intake, regardless of the type of macronutrient excess. Therefore, the higher the energy intake, the greater the IR, which supports the possibility that IR is a protective response in favor of the intracellular environment when exposed to an excess of energy substrate. If an excessive amount of glucose rapidly accumulates inside the cell, there is a risk of osmotic damage. Second, IR is a protective mechanism against oxidative damage caused by excessive nutrient and energy accumulation. Supporting this hypothesis, mitochondrial oxidative stress is known to occur due to intracellular energy substrate overflow [30]. Furthermore, a high glucose flux might force pathways, including glycogen synthesis, polyol, and hexosamine pathways, and the production of advanced glycation end-product precursors (AGEs), resulting in cellular damage [31,32,33]. Hoehn et al. [34] demonstrated in vitro and in a murine model that mitochondrial superoxide production in response to energy substrate overflow drives IR, as it is a sensor of cellular nutrient homeostasis. Therefore, IR protects the intracellular environment from oxidative stress, and mitochondrial superoxide may be a signal that drives a cellular response to dampen glucose uptake via the antagonism of GLUT4. One logical consequence is that there might be a need to reconsider the idea of pharmacologically eliminating IR. Attempting to remove this protective mechanism could have adverse effects and should be approached with caution. Similar to all compensatory mechanisms, persistent IR is expected to favor other well-known clinical problems of metabolic syndromes, such as type 2 diabetes and atherosclerosis. Therefore, the only possible rational approach to treat IR seems to be to reduce energy intake with diet, possibly using anti-obesity drugs that regulate food intake when diet alone fails.
This study had some important limitations. First, only PNPLA3 and TM6SF2 genes were evaluated, and other known genes involved in beta cell function and IR were not considered. However, these two genes were included in other investigations of liver steatosis in the ABCD study. This study did not aim to investigate the specific genetic causes of body weight gain and insulin resistance; however, we did not exclude the need for further in-depth genetic investigations of this cohort. Another important limitation is that we used HOMA-IR as a surrogate assessment of insulin resistance instead of the gold standard technique, that is, the euglycemic hyperinsulinemic clamp (EHC). However, EHC has been previously shown to correlate well with HOMA-IR values [35]; it is not a simple technique to perform in large cohorts, and to our knowledge, there is a paucity of studies using this technique beyond the first 6 months post weight loss bariatric surgery interventions [36, 37]. Unfortunately, we did not perform body composition analysis in the ABCD_1 study; therefore, we could not include body composition changes in our analysis. However, the evolution of body circumference was consistent with body weight change, and we are confident that the data on body composition modification would not have contradicted the conclusions of this study.
This study demonstrated that excessive energy intake is primarily associated with body weight gain and that genetic factors might favor a positive energy balance. Body weight gain is followed by insulin resistance, which is correlated with energy intake, and is probably a protective mechanism against intracellular oxidative stress resulting from energy substrate overflow.
Data availability
Individual de-identified participant data underlying the results reported in this article will be shared with researchers who provide a methodologically sound proposal. Data will be available beginning at 9 months and ending at 36 months after the publication of the article. Proposals should be directed toward silvio.buscemi@unipa.it. To gain access, the data requestors must sign a data-access agreement.
References
World Obesity Federation, World Obesity Atlas 2023. https://data.worldobesity.org/publications/?cat=19. Accessed September 5, 2019.
Piaggi P. Metabolic determinants of weight gain in humans. Obesity. 2019;27:691–9.
Page MM, Johnson JD. Mild suppression of hyperinsulinemia to treat obesity and insulin resistance. Trends Endocrinol Metab. 2018;29:389–99.
Corkey BE. Diabetes: have we got it all wrong? Insulin hypersecretion and food additives: cause of obesity and diabetes? Diabetes Care. 2012;35:2432–7.
Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med. 2017;23:804–14.
Ludwig DS, Ebbeling CB. The carbohydrate-insulin model of obesity: beyond “calories in, calories out. JAMA Intern Med. 2018;178:1098–103.
Ravussin E, Swinburn BA. Metabolic predictors of obesity: cross-sectional versus longitudinal data. Int J Obes Relat Metab Disord. 1993;17 Suppl 3:S28–42.
Lazarus R, Sparrow D, Weiss S. Temporal relations between obesity and insulin: longitudinal data from the Normative Aging Study. Am J Epidemiol. 1998;147:173–9.
Sedaka NM, Olsen CH, Yannai LE, Stutzman WE, Krause AJ, Sherafat-Kazemzadeh R, et al. A longitudinal study of serum insulin and insulin resistance as predictors of weight and body fat gain in African American and Caucasian children. Int J Obes. 2017;41:61–70.
Labayen I, Ruiz JR, Ortega FB, Harro J, Merenäkk L, Oja L, et al. Insulin sensitivity at childhood predicts changes in total and central adiposity over a 6-year period. Int J Obes. 2011;35:1284–8.
Herman R, Kravos NA, Jensterle M, Janež A, Dolžan V. Metformin and insulin resistance: a review of the underlying mechanisms behind changes in GLUT4-mediated glucose transport. Int J Mol Sci. 2022;23:1264.
Buscemi S, Nicolucci A, Mattina A, Rosafio G, Massenti FM, Lucisano G, et al. Association of dietary patterns with insulin resistance and clinically silent carotid atherosclerosis in apparently healthy people. Eur J Clin Nutr. 2013;67:1284–90.
Buscemi S, Geraci G, Massenti FM, Buscemi C, Costa F, D’Orio C, et al. Renal function and carotid atherosclerosis in adults with no known kidney disease. Nutr Metab Cardiovasc Dis. 2017;27:267–73.
Buscemi S, Corleo D, Vasto S, Buscemi C, Massenti MF, Nuzzo D, et al. Factors associated with circulating concentrations of irisin in the general population cohort of the ABCD study. Int J Obes. 2018;42:398–404.
Buscemi S, Rosafio G, Vasto S, Massenti FM, Grosso G, Galvano F, et al. Validation of a food frequency questionnaire for use in Italian adults living in Sicily. Int J Food Sci Nutr. 2015;66:426–38.
Sofi F, Dinu M, Pagliai G, Marcucci R, Casini A. Validation of a literature-based adherence score to Mediterranean diet: the MEDI-LITE score. Int J Food Sci Nutr. 2017;68:757–62.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37:S81–S90.
World Health Organization. Global health observatory. https://www.who.int/data/gho/data/themes/theme-details/GHO/gho-nutrition. Accessed September 1, 2023.
Buscemi S, Blunda G, Maneri R, Verga S. Bioelectrical characteristics of type 1 and type 2 diabetic subjects with reference to body water compartments. Acta Diabetol. 1998;35:220–3.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Rössner S. Defining success in obesity management. Int J Obes Relat Metab Disord. 1997;21 Suppl 1:S2–S4.
Jia G, Shu X, Liu Y, Li HL, Cai H, Gao J, et al. Association of adult weight gain with major health outcomes among middle-aged Chinese persons with Low body weight in early adulthood. JAMA Netw Open. 2019;2:e1917371.
Petta S, Di Marco V, Pipitone RM, Grimaudo S, Buscemi C, Craxì A, et al. Prevalence and severity of nonalcoholic fatty liver disease by transient elastography: genetic and metabolic risk factors in a general population. Liver Int. 2018;38:2060–8.
Cinque F, Cespiati A, Lombardi R, Costantino A, Maffi G, Alletto F, et al. Interaction between lifestyle changes and PNPLA3 genotype in NAFLD patients during the COVID-19 lockdown. Nutrients. 2022;14:556.
Negoita F, Blomdahl J, Wasserstrom S, Winberg ME, Osmark P, Larsson S, et al. PNPLA3 variant M148 causes resistance to starvation-mediated lipid droplet autophagy in human hepatocytes. J Cell Biochem. 2019;120:343–56.
BasuRay S, Wang Y, Smagris E, Cohen JC, Hobbs HH. Accumulation of PNPLA3 on lipid droplets is the basis of associated hepatic steatosis. Proc Natl Acad Sci USA 2019;116:9521–6.
Filali-Mouncef Y, Hunter C, Roccio F, Zagkou S, Dupont N, Primard C, et al. The ménage à trois of autophagy, lipid droplets and liver disease. Autophagy. 2022;18:50–72.
Savage DB, Petersen KF, Shulman GI. Disordered lipid metabolism and the pathogenesis of insulin resistance. Physiol Rev. 2007;87:507–20.
Nolan CJ, Prentki M. Insulin resistance and insulin hypersecretion in the metabolic syndrome and type 2 diabetes: Time for a conceptual framework shift. Diab Vasc Dis Res. 2019;16:118–27.
Chess DJ, Stanley WC. Role of diet and fuel overabundance in the development and progression of heart failure. Cardiovasc Res. 2008;79:269–78.
Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54:1615–25.
Hoehn KL, Salmon AB, Hohnen-Behrens C, Turner N, Hoy AJ, Maghzal GJ, et al. Insulin resistance is a cellular antioxidant defense mechanism. Proc Natl Acad Sci USA 2009;106:17787–92.
Tosi F, Bonora E, Moghetti P. Insulin resistance in a large cohort of women with polycystic ovary syndrome: a comparison between euglycaemic-hyperinsulinaemic clamp and surrogate indexes. Hum Reprod. 2017;32:2515–21.
Su Z, Zhu L, Gao X, Li P, Li W, Sun L, et al. Effect of laparoscopic Roux-en-Y gastric bypass on improvement of insulin resistance in Type 2 diabetic patients evaluated by hyperinsulinemic-euglycemic clamp. Zhong Nan Da Xue Xue. Bao Yi Xue Ban. 2021;46:609–14.
Dirksen C, Eiken A, Bojsen-Møller KN, Svane MS, Martinussen C, Jørgensen NB, et al. No islet cell hyperfunction, but altered gut-islet regulation and postprandial hypoglycemia in glucose-tolerant patients 3 years after gastric bypass surgery. Obes Surg. 2016;26:2263–7.
Acknowledgements
This research received no external funds.
Author information
Authors and Affiliations
Contributions
Conceptualization, CB, CR, and SB; data collection and literature search, AMB, RCa, PC, ML, and RC; laboratory tests, RCa; data analysis and interpretation, CB, CR, SBo, VP, SB, AMB, and AEM; writing of the manuscript, CB, SB, SBo, AMB, and AEM; SB, general responsibility of the study. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Buscemi, C., Randazzo, C., Barile, A.M. et al. Factors associated with body weight gain and insulin-resistance: a longitudinal study. Nutr. Diabetes 14, 21 (2024). https://doi.org/10.1038/s41387-024-00283-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41387-024-00283-5