Abstract
Osteoarthritis (OA) is associated with cartilage destruction, subchondral bone remodeling and inflammation of the synovial membrane, although the etiology and pathogenesis underlying this debilitating disease are poorly understood. Secreted inflammatory molecules, such as proinflammatory cytokines, are among the critical mediators of the disturbed processes implicated in OA pathophysiology. Interleukin (IL)-1β and tumor necrosis factor (TNF), in particular, control the degeneration of articular cartilage matrix, which makes them prime targets for therapeutic strategies. Animal studies provide support for this approach, although only a few clinical studies have investigated the efficacy of blocking these proinflammatory cytokines in the treatment of OA. Apart from IL-1β and TNF, several other cytokines including IL-6, IL-15, IL-17, IL-18, IL-21, leukemia inhibitory factor and IL-8 (a chemokine) have also been shown to be implicated in OA and could possibly be targeted therapeutically. This Review discusses the current knowledge regarding the role of proinflammatory cytokines in the pathophysiology of OA and addresses the potential of anticytokine therapy in the treatment of this disease.
Key Points
-
Osteoarthritis (OA) is associated with cartilage destruction, subchondral bone remodeling and synovial membrane inflammation
-
Proinflammatory cytokines are critical mediators in the disturbed metabolism and enhanced catabolism of tissue in the OA joint
-
Interleukin (IL)-1β, tumor necrosis factor (TNF) and IL-6 seem to be the main proinflammatory cytokines involved in the pathophysiology of OA
-
Data from cellular and animal studies have provided substantial evidence that blocking IL-1β and TNF production could counteract the degradative mechanisms associated with OA pathology
-
Anticytokine therapies in OA clinical trials have so far yielded variable results
-
A better understanding of the individual roles and functions of cytokines, such as IL-1β, TNF and IL-6, is of the utmost importance in order to develop adequate and specific anticytokine therapies
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Felson, D. T. Clinical practice. Osteoarthritis of the knee. N. Engl. J. Med. 354, 841–848 (2006).
Ayral, X., Pickering, E. H., Woodworth, T. G., Mackillop, N. & Dougados, M. Synovitis: a potential predictive factor of structural progression of medial tibiofemoral knee osteoarthritis—results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthritis Cartilage 13, 361–367 (2005).
Pozgan, U. et al. Expression and activity profiling of selected cysteine cathepsins and matrix metalloproteinases in synovial fluids from patients with rheumatoid arthritis and osteoarthritis. Biol. Chem. 391, 571–579 (2010).
Martel-Pelletier, J., Lajeunesse, D. & Pelletier, J. P. in Arthritis and Allied Conditions. A Textbook of Rheumatology 15th edn (eds Koopman, W. J. & Moreland, L. W.) 2199–2226 (Lippincott Williams & Wilkins, Baltimore, USA, 2005).
Page Thomas, D. P., King, B., Stephens, T. & Dingle, J. T. In vivo studies of cartilage regeneration after damage induced by catabolin/interleukin-1. Ann. Rheum. Dis. 50, 75–80 (1991).
Henderson, B. & Pettipher, E. R. Arthritogenic actions of recombinant IL-1 and tumour necrosis factor α in the rabbit: evidence for synergistic interactions between cytokines in vivo. Clin. Exp. Immunol. 75, 306–310 (1989).
Clements, K. M. et al. Gene deletion of either interleukin-1β, interleukin-1β-converting enzyme, inducible nitric oxide synthase, or stromelysin 1 accelerates the development of knee osteoarthritis in mice after surgical transection of the medial collateral ligament and partial medial meniscectomy. Arthritis Rheum. 48, 3452–3463 (2003).
Arend, W. P. Interleukin-1 receptor antagonist. Adv. Immunol. 54, 167–227 (1993).
Martel-Pelletier, J. et al. The interleukin-1 receptor in normal and osteoarthritic human articular chondrocytes. Identification as the type I receptor and analysis of binding kinetics and biologic function. Arthritis Rheum. 35, 530–540 (1992).
Sadouk, M. B. et al. Human synovial fibroblasts coexpress IL-1 receptor type I and type II mRNA. The increased level of the IL-1 receptor in osteoarthritic cells is related to an increased level of the type I receptor. Lab. Invest. 73, 347–355 (1995).
Colotta, F., Dower, S. K., Sims, J. E. & Mantovani, A. The type II 'decoy' receptor: a novel regulatory pathway for interleukin 1. Immunol. Today 15, 562–566 (1994).
Palmer, G. et al. Production of interleukin-1 receptor antagonist by human articular chondrocytes. Arthritis Res. 4, 226–231 (2002).
Seitz, M. et al. Production of interleukin-1 receptor antagonist, inflammatory chemotactic proteins, and prostaglandin E by rheumatoid and osteoarthritic synoviocytes—regulation by IFN-γ and IL-4. J. Immunol. 152, 2060–2065 (1994).
Alaaeddine, N. et al. Osteoarthritic synovial fibroblasts possess an increased level of tumor necrosis factor-receptor 55 (TNF-R55) that mediates biological activation by TNFα. J. Rheumatol. 24, 1985–1994 (1997).
Naume, B., Shalaby, R., Lesslauer, W. & Espevik, T. Involvement of the 55- and 75-kDa tumor necrosis factor receptors in the generation of lymphokine-activated killer cell activity and proliferation of natural killer cells. J. Immunol. 146, 3045–3048 (1991).
Hohmann, H. P. et al. Expression of the types A and B tumor necrosis factor (TNF) receptors is independently regulated, and both receptors mediate activation of the transcription factor NF-κB. TNFα is not needed for induction of a biological effect via TNF receptors. J. Biol. Chem. 265, 22409–22417 (1990).
Westacott, C. I., Atkins, R. M., Dieppe, P. A. & Elson, C. J. Tumor necrosis factor α receptor expression on chondrocytes isolated from human articular cartilage. J. Rheumatol. 21, 1710–1715 (1994).
Saklatvala, J. Tumour necrosis factor α stimulates resorption and inhibits synthesis of proteoglycan in cartilage. Nature 322, 547–549 (1986).
Goldring, M. B., Fukuo, K., Birkhead, J. R., Dudek, E. & Sandell, L. J. Transcriptional suppression by interleukin-1 and interferon-γ of type II collagen gene expression in human chondrocytes. J. Cell. Biochem. 54, 85–99 (1994).
Chadjichristos, C. et al. Sp1 and Sp3 transcription factors mediate interleukin-1β down-regulation of human type II collagen gene expression in articular chondrocytes. J. Biol. Chem. 278, 39762–39772 (2003).
Shakibaei, M., Schulze-Tanzil, G., John, T. & Mobasheri, A. Curcumin protects human chondrocytes from IL-l1β -induced inhibition of collagen type II and β1-integrin expression and activation of caspase-3: an immunomorphological study. Ann. Anat. 187, 487–497 (2005).
Stöve, J., Huch, K., Günther, K. P. & Scharf, H. P. Interleukin-1β induces different gene expression of stromelysin, aggrecan and tumor-necrosis-factor-stimulated gene 6 in human osteoarthritic chondrocytes in vitro. Pathobiology 68, 144–149 (2000).
Nietfeld, J. J., Wilbrink, B., Den Otter, W., Huber, J. & Huber-Bruning, O. The effect of human interleukin 1 on proteoglycan metabolism in human and porcine cartilage explants. J. Rheumatol. 17, 818–826 (1990).
Gouze, J. N. et al. Interleukin-1β down-regulates the expression of glucuronosyltransferase I, a key enzyme priming glycosaminoglycan biosynthesis: influence of glucosamine on interleukin-1β-mediated effects in rat chondrocytes. Arthritis Rheum. 44, 351–360 (2001).
Séguin, C. A. & Bernier, S. M. TNFα suppresses link protein and type II collagen expression in chondrocytes: Role of MEK1/2 and NF-κB signaling pathways. J. Cell. Physiol. 197, 356–369 (2003).
Mengshol, J. A., Vincenti, M. P., Coon, C. I., Barchowsky, A. & Brinckerhoff, C. E. Interleukin-1 induction of collagenase 3 (matrix metalloproteinase 13) gene expression in chondrocytes requires p38, c-Jun N-terminal kinase, and nuclear factor κB: differential regulation of collagenase 1 and collagenase 3. Arthritis Rheum. 43, 801–811 (2000).
Lefebvre, V., Peeters-Joris, C. & Vaes, G. Modulation by interleukin 1 and tumor necrosis factor α of production of collagenase, tissue inhibitor of metalloproteinases and collagen types in differentiated and dedifferentiated articular chondrocytes. Biochim. Biophys. Acta 1052, 366–378 (1990).
Reboul, P., Pelletier, J. P., Tardif, G., Cloutier, J. M. & Martel-Pelletier, J. The new collagenase, collagenase-3, is expressed and synthesized by human chondrocytes but not by synoviocytes. A role in osteoarthritis. J. Clin. Invest. 97, 2011–2019 (1996).
Glasson, S. S. et al. Characterization of and osteoarthritis susceptibility in ADAMTS-4-knockout mice. Arthritis Rheum. 50, 2547–2558 (2004).
Glasson, S. S. et al. Deletion of active ADAMTS5 prevents cartilage degradation in a murine model of osteoarthritis. Nature 434, 644–648 (2005).
Tortorella, M. D., Malfait, A. M., Deccico, C. & Arner, E. The role of ADAM-TS4 (aggrecanase-1) and ADAM-TS5 (aggrecanase-2) in a model of cartilage degradation. Osteoarthritis Cartilage 9, 539–552 (2001).
Bondeson, J., Wainwright, S. D., Lauder, S., Amos, N. & Hughes, C. E. The role of synovial macrophages and macrophage-produced cytokines in driving aggrecanases, matrix metalloproteinases, and other destructive and inflammatory responses in osteoarthritis. Arthritis Res. Ther. 8, R187 (2006).
Guerne, P. A., Carson, D. A. & Lotz, M. IL-6 production by human articular chondrocytes. Modulation of its synthesis by cytokines, growth factors, and hormones in vitro. J. Immunol. 144, 499–505 (1990).
Lotz, M., Terkeltaub, R. & Villiger, P. M. Cartilage and joint inflammation. Regulation of IL-8 expression by human articular chondrocytes. J. Immunol. 148, 466–473 (1992).
Villiger, P. M., Terkeltaub, R. & Lotz, M. Monocyte chemoattractant protein-1 (MCP-1) expression in human articular cartilage. Induction by peptide regulatory factors and differential effects of dexamethasone and retinoic acid. J. Clin. Invest. 90, 488–496 (1992).
Alaaeddine, N., Olee, T., Hashimoto, S., Creighton-Achermann, L. & Lotz, M. Production of the chemokine RANTES by articular chondrocytes and role in cartilage degradation. Arthritis Rheum. 44, 1633–1643 (2001).
Afonso, V., Champy, R., Mitrovic, D., Collin, P. & Lomri, A. Reactive oxygen species and superoxide dismutases: role in joint diseases. Joint Bone Spine 74, 324–329 (2007).
Mathy-Hartert, M. et al. Interleukin-1β and interleukin-6 disturb the antioxidant enzyme system in bovine chondrocytes: a possible explanation for oxidative stress generation. Osteoarthritis Cartilage 16, 756–763 (2008).
Scott, J. L. et al. Superoxide dismutase downregulation in osteoarthritis progression and end-stage disease. Ann. Rheum. Dis. 69, 1502–1510 (2010).
Roman-Blas, J. A. & Jimenez, S. A. NF-κB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthritis Cartilage 14, 839–848 (2006).
Chen, L. X. et al. Suppression of early experimental osteoarthritis by in vivo delivery of the adenoviral vector-mediated NF-κBp65-specific siRNA. Osteoarthritis Cartilage 16, 174–184 (2008).
Blom, A. B. et al. Involvement of the Wnt signaling pathway in experimental and human osteoarthritis: prominent role of Wnt-induced signaling protein 1. Arthritis Rheum. 60, 501–512 (2009).
Yuasa, T., Otani, T., Koike, T., Iwamoto, M. & Enomoto-Iwamoto, M. Wnt/β-catenin signaling stimulates matrix catabolic genes and activity in articular chondrocytes: its possible role in joint degeneration. Lab. Invest. 88, 264–274 (2008).
Lane, N. E., Nevitt, M. C., Lui, L. Y., de Leon, P. & Corr, M. Wnt signaling antagonists are potential prognostic biomarkers for the progression of radiographic hip osteoarthritis in elderly Caucasian women. Arthritis Rheum. 56, 3319–3325 (2007).
Fahmi, H., Pelletier, J. P. & Martel-Pelletier, J. PPARg ligands as modulators of inflammatory and catabolic responses in arthritis. An overview. J. Rheumatol. 29, 3–14 (2002).
Kobayashi, T. et al. Pioglitazone, a peroxisome proliferator-activated receptor γ agonist, reduces the progression of experimental osteoarthritis in guinea pigs. Arthritis Rheum. 52, 479–487 (2005).
Boileau, C. et al. The peroxisome proliferator-activated receptor γ agonist pioglitazone reduces the development of cartilage lesions in an experimental dog model of osteoarthritis: in vivo protective effects mediated through the inhibition of key signaling and catabolic pathways. Arthritis Rheum. 56, 2288–2298 (2007).
Kobayashi, M. et al. Role of interleukin-1 and tumor necrosis factor α in matrix degradation of human osteoarthritic cartilage. Arthritis Rheum. 52, 128–135 (2005).
Caron, J. P. et al. Chondroprotective effect of intraarticular injections of interleukin-1 receptor antagonist in experimental osteoarthritis. Suppression of collagenase-1 expression. Arthritis Rheum. 39, 1535–1544 (1996).
Pelletier, J. P. et al. In vivo suppression of early experimental osteoarthritis by interleukin-1 receptor antagonist using gene therapy. Arthritis Rheum. 40, 1012–1019 (1997).
Fernandes, J. et al . In vivo transfer of interleukin-1 receptor antagonist gene in osteoarthritic rabbit knee joints: prevention of osteoarthritis progression. Am. J. Pathol. 154, 1159–1169 (1999).
Zhang, X., Mao, Z. & Yu, C. Suppression of early experimental osteoarthritis by gene transfer of interleukin-1 receptor antagonist and interleukin-10. J. Orthop. Res. 22, 742–750 (2004).
Frisbie, D. D., Ghivizzani, S. C., Robbins, P. D., Evans, C. H. & McIlwraith, C. W. Treatment of experimental equine osteoarthritis by in vivo delivery of the equine interleukin-1 receptor antagonist gene. Gene Ther. 9, 12–20 (2002).
Chevalier, X. et al. Safety study of intraarticular injection of interleukin 1 receptor antagonist in patients with painful knee osteoarthritis: a multicenter study. J. Rheumatol. 32, 1317–1323 (2005).
Chevalier, X. et al. Intraarticular injection of anakinra in osteoarthritis of the knee: a multicenter, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 61, 344–352 (2009).
Bacconnier, L., Jorgensen, C. & Fabre, S. Erosive osteoarthritis of the hand: clinical experience with anakinra. Ann. Rheum. Dis. 68, 1078–1079 (2009).
Attur, M. G. et al. Functional genomic analysis of type II IL-1β decoy receptor: potential for gene therapy in human arthritis and inflammation. J. Immunol. 168, 2001–2010 (2002).
Grunke, M. & Schulze-Koops, H. Successful treatment of inflammatory knee osteoarthritis with tumour necrosis factor blockade. Ann. Rheum. Dis. 65, 555–556 (2006).
Fioravanti, A., Fabbroni, M., Cerase, A. & Galeazzi, M. Treatment of erosive osteoarthritis of the hands by intra-articular infliximab injections: a pilot study. Rheumatol. Int. 29, 961–965 (2009).
Magnano, M. D. et al. A pilot study of tumor necrosis factor inhibition in erosive/inflammatory osteoarthritis of the hands. J. Rheumatol. 34, 1323–1327 (2007).
Efficacy study of an anti-tumor necrosis factor (TNF)-α agent in patients with hand osteoarthritis (DORA). http://clinicaltrials.gov [online], (2010).
Skiles, J. W., Gonnella, N. C. & Jeng, A. Y. The design, structure, and clinical update of small molecular weight matrix metalloproteinase inhibitors. Curr. Med. Chem. 11, 2911–2977 (2004).
Wojtowicz-Praga, S. et al. Phase I trial of Marimastat, a novel matrix metalloproteinase inhibitor, administered orally to patients with advanced lung cancer. J. Clin. Oncol. 16, 2150–2156 (1998).
Murphy, G. & Nagase, H. Reappraising metalloproteinases in rheumatoid arthritis and osteoarthritis: destruction or repair? Nat. Clin. Pract. Rheumatol. 4, 128–135 (2008).
Krzeski, P. et al. Development of musculoskeletal toxicity without clear benefit after administration of PG-116800, a matrix metalloproteinase inhibitor, to patients with knee osteoarthritis: a randomized, 12-month, double-blind, placebo-controlled study. Arthritis Res. Ther. 9, R109 (2007).
Clutterbuck, A. L., Asplin, K. E., Harris, P., Allaway, D. & Mobasheri, A. Targeting matrix metalloproteinases in inflammatory conditions. Curr. Drug Targets 10, 1245–1254 (2009).
Johnson, A. R. et al. Discovery and characterization of a novel inhibitor of matrix metalloprotease-13 that reduces cartilage damage in vivo without joint fibroplasia side effects. J. Biol. Chem. 282, 27781–27791 (2007).
Tortorella, M. D., Malfait, F., Barve, R. A., Shieh, H. S. & Malfait, A. M. A review of the ADAMTS family, pharmaceutical targets of the future. Curr. Pharm. Des. 15, 2359–2374 (2009).
Marcu, K. B., Otero, M., Olivotto, E., Borzi, R. M. & Goldring, M. B. NF-κB signaling: multiple angles to target OA. Curr. Drug Targets 11, 599–613 (2010).
Wegenka, U. M., Buschmann, J., Lütticken, C., Heinrich, P. C. & Horn, F. Acute-phase response factor, a nuclear factor binding to acute-phase response elements, is rapidly activated by interleukin-6 at the posttranslational level. Mol. Cell. Biol. 13, 276–288 (1993).
Zhong, Z., Wen, Z. & Darnell, J. E. Jr. Stat3: a STAT family member activated by tyrosine phosphorylation in response to epidermal growth factor and interleukin-6. Science 264, 95–98 (1994).
Bender, S. et al. Interleukin-1β induces synthesis and secretion of interleukin-6 in human chondrocytes. FEBS Lett. 263, 321–324 (1990).
Wang, P., Zhu, F. & Konstantopoulos, K. Prostaglandin E2 induces interleukin-6 expression in human chondrocytes via cAMP/protein kinase A- and phosphatidylinositol 3-kinase-dependent NF-κB activation. Am. J. Physiol. Cell Physiol. 298, C1445–C1456 (2010).
Wang, P., Zhu, F., Lee, N. H. & Konstantopoulos, K. Shear-induced interleukin-6 synthesis in chondrocytes: roles of E prostanoid (EP) 2 and EP3 in cAMP/protein kinase A- and PI3-K/Akt-dependent NF-κB activation. J. Biol. Chem. 285, 24793–24804 (2010).
Steensberg, A., Fischer, C. P., Keller, C., Møller, K. & Pedersen, B. K. IL-6 enhances plasma IL-1ra, IL-10, and cortisol in humans. Am. J. Physiol. Endocrinol. Metab. 285, E433–E437 (2003).
Haider, D. G. et al. C-reactive protein is expressed and secreted by peripheral blood mononuclear cells. Clin. Exp. Immunol. 146, 533–539 (2006).
Pearle, A. D. et al. Elevated high-sensitivity C-reactive protein levels are associated with local inflammatory findings in patients with osteoarthritis. Osteoarthritis Cartilage 15, 516–523 (2007).
Pelletier, J. P. et al. Decrease in serum level of matrix metalloproteinases is predictive of the disease-modifying effect of osteoarthritis drugs assessed by quantitative MRI in patients with knee osteoarthritis. Ann. Rheum. Dis. doi:10.1136/ard.2009.122002.
Kugisaki, H. et al. Serum concentrations of interleukin-6 in patients following unilateral versus bilateral total knee arthroplasty. J. Orthop. Sci. 14, 437–442 (2009).
Livshits, G. et al. Interleukin-6 is a significant predictor of radiographic knee osteoarthritis: The Chingford Study. Arthritis Rheum. 60, 2037–2045 (2009).
Kaneko, S. et al. Interleukin-6 and interleukin-8 levels in serum and synovial fluid of patients with osteoarthritis. Cytokines Cell. Mol. Ther. 6, 71–79 (2000).
Cawston, T. E. et al. The role of oncostatin M in animal and human connective tissue collagen turnover and its localization within the rheumatoid joint. Arthritis Rheum. 41, 1760–1771 (1998).
Rowan, A. D. et al. Synergistic effects of glycoprotein 130 binding cytokines in combination with interleukin-1 on cartilage collagen breakdown. Arthritis Rheum. 44, 1620–1632 (2001).
Sui, Y. et al. Mechanical injury potentiates proteoglycan catabolism induced by interleukin-6 with soluble interleukin-6 receptor and tumor necrosis factor α in immature bovine and adult human articular cartilage. Arthritis Rheum. 60, 2985–2996 (2009).
Porée, B. et al. Interleukin-6 (IL-6) and/or soluble IL-6 receptor down-regulation of human type II collagen gene expression in articular chondrocytes requires a decrease of Sp1.Sp3 ratio and of the binding activity of both factors to the COL2A1 promoter. J. Biol. Chem. 283, 4850–4865 (2008).
Alonzi, T. et al. Interleukin 6 is required for the development of collagen-induced arthritis. J. Exp. Med. 187, 461–468 (1998).
van de Loo, F. A., Kuiper, S., van Enckevort, F. H., Arntz, O. J. & van den Berg, W. B. Interleukin-6 reduces cartilage destruction during experimental arthritis. A study in interleukin-6-deficient mice. Am. J. Pathol. 151, 177–191 (1997).
de Hooge, A. S. et al. Male IL-6 gene knock out mice developed more advanced osteoarthritis upon aging. Osteoarthritis Cartilage 13, 66–73 (2005).
Tilg, H., Dinarello, C. A. & Mier, J. W. IL-6 and APPs: anti-inflammatory and immunosuppressive mediators. Immunol. Today 18, 428–432 (1997).
Kwan Tat, S., Padrines, M., Théoleyre, S., Heymann, D. & Fortun, Y. IL-6, RANKL, TNFα/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 15, 49–60 (2004).
Liu, X. H., Kirschenbaum, A., Yao, S. & Levine, A. C. The role of the interleukin-6/gp130 signaling pathway in bone metabolism. Vitam. Horm. 74, 341–355 (2006).
Massicotte, F. et al. Can altered production of interleukin-1β, interleukin-6, transforming growth factor β and prostaglandin E(2) by isolated human subchondral osteoblasts identify two subgroups of osteoarthritic patients. Osteoarthritis Cartilage 10, 491–500 (2002).
Kwan Tat, S. et al. The differential expression of osteoprotegerin (OPG) and receptor activator of nuclear factor κB ligand (RANKL) in human osteoarthritic subchondral bone osteoblasts is an indicator of the metabolic state of these disease cells. Clin. Exp. Rheumatol. 26, 295–304 (2008).
Chenoufi, H. L. et al. Increased mRNA expression and protein secretion of interleukin-6 in primary human osteoblasts differentiated in vitro from rheumatoid and osteoarthritic bone. J. Cell. Biochem. 81, 666–678 (2001).
Jochems, C., Lagerquist, M., Håkansson, C., Ohlsson, C. & Carlsten, H. Long-term anti-arthritic and anti-osteoporotic effects of raloxifene in established experimental postmenopausal polyarthritis. Clin. Exp. Immunol. 152, 593–597 (2008).
Genovese, M. C. et al. Interleukin-6 receptor inhibition with tocilizumab reduces disease activity in rheumatoid arthritis with inadequate response to disease-modifying antirheumatic drugs: the tocilizumab in combination with traditional disease-modifying antirheumatic drug therapy study. Arthritis Rheum. 58, 2968–2980 (2008).
Smolen, J. S. et al. Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double-blind, placebo-controlled, randomised trial. Lancet 371, 987–997 (2008).
Garnero, P., Thompson, E., Woodworth, T. & Smolen, J. S. Rapid and sustained improvement in bone and cartilage turnover markers with the anti-interleukin-6 receptor inhibitor tocilizumab plus methotrexate in rheumatoid arthritis patients with an inadequate response to methotrexate: results from a substudy of the multicenter double-blind, placebo-controlled trial of tocilizumab in inadequate responders to methotrexate alone. Arthritis Rheum. 62, 33–43 (2010).
Doschak, M. R., Wohl, G. R., Hanley, D. A., Bray, R. C. & Zernicke, R. F. Antiresorptive therapy conserves some periarticular bone and ligament mechanical properties after anterior cruciate ligament disruption in the rabbit knee. J. Orthop. Res. 22, 942–948 (2004).
Jones, M. D. et al. In vivo microfocal computed tomography and micro-magnetic resonance imaging evaluation of antiresorptive and antiinflammatory drugs as preventive treatments of osteoarthritis in the rat. Arthritis Rheum. 62, 2726–2735 (2010).
Bingham, C. O. 3rd et al. Risedronate decreases biochemical markers of cartilage degradation but does not decrease symptoms or slow radiographic progression in patients with medial compartment osteoarthritis of the knee: results of the two-year multinational knee osteoarthritis structural arthritis study. Arthritis Rheum. 54, 3494–3507 (2006).
Garnero, P. et al. Relationships between biochemical markers of bone and cartilage degradation with radiological progression in patients with knee osteoarthritis receiving risedronate: the Knee Osteoarthritis Structural Arthritis randomized clinical trial. Osteoarthritis Cartilage 16, 660–666 (2008).
Raynauld, J. P. et al. Protective effects of licofelone, a 5-lipoxygenase and cyclo-oxygenase inhibitor, versus naproxen on cartilage loss in knee osteoarthritis: a first multicentre clinical trial using quantitative MRI. Ann. Rheum. Dis. 68, 938–947 (2009).
Scanzello, C. R. et al. Local cytokine profiles in knee osteoarthritis: elevated synovial fluid interleukin-15 differentiates early from end-stage disease. Osteoarthritis Cartilage 17, 1040–1048 (2009).
Martel-Pelletier, J., Mineau, F., Jovanovic, D., Di Battista, J. A. & Pelletier, J. P. Mitogen-activated protein kinase and nuclear factor κB together regulate interleukin-17-induced nitric oxide production in human osteoarthritic chondrocytes: possible role of transactivating factor mitogen-activated protein kinase-activated proten kinase (MAPKAPK). Arthritis Rheum. 42, 2399–2409 (1999).
Lubberts, E., Joosten, L. A., van de Loo, F. A., van den Gersselaar, L. A. & van den Berg, W. B. Reduction of interleukin-17-induced inhibition of chondrocyte proteoglycan synthesis in intact murine articular cartilage by interleukin-4. Arthritis Rheum. 43, 1300–1306 (2000).
Olee, T., Hashimoto, S., Quach, J. & Lotz, M. IL-18 is produced by articular chondrocytes and induces proinflammatory and catabolic responses. J. Immunol. 162, 1096–1100 (1999).
Alaaeddine, N. et al. Differential effects of IL-8, LIF (pro-inflammatory) and IL-11 (anti-inflammatory) on TNF-α-induced PGE2 release and on signalling pathways in human OA synovial fibroblasts. Cytokine 11, 1020–1030 (1999).
Ishii, H. et al. Characterization of infiltrating T cells and TH1/TH2-type cytokines in the synovium of patients with osteoarthritis. Osteoarthritis Cartilage 10, 277–281 (2002).
Alsalameh, S. et al. Cellular immune response toward human articular chondrocytes. T cell reactivities against chondrocyte and fibroblast membranes in destructive joint diseases. Arthritis Rheum. 33, 1477–1486 (1990).
Pacquelet, S. et al. Interleukin 17, a nitric oxide-producing cytokine with a peroxynitrite-independent inhibitory effect on proteoglycan synthesis. J. Rheumatol. 29, 2602–2610 (2002).
Benderdour, M. et al. Interleukin 17 (IL-17) induces collagenase-3 production in human osteoarthritic chondrocytes via AP-1 dependent activation: differential activation of AP-1 members by IL-17 and IL-1β. J. Rheumatol. 29, 1262–1272 (2002).
Honorati, M. C., Bovara, M., Cattini, L., Piacentini, A. & Facchini, A. Contribution of interleukin 17 to human cartilage degradation and synovial inflammation in osteoarthritis. Osteoarthritis Cartilage 10, 799–807 (2002).
Kauffmann, C. et al. Computer-aided method for quantification of cartilage thickness and volume changes using MRI: validation study using a synthetic model. IEEE Trans. Biomed. Eng. 50, 978–988 (2003).
Raynauld, J. P. et al. Reliability of a quantification imaging system using magnetic resonance images to measure cartilage thickness and volume in human normal and osteoarthritic knees. Osteoarthritis Cartilage 11, 351–360 (2003).
Berthiaume, M. J. et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann. Rheum. Dis. 64, 556–563 (2005).
Raynauld, J. P. et al. Correlation between bone lesion changes and cartilage volume loss in patients with osteoarthritis of the knee as assessed by quantitative magnetic resonance imaging over a 24-month period. Ann. Rheum. Dis. 67, 683–688 (2008).
Pelletier, J. P. et al. A new non-invasive method to assess synovitis severity in relation to symptoms and cartilage volume loss in knee osteoarthritis patients using MRI. Osteoarthritis Cartilage 16 (Suppl. 3), S8–S13 (2008).
Li, W. et al. Human hip joint cartilage: MRI quantitative thickness and volume measurements discriminating acetabulum and femoral head. IEEE Trans. Biomed. Eng. 55, 2731–2740 (2008).
Li, W. et al. Fully automated system for the quantification of human osteoarthritic knee joint effusion volume using magnetic resonance imaging. Arthritis Res. Ther. 12, R173 (2010).
Acknowledgements
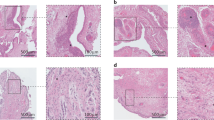
The authors would like to thank Francois Mineau for his work on the figure for this review article.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to researching data for the article, providing a substantial contribution to discussions of the content, writing the article, and to the review and/or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Kapoor, M., Martel-Pelletier, J., Lajeunesse, D. et al. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7, 33–42 (2011). https://doi.org/10.1038/nrrheum.2010.196
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2010.196
This article is cited by
-
Vitamin B6 alleviates osteoarthritis by suppressing inflammation and apoptosis
BMC Musculoskeletal Disorders (2024)
-
Saikosaponin D alleviates inflammatory response of osteoarthritis and mediates autophagy via elevating microRNA-199-3p to target transcription Factor-4
Journal of Orthopaedic Surgery and Research (2024)
-
Is occupational noise associated with arthritis? Cross-sectional evidence from US population
BMC Public Health (2024)
-
Synergism of fermented feed and ginseng polysaccharide on growth performance, intestinal development, and immunity of Xuefeng black-bone chickens
BMC Veterinary Research (2024)
-
Molecular imaging for evaluation of synovitis associated with osteoarthritis: a narrative review
Arthritis Research & Therapy (2024)