Key Points
-
Effector and memory CD4+ T helper 1 (TH1) and CD8+ T cells exhibit remarkable phenotypic and functional heterogeneity. The heterogeneity of such responses has important implications for whether they are protective or not.
-
Development of techniques to more fully characterize T-cell responses will lead to a better fundamental understanding of T-cell effector and memory differentiation as well as function. Multiparameter flow cytometry is a technique that has been used to simultaneously evaluate the secretion of multiple cytokines by a single T cell.
-
The ability to delineate a number of discrete functional populations of CD4+ TH1 and CD8+ T cells based on their pattern of cytokine secretion is termed the quality of the response. The demonstration that TH1 and CD8+ T cells that produce multiple cytokines have enhanced effector function and correlate best with protection establishes that the quality of the response is a crucial aspect of T-cell biology.
-
The factors that control the quality of the response include antigen dose and innate immunity.
-
Vaccine design for infections requiring T cells to mediate protection can now be tailored to optimize both the magnitude and quality of T cells that provide durable immunity and protection.
Abstract
T cells mediate effector functions through a variety of mechanisms. Recently, multiparameter flow cytometry has allowed a simultaneous assessment of the phenotype and multiple effector functions of single T cells; the delineation of T cells into distinct functional populations defines the quality of the response. New evidence suggests that the quality of T-cell responses is crucial for determining the disease outcome to various infections. This Review highlights the importance of using multiparameter flow cytometry to better understand the functional capacity of effector and memory T-cell responses, thereby enabling the development of preventative and therapeutic vaccine strategies for infections.
Similar content being viewed by others
Main
T cells have an essential role in protection against a variety of infections. Indeed, the development of successful vaccines against HIV, malaria or tuberculosis will require the generation of potent and durable T-cell responses (Box 1). Although a variety of promising vaccine formulations that are capable of eliciting strong T-cell immunity are currently being tested in humans, there are still no clearly defined immune correlates of protection for these infections. As T cells are functionally heterogeneous and mediate their effects through a variety of mechanisms, a major hurdle in quantifying protective T-cell responses has been the technical limitations in assessing the complexity of such responses. Methods to define the full characteristics of T cells are crucial for developing preventative and therapeutic vaccines for infections and cancer.
The fundamental characteristic in describing a T-cell response is its magnitude. This is commonly represented as the frequency of antigen-specific T cells or the expression of a specific effector function, such as interferon-γ (IFNγ) production. However, the magnitude of a T-cell response as measured by a single parameter does not reflect its full functional potential. In this regard, the range of T-cell functions include the ability to proliferate or induce proliferation of other cells (through the secretion of growth factors), organize immune responses (by secreting chemoattractants) and carry out effector functions by directly killing infected cells through cytolytic mechanisms or secretion of cytokines. These functions can be expressed in complex combinations that we define as the 'quality' of the T-cell response. This quality can be defined on an individual T-cell basis or for a population of antigen-specific T cells. Currently, flow cytometry is the only technique that can simultaneously characterize multiple functions, enabling a broad assessment of the magnitude, phenotype and functional capacity of T-cell effector functions1.
As we discuss in this Review article, a series of recent studies in mice, non-human primates and humans used multiparameter flow cytometry to characterize the quality of the T-cell response following immunization with various vaccines or after certain viral or parasitic infections2,3,4,5,6,7,8. The results provide compelling evidence that the quality of the T-cell response is a crucial factor in defining a protective T-cell response. In addition, recent results provide a mechanism for why distinct functional populations of cytokine-producing T cells are better effectors. We focus on the quality of CD4+ and CD8+ T-cell responses in the context of disease pathogenesis and vaccine development for viral, parasitic and mycobacterial infections. Although it is likely that regulatory T cells or inhibitory cytokines such as interleukin-10 (IL-10) will have a substantial influence on the magnitude and quality of such responses, discussion of their role will not be covered. Finally, this Review should inform the reader as to the importance of using multiparameter flow cytometry to address fundamental questions about memory and effector T-cell differentiation.
Multiparameter cytometry and T-cell quality
As a population, T cells exhibit marked heterogeneity9,10 and are capable of a broad array of functions; individual T cells may carry out a particular subset of these functions. For example, it has long been known that there are strong biases in the specific types of cytokines expressed by CD4+ T cells. The discovery that CD4+ T cells that secrete IFNγ and IL-4 could be segregated into subsets termed T helper 1 (TH1) and TH2 cells, respectively, provided a seminal demonstration of functional heterogeneity11. Within this particular paradigm, there are well-established models showing that one or the other TH-cell subset is the protective element against certain diseases or infections. On this basis, one can predict that the most effective T cells in a protective immune response against any given infectious agent may come from a particular functionally defined subset of T cells that express a unique combination of effector functions.
Flow cytometry is a powerful technology that is capable of quantifying individual functions independently and simultaneously on a single-cell basis (and, in some cases, under conditions that can preserve the viability of the cell for further use). Quantification of multiple functions of T cells requires at least six-colour technology (Fig. 1): three colours to identify the T-cell lineage (typically, these label CD3, CD4 and CD8), one colour for viability and/or as a dump channel to remove unwanted cell populations, and two or more colours devoted to the effector functions of interest (Fig. 1a). Furthermore, delineation of memory T-cell subsets requires an additional two or more colours to distinguish differentiation stages.
a | A typical 'gating tree' hierarchically identifies unique functional subsets of CD4+ and CD8+ T cells based on the fluorescence staining of live cells and on the expression of other relevant markers, such as CD3, CD4, CD8, CD45RA, CC-chemokine receptor 7 (CCR7), interferon-γ (IFNγ), interleukin-2 (IL-2) and tumour-necrosis factor (TNF), following antigenic stimulation. The viability marker (ViViD) excludes dead cells that can often show non-specific binding to other reagents. Live, CD3+ T cells are separated into CD4+ and CD8+ T-cell lineages; within each lineage, memory T cells are selected based on the expression of (for example) CCR7 and CD45RA. Other combinations of differentiation markers can similarly exclude naive T cells from functional analysis. b | Within the memory T-cell population (only the CD4+ memory T-cell subset is shown), the subset of cells that express each functional marker (for example, IFNγ, TNF and IL-2) is entered into a 'Boolean gating' analysis that separately identifies the seven subsets that express each possible combination of functions. c | The frequency of each functional subset within the memory T-cell population is shown in the bar chart; the representation can also be shown as a fraction of the total response in a pie chart. Here, the subsets that simultaneously express one (blue), two (green) or three (red) different cytokines are grouped by colour. FSC, forward scatter; SSC, side scatter.
Initial studies characterizing T-cell responses using IL-2 and IFNγ production revealed that antigen-specific T-cell populations include subsets of T cells that express different combinations of these two cytokines, and that the relative contributions of these subsets was highly relevant for clinical and immunological function12,13 (see later). Because T cells are capable of many more functions than just the production of these two cytokines, a substantial fraction of the antigen-specific population may be missed even with two-function measurements. By expanding the assay to encompass three to five different functions, a larger fraction of the antigen-specific response is obtained. Of note, the number of possible functionally unique subsets increases geometrically with the number of measurements made. By applying boolean gating, all possible combinations of T cells that produce the cytokines measured can be determined (Fig. 1b). Therefore, by measuring IL-2 and IFNγ (that is, measuring two simultaneous functions), there are three possible functional states: two single producer states (only IL-2 expression or only IFNγ expression), and a double producer state (expression of both IFNγ and IL-2). Measuring three simultaneous functions therefore leads to seven functional states (Fig. 1c), whereas five functions leads to 31 states. In general, not all possible combinations are represented in any given antigen response; rather, the overall response is typically limited to a subset of the individual combinations of the functions. Based on the frequency of each distinct functional subset, a pie chart can be assembled to show the composition of a total cytokine response (Fig. 1c). It should be noted that the precision with which the quality of a response can be determined is based on the number of events collected; the subdivision of a low-level response into multiple categories must be done with careful consideration of the inherent variability of counting such rare populations. Tools for statistical analysis of the quality of the response are only now being developed and assessed; in general, these analyses require the collection of more than one million events per sample.
The remainder of the Review highlights how this extended analysis provides insight into basic T-cell biology and has relevance for vaccine design and protection against infection.
Determining which functions to measure. The frequency of IFNγ-producing T cells has been the most widely used parameter to assess vaccine-induced responses specific for infections that require cellular immunity for protection. In terms of effector function, IFNγ has been shown to have a role in the clearance of various bacterial, parasitic, viral or fungal infections14,15,16; however, there are many examples in which the frequency of IFNγ-producing T cells is not a sufficient immune correlate of protection17,18,19. In this regard, tumour-necrosis factor (TNF) is another cytokine capable of mediating the killing of a variety of intracellular infectious viruses, bacteria and parasites20,21. Furthermore, production of IFNγ and TNF together lead to enhanced killing of Leishmania major and Mycobacterium tuberculosis22,23,24 compared with either cytokine alone22.
The third cytokine in the panel should be IL-2. Although IL-2 has little direct effector function, it promotes the expansion of CD4+ and CD8+ T cells, thereby serving to amplify effector T-cell responses. IL-2 may also be crucial for 'programming' CD8+ T cells for improved memory capacity and effector function25. Finally, IL-2 produced by T cells can enhance natural killer (NK)-cell activity that could contribute to the early control of infection following challenge. Therefore, IL-2, TNF and IFNγ provide a relatively simple set of cytokines that can be used to define a vaccine-elicited response against specific infections that require T cells for protection.
In addition to cytokines, CD8+ (and some CD4+) T cells mediate cytolytic activity through the release of perforin or granzymes. Measuring these directly (or by using CD107 as an indirect measure of degranulation) provides further insight into important effector pathways26, especially for viral infections such as HIV. Also, chemokines such as CC-chemokine ligand 4 (CCL4; previously known as MIP-1β) may act as antagonists to HIV infection27. Finally, the expression of CD154 (also known as CD40L) can be used to identify TH1 cells that provide help for humoral responses as well as activate dendritic cells (DCs)28. In conclusion, combinations of these functions together with the simple set of cytokines provide a more detailed picture of the antigen-specific T-cell response.
Functional heterogeneity of T-cell responses
Much of the data that correlates T-cell quality with clinical outcome has been generated from studies on HIV infection2,8,12,29. HIV infection is a useful model for assessing the clinical importance of T-cell quality for several reasons. First, although CD8+ T-cell responses are crucial for controlling HIV infection, the magnitude of such responses does not correlate with disease progression30,31. Second, differences in the proliferative capacity rather than the magnitude of HIV-specific CD4+ T cells have been associated with improved control of infection32,33. Furthermore, production of IL-2 by HIV-specific CD4+ T cells supports their proliferative capacity and may enhance HIV-specific CD8+ T-cell function34,35. Third, comparing T-cell responses from long-term non-progressors (LTNPs) or individuals on drug treatment with those with progressive disease allows for a correlation between the magnitude and quality of T-cell responses with the clinical course of infection in the context of varying levels of viral load.
Quality of CD4+ T-cell responses during infection. Initial studies analysing the production of IL-2 and IFNγ by CD4+ T cells from individuals infected with HIV showed that LTNPs, or individuals treated with antiviral therapy, had increased frequencies of T cells expressing IL-2 only or both IL-2 and IFNγ, whereas progressors had predominantly CD4+ T cells that only produced IFNγ (Refs 12,13,36,37). Similar results were observed in the course of infection with chronic hepatitis C virus (HCV)38 or M. tuberculosis39. More recently, multiparameter flow cytometry using IL-2, TNF and IFNγ with CD107 and CCL4 has been used to delineate 31 functional populations of T cells specific for HIV and cytomegalovirus (CMV)3. In comparing HIV-infected progressors with LTNPs there was a dramatic difference in the quality of the T-cell responses. Individuals with high viral loads had increased frequencies of T cells producing IFNγ only, and these cells constituted ∼40–50% of the total cytokine response. By contrast, the frequencies of IFNγ+TNF+IL-2+ or IL-2+IFNγ+ T cells represented ∼50% of the total responses from LTNPs or individuals on anti-retroviral treatment7,8. Therefore, improved control of HIV was associated with increased frequency of multifunctional CD4+ T cells that produce two or more different cytokines. Indeed, multifunctional CD4+ T cells represented a higher percentage of the total cytokine response from CD4+ T cells following exposure to viruses that have cleared or persist at low levels, such as influenza virus, Epstein–Barr virus (EBV), varicella-zoster virus (VZV; the causative agent of chickenpox) or CMV than from HIV-infected individuals that were not on anti-retroviral treatment and have a high level of persistent antigen7,8.
Taken together these results suggest that during the course of HIV infection, the presence of persistent antigen skews the differentiation of CD4+ T cells towards a population that is comprised largely of single-positive IFNγ-producing T cells, resulting in cell death, gradual CD4+ T-cell depletion and disease progression. By contrast, multifunctional CD4+ T cells are maintained during viral infections that are cleared or persist at low levels.
Although these studies provide insight into how different viruses, antigen load and persistence influence the quality of the response in humans, it is not clear whether maintenance of multifunctional T cells is a cause or an effect of viral control40. Hence, the most compelling evidence for the importance of multifunctional TH1 cells in mediating protection is in the mouse model of L. major infection4. Following immunization with various vaccine formulations encoding specific L. major antigens or after primary infection with L. major, the generation of multifunctional T cells that secrete IFNγ, IL-2 and TNF was found to strongly correlate with protection against subsequent challenge. Importantly, these studies showed that measuring the magnitude of IFNγ-producing CD4+ T cells alone was not sufficient to predict protection, and provided the first prospective evidence that measuring the quality of the CD4+ T-cell response, vis-à-vis multifunctional T cells, is required. Furthermore, following L. major infection, ∼100% of the total L. major-specific cytokine response is comprised of IFNγ+TNF+IL-2+ or IFNγ+TNF+ T cells that are maintained throughout the life of the mouse4. Of note, clearance of the parasites results in reduced immunity and protection41,42. Hence, in this model sustained immunity that is sufficient for life-long protection may require the persistence of low-level infection or repeated exposure to antigen to maintain a high frequency of multifunctional CD4+ T cells.
Quality of CD8+ T-cell responses during infection. The importance of CD8+ T-cell quality for protection has also been recently investigated. In a unique cohort of HIV-infected LTNPs, CD8+ T cells had increased proliferative capacity and cytolytic function after in vitro culture compared with CD8+ T cells from progressors, which only maintained an ability to produce IFNγ (Ref. 29). As the magnitude of HIV-specific CD8+ T-cell responses does not predict how disease will progress, these results suggested that the enhanced proliferative capacity by CD8+ T cells is associated with better control of HIV infection. More recently, using multiparameter flow cytometry to assess the quality of CD8+ T-cell responses in HIV-infected individuals, Betts et al. found a significantly higher frequency of CD8+ T cells from LTNPs that are IFNγ+TNF+CCL4+CD107+ and IL-2− compared with CD8+ T cells from progressors (and a small but significant increase in the frequency of CD8+ T cells that express all five functions)2; similar profiles were also observed in CD8+ T cells from the rectal mucosa of LTNPs43.
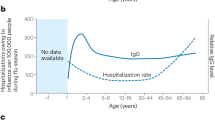
Collectively, these results suggest that there are distinct populations of multifunctional CD8+ T cells that mediate effector functions through different mechanisms. One population of CD8+ T cells that secretes IFNγ, TNF, IL-2 and CCL4 could rapidly expand following activation, and another population of CD8+ T cells that produces IFNγ, TNF, CCL4 and expresses CD107 could provide more immediate cytolytic function in non-lymphoid organs34,44. Finally, as described for CD4+ T cells earlier, the level and amount of persistent antigen influences the quality of the response (Fig. 2).
CD8+ T-cell functional quality in humans infected with different viruses was determined using a five-function assay that measured expression of interleukin-2 (IL-2), interferon-γ (IFNγ), tumour-necrosis factor (TNF), CC-chemokine ligand 4 (CCL4; previously known as MIP-1β) and CD107 following stimulation with antigenic peptides. The black arcs highlight the fraction of the multifunctional (3–5-expressing) CD8+ T cells within each response. An inverse correlation between the multifunctionality of the response and the persistence of antigen load is observed (background shading). CMV, cytomegalovirus; LTNP, long-term non-progressor.
Multifunctional T cells are optimized for effector function. The fact that multifunctional T cells are associated with enhanced protection might be explained solely by the fact that each cell is capable of a broader repertoire of functions. However, investigation into the mechanisms responsible for the protective function of these T cells revealed additional features. Remarkably, following immunization of mice with non-live vaccines encoding L. major antigens or of mice or humans with a live Mycobacterium bovis bacillus Calmette–Guérin (BCG) vaccine, we noted that there was a progressive increase in the median fluorescence intensity (MFI) for IFNγ, TNF and IL-2 from CD4+ T cells that secrete all three cytokines compared with double- or single-cytokine-producing CD4+ T cells4 (Fig. 3). The difference is substantial, with multifunctional CD4+ T cells making as much as 10-fold more IFNγ on a per-cell basis than monofunctional CD4+ T cells. The relative difference in MFI between distinct functional populations of cytokine-producing CD4+ T cells was greatest for IFNγ and least for IL-2 production4. Importantly, similar results were obtained in a study characterizing the quality of CD4+ T cells in non-human primates (R.A.S., unpublished observations) or humans exposed to HIV, CMV, influenza virus or immunized with vaccinia virus7 or CD8+ T-cell responses following Dryvax (wild-type vaccinia virus) or modified vaccinia virus Ankara (MVA; an attenuated vaccinia virus derived from multiple in vitro passages)5 (Fig. 3 and supplementary information S1 (Figure)). Therefore, at the single-cell level, maximal functional differentiation for IFNγ production occurs in cells from mice, non-human primates or humans that secrete three or more cytokines. Collectively these observations show that the MFI for IFNγ is associated with the number of cytokines produced by a T cell, irrespective of the particular vaccine or infection used to activate that cell. In this regard, assessing just the MFI for IFNγ could be used as a first approximation of the underlying quality of a T-cell response in resource-limited settings that do not have the capacity to carry out the multiparameter analysis. Indeed, we recently developed a metric that accounts for both the magnitude and quality of a CD4+ T-cell response by multiplying the MFI for IFNγ by the total frequency of antigen-specific T cells.
The amount of cytokine produced by a T cell can be estimated by the median fluorescence intensity (MFI) of the staining for that cytokine. An increase in the MFI reflects greater production of the cytokine. a | A representative graph showing the distribution of T cells expressing one (blue), two (green) or three (red) of the simultaneously measured cytokines — interferon-γ (IFNγ), interleukin-2 (IL-2) or tumour-necrosis factor (TNF). The further shifted the T cells are from the background (grey), the more cytokine they have expressed. Note the logarithmic scale: triple-cytokine-producing T cells (red) express 10-fold more IFNγ than double- or single-cytokine-producing T cells. b | There is a hierarchy of IFNγ expression within functionally defined subsets of cytokine-producing T cells. T cells that express more functions have an increased fluorescence intensity for IFNγ on a per-cell basis. The most dramatic example is the difference in MFI for T cells that only secrete IFNγ (blue) versus T cells that secrete all three cytokines (red). The schematic representation of such responses is derived from data obtained in mice, non-human primates and humans following vaccination or infection (see Supplementary information S1 (figure)).
In summary, several mechanisms account for the optimal protection of multifunctional CD4+ or CD8+ T cells. First, they secrete more IFNγ on a per-cell basis. Second, the secretion of both IFNγ and TNF from the same T cell mediates more efficient killing compared with either cytokine alone22,23; CD8+ T cells that secrete both IFNγ and TNF have enhanced cytolytic activity compared with CD8+ T cells that secrete IFNγ alone2,34,44. And third, secretion of IL-2 promotes the expansion of T cells in an autocrine or paracrine manner, which could enhance CD8+ T-cell memory function45.
Hierarchical control of multifunctional responses
The functional heterogeneity of T-cell responses raises several questions, the answers to which will be crucial in furthering our understanding of the control of effector and memory T-cell responses. Later we discuss whether there are distinct thresholds of activation for distinct functional subsets of cytokine-producing T cells and whether such T cells proceed through a defined differentiation pathway in which specific cytokines are progressively lost. Finally, it will be crucial to understand how the functional capacity of each subset of cytokine-producing T cells relates to their durability.
Activation threshold in multifunctional T cells. Activation of naive T cells requires the engagement of the clonotypic T-cell receptor (TCR) with the specific antigenic peptide presented by MHC molecules on antigen-presenting cells (APCs; this is referred to as signal 1). Full expansion of the primary T-cell response requires interaction of co-stimulatory molecules on the APCs with their ligand on T cells (this is referred to as signal 2). The amount of peptide–MHC complexes required to induce TCR activation is termed the avidity of the response. Therefore, T cells with a higher avidity require less peptide–MHC complexes to be activated. Indeed the avidity of a T-cell response can also relate to the functional capacity of the T cells to produce IFNγ or IL-2. In studies that analysed cytokine production from individual mouse TH1 cells, IFNγ but not IL-2 was detected when the TH1 cells were stimulated with low concentrations of the TCR ligand46. Stimulation with an increased concentration of the ligand resulted in the production of both IFNγ and IL-2 from the same cell. Similarly, in assessing CMV-specific CD4+ memory T-cell responses from humans, the production of IL-2 was more dependent on the increasing levels of co-stimulation than was IFNγ (Ref. 47). These data fit well with the observation that co-stimulation and the ligand–TCR density combine to provide a threshold that serves to regulate the response48. Taken together, these data show that an individual CD4+ T cell that has the capacity to produce both IFNγ and IL-2 may secrete only IFNγ if there is limited antigen or co-stimulation. Finally, for CD8+ T cells, the avidity of the TCR–peptide–MHC complex for inducing the production of IL-2 from influenza virus-specific memory CD8+ T cells was also lower than that for IFNγ (Ref. 49). Therefore, a commonality for both CD4+ and CD8+ T cells is that more antigen is required to elicit the production of IL-2 than the production of IFNγ.
The hierarchical organization of TCR-signalling thresholds and kinetics for IFNγ and IL-2 responses may allow the immune response to mediate effector function and maintain memory capacity. Therefore, in the setting of relatively low antigen load, IFNγ but not IL-2 is secreted, allowing for an effector function that is sufficient to mediate protection. In circumstances in which antigen load is increased, the induction of IL-2 as well as IFNγ from T cells would allow for the expansion of the responding T cells. The ability of antigen load to regulate effector T-cell function as needed and preserve multifunctional T cells provides a useful mechanism for fine-tuning the immune response to optimize protection and durability.
A linear differentiation model for TH1-cell responses. Based on the composition of CD4+ T-cell cytokine responses analysed from mice, humans and non-human primates following vaccination or infection, we propose a linear model of differentiation for CD4+ TH1 cells (Fig. 4a). TNF is the most ubiquitous cytokine and it is produced by most activated CD4+ T cells4,50,51 generated under conditions that favour TH1-cell differentiation. IL-2 expression is most often associated with TNF expression, regardless of whether IFNγ is expressed. CD4+ T cells that secrete IL-2 regardless of TNF expression can be sustained over a prolonged period of time and can develop into IFNγ-producing T cells following subsequent stimulation10. Therefore, CD4+ T cells that secrete IL-2, TNF or both serve as a reservoir of memory CD4+ T cells with effector potential10,52.
a | CD4+ T-cell differentiation can be modelled as a linear process, in which cells progressively gain functionality with further differentiation, until they reach the stage that is optimized for their effector function (such as the production of interleukin-2 (IL-2), interferon-γ (IFNγ) and tumour-necrosis factor (TNF)). Continued antigenic stimulation can lead to progressive loss of memory potential as well as cytokine production, resulting in terminally differentiated CD4+ T cells that only produce IFNγ and are short-lived. Following antigen stimulation, any of these stable differentiated subsets can also develop into activated effector CD4+ T cells, leading to their death. The amount of initial antigen exposure or innate-immune factors in the microenvironment will govern the extent of differentiation. b | Following stimulation, naive CD8+ T cells fully differentiate into activated effector CD8+ T cells that secrete IFNγ, most with cytolytic activity. Two models for the generation of CD8+ central memory T cells (TCM cells) and CD8+ effector memory T cells (TEM cells) are depicted by colour ('linear differentiation' is shown with black dotted arrows; 'fixed lineage' with red dotted arrows73; and black arrows depict transitions for both models). As for CD4+ T cells, continued antigenic stimulation of CD8+ T cells can lead to terminal differentiation and cell death. Unlike CD4+ TEM cells, CD8+ TEM cells may be able to re-acquire IL-2 expression and become CD8+ TCM cells.
IFNγ-producing T cells can also produce TNF, with or without IL-2. Single-positive, IFNγ-producing T cells can comprise a relatively large fraction of the total cytokine-producing CD4+ T-cell population in settings of acute and chronic antigen exposure, such as during infection, or immediately after immunization4,7,8. Such T cells have a limited capacity to be sustained as memory T cells and are at the final stage of CD4+ T-cell differentiation. Therefore, vaccines that elicit a high proportion of such T cells would not be protective, and provide a clear example for why the quality of the response is far more useful in assessing long-term protection than just measuring the frequency of IFNγ-producing CD4+ T cells.
Once CD4+ T cells have developed into IFNγ+ TNF+IL-2+ T cells they have three potential fates: they can persist as memory or effector T cells; they can further differentiate into less-functional T cells; or they can die following activation. The enhanced effector function and the differences in memory capacity between the discrete populations of cytokine-producing CD4+ T cells have important implications for vaccine design. Optimal protection would be achieved by having a population of multifunctional T cells that can mediate an effector function quickly and have a reservoir of memory T cells4,52 that secrete IL-2, TNF or both and have effector potential.
The linear differentiation model is most evident under conditions of transient antigenic and innate stimulation, such as vaccination with protein and adjuvant or with DNA. With greater stimulations, such as high doses of viral vectors or live infections, differentiation proceeds rapidly (or immediately) to IFNγ-secreting effector CD4+ T-cell populations.
Hierarchical control of CD8+ T-cell cytokine responses. In characterizing the hierarchy of cytokine production from CD8+ T cells following acute infection with LCMV53,54, VSV54 or influenza virus49 in mice, IFNγ is expressed by virtually all CD8+ T cells at the peak of the response. Contained within the population of IFNγ-producing CD8+ T cells is a subpopulation of T cells that also secretes TNF, and a smaller subpopulation that secretes both TNF and IL-2. Furthermore, compared with that of IFNγ and TNF, the induction of IL-2-producing CD8+ T cells is detected at a later time point, and its expression increases over time. In contrast to acute infection, few TNF- or IL-2-producing CD8+ T cells are generated during chronic LCMV infection, with IL-2 being lost first. Based on these data, Wherry et al. postulated that the level and duration of the stimulating antigen drives the hierarchical loss of effector-cytokine production by CD8+ T cells53,55. Indeed, this premise is supported by human studies showing that CD8+ T cells specific for the CMV peptide pp65 had a relatively high frequency (∼40–50%) of T cells that secreted both IFNγ and TNF44, whereas individuals with progressive HIV infection had few IFNγ-producing T cells that also secreted IL-2, TNF or both2.
Correlating phenotype with T-cell quality. The paradigm of segregating T cells into 'central memory' T cells (TCM cells) and 'effector memory' T cells (TEM cells), on the basis of their expression of CC-chemokine receptor 7 (CCR7) or CD62L, along with CD45RA56, provided a conceptual advance in our understanding of T-cell dynamics and the importance of compartmentalization of the immune response in mediating protection in lymphoid and non-lymphoid organs. This differential expression of CCR7 and CD62L provides crucial information on the ability of memory T cells to traffic into lymphoid and non-lymphoid organs. In addition, segregating CD4+ and CD8+ T cells into TCM or TEM cells has also been used as a correlate of protection based on the fact that distinct patterns of cytokines (that is, IFNγ and IL-2) can be associated with these specific subsets of memory T cells. The data reveal that both the phenotype and function of these specific subsets provide two independent facets of the immune response that together better inform whether such responses would be protective.
The seminal study by Sallusto and Lanzavecchia showed that CD4+CCR7+ TCM cells are enriched in T-cell populations that express IL-2, whereas CD4+CCR7− TEM cells produce more IFNγ (Ref. 56) (Fig. 4a). However, other reports show a less clear delineation between the TCM-cell and TEM-cell phenotype and IL-2 production by CD4+ T cells. For example, in HIV-infected adults on drug treatment, ∼50–80% of the IL-2-producing CD4+ T cells that were specific for antigens from CMV, influenza virus, EBV, HSV or the HIV gag protein were TEM cells8,57. Similarly, in mice infected with L. major30, or humans infected with vaccinia virus7, the majority of IL-2 that was produced was by multifunctional CD4+ TEM cells. Collectively, these studies show that the type of infection or the differences in the amount or duration of antigen exposure influences which subset of memory CD4+ T cells becomes the predominant source of IL-2: under conditions of persistent low-level infection or immediately following vaccination, IL-2 would be produced mostly by TEM cells.
Finally, a recent study in non-human primates showed that CCR7−CD4+ T cells that also express CD28 denote a population that has been termed 'transitional memory T cells', which express far more IL-2 than do CCR7−CD28−CD4+ TEM cells58. These examples show that under different stimulatory conditions the production of IL-2 may be associated with TEM or TCM cells, and highlight why this phenotypic designation of memory T cells may be misleading in terms of functional potential of the CD4+ T cells.
For CD8+ T cells, differences in IFNγ production and even in lytic function between TEM and TCM cells may be far less apparent59. In this regard, differences in the proliferative capacity of TEM and TCM cells, and their capacity to secrete IL-2 provide the most useful functional distinction between these subsets. Therefore, following activation, naive CD8+ T cells quickly develop into activated effector T cells as defined by their production of IFNγ, cytolytic function or both; however, it remains controversial whether the transition of activated effector T cells to TEM cells and TCM cells is linear or whether both populations arise and are sustained independently55,60 (Fig. 4b). Nevertheless, TCM cells have an enhanced capacity to proliferate and secrete IL-2. Therefore, in contrast to CD4+ T cells, it is very rare to find CD8+ TEM cells that produce IL-2. The enhanced ability of CD8+ TCM cells to produce IL-2 has been shown to confer improved protection compared with CD8+ TEM cells against a systemic viral challenge55. This observation is consistent with the fact that the expression of CCR7 by CD8+ TCM cells retains the T cells in secondary lymphoid organs and would be crucial for mediating protection against systemic infections by the ability of such T cells to rapidly expand.
Finally, it should be noted that in other mouse models of viral infection, CD8+ effector T cells or CD8+ TEM cells with enhanced cytolytic function but limited proliferative capacity mediated equal or better protection than CD8+ TCM cells following viral challenge at non-lymphoid sites61,62. Therefore, the location and speed at which the T cells are needed may determine the type of response that would mediate protection. The factors that influence the fate decisions, such as the relative frequency of CD8+ TEM versus CD8+ TCM cells, or kinetics of the transition from CD8+ TEM to CD8+ TCM cells include the amount and duration of the antigen or innate immunity and clonal competition60,63,64,65. Therefore, the quality of a CD8+ memory T-cell response can be controlled at the onset of priming.
In summary, determining the quality of a T-cell response in combination with the cell-surface receptor phenotype increases our fundamental understanding of T-cell memory and effector differentiation by defining the T cells' functional capacity, durability, history of antigen exposure and their capacity to traffic to lymphoid and non-lymphoid organs. Hence, a combined phenotypic and functional analysis of T cells should allow greater insight into whether a response is protective than either measurement alone.
T-cell quality following vaccination
Successful vaccines against HIV, malaria and tuberculosis will require the generation of durable T-cell responses of sufficient magnitude and quality. The relatively recent development of novel viral vaccine vectors and regimens capable of eliciting potent T-cell responses combined with improvements in the technical ability to assess T-cell responses offer hope that effective vaccines can be developed for these infections.
Factors regulating the quality of responses. Cytokines such as IL-12 and type I IFNs have been shown in many models to be crucial for the generation of CD4+ and CD8+ T cells, respectively. Importantly, there is substantial redundancy in the innate immune pathways that control T-cell responses and this differs depending on the adjuvant used or the infectious organism. Therefore, understanding the mechanisms by which innate immunity controls the quality of T-cell responses will enable better vaccine design. An example of this stems from studies with non-human primates, which show that protein vaccines administered with ligands for Toll-like receptor 7 (TLR7) and TLR8 elicit a high frequency of multifunctional T-cell responses50. As TLR7 and TLR8 are expressed by plasmacytoid DCs and myeloid DCs respectively66,67, these data suggest that activating both DC subsets may be important for generating multifunctional T-cell responses50. The discussion below highlights major differences in the quality of the T-cell responses following immunization with a variety of vaccine formulations.
Qualitative responses to vaccines. The first evidence for functional heterogeneity of CD4+ T-cell-dependent cytokine responses using multiparameter flow cytometry was assessed in humans immunized with vaccines against hepatitis B or tetanus toxin68. In this and subsequent studies51, TNF and IL-2 comprised the majority of the cytokine response, with a small frequency of IFNγ-producing CD4+ T cells. As the adjuvants that were used with these vaccines do not elicit strong innate immunity, the magnitude of such responses was relatively modest. By contrast, viral vaccines such as those that contain replication-defective recombinant adenovirus serotype-5 (rADV-5) or recombinant poxvirus vectors are currently the most promising formulations for inducing strong cytokine-producing T-cell responses in humans69. Importantly, there may be major differences in the magnitude and quality of the T-cell responses induced by rADV-5 and poxvirus vectors70. Although there are few direct studies comparing rADV-5 and poxvirus vectors with the same inserts, it seems that rADV-5 vectors engender stronger CD8+ T-cell responses than poxvirus vectors70 (N. Letvin, personal communication). Moreover, a rADV-5 vector encoding the HIV gag protein preferentially elicits CD8+ T-cell responses, whereas poxvirus vectors appear to induce a more balanced CD4+ and CD8+ T-cell response (N. Letvin and D. Barouch, personal communication). Thus, the type of T-cell response generated will be influenced by the dose and serotype of rADV, the type of poxvirus (for example MVA, NYVAC (New York vaccinia) and canarypox virus), as well as the specific antigen.
In terms of the quality of T-cell responses elicited by these vectors, rADV vaccines that encode antigens from HIV and other viruses induce CD4+ and CD8+ T cells that are IFNγ+TNF+ or IFNγ+, but few T cells that produce IL-2 (Refs 4,50) (R.A.S., unpublished observations) (Fig. 5). A first indication of whether rADV-5 vectors that encode specific HIV antigens would be protective in humans against HIV infection following immunization was recently revealed. In this Phase IIb clinical trial, up to 75% of volunteers immunized with an rADV-5 vector encoding HIV Gag–Pol and Nef (negative factor) had IFNγ-producing cells, as detected by elispot analysis. Unfortunately, the clinical trial was halted before its completion after the first analysis showed no efficacy in terms of viral load. Although there are many potential reasons for failure, it is possible that the magnitude and quality of the response were not optimal.
a | The quality of CD8+ T-cell responses (five functions measured) to the HIV envelope protein in humans is illustrated following immunization with DNA or replication-defective recombinant adenovirus (rADV) vectors containing the protein, or after priming with the DNA vector followed by boosting with rADV or poxvirus vectors (New York vaccinia (NYVAC)). The black arcs highlight the fraction of the multifunctional (3–5-expressing) CD8+ T cells within each response. b | The quality of the CD4+ T-cell response (3 functions measured) to Leishmania major proteins is shown following immunization with low- or high-dose rADV vaccines, protein vaccine with CpG-containing motifs, or live infection. c | Comparing only triple-cytokine-producing CD4+ T cells induced by each vaccination reveals a hierarchy of IFNγ median fluorescence intensity (MFI) that correlates with the level of protection following subsequent challenge with L. major.
A final aspect from this study was that men with high titres of antibodies against adenovirus serotype-5 generated in response to a prior natural adenoviral infection had a trend towards increased acquisition of infection following vaccination with the rADV-5 vector encoding Gag–Pol and Nef. Although there is no clear explanation for this, it raises the question as to whether this observation is specific for this particular rADV-5 vector or whether it could be seen with other rADV-5 vectors, alternative rADVs or other live-attenuated viral vectors. Nevertheless, there is active development of other viral vectors capable of eliciting strong T-cell responses with favourable quality in humans. In this regard, humans immunized with vaccinia virus or MVA have a relatively high frequency (∼30%) of CD4+ and CD8+ T cells that secrete four or five different cytokines, including IL-2 (Refs 5,7,71). Similarly, recombinant poxvirus vectors that encode HIV envelope proteins have also been shown to elicit multifunctional CD4+ and CD8+ T cells that secrete IL-2 (Ref. 5) (N. Letvin, personal communication). Finally, as discussed below, heterologous prime–boost immunization can influence the magnitude and quality of T-cell responses elicited by rADV-5 vaccines.
The only prospective evidence for how the quality of a T-cell response influences protection was shown in a study using a mouse model of L. major infection4. In this study, the quality of responses differed dramatically between the different vaccine groups. Protective vaccine regimens elicited induced a high frequency of IFNγ+TNF+IL-2+ producing CD4+ T cells, constituting ∼50% of the total cytokine response, whereas non-protective vaccine strategies induced mostly T cells that produced one or two different cytokines only. This study showed a strong correlation between the protection of vaccine regimens and their ability to induce high frequencies of multifunctional T cells. Importantly, the potential importance of multifunctional T cells for mediating protection was extended to the mouse model of M. tuberculosis infection4, in which protective BCG immunization generated a high level of CD4+ T cells that secrete IFNγ and TNF, with or without IL-2. A final point is that there can be dramatic differences in the IFNγ MFI among multifunctional CD4+ T cells elicited by different vaccine formulations4. Therefore, in choosing vaccine regimens it will be important to optimize the potency of multifunctional T-cell responses.
Prime-boost immunization influences T-cell quality. The findings that varying amounts of the same vaccine (for example, rADV vaccines) elicit distinct qualitative CD4+ T-cell responses provide evidence for how antigen load, innate immunity or both influence the response. rADV vaccines require a relatively high dose of the vaccine to induce CD8+ T-cell responses compared with CD4+ T cells. As high-dose rADV-5 elicits a TH1-type response of poor quality4, optimizing the magnitude and quality of both the CD4+ and CD8+ T-cell responses with rADV vaccines alone may be difficult. However, heterologous prime–boost immunization using rADV or poxvirus vectors with DNA or antigenic protein plus a TLR ligand may optimize both the CD4+ T-cell and CD8+ T-cell responses. It is crucial to note that the order and type of vaccine formulation profoundly influence both the magnitude and quality of the T-cell responses generated. Thus, for optimizing CD8+ T-cell responses, viral vectors are best used as a boost following priming with DNA or protein vaccines plus an adjuvant.
Stability of multifunctional T-cell responses and imprinting. As protection by T cells is dependent on both the magnitude and quality of the response, it is important to understand the factors that regulate the stability of distinct functional populations of cytokine-producing T cells. In this regard, following immunization with a vaccine containing a Leshmania spp. protein plus CpG-containing DNA motifs (a TLR ligand) or with an rADV vaccine, the quality of the CD4+ T-cell response in mice was established within 28 days and remained constant for at least 3 months4. Furthermore, the magnitude of the response decreased within 2–4 weeks after immunization and then remained stable for up to 3 months. Similarly, after prime–boost immunization of non-human primates with the HIV gag protein and a TLR7 and TLR8 or TLR9 ligand followed by an HIV-gag-containing rADV vaccine, the quality of CD4+ and CD8+ T-cell responses remained stable for 1 year50. Moreover, data from human HIV vaccine studies show that the quality of the T-cell responses following immunization with DNA, rADV or DNA and rADV vaccines are stable over at least 18 months (M.R., unpublished observations). Finally, in humans vaccinated against smallpox with vaccinia virus, there was a high frequency of CD4+ and CD8+ T cells that produce both IFNγ and TNF 1 year following immunization and this T-cell response persisted for up to 50 years, albeit at far lower frequencies72.
Taken together, these data suggest that the quality of a T-cell response induced by vaccines or infections in which antigen is cleared is imprinted early and remains relatively stable over time. This raises a crucial question as to whether distinct functional populations of T cells have different capacities for survival over a prolonged period of time. In addition, the magnitude and quality of T-cell responses will be altered by subsequent immunization and may be affected by nonspecific innate immune responses. Therefore, a fundamental understanding of the dynamics of T-cell quality will help determine when immune boosting is needed and how it will affect the immune response.
Conclusion
This article reviews the importance that the quality of T-cell responses has in mediating protection. However, there still remains no single metric for defining a protective T-cell response. Clearly, this metric will involve a calculation that takes into account both the magnitude and the multifunctional quality of the response, as a low frequency of high-quality T cells may be as protective as a high frequency of lesser-quality T cells (although the persistence of the latter is likely to be much shorter). One possible metric is the integrated MFI (iMFI) calculation that incorporates the magnitude and the potency (on a single-cell basis) of the response4. In upcoming proof-of-concept clinical trials using a T-cell-based vaccine approach against HIV, it will be crucial to analyse the quality of the T-cell responses from individuals that show any degree of protection, which would provide crucial information for follow-on studies. Finally, it will be important to extend the analysis of T-cell responses to additional proteins that would be involved in protection. In this regard, genomic analysis of antigen-specific T-cell responses following vaccination should identify a broader array of proteins and functions to assess.
References
Perfetto, S. P., Chattopadhyay, P. K. & Roederer, M. Seventeen-colour flow cytometry: unravelling the immune system. Nature Rev. Immunol. 4, 648–655 (2004). This article reviews the development and application of multiparameter flow cytometry for immunological assessments.
Betts, M. R. et al. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107, 4781–4789 (2006). This is the first paper to use multiparameter flow cytometry to characterize the quality of CD8+ T-cell responses in humans following an infection and suggest that multifunctional cells are beneficial.
Casazza, J. P. et al. Acquisition of direct antiviral effector functions by CMV-specific CD4+ T lymphocytes with cellular maturation. J. Exp. Med. 203, 2865–2877 (2006).
Darrah, P. A. et al. Multifunctional TH1 cells define a correlate of vaccine-mediated protection against Leishmania major. Nature Med. 13, 843–850 (2007). This is the first study to prospectively show that multifunctional T H 1 cells are correlated with protection and have enhanced effector function.
Precopio, M. L. et al. Immunization with vaccinia virus induces polyfunctional and phenotypically distinctive CD8+ T cell responses. J. Exp. Med. 204, 1405–1416 (2007).
Wille-Reece, U. et al. HIV Gag protein conjugated to a Toll-like receptor 7/8 agonist improves the magnitude and quality of Th1 and CD8+ T cell responses in nonhuman primates. Proc. Natl Acad. Sci. USA 102, 15190–15194 (2005).
Kannanganat, S., Ibegbu, C., Chennareddi, L., Robinson, H. L. & Amara, R. R. Multiple-cytokine-producing antiviral CD4 T cells are functionally superior to single-cytokine-producing cells. J. Virol. 81, 8468–8476 (2007). This is the first study in humans to show that multifunctional T cells have increased MFI for IFN γ compared with all other populations.
Tilton, J. C. et al. Changes in paracrine interleukin-2 requirement, CCR7 expression, frequency, and cytokine secretion of human immunodeficiency virus-specific CD4+ T cells are a consequence of antigen load. J. Virol. 81, 2713–2725 (2007). This study shows that IL-2 is produced by a substantial majority of CD4+ T EM cells in humans in response to infection with various viruses.
Woodland, D. L. & Dutton, R. W. Heterogeneity of CD4+ and CD8+ T cells. Curr. Opin. Immunol. 15, 336–342 (2003).
Wu, C. Y. et al. Distinct lineages of TH1 cells have differential capacities for memory cell generation in vivo. Nature Immunol. 3, 852–858 (2002).
Mosmann, T. R., Cherwinski, H., Bond, M. W., Giedlin, M. A. & Coffman, R. L. Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. 1986. J. Immunol. 175, 5–14 (2005).
Harari, A., Petitpierre, S., Vallelian, F. & Pantaleo, G. Skewed representation of functionally distinct populations of virus-specific CD4 T cells in HIV-1-infected subjects with progressive disease: changes after antiretroviral therapy. Blood 103, 966–972 (2004).
Younes, S. A. et al. HIV-1 viremia prevents the establishment of interleukin 2-producing HIV-specific memory CD4+ T cells endowed with proliferative capacity. J. Exp. Med. 198, 1909–1922 (2003).
Cooper, A. M. et al. Disseminated tuberculosis in interferon γ gene-disrupted mice. J. Exp. Med. 178, 2243–2247 (1993).
Flynn, J. L. et al. An essential role for interferon gamma in resistance to Mycobacterium tuberculosis infection. J. Exp. Med. 178, 2249–2254 (1993).
Wang, Z. E., Reiner, S. L., Zheng, S., Dalton, D. K. & Locksley, R. M. CD4+ effector cells default to the Th2 pathway in interferon γ-deficient mice infected with Leishmania major. J. Exp. Med. 179, 1367–1371 (1994).
Elias, D., Akuffo, H. & Britton, S. PPD induced in vitro interferon γ production is not a reliable correlate of protection against Mycobacterium tuberculosis. Trans. R. Soc. Trop. Med. Hyg. 99, 363–368 (2005).
Pfeffer, K. Biological functions of tumor necrosis factor cytokines and their receptors. Cytokine Growth Factor Rev. 14, 185–191 (2003).
Skinner, M. A. et al. A DNA prime-live vaccine boost strategy in mice can augment IFN-γ responses to mycobacterial antigens but does not increase the protective efficacy of two attenuated strains of Mycobacterium bovis against bovine tuberculosis. Immunology 108, 548–555 (2003).
Blackwell, J. M. Genetic susceptibility to leishmanial infections: studies in mice and man. Parasitology 112, S67–S74 (1996).
Bloom, B. R., Flynn, J., McDonough, K., Kress, Y. & Chan, J. Experimental approaches to mechanisms of protection and pathogenesis in M. tuberculosis infection. Immunobiology 191, 526–536 (1994).
Bogdan, C., Moll, H., Solbach, W. & Rollinghoff, M. Tumor necrosis factor-α in combination with interferon-γ, but not with interleukin 4 activates murine macrophages for elimination of Leishmania major amastigotes. Eur. J. Immunol. 20, 1131–1135 (1990).
Liew, F. Y., Li, Y. & Millott, S. Tumor necrosis factor-α synergizes with IFN-γ in mediating killing of Leishmania major through the induction of nitric oxide. J. Immunol. 145, 4306–4310 (1990).
Chan, J., Xing, Y., Magliozzo, R. S. & Bloom, B. R. Killing of virulent Mycobacterium tuberculosis by reactive nitrogen intermediates produced by activated murine macrophages. J. Exp. Med. 175, 1111–1122 (1992).
Williams, M. A., Holmes, B. J., Sun, J. C. & Bevan, M. J. Developing and maintaining protective CD8+ memory T cells. Immunol. Rev. 211, 146–153 (2006).
Betts, M. R. et al. Sensitive and viable identification of antigen-specific CD8+ T cells by a flow cytometric assay for degranulation. J. Immunol. Methods 281, 65–78 (2003).
Cocchi, F. et al. Identification of RANTES, MIP-1α, and MIP-1β as the major HIV-suppressive factors produced by CD8+ T cells. Science 270, 1811–1815 (1995).
Chattopadhyay, P. K., Yu, J. & Roederer, M. Live-cell assay to detect antigen-specific CD4+ T-cell responses by CD154 expression. Nature Protoc. 1, 1–6 (2006).
Migueles, S. A. et al. HIV-specific CD8+ T cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nature Immunol. 3, 1061–1068 (2002).
Betts, M. R. et al. Analysis of total human immunodeficiency virus (HIV)-specific CD4+ and CD8+ T-cell responses: relationship to viral load in untreated HIV infection. J. Virol. 75, 11983–11991 (2001).
Gea-Banacloche, J. C. et al. Maintenance of large numbers of virus-specific CD8+ T cells in HIV-infected progressors and long-term nonprogressors. J. Immunol. 165, 1082–1092 (2000).
Rosenberg, E. S. et al. Vigorous HIV-1-specific CD4+ T cell responses associated with control of viremia. Science 278, 1447–1450 (1997).
McNeil, A. C. et al. High-level HIV-1 viremia suppresses viral antigen-specific CD4+ T cell proliferation. Proc. Natl Acad. Sci. USA 98, 13878–13883 (2001).
Lichterfeld, M. et al. HIV-1-specific cytotoxicity is preferentially mediated by a subset of CD8+ T cells producing both interferon-γ and tumor necrosis factor-α. Blood 104, 487–494 (2004).
Zimmerli, S. C. et al. HIV-1-specific IFN-γ/IL-2-secreting CD8 T cells support CD4-independent proliferation of HIV-1-specific CD8 T cells. Proc. Natl Acad. Sci. USA 102, 7239–7244 (2005).
Boaz, M. J., Waters, A., Murad, S., Easterbrook, P. J. & Vyakarnam, A. Presence of HIV-1 Gag-specific IFN-γ+IL-2+ and CD28+IL-2+ CD4 T cell responses is associated with nonprogression in HIV-1 infection. J. Immunol. 169, 6376–6385 (2002).
Duvall, M. G. et al. Maintenance of HIV-specific CD4+ T cell help distinguishes HIV-2 from HIV-1 infection. J. Immunol. 176, 6973–6981 (2006).
Semmo, N. et al. Preferential loss of IL-2-secreting CD4+ T helper cells in chronic HCV infection. Hepatology 41, 1019–1028 (2005).
Millington, K. A. et al. Dynamic relationship between IFN-γ and IL-2 profile of Mycobacterium tuberculosis-specific T cells and antigen load. J. Immunol. 178, 5217–5226 (2007).
Jansen, C. A. et al. Prognostic value of HIV-1 Gag-specific CD4+ T-cell responses for progression to AIDS analyzed in a prospective cohort study. Blood 107, 1427–1433 (2006).
Uzonna, J. E., Wei, G., Yurkowski, D. & Bretscher, P. Immune elimination of Leishmania major in mice: implications for immune memory, vaccination, and reactivation disease. J. Immunol. 167, 6967–6974 (2001).
Belkaid, Y., Piccirillo, C. A., Mendez, S., Shevach, E. M. & Sacks, D. L. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature 420, 502–507 (2002).
Critchfield, J. W. et al. Multifunctional human immunodeficiency virus (HIV) gag-specific CD8+ T-cell responses in rectal mucosa and peripheral blood mononuclear cells during chronic HIV type 1 infection. J. Virol. 81, 5460–5471 (2007).
Sandberg, J. K., Fast, N. M. & Nixon, D. F. Functional heterogeneity of cytokines and cytolytic effector molecules in human CD8+ T lymphocytes. J. Immunol. 167, 181–187 (2001).
Williams, M. A., Tyznik, A. J. & Bevan, M. J. Interleukin-2 signals during priming are required for secondary expansion of CD8+ memory T cells. Nature 441, 890–893 (2006).
Itoh, Y. & Germain, R. N. Single cell analysis reveals regulated hierarchical T cell antigen receptor signaling thresholds and intraclonal heterogeneity for individual cytokine responses of CD4+ T cells. J. Exp. Med. 186, 757–766 (1997).
Waldrop, S. L., Davis, K. A., Maino, V. C. & Picker, L. J. Normal human CD4+ memory T cells display broad heterogeneity in their activation threshold for cytokine synthesis. J. Immunol. 161, 5284–5295 (1998).
Viola, A. & Lanzavecchia, A. T cell activation determined by T cell receptor number and tunable thresholds. Science 273, 104–106 (1996).
La Gruta, N. L., Turner, S. J. & Doherty, P. C. Hierarchies in cytokine expression profiles for acute and resolving influenza virus-specific CD8+ T cell responses: correlation of cytokine profile and TCR avidity. J. Immunol. 172, 5553–5560 (2004).
Wille-Reece, U. et al. Toll-like receptor agonists influence the magnitude and quality of memory T cell responses after prime-boost immunization in nonhuman primates. J. Exp. Med. 203, 1249–1258 (2006).
Stubbe, M., Vanderheyde, N., Goldman, M. & Marchant, A. Antigen-specific central memory CD4+ T lymphocytes produce multiple cytokines and proliferate in vivo in humans. J. Immunol. 177, 8185–8190 (2006).
Zaph, C., Uzonna, J., Beverley, S. M. & Scott, P. Central memory T cells mediate long-term immunity to Leishmania major in the absence of persistent parasites. Nature Med. 10, 1104–1110 (2004).
Wherry, E. J., Blattman, J. N., Murali-Krishna, K., van der Most, R. & Ahmed, R. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J. Virol. 77, 4911–4927 (2003).
Kristensen, N. N., Christensen, J. P. & Thomsen, A. R. High numbers of IL-2-producing CD8+ T cells during viral infection: correlation with stable memory development. J. Gen. Virol. 83, 2123–2133 (2002).
Wherry, E. J. et al. Lineage relationship and protective immunity of memory CD8 T cell subsets. Nature Immunol. 4, 225–234 (2003).
Sallusto, F., Lenig, D., Forster, R., Lipp, M. & Lanzavecchia, A. Two subsets of memory T lymphocytes with distinct homing potentials and effector functions. Nature 401, 708–712 (1999).
Harari, A., Vallelian, F. & Pantaleo, G. Phenotypic heterogeneity of antigen-specific CD4 T cells under different conditions of antigen persistence and antigen load. Eur. J. Immunol. 34, 3525–3533 (2004).
Okoye, A. et al. Progressive CD4+ central memory T cell decline results in CD4+ effector memory insufficiency and overt disease in chronic SIV infection. J. Exp. Med. 204, 2171–2185 (2007).
Unsoeld, H., Krautwald, S., Voehringer, D., Kunzendorf, U. & Pircher, H. Cutting edge: CCR7+ and CCR7− memory T cells do not differ in immediate effector cell function. J. Immunol. 169, 638–641 (2002).
Marzo, A. L. et al. Initial T cell frequency dictates memory CD8+ T cell lineage commitment. Nature Immunol. 6, 793–799 (2005).
Bachmann, M. F., Wolint, P., Schwarz, K., Jager, P. & Oxenius, A. Functional properties and lineage relationship of CD8+ T cell subsets identified by expression of IL-7 receptor alpha and CD62L. J. Immunol. 175, 4686–4696 (2005).
Roberts, A. D. & Woodland, D. L. Cutting edge: effector memory CD8+ T cells play a prominent role in recall responses to secondary viral infection in the lung. J. Immunol. 172, 6533–6537 (2004).
Badovinac, V. P., Messingham, K. A., Jabbari, A., Haring, J. S. & Harty, J. T. Accelerated CD8+ T-cell memory and prime-boost response after dendritic-cell vaccination. Nature Med. 11, 748–756 (2005).
Intlekofer, A. M. et al. Requirement for T-bet in the aberrant differentiation of unhelped memory CD8+ T cells. J. Exp. Med. 204, 2015–2021 (2007).
Joshi, N. S. et al. Inflammation directs memory precursor and short-lived effector CD8+ T cell fates via the graded expression of T-bet transcription factor. Immunity 27, 281–295 (2007).
Jarrossay, D., Napolitani, G., Colonna, M., Sallusto, F. & Lanzavecchia, A. Specialization and complementarity in microbial molecule recognition by human myeloid and plasmacytoid dendritic cells. Eur. J. Immunol. 31, 3388–3393 (2001).
Kadowaki, N. et al. Subsets of human dendritic cell precursors express different toll-like receptors and respond to different microbial antigens. J. Exp. Med. 194, 863–869 (2001).
De Rosa, S. C. et al. Vaccination in humans generates broad T cell cytokine responses. J. Immunol. 173, 5372–5380 (2004). This paper demonstrates the use of multiparameter flow cytometry to identify and enumerate a broad range of antigen-specific T cells, and is the first to show simultaneous measurement of five functions on a cell-by-cell basis.
Harari, A. et al. An HIV-1 Clade C DNA Prime, NYVAC Boost Vaccine Regimen induces reliable, polyfunctional and long-lasting T cell responses. J. Exp. Med., 205, 63–77 (2008).
Shiver, J. W. et al. Replication-incompetent adenoviral vaccine vector elicits effective anti-immunodeficiency-virus immunity. Nature 415, 331–335 (2002).
Beveridge, N. E. et al. Immunisation with BCG and recombinant MVA85A induces long-lasting, polyfunctional Mycobacterium tuberculosis-specific CD4+ memory T lymphocyte populations. Eur. J. Immunol. 37, 3089–3100 (2007).
Hammarlund, E. et al. Duration of antiviral immunity after smallpox vaccination. Nature Med. 9, 1131–1137 (2003).
Kaech, S. M. & Wherry, E. J. Heterogeneity and cell-fate decisions in effector and memory CD8+ T cell differentiation during viral infection. Immunity 27, 393–405 (2007).
Acknowledgements
This work is supported by the Intramural Research Program of the US National Institutes of Health, Vaccine Research Center, NIAID.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
supplementary information
Multifunctional T cells are optimized for effector function. (PDF 250 kb)
Related links
Glossary
- Correlates of protection
-
A measurable predictor of an individual's immunity to a pathogen following vaccination or infection. For most licensed vaccines, antibody titres serve as a strong immune correlate of protection.
- Magnitude of a T-cell response
-
This term generally refers to a quantitative measurement of the T-cell response, often expressed as the frequency of CD4+ or CD8+ T cells that are antigen specific. It can also refer to bulk measurements, such as total cytokine secretion, cytolytic activity or proliferation.
- Quality of the T-cell response
-
The quality of a T-cell response is distinct from the phenotype or frequency of the T cells and refers to the specific combination of functions that the T cells are capable of carrying out. T-cell responses with a better quality (that is, a greater degree of multifunctionality) have been shown to correlate with disease non-progression and protection in some models.
- T helper 1 (TH1) and TH2 cells
-
Functional subsets of CD4+ T cells expressing the αβ-T-cell receptor that produce either type-1 cytokines (IL-2, IFNγ and other cytokines that support macrophage activation, the generation of cytotoxic T cells and the production of opsonizing antibodies), or type-2 cytokines (IL-4, IL-5, IL-13 and other cytokines that support B-cell activation, production of non-opsonizing antibodies, allergic reactions and expulsion of extracellular parasites).
- Dump channel
-
A flow cytometric measurement that combines the fluorescence from reagents specific for dead or unwanted cells to eliminate those cells within a single gate.
- Boolean gating
-
A flow cytometric data analysis technique in which cells are divided into all possible combinations of the functions measured by using the Boolean operations 'and' and 'not' on analysis gates applied to those measurements. These populations of cells can be expressed as absolute frequencies or as a fraction of the total response.
- Perforin
-
A component of cytolytic granules that permeabilizes plasma membranes, allowing granzymes and other cytotoxic components to enter target cells.
- Granzymes
-
Secreted serine proteases that enter target cells through perforin pores, and cleave and activate intracellular caspases that lead to the induction of apoptosis of target cells.
- CD107
-
A lysosomal-associated membrane protein (LAMP) associated with cytolytic granules that can be detected on the surface of T cells following degranulation.
- Long-term non-progressors
-
(LTNPs). There is no universally adopted definition of LTNPs, and often the term LTNP is used interchangeably with HIV controller, because control of viraemia is strongly predictive of LTNP. Loosely, LTNP refers to individuals infected with HIV whose plasma viral load is less than 1,000 HIV RNA copies per ml for extended periods. Stricter definitions of LTNP include the duration of infection and the number of CD4+ T cells.
- Multifunctional CD4+ T cells
-
Also referred to as polyfunctional T cells, these are CD4+ T cells (or CD8+ T cells in the case of multifunctional CD8+ T cells) that have two or more functions including, but not limited to, the degranulation or the production of cytokines or chemokines. The development of multiparameter flow cytometry has facilitated this extensive analysis of T-cell effector functions at the single-cell level.
- Adjuvant
-
An agent that when mixed with an antigen in a vaccine can increase the immune response to that antigen after immunization.
- Central memory T cells
-
(TCM cells). Antigen-experienced T cells that express cell-surface receptors required for homing to secondary lymphoid organs. These cells are generally thought to be long-lived and can serve as the precursors for effector T cells for recall responses.
- Effector memory T cells
-
(TEM cells). Antigen-experienced T cells that have immediate effector capabilities, such as cytotoxicity, and can efficiently migrate to peripheral sites of inflammation.
- ELISPOT
-
An antibody-capture-based method for enumerating specific T cells (CD4+ and CD8+) that secrete a particular cytokine (often interferon-γ).
- Heterologous prime–boost immunization
-
In contrast to homologous immunization in which the same antigen formulation is repetitively administered, heterologous prime–boosting refers to the use of different formulations to initiate and to boost the immune response. This approach often elicits T-cell responses of greater breadth, magnitude or quality.
- Integrated MFI
-
(iMFI). A value that results from the multiplication of the frequency of a cytokine-producing subset of cells with the median fluorescence intensity of intracellular staining for that cytokine.
Rights and permissions
About this article
Cite this article
Seder, R., Darrah, P. & Roederer, M. T-cell quality in memory and protection: implications for vaccine design. Nat Rev Immunol 8, 247–258 (2008). https://doi.org/10.1038/nri2274
Issue Date:
DOI: https://doi.org/10.1038/nri2274