Key Points
-
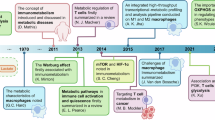
Immunometabolism describes the changes that occur in intracellular metabolic pathways in immune cells during activation.
-
Six major pathways have been studied in immune cells in detail: glycolysis, the tricarboxylic acid (TCA) cycle, the pentose phosphate pathway, fatty acid oxidation, fatty acid synthesis and amino acid metabolism.
-
Glycolysis and fatty acid synthesis are key features of lipopolysaccharide (LPS)-activated macrophages; by contrast, interleukin-4 (IL-4)-activated macrophages mainly use oxidative phosphorylation and fatty acid oxidation to generate energy.
-
Effector T cells are highly glycolytic whereas memory T cells have an oxidative metabolism.
-
Metabolites, such as succinate and citrate, and enzymes, such as pyruvate kinase isoenzyme M2 (PKM2), glyceraldehyde 3-phosphate dehydrogenase (GAPDH) and enolase, have roles outside of metabolism that promote specific events during immune cell activation.
-
Small molecules can target metabolic pathways and alter the phenotype of immune cells, raising the possibility of therapeutic intervention
Abstract
In recent years a substantial number of findings have been made in the area of immunometabolism, by which we mean the changes in intracellular metabolic pathways in immune cells that alter their function. Here, we provide a brief refresher course on six of the major metabolic pathways involved (specifically, glycolysis, the tricarboxylic acid (TCA) cycle, the pentose phosphate pathway, fatty acid oxidation, fatty acid synthesis and amino acid metabolism), giving specific examples of how precise changes in the metabolites of these pathways shape the immune cell response. What is emerging is a complex interplay between metabolic reprogramming and immunity, which is providing an extra dimension to our understanding of the immune system in health and disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Newsholme, P., Curi, R., Gordon, S. & Newsholme, E. A. Metabolism of glucose, glutamine, long-chain fatty acids and ketone bodies by murine macrophages. Biochem. J. 239, 121–125 (1986). One of the key pioneering studies on macrophage metabolism.
Alonso, D. & Nungester, W. J. Comparative study of host resistance of guinea pigs and rats V. The effect of pneumococcal products on glycolysis and oxygen uptake by polymorphonuclear leucocytes. J. Infect. Dis. 99, 174–181 (1956).
Oren, R., Farnham, A. E., Saito, K., Milofsky, E. & Karnovsky, M. L. Metabolic patterns in three types of phagocytizing cells. J. Cell Biol. 17, 487–501 (1963). An important early study on metabolism in different types of macrophages.
Fukuzumi, M., Shinomiya, H., Shimizu, Y., Ohishi, K. & Utsumi, S. Endotoxin-induced enhancement of glucose influx into murine peritoneal macrophages via GLUT1. Infect. Immun. 64, 108–112 (1996).
Liu, Y., Zhang, D. T. & Liu, X. G. mTOR signaling in T cell immunity and autoimmunity. Int. Rev. Immunol. 34, 50–66 (2015).
Weichhart, T., Hengstschlager, M. & Linke, M. Regulation of innate immune cell function by mTOR. Nat. Rev. Immunol. 15, 599–614 (2015).
O'Neill, L. A. & Hardie, D. G. Metabolism of inflammation limited by AMPK and pseudo-starvation. Nature 493, 346–355 (2013).
Michl, J., Ohlbaum, D. J. & Silverstein, S. C. 2-Deoxyglucose selectively inhibits Fc and complement receptor-mediated phagocytosis in mouse peritoneal macrophages. I. Description of the inhibitory effect. J. Exp. Med. 144, 1465–1483 (1976).
Hamilton, J. A., Vairo, G. & Lingelbach, S. R. CSF-1 stimulates glucose uptake in murine bone marrow-derived macrophages. Biochem. Biophys. Res. Commun. 138, 445–454 (1986).
Rodriguez-Prados, J. C. et al. Substrate fate in activated macrophages: a comparison between innate, classic, and alternative activation. J. Immunol. 185, 605–614 (2010).
Krawczyk, C. M. et al. Toll-like receptor-induced changes in glycolytic metabolism regulate dendritic cell activation. Blood 115, 4742–4749 (2010). This was one of the first papers to analyse the Warburg effect in DCs activated by TLR4.
Donnelly, R. P. et al. mTORC1-dependent metabolic reprogramming is a prerequisite for NK cell effector function. J. Immunol. 193, 4477–4484 (2014).
Michalek, R. D. et al. Cutting edge: distinct glycolytic and lipid oxidative metabolic programs are essential for effector and regulatory CD4+ T cell subsets. J. Immunol. 186, 3299–3303 (2011). In this paper, we see one of the first reports of different metabolic processes occurring in T cell subsets, with glycolysis and fatty acid synthesis being a feature of T H 1 cells, and fatty acid oxidation being more prominent in T reg cells.
Doughty, C. A. et al. Antigen receptor-mediated changes in glucose metabolism in B lymphocytes: role of phosphatidylinositol 3-kinase signaling in the glycolytic control of growth. Blood 107, 4458–4465 (2006).
Shi, L. Z. et al. HIF1α-dependent glycolytic pathway orchestrates a metabolic checkpoint for the differentiation of TH17 and Treg cells. J. Exp. Med. 208, 1367–1376 (2011). This paper is notable for demonstrating that the phenotype of the T cell can change when glycolysis is inhibited, effectively turning from a T H 17 cell into a T reg cell. This study ushered in the concept of metabolic reprogramming.
Gubser, P. M. et al. Rapid effector function of memory CD8+ T cells requires an immediate-early glycolytic switch. Nat. Immunol. 14, 1064–1072 (2013).
Shrestha, S. et al. Treg cells require the phosphatase PTEN to restrain TH1 and TFH cell responses. Nat. Immunol. 16, 178–187 (2015).
Huynh, A. et al. Control of PI(3) kinase in Treg cells maintains homeostasis and lineage stability. Nat. Immunol. 16, 188–196 (2015).
Wei, J. et al. Autophagy enforces functional integrity of regulatory T cells by coupling environmental cues and metabolic homeostasis. Nat. Immunol. 17, 277–285 (2016).
Everts, B. et al. TLR-driven early glycolytic reprogramming via the kinases TBK1-IKKɛ supports the anabolic demands of dendritic cell activation. Nat. Immunol. 15, 323–332 (2014).
Tannahill, G. M. et al. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature 496, 238–242 (2013). This is the first report to show that a TCA cycle intermediate, succinate, can serve as an activation signal in macrophages and promote IL-1 β production by activating HIF1 α.
Palsson-McDermott, E. M. et al. Pyruvate kinase M2 regulates Hif-1α activity and IL-1β induction and is a critical determinant of the warburg effect in LPS-activated macrophages. Cell Metab. 21, 65–80 (2015).
Luo, W. et al. Pyruvate kinase M2 is a PHD3-stimulated coactivator for hypoxia-inducible factor 1. Cell 145, 732–744 (2011).
Shirai, T. et al. The glycolytic enzyme PKM2 bridges metabolic and inflammatory dysfunction in coronary artery disease. J. Exp. Med. 213, 337–354 (2016).
Jha, A. K. et al. Network integration of parallel metabolic and transcriptional data reveals metabolic modules that regulate macrophage polarization. Immunity 42, 419–430 (2015).
Gerriets, V. A. et al. Metabolic programming and PDHK1 control CD4+ T cell subsets and inflammation. J. Clin. Invest. 125, 194–207 (2015).
Beier, U. H. et al. Essential role of mitochondrial energy metabolism in Foxp3+ T-regulatory cell function and allograft survival. FASEB J. 29, 2315–2326 (2015).
Procaccini, C. et al. The proteomic landscape of human ex vivo regulatory and conventional T cells reveals specific metabolic requirements. Immunity 44, 406–421 (2016).
De Rosa, V. et al. Glycolysis controls the induction of human regulatory T cells by modulating the expression of FOXP3 exon 2 splicing variants. Nat. Immunol. 16, 1174–1184 (2015).
Mukhopadhyay, R., Jia, J., Arif, A., Ray, P. S. & Fox, P. L. The GAIT system: a gatekeeper of inflammatory gene expression. Trends Biochem. Sci. 34, 324–331 (2009).
Chang, C. H. et al. Posttranscriptional control of T cell effector function by aerobic glycolysis. Cell 153, 1239–1251 (2013). An important paper that demonstrates that GAPDH 'moonlights' — its other role being to repress expression of IFN γ in T H 1 cells.
Moon, J. S. et al. mTORC1-induced HK1-dependent glycolysis regulates NLRP3 inflammasome activation. Cell Rep. 12, 102–115 (2015).
Haschemi, A. et al. The sedoheptulose kinase CARKL directs macrophage polarization through control of glucose metabolism. Cell Metab. 15, 813–826 (2012). The pentose phosphate pathway is shown in this study to be crucial for macrophage polarization.
O'Sullivan, D. et al. Memory CD8+ T cells use cell-intrinsic lipolysis to support the metabolic programming necessary for development. Immunity 41, 75–88 (2014).
Infantino, V. et al. The mitochondrial citrate carrier: a new player in inflammation. Biochem. J. 438, 433–436 (2011).
Michelucci, A. et al. Immune-responsive gene 1 protein links metabolism to immunity by catalyzing itaconic acid production. Proc. Natl Acad. Sci. USA 110, 7820–7825 (2013).
Clementi, E., Brown, G. C., Feelisch, M. & Moncada, S. Persistent inhibition of cell respiration by nitric oxide: crucial role of S-nitrosylation of mitochondrial complex I and protective action of glutathione. Proc. Natl Acad. Sci. USA 95, 7631–7636 (1998).
Carpenter, K. L. et al. Macrophages, lipid oxidation, ceroid accumulation and alpha-tocopherol depletion in human atherosclerotic lesions. Gerontology 41, 53–67 (1995).
Lusis, A. J. Atherosclerosis. Nature 407, 233–241 (2000).
Shoelson, S. E., Lee, J. & Goldfine, A. B. Inflammation and insulin resistance. J. Clin. Invest. 116, 1793–1801 (2006).
Freigang, S. et al. Fatty acid-induced mitochondrial uncoupling elicits inflammasome-independent IL-1α and sterile vascular inflammation in atherosclerosis. Nat. Immunol. 14, 1045–1053 (2013).
Malandrino, M. I. et al. Enhanced fatty acid oxidation in adipocytes and macrophages reduces lipid-induced triglyceride accumulation and inflammation. Am. J. Physiol. Endocrinol. Metab. 308, E756–E769 (2015).
Vats, D. et al. Oxidative metabolism and PGC-1β attenuate macrophage-mediated inflammation. Cell Metab. 4, 13–24 (2006).
Huang, S. C. et al. Cell-intrinsic lysosomal lipolysis is essential for alternative activation of macrophages. Nat. Immunol. 15, 846–855 (2014).
Nomura, M. et al. Fatty acid oxidation in macrophage polarization. Nat. Immunol. 17, 216–217 (2016).
Wang, R. et al. The transcription factor Myc controls metabolic reprogramming upon T lymphocyte activation. Immunity 35, 871–882 (2011).
Patsoukis, N. et al. PD-1 alters T-cell metabolic reprogramming by inhibiting glycolysis and promoting lipolysis and fatty acid oxidation. Nat. Commun. 6, 6692 (2015).
Bruno, L., von Boehmer, H. & Kirberg, J. Cell division in the compartment of naive and memory T lymphocytes. Eur. J. Immunol. 26, 3179–3184 (1996).
van der Windt, G. J. et al. CD8 memory T cells have a bioenergetic advantage that underlies their rapid recall ability. Proc. Natl Acad. Sci. USA 110, 14336–14341 (2013).
van der Windt, G. J. et al. Mitochondrial respiratory capacity is a critical regulator of CD8+ T cell memory development. Immunity 36, 68–78 (2012).
Posokhova, E. N., Khoshchenko, O. M., Chasovskikh, M. I., Pivovarova, E. N. & Dushkin, M. I. Lipid synthesis in macrophages during inflammation in vivo: effect of agonists of peroxisome proliferator activated receptors α and γ and of retinoid X receptors. Biochem. (Mosc) 73, 296–304 (2008).
Feingold, K. R. et al. Mechanisms of triglyceride accumulation in activated macrophages. J. Leukoc. Biol. 92, 829–839 (2012).
Ecker, J. et al. Induction of fatty acid synthesis is a key requirement for phagocytic differentiation of human monocytes. Proc. Natl Acad. Sci. USA 107, 7817–7822 (2010).
Moon, J. S. et al. UCP2-induced fatty acid synthase promotes NLRP3 inflammasome activation during sepsis. J. Clin. Invest. 125, 665–680 (2015).
Chen, H. W., Heiniger, H. J. & Kandutsch, A. A. Relationship between sterol synthesis and DNA-synthesis in phytohemagglutinin-stimulated mouse lymphocytes. Proc. Natl Acad. Sci. USA 72, 1950–1954 (1975).
Dufort, F. J. et al. Glucose-dependent de novo lipogenesis in B lymphocytes: a requirement for atp-citrate lyase in lipopolysaccharide-induced differentiation. J. Biol. Chem. 289, 7011–7024 (2014).
Lee, J. et al. Regulator of fatty acid metabolism, acetyl coenzyme a carboxylase 1, controls T cell immunity. J. Immunol. 192, 3190–3199 (2014).
Berod, L. et al. De novo fatty acid synthesis controls the fate between regulatory T and T helper 17 cells. Nat. Med. 20, 1327–1333 (2014). In this study, fatty acid metabolism is shown to govern the fate of T H cell subtypes.
Wang, C. et al. CD5L/AIM regulates lipid biosynthesis and restrains Th17 cell pathogenicity. Cell 163, 1413–1427 (2015).
Guglani, L. & Khader, S. A. Th17 cytokines in mucosal immunity and inflammation. Curr. Opin. HIV AIDS 5, 120–127 (2010).
Zielinski, C. E. et al. Pathogen-induced human TH17 cells produce IFN-γ or IL-10 and are regulated by IL-1β. Nature 484, 514–518 (2012).
Fessler, M. B. Regulation of adaptive immunity in health and disease by cholesterol metabolism. Curr. Allergy Asthma Rep. 15, 48 (2015).
Maceyka, M. & Spiegel, S. Sphingolipid metabolites in inflammatory disease. Nature 510, 58–67 (2014).
Kelly, D. & Wischmeyer, P. E. Role of L-glutamine in critical illness: new insights. Curr. Opin. Clin. Nutr. Metab. Care 6, 217–222 (2003).
Parry-Billings, M., Evans, J., Calder, P. C. & Newsholme, E. A. Does glutamine contribute to immunosuppression after major burns? Lancet 336, 523–525 (1990).
Wallace, C. & Keast, D. Glutamine and macrophage function. Metabolism 41, 1016–1020 (1992).
Murphy, C. & Newsholme, P. Importance of glutamine metabolism in murine macrophages and human monocytes to L-arginine biosynthesis and rates of nitrite or urea production. Clin. Sci. (Lond.) 95, 397–407 (1998).
Bellows, C. F. & Jaffe, B. M. Glutamine is essential for nitric oxide synthesis by murine macrophages. J. Surg. Res. 86, 213–219 (1999).
Carr, E. L. et al. Glutamine uptake and metabolism are coordinately regulated by ERK/MAPK during T lymphocyte activation. J. Immunol. 185, 1037–1044 (2010).
Crawford, J. & Cohen, H. J. The essential role of L-glutamine in lymphocyte differentiation in vitro. J. Cell. Physiol. 124, 275–282 (1985).
Le, A. et al. Glucose-independent glutamine metabolism via TCA cycling for proliferation and survival in B cells. Cell Metab. 15, 110–121 (2012).
Nakaya, M. et al. Inflammatory T cell responses rely on amino acid transporter ASCT2 facilitation of glutamine uptake and mTORC1 kinase activation. Immunity 40, 692–705 (2014).
Rath, M., Muller, I., Kropf, P., Closs, E. I. & Munder, M. Metabolism via arginase or nitric oxide synthase: two competing arginine pathways in macrophages. Front. Immunol. 5, 532 (2014).
MacMicking, J., Xie, Q. W. & Nathan, C. Nitric oxide and macrophage function. Annu. Rev. Immunol. 15, 323–350 (1997).
MacMicking, J. D. et al. Altered responses to bacterial infection and endotoxic shock in mice lacking inducible nitric oxide synthase. Cell 81, 641–650 (1995).
Albina, J. E. et al. Arginine metabolism in wounds. Am. J. Physiol. 254, E459–E467 (1988).
Pesce, J. T. et al. Arginase-1-expressing macrophages suppress Th2 cytokine-driven inflammation and fibrosis. PLoS Pathog. 5, e1000371 (2009).
Takele, Y. et al. Arginase activity in the blood of patients with visceral leishmaniasis and HIV infection. PLoS Negl. Trop. Dis. 7, e1977 (2013).
Rodriguez, P. C. et al. Regulation of T cell receptor CD3ζ chain expression by l-arginine. J. Biol. Chem. 277, 21123–21129 (2002).
Rodriguez, P. C., Quiceno, D. G. & Ochoa, A. C. l-arginine availability regulates T-lymphocyte cell-cycle progression. Blood 109, 1568–1573 (2007).
Cobbold, S. P. et al. Infectious tolerance via the consumption of essential amino acids and mTOR signaling. Proc. Natl Acad. Sci. USA 106, 12055–12060 (2009).
Silver, R. M. et al. Scleroderma, fasciitis, and eosinophilia associated with the ingestion of tryptophan. N. Engl. J. Med. 322, 874–881 (1990).
Stahl, J. L., Cook, E. B., Pariza, M. A., Cook, M. E. & Graziano, F. M. Effect of l-tryptophan supplementation on eosinophils and eotaxin in guinea pigs. Exp. Biol. Med. (Maywood) 226, 177–184 (2001).
Yoshida, R. & Hayaishi, O. Induction of pulmonary indoleamine 2,3-dioxygenase by intraperitoneal injection of bacterial lipopolysaccharide. Proc. Natl Acad. Sci. USA 75, 3998–4000 (1978).
Yoshida, R., Imanishi, J., Oku, T., Kishida, T. & Hayaishi, O. Induction of pulmonary indoleamine 2,3-dioxygenase by interferon. Proc. Natl Acad. Sci. USA 78, 129–132 (1981).
Werner, E. R. et al. Parallel induction of tetrahydrobiopterin biosynthesis and indoleamine 2,3-dioxygenase activity in human cells and cell lines by interferon-γ. Biochem. J. 262, 861–866 (1989).
Pfefferkorn, E. R. Interferon γ blocks the growth of Toxoplasma gondii in human fibroblasts by inducing the host cells to degrade tryptophan. Proc. Natl Acad. Sci. USA 81, 908–912 (1984).
Schroten, H. et al. Potential role of human brain microvascular endothelial cells in the pathogenesis of brain abscess: inhibition of Staphylococcus aureus by activation of indoleamine 2,3-dioxygenase. Neuropediatrics 32, 206–210 (2001).
Lee, G. K. et al. Tryptophan deprivation sensitizes activated T cells to apoptosis prior to cell division. Immunology 107, 452–460 (2002).
Munn, D. H. et al. Inhibition of T cell proliferation by macrophage tryptophan catabolism. J. Exp. Med. 189, 1363–1372 (1999).
Liu, H. et al. GCN2-dependent metabolic stress is essential for endotoxemic cytokine induction and pathology. Mol. Cell. Biol. 34, 428–438 (2014).
Bessede, A. et al. Aryl hydrocarbon receptor control of a disease tolerance defence pathway. Nature 511, 184–190 (2014).
Uyttenhove, C. et al. Evidence for a tumoral immune resistance mechanism based on tryptophan degradation by indoleamine 2,3-dioxygenase. Nat. Med. 9, 1269–1274 (2003). Tryptophan metabolism by the enzyme IDO is shown here to be crucial for antitumour immunity.
Okamoto, A. et al. Indoleamine 2,3-dioxygenase serves as a marker of poor prognosis in gene expression profiles of serous ovarian cancer cells. Clin. Cancer Res. 11, 6030–6039 (2005).
Munn, D. H. et al. Expression of indoleamine 2,3-dioxygenase by plasmacytoid dendritic cells in tumor-draining lymph nodes. J. Clin. Invest. 114, 280–290 (2004).
Weinlich, G., Murr, C., Richardsen, L., Winkler, C. & Fuchs, D. Decreased serum tryptophan concentration predicts poor prognosis in malignant melanoma patients. Dermatology 214, 8–14 (2007).
Holmgaard, R. B., Zamarin, D., Munn, D. H., Wolchok, J. D. & Allison, J. P. Indoleamine 2,3-dioxygenase is a critical resistance mechanism in antitumor T cell immunotherapy targeting CTLA-4. J. Exp. Med. 210, 1389–1402 (2013).
Yin, Y. et al. Normalization of CD4+ T cell metabolism reverses lupus. Sci Transl Med. 7, 274ra18 (2015).
Lee, C. F. et al. Preventing allograft rejection by targeting immune metabolism. Cell Rep. 13, 760–770 (2015).
Acknowledgements
L.A.J.O. acknowledges Science Foundation Ireland, The European Research Council and The Wellcome Trust for research funding.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Mechanistic target of rapamycin
-
(mTOR). An atypical serine/threonine kinase that is present in two distinct complexes. mTOR complex 1 (mTORC1), is composed of mTOR, Raptor, MLST8 (also known as GβL), PRAS40 and DEPTOR; it is inhibited by rapamycin.
- Electron transport chain
-
The series of proteins in the inner mitochondrial membrane that transfer electrons in a series of redox reactions, leading to proton pumping across the membrane.
- 2-deoxyglucose
-
A derivative of glucose that inhibit hexokinase, thereby blocking the first step in glycolysis.
- Aerobic glycolysis
-
Glycolysis occurring when oxygen is present.
- Foam cells
-
Fat-laden macrophages commonly seen in the plaques occurring in atherosclerosis.
- Futile cycle
-
Two metabolic pathways running in opposite directions that seem to cancel each other out metabolically.
- Metabolic enzymes
-
Enzymes in metabolic pathways that convert substrates into products. Major classes are dehydrogenases (which remove hydrogen from a substrate in an oxidation–reduction reaction), isomerases (which convert a molecule from one isomer to another), synthases (which link two molecules together without using ATP as an energy source), carboxylases (which add a carboxyl group to a substrate) and kinases (which add a phosphate group to a molecule).
Rights and permissions
About this article
Cite this article
O'Neill, L., Kishton, R. & Rathmell, J. A guide to immunometabolism for immunologists. Nat Rev Immunol 16, 553–565 (2016). https://doi.org/10.1038/nri.2016.70
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri.2016.70
This article is cited by
-
“Feed a Cold, Starve a Fever?” A Review of Nutritional Strategies in the Setting of Bacterial Versus Viral Infections
Current Nutrition Reports (2024)
-
Intestinal Microbiota Modulates the Antitumor Effect of Oncolytic Virus Vaccines in Colorectal Cancer
Digestive Diseases and Sciences (2024)
-
Fluoride-Induced Mitochondrial Dysfunction and Approaches for Its Intervention
Biological Trace Element Research (2024)
-
The role of tumor-associated macrophages in tumor immune evasion
Journal of Cancer Research and Clinical Oncology (2024)
-
ACLY as a modulator of liver cell functions and its role in Metabolic Dysfunction-Associated Steatohepatitis
Journal of Translational Medicine (2023)