Key Points
-
Biofilm bacteria have been demonstrated to be significant contributors to human disease, yet our understanding of the nature of biofilm infections and their effective treatment remains underdeveloped. Recent research has begun to unlock many of the mysteries associated with biofilm infections; however, substantial research will be necessary before adequate control of biofilm infections will be generally attainable.
-
Biofilms have been shown to be generally more resistant to antimicrobial chemotherapies than free-living bacteria. No current consensus exists regarding the mechanisms of biofilm resistance to antibacterial agents. Numerous competing theories are presently under investigation, yet the phenomenon of biofilm resistance remains a subject generating many questions but few answers.
-
Multiple factors appear to contribute to the overall resistance of biofilm bacteria. These include reduced metabolic and growth rates, protection by extracellular polymeric substances and specific resistance mechanisms conferred by the altered physiology of biofilm bacteria compared with planktonic bacteria.
-
The failure of antibacterial agents to rapidly penetrate into all areas of a biofilm has been considered as a contributing factor to biofilm resistance. Reports indicate that species-composition of biofilms and the choice of antibiotic have a marked impact on antibiotic penetration.
-
Biofilm cells have been shown by a number of investigators to have reduced growth rates, and this is believed to impact the effectiveness of antibiotics that target rapidly multiplying cells. Therefore, antibiotics such as the fluoroquinolones or macrolides may be better therapeutic choices than β-lactams when treating biofilm infections.
-
Altered physiological states of biofilm cells compared with planktonic cells have been demonstrated for a number of bacteria. The activation of specific resistance genes in biofilms has been demonstrated in a few instances. Specific resistance mechanisms should, therefore, be considered when treating biofilm infections.
-
A number of alternative approaches to antibacterial treatment have been proposed for biofilms. Many of these are non-lethal treatments that are expected to enhance the activity of currently used antibiotics. For example, manipulation of electrical fields has shown some promise in enhancing the activity of certain antibiotics against biofilms. The finding that in certain bacteria autoinducers mediate the production of virulence factors, and possibly also biofilm formation, has led to developmental work on autoinducer-blocking agents. These blocking agents are expected, in certain cases, to limit disease progression at the same time as antibiotics are being administered, and, in other cases, to act to enhance the activity of an antibiotic. Biofilm-dispersion agents are currently under development and are anticipated to result in improved access of antibiotics to bacteria, and possibly to alter the physiological status of the bacteria making them more susceptible to antibiotic exposure.
-
The current state of the field indicates that enhanced antimicrobial resistance is a general trait of biofilms and is the result of numerous specific factors which depend on the species involved, the environment of the biofilm and the antimicrobial agent used. It is expected, therefore, that the effective treatment of biofilms in the future will depend on tailoring treatment strategies to specific infection conditions rather than to any general phenomenon common to all biofilms.
Abstract
According to a public announcement by the US National Institutes of Health, “Biofilms are medically important, accounting for over 80% of microbial infections in the body”. Yet bacterial biofilms remain poorly understood and strategies for their control remain underdeveloped. Standard antimicrobial treatments typically fail to eradicate biofilms, which can result in chronic infection and the need for surgical removal of afflicted areas. The need to create effective therapies to counter biofilm infections presents one of the most pressing challenges in anti-bacterial drug development. In this article, the mechanisms that underlie biofilm resistance to antimicrobial chemotherapy will be examined, with particular attention being given to potential avenues for the effective treatment of biofilms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Lawrence, J. R., Korber, D. R., Hoyle, B. D., Costerton, J. W. & Caldwell, D. E. Optical sectioning of microbial biofilms. J. Bacteriol. 173, 6558–6567 (1991). One of the first descriptions of the 3-dimensional structure of natural biofilms.
Lawrence, J. R. & Neu, T. R. Confocal laser scanning microscopy for analysis of microbial biofilms. Methods Enzymol. 310, 131–144 (1999).
Lewandowski, Z., Stoodley, P., Altobelli, S. & Fukushima, E. Hydrodynamics and kinetics in biofilm systems — recent advances and new problems. Proceedings of the Second IAWQ International Specialized Conference on Biofilm Reactors. Paris, France, pp. 313–319 (1993).
DeBeer, D., Stoodley, P., Roe, F. & Lewandowski, Z. Effects of biofilm structure on oxygen distribution and mass transport. Biotech. Bioeng. 43, 1131–1138 (1994).
Davies, D. G. et al. The involvement of cell-to-cell signals in the development of a bacterial biofilm. Science 280, 295–298 (1998). The first paper to link biofilm development with intercellular communication.
Martinelli, D., Bachofen, R. & Brandl, H. Effect of medium composition, flow rate, and signaling compounds on the formation of soluble extracellular materials by biofilms of Chromobacterium violaceum. Appl. Microbiol. Biotechnol. 59, 278–283 (2002).
Huber, B. et al. Genetic analysis of functions involved in the late stages of biofilm development in Burkholderia cepacia H111. Mol. Microbiol. 46, 411–426 (2002).
National Institute of Dental Research. The Oral Health of United States Adults. The National Survey of Dental Caries in US Employed Adults and Seniors: 1985–1986. DHHS Pub. No. (NIH) 87–2868. (US Department of Health and Human Services, Bethesda, Maryland 1987).
National Institute of Dental Research. Oral health of United States children. The National Survey of Dental Caries in US School Children, 1986–1987. DHHS Pub. No. (NIH) 89–2247. (Department of Health and Human Services, Bethesda, Maryland 1989).
Passerini, L., Lam, K., Costerton, J. W. & King, E. G. Biofilms on indwelling vascular catheters. Crit. Care Med. 20, 665–673 (1992).
Pople, I. J., Bayston, R. & Hayward, R. D. Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J. Neurosurg. 77, 29–36 (1992).
Costerton, J. W. et al. Bacterial biofilms in nature and disease. Annu. Rev. Microbiol. 41, 435–464 (1987).
Hoiby, N. et al. in Microbial Biofilms (eds Lappin–Scott, H. M. & Costerton, J. W.) (Cambridge University Press, Cambridge, 1995).
Luppens, S. B., Reij, M. W. van der Heijden, R. W., Rombouts, F. M. & Abee, T. Development of a standard test to assess the resistance of Staphylococcus aureus biofilm cells to disinfectants. Appl. Environ. Microbiol. 68, 4194–4200 (2002).
Brown, M. R., Allison, D. G. & Gilbert, P. Resistance of bacterial biofilms to antibiotics: a growth-rate related effect? J. Antimicrob. Chemother. 22, 777–783 (1988).
Anwar, H., Strap, J. L. & Costerton, J. W. Establishment of aging biofilms: possible mechanism of bacterial resistance to antimicrobial therapy. Antimicrob. Agents Chemother. 36, 1347–1351 (1992).
Mah, T. F. & O'Toole, G. A. Mechanisms of biofilm resistance to antimicrobial agents. Trends Microbiol. 9, 34–39 (2001).
Sauer, K. & Camper, A. K. Characterization of phenotypic changes in Pseudomonas putida in response to surface-associated growth. J. Bacteriol. 183, 6579–6589 (2001).
Stewart, P. S. Mechanisms of antibiotic resistance in bacterial biofilms. Int. J. Med. Microbiol. 292, 107–113 (2002). An excellent review from an engineering perspective on antibiotic resistance in bacterial biofilms.
Donlan, R. M. & Costerton, J. W. Biofilms: survival mechanisms of clinically relevant microorganisms. Clin. Microbiol. Rev. 15, 167–193 (2002). A comprehensive review outlining many organisms of medical importance and what is known about their resistance to specific antibiotics.
Gilbert, P., Maira-Litran, T., McBain, A. J., Rickard, A. H. & White, F. W. The physiology and collective recalcitrance of microbial biofilm communities. Adv. Microb. Physiol. 46, 202–256 (2002). A thoughtful and insightful look at the mechanisms underlying the resistance of biofilms to antibiotic treatments.
Gilbert, P., Allison, D. G. & McBain, A. J. Biofilms in vitro and in vivo: do singular mechanisms imply cross-resistance?. J. Appl. Microbiol. Suppl. 98, S–110S (2002).
Yu, F. P. & McFeters, G. A. Rapid in situ assessment of physiological activities in bacterial biofilms using fluorescent probes. J. Microbiol. Methods 20, 1–10 (1994).
Huang, C. -T., Yu, F. P., McFeters, G. A. & Stewart, P. S. Nonuniform spatial patterns of respiratory activity within biofilms during disinfection. Appl. Environ. Microbiol. 61, 2252–2256 (1995). A classic paper that visually demonstrates the effect of an antimicrobial agent against a biofilm in situ.
Onarheim, H. et al. Outbreak of multiresistant Acenetobacter baumannii infection. Tidsskr. Nor. Laegeforen. 120, 1028–1033 (2000).
Still, J., Law, E., Friedman, B., Furman, S. & Newton, T. Vancomycin resistant organisms in a burn unit. South Med. J. 94, 810–812 (2001).
Rastegar, L. A., Bahrami, H. H. & Alaghebandan, R. Pseudomonas infections in Tohid Burn Center, Iran. Burns 24, 637–641 (1998).
Olson, M. E., Ceri, H., Morck, D. W., Buret, A. G. & Read, R. R. Biofilm bacteria: formation and comparative susceptibility to antibiotics. Can. J. Vet. Res. 66, 86–92 (2002).
Jensen, E. T. et al. Complement activation by Pseudomonas aeruginosa biofilms. Microb. Pathol. 15, 377–388 (1993).
Rogers, J., Phillip, F. & Olliff, C. The effects of extracellular slime from Staphylococcus epidermidis on phagocytic ingestion and killing. FEMS Immunol. Med. Microbiol. 9, 109–115 (1994).
Moran, F. J. et al. Phagocytosis and killing of slime-producing Staphylococcus epidermidis by polymorphonuclear leukocytes. Effects of sparfloxacin. Rev. Esp. Quimioter. 11, 52–57 (1998).
Costerton, J. W., Lewandowski, Z., Caldwell, D., Korber, D. & Lappin-Scott, H. M. Microbial biofilms. Annu. Rev. Microbiol. 49, 711–745 (1995).
Costerton, J. W., Stewart, P. S. & Greenberg, E. P. Bacterial biofilms: a common cause of persistent infections. Science 284, 1318–1322 (1999).
Meluleni, G. J., Grout, M., Evans, D. J. & Pier, G. B. Mucoid Pseudomonas aeruginosa growing in a biofilm in vitro are killed by opsonic antibodies to the mucoid exopolysaccharide capsule but not by antibodies produced during chronic lung infection in cystic fibrosis patients. J. Immunol. 155, 2029–2038 (1995).
Dasgupta, M. K. Biofilm causes decreased production of interferon-γ. J. Am. Soc. Nephrol. 7, 877–882 (1996).
Suci, P. A., Mittelman, M. W., Yu, F. P. & Geesey, G. G. Investigation of ciprofloxacin penetration into Pseudomonas aeruginosa biofilms. Antimicrob. Agents Chemother. 38, 2125–2133 (1994). An excellent paper describing a novel in situ method for determining antibiotic penetration into biofilms.
Vrany, J. D., Stewart, P. S. & Suci, P. S. Comparison of recalcitrance to ciprofloxacin and levofloxacin exhibited by Pseudomonas aeruginosa bofilms displaying rapid-transport characteristics. Antimicrob. Agents Chemother. 41, 1352–1358 (1997).
Anderl, J., Franklin, M. J. & Stewart, P. S. Role of antibiotic penetration limitation in Klebsiella pneumoniae biofilm resistance to ampicillin and ciprofloxicin. Antimicrob. Agents Chemother. 44, 1818–1824 (2000).
Stone, G., Wood, P., Dixon, M., Keyhan, M. & Matin, A. Tetracycline rapidly reaches all the constituent cells of uropothogenic Escherichia coli biofilms. Antimicrob. Agents Chemother. 46, 2458–2461 (2002).
Larsen, T. Susceptibility of Porphyromonas gingivalis in biofilms to amoxicillin, doxycycline and metronidazole. Oral Microbiol. Immunol. 5, 267–271 (2002).
Campanac, C., Pineau, L., Payard, A., Baziard-Mouysset, G. & Roques, C. Interactions between biocide cationic agents and bacterial biofilms. Antimicrob. Agents Chemother. 46, 1469–1474 (2002).
Stoodley, P., deBeer, D. & Lappin-Scott, H. M. Influence of electric fields and pH on biofilm structure as related to the bioelectric effect. Antimicrob. Agents Chemother. 41, 1876–1879 (1997).
Costerton, J. W., Ellis, B., Lam, K., Johnson, F. & Koury, A. E. Mechanism of electrical enhancement of efficacy of antibiotics in killing biofilm bacteria. Antimicrob. Agents Chemother. 38, 2803–2809 (1994). Introduction of a novel strategy using electrical fields to enhance the effectiveness of antibiotics against biofilms.
McLeod, B. R., Fortun, S., Costerton, J. W. & Stewart, P. S. Enhanced bacterial biofilm control using electromagnetic fields in combination with antibiotics. Methods Enzymol. 310, 656–670 (1999).
Sternberg, C. et al. Distribution of bacterial growth activity in flow-chamber biofilms. Appl. Environ. Microbiol. 65, 4108–4117 (1999). A landmark paper demonstrating the activity and positioning of single cells in biofilms in real time.
Ashby, M. J., Neale, J. E. & Critchley, I. A. Effect of antibiotics on non-growing planktonic cells and biofilms of Escherichia coli. J. Antimicrob. Chemotherapy 33, 443–452 (1994).
Shigeta, M. G. et al. Permeation of antimicrobial agents through Pseudomonas aeruginosa biofilms: a simple method. Chemotherapy 43, 340–345 (1997).
Shigeta, M., Komatsuzawa, M., Sugai, M., Suginaka, H. & Usui, T. Effect of the growth rate of Pseudomonas aeruginosa biofilms on the susceptibility to antimicrobial agents. Chemotherapy 43, 137–141 (1997).
Tanaka G. et al. Effect of the growth rate of Pseudomonas aeruginosa biofilms on the susceptibility to antimicrobial agents: beta-lactams and fluoroquinolones. Chemotherapy 45, 28–36 (1999).
Spoering A. L. & K. Lewis, K. Biofilms and planktonic cells of Pseudomonas aeruginosa have similar resistance to killing by antimicrobials. J. Bacteriol. 183, 6746–6751 (2001). An examination of bacterial resistance based on defects in preprogrammed cell death. This paper has stimulated considerable debate regarding the mechanism of biofilm resistance.
McCoy, W. F. & Costerton, J. W. Fouling biofilm development in tubular flow systems. Dev. in Indust. Microbiol. 23, 551–558 (1982).
Morisaki, H. Effect of solid-liquid interface on metabolic activity of E. coli. J. Gen. Appl. Microbiol. 29, 195–204 (1983).
Jeffrey, W. H. & Paul, J. H. Activity of an attached and free-living Vibrio sp. As measured by thymidine incorporation, p-iodonitrotetrazolium reduction, and ATP/ADP ratios. Appl. Environ. Microbiol. 51, 150–156 (1986).
Davies, D. G. & McFeters, G. A. Growth and comparative physiology of Klebsiella oxytoca attached to granular activated carbon particles and in liquid media. Microb. Ecol. 15, 165–175 (1988).
Davies, D. G. & Geesey, G. G. Regulation of the alginate biosynthesis gene algC in Pseudomonas aeruginosa during biofilm development in continuous culture. Appl. Environ. Microbiol. 61, 860–867 (1995).
Prigent-Combaret, C., Vidal, O., Dorel, C. & Lejeune, P. Abiotic surface sensing and biofilm-dependent regulation of gene expression in E. coli. J. Bacteriol. 181, 5993–6002 (1999).
Whiteley, M. et al. Gene expression in Pseudomonas aeruginosa biofilms. Nature 413, 860–864 (2001).
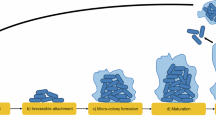
Sauer, K., Camper, A. K., Ehrlich, G. D., Costerton, J. W. & Davies, D. G. Pseudomonas aeruginosa displays multiple phenotypes as a biofilm. J. Bacteriol. 184, 1140–1154 (2002). A paper describing the different phenotypic stages of biofilm development using primarily a proteomics approach. It was the first paper to outline the complete life-cycle of a biofilm-forming pathogen.
Drenkard, E. & Ausubel, F. M. Pseudomonas biofilm formation and antibiotic resistance are linked to phenotypic variation. Nature 416, 740–743 (2002). An important paper linking phenotypic differences in biofilms to antibiotic susceptibility.
Schurr, M. J., Martin, D. W., Mudd, M. H. & Deretic, V. Gene cluster controlling conversion to alginate-overproducing phenotype in Pseudomonas aeruginosa: functional analysis in a heterologous host and role in the instability of mucoidy. J. Bacteriol. 176, 3375–3382 (1994).
O'Toole, G. A., Kaplan, H. B. & Kolter, R. Biofilm formation as microbial development. Annu. Rev. Microbiol. 54, 49–79 (2000).
Belas, R., Simon, M. & Silverman, M. Regulation of lateral flagella gene transcription in Vibrio parahaemolyticus. J. Bacteriol. 167, 210–218 (1986).
Dagastino, L., Goodman, A. E. & Marshall, K. C. Physiological responses induced in bacteria adhering to surfaces. Biofouling 4, 113–119 (1991).
Santos, R., Callow, M. E. & Bott, T. R. The structure of Pseudomonas fluorescens biofilms in contact with flowing systems. Biofouling 4, 319–336 (1991).
Davies, D. G., Chakrabarty, A. M. & Geesey, G. G. Exopolysaccharide production in biofilms: substratum activation of alginate gene expression in Pseudomonas aeruginosa. Appl. Environ. Microbiol. 59, 1181–1186 (1993). First report of the the detection of specific gene activity in bacteria at the single-cell level, in real time and in situ.
Dalton, H. M. & March, P. E. Molecular genetics of bacterial attachment and biofouling. Biotechnology 9, 252–255 (1998).
Dekkers, L. C. et al. Role of the O-antigen of lipopolysaccharide, and possible roles of growth rate and of NADH:ubiquinone oxidoreductase (nuo) in competitive tomato root-tip colonization by Pseudomonas fluorescens WCS365. Mol. Plant Microbe Interact. 11, 763–771 (1998).
O'Toole, G. A. & Kolter, R. Flagellar and twitching motility are necessary for Pseudomonas aeruginosa biofilm development. Mol. Microbiol. 30, 295–304 (1998).
O'Toole, G. A. & Kolter, R. Initiation of biofilm formation in Pseudomonas fluorescens WCS365 proceeds via multiple, convergent signalling pathways: a genetic analysis. Mol. Microbiol. 28, 419–461 (1998).
DeFlaun, M. F., Oppenheimer, S. R., Streger, S., Condee, C. W. & Fletcher, M. Alterations in adhesion, transport, and membrane characteristics in an adhesion-deficient pseudomonad. Appl. Environ. Microbiol. 65, 759–765 (1999).
Genevaux, P., Bauda, P., DuBow, M. S. & Oudega, B. Identification of Tn10 insertions in the rfaG, rfaP, and galU genes involved in lipopolysaccharide core biosynthesis that affect Escherichia coli adhesion. Arch. Microbiol. 172, 1–8 (1999).
Pratt, L. A. & Kolter, R. Genetic analysis of Escherichia coli biofilm formation: roles of flagella, motility, chemotaxis and type I pili. Mol. Microbiol. 30, 285–293 (1998).
Rodriguez-Herva, J. J., Reniero, D., Galli, E. & Ramos, J. L. Cell envelope mutants of Pseudomonas putida: physiological characterization and analysis of their ability to survive in soil. Environ. Microbiol. 1, 479–488 (1999).
Steyn B, Oosthuizen, M. C., MacDonald, R., Theron, J. & Brozel, V. S. The use of glass wool as an attachment surface for studying phenotypic changes in Pseudomonas aeruginosa biofilms by two-dimensional gel electrophoresis. Proteomics 1, 871–879 (2001).
Brözel, V. S., Strydom, G. M. & Cloete, T. E. E. A method for the study of de novo protein synthesis in Pseudomonas aeruginosa after attachment. Biofouling 8, 195–210 (1995).
Svensater, G., Welin, J., Wilkins, J. C., Beighton, D. & Hamilton, I. R. Protein expression by planktonic and biofilm cells of Streptococcus mutans. FEMS Microbiol. Lett. 205, 139–146 (2001).
Espinosa-Urgel, M., Salido, A. & Ramos, J. L. Genetic analysis of functions involved in adhesion of Pseudomonas putida to seeds. J. Bacteriol. 182, 2363–2369 (2000).
Grobe, K. J., Zahller, J. J. & Stewart, P. S. Role of dose concentraion in biocide efficacy against Pseudomonas aeruginosa. J. Indust. Microbiol. Biotechnol. 29, 10–15 (2002).
Allison, D. G., B. Ruiz, B., SanJose, C., Jaspe, A. & Gilbert, P. Extracellular products as mediators of the formation and detachment of Pseudomonas fluorescens biofilms. FEMS Microbiol. Lett. 167, 179–184 (1988).
Vats, N. & Lee, S. F. Active detachment of Streptococcus mutans cells adhered to epon-hydroxylapatite surfaces coated with salivary proteins in vitro. Arch. Oral Biol. 45, 305–314 (2000). An interesting and significant report on the regulation of autodispersion of biofilms.
Jackson, D. W. et al. Biofilm formation and dispersion under the influence of the global regulator CsrA of Escherichia coli. J. Bacteriol. 184, 290–301 (2002).
Choi, J. Y. et al. Identificationof virulence genes in a pathogenic strain of Pseudomonas aeruginosa by representational difference analysis. J. Bacteriol. 184, 952–961 (2002).
Hubank, M. & Schatz, D. G. Identifying differences in mRNA expression by representational difference analysis of cDNA. Nucleic Acids Res. 22, 5640–5648 (1994).
Jander, G., Rahme, L. G. & Ausubel, F. M. Positive correlation between virulence of Pseudomonas aeruginosa mutants in mice and insects. J. Bacteriol. 182, 3843–3845 (2000). A well-conducted investigation of the differences in virulence of an important pathogen in different model hosts.
Tan, M. W., Mahajan-Miklos, S. & Ausubel, F. M. Killing of Caenorhabditis elegans by Pseudomonas aeruginosa used to model mammalian bacterial pathogenesis. Proc. Natl Acad. Sci. USA 96, 715–720 (1999).
Tan, M. W., Rahme, L. G., Sternberg, J. A., Tompkins, R. G. & Ausubel, F. M. Pseudomonas aeruginosa killing of Caenorhabditis elegans used to identify P. aeruginosa virulence factors. Proc. Natl Acad. Sci. USA 96, 2408–2413 (1999).
Brooun, A., Liu, S. & Lewis, K. A dose-response study of antibiotic resistance in Pseudomonas aeruginosa biofilms. Antimicrob. Agents Chemother. 44, 640–466 (2000).
Lewis, K. Riddle of biofilm resistance. Antimicrob. Agents Chemother. 45, 999–1007 (2001).
Latifi, A., Foglino, M., Tanaka, K., Williams, P. & Lazdunski, A. A hierarchical quorum-sensing cascade in Pseudomonas aeruginosa links the transcriptional activators LasR and RhlR (VsmR) to expression of the stationary-phase sigma factor RpoS. Mol. Microbiol. 21, 1137–1146 (1996).
Fuqua, W. C., Winans, S. C. & Greenberg, E. P. Quorum sensing in bacteria: the LuxR-LuxI family of cell density-responsive transcriptional regulators. J. Bacteriol. 176, 269–275 (1994).
May, T. B. et al. Alginate synthesis by Pseudomonas aeruginosa: a key pathogenic factor in chronic pulmonary infections of cystic fibrosis patients. Clin. Microbiol. Rev. 4, 191–206 (1991).
Singh, P. et al. Quorum-sensing signals indicate that cystic fibrosis lungs are infected with bacterial biofilms. Nature 407, 762–764 (2000).
Author information
Authors and Affiliations
Related links
Related links
FURTHER INFORMATION
Encyclopedia of Life Sciences
US National Institutes of Health Guide: SBIR/STTR Study and Control of Microbial Biofilms
Glossary
- CONFOCAL LASER SCANNING MICROSCOPY
-
A microscopy technique which uses scanning laser light to excite fluorescent dyes within a thick sample, such as a biofilm. The image is collected in two dimensions and several images can be combined in an image stack to produce a cross sectional image through a sample or to create a three-dimensional rendering of the sample. CLSM is particularly useful for imaging the positioning of biological structures within a three dimensional space.
- MICROCOLONY
-
A microscopic aggregation of cells in a biofilm.
- GINGIVITIS
-
Infection of the gingival crevice (periodontal pocket) of the oral cavity with a variety of microorganisms, causing inflammation of the periodontal tissue and bone loss. Caused by members of the genus Capnocytophaga, Porphyromonas, Rothia and others.
- PLANKTONIC
-
Organisms that are free-floating in a fluid environment.
- MULTIDRUG EFFLUX PUMP
-
A molecular pump integrated into the cell envelop of certain bacteria which is able to transport antibiotics into and out of the cell.
- REGULON
-
A set of operons that are controlled by a single regulatory protein.
- NIDUS
-
Latin for nest, but in this context a place or point in a host where a pathogen can develop and breed.
- NOSOCOMIAL
-
Something acquired or originating in a hospital, such as a nosocomial infection.
- COMPELEMENT
-
A complex of blood serum proteins of the immune system that interact sequentially with antibody–antigen complexes.
- HUMORAL IMMUNE SYSTEM
-
Extracellular branch of the immune system mediated by antibodies.
- MINIMUM INHIBITORY CONCENTRATION
-
The minimum concentration of a substance required to prevent growth of a microoganism.
- EXOPOLYMERIC MATRIX
-
A network of long-chain polymers produced by microorganisms of a biofilm which supports the structure of the biofilm.
- AUXOTROPH
-
An organism that has acquired a nutritional requirement through the process of mutation.
- SPORULATION
-
The production an endospore by bacteria of the genera Clostridia and Bacillus.
- SIGMA FACTOR
-
Any of several bacterial DNA-binding proteins that direct the binding of DNA-directed RNA-polymerase to the promoter of an operon.
- SWARMER-TO-STALK CELL TRANSITION
-
Upon exhaustion of nutrients, members of the group of fruiting myxobacteria swarmer cells migrate together and undergo differentiation into stalk cells, forming a vertical structure rising above a surface.
- FRUITING-BODY
-
A structure of the fruiting myxobacteria at the end of a stalk composed of differentiated cells which are converted to myxospores (resting bodies).
- TRANSPOSON
-
A mobile segment of DNA that has the ability to integrate into a chromosome. Transposons usually carry genes that are used in transposition as well as other genes, often selectable markers, such as for antibiotic resistance.
- AUTODISPERSION
-
The disaggregation of a biofilm or biofilm microcolony as a result of physiological activity of the resident microorganisms.
- HAEMOLYMPH
-
The body fluid that bathes tissues of invertebrates having an open circulatory system.
Rights and permissions
About this article
Cite this article
Davies, D. Understanding biofilm resistance to antibacterial agents. Nat Rev Drug Discov 2, 114–122 (2003). https://doi.org/10.1038/nrd1008
Issue Date:
DOI: https://doi.org/10.1038/nrd1008
This article is cited by
-
Anti-biofilm properties of laser-synthesized, ultrapure silver–gold-alloy nanoparticles against Staphylococcus aureus
Scientific Reports (2024)
-
Inhibition and eradication effects of Thymus leptobotrys and Thymus satureioïdes essential oils against multidrug resistant Acinetobacter baumannii biofilms
Biologia (2024)
-
Phage Therapy for Respiratory Infections: Opportunities and Challenges
Lung (2024)
-
Unveiling antibiofilm potential: proteins from Priestia sp. targeting Staphylococcus aureus biofilm formation
Antonie van Leeuwenhoek (2024)
-
Near infrared II excitation nanoplatform for photothermal/chemodynamic/antibiotic synergistic therapy combating bacterial biofilm infections
Journal of Nanobiotechnology (2023)