Abstract
Accumulation of pathological tau protein is a major hallmark of Alzheimer's disease. Tau protein spreads from the entorhinal cortex to the hippocampal region early in the disease. Microglia, the primary phagocytes in the brain, are positively correlated with tau pathology, but their involvement in tau propagation is unknown. We developed an adeno-associated virus–based model exhibiting rapid tau propagation from the entorhinal cortex to the dentate gyrus in 4 weeks. We found that depleting microglia dramatically suppressed the propagation of tau and reduced excitability in the dentate gyrus in this mouse model. Moreover, we demonstrate that microglia spread tau via exosome secretion, and inhibiting exosome synthesis significantly reduced tau propagation in vitro and in vivo. These data suggest that microglia and exosomes contribute to the progression of tauopathy and that the exosome secretion pathway may be a therapeutic target.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Accession codes
References
Braak, H. & Braak, E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 82, 239–259 (1991).
Clavaguera, F. et al. Transmission and spreading of tauopathy in transgenic mouse brain. Nat. Cell Biol. 11, 909–913 (2009).
Ahmed, Z. et al. A novel in vivo model of tau propagation with rapid and progressive neurofibrillary tangle pathology: the pattern of spread is determined by connectivity, not proximity. Acta Neuropathol. 127, 667–683 (2014).
Boluda, S. et al. Differential induction and spread of tau pathology in young PS19 tau transgenic mice following intracerebral injections of pathological tau from Alzheimer's disease or corticobasal degeneration brains. Acta Neuropathol. 129, 221–237 (2015).
Iba, M. et al. Synthetic tau fibrils mediate transmission of neurofibrillary tangles in a transgenic mouse model of Alzheimer's-like tauopathy. J. Neurosci. 33, 1024–1037 (2013).
Harris, J.A. et al. Human P301L-mutant tau expression in mouse entorhinal-hippocampal network causes tau aggregation and presynaptic pathology but no cognitive deficits. PLoS ONE 7, e45881 (2012).
de Calignon, A. et al. Propagation of tau pathology in a model of early Alzheimer's disease. Neuron 73, 685–697 (2012).
Liu, L. et al. Trans-synaptic spread of tau pathology in vivo. PLoS ONE 7, e31302 (2012).
Peeraer, E. et al. Intracerebral injection of preformed synthetic tau fibrils initiates widespread tauopathy and neuronal loss in the brains of tau transgenic mice. Neurobiol. Dis. 73, 83–95 (2015).
Yamada, K. et al. Neuronal activity regulates extracellular tau in vivo. J. Exp. Med. 211, 387–393 (2014).
Sanders, D.W. et al. Distinct tau prion strains propagate in cells and mice and define different tauopathies. Neuron 82, 1271–1288 (2014).
Vingtdeux, V., Sergeant, N. & Buee, L. Potential contribution of exosomes to the prion-like propagation of lesions in Alzheimer's disease. Front. Physiol. 3, 229 (2012).
Saman, S. et al. Exosome-associated tau is secreted in tauopathy models and is selectively phosphorylated in cerebrospinal fluid in early Alzheimer disease. J. Biol. Chem. 287, 3842–3849 (2012).
Fiandaca, M.S. et al. Identification of preclinical Alzheimer's disease by a profile of pathogenic proteins in neurally derived blood exosomes: a case-control study. Alzheimers Dement. 11, 600–607 (2015).
Neumann, H., Kotter, M.R. & Franklin, R.J. Debris clearance by microglia: an essential link between degeneration and regeneration. Brain 132, 288–295 (2009).
Schafer, D.P. et al. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron 74, 691–705 (2012).
El Andaloussi, S., Mager, I., Breakefield, X.O. & Wood, M.J. Extracellular vesicles: biology and emerging therapeutic opportunities. Nat. Rev. Drug Discov. 12, 347–357 (2013).
Ghoshal, N. et al. Tau-66: evidence for a novel tau conformation in Alzheimer's disease. J. Neurochem. 77, 1372–1385 (2001).
Serrano-Pozo, A. et al. Reactive glia not only associates with plaques but also parallels tangles in Alzheimer's disease. Am. J. Pathol. 179, 1373–1384 (2011).
Shevtsova, Z., Malik, J.M., Michel, U., Bahr, M. & Kugler, S. Promoters and serotypes: targeting of adeno-associated virus vectors for gene transfer in the rat central nervous system in vitro and in vivo. Exp. Physiol. 90, 53–59 (2005).
Schofield, E., Kersaitis, C., Shepherd, C.E., Kril, J.J. & Halliday, G.M. Severity of gliosis in Pick's disease and frontotemporal lobar degeneration: tau-positive glia differentiate these disorders. Brain 126, 827–840 (2003).
Fricker, M. et al. MFG-E8 mediates primary phagocytosis of viable neurons during neuroinflammation. J. Neurosci. 32, 2657–2666 (2012).
Yoshiyama, Y. et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron 53, 337–351 (2007).
Elmore, M.R. et al. Colony-stimulating factor 1 receptor signaling is necessary for microglia viability, unmasking a microglia progenitor cell in the adult brain. Neuron 82, 380–397 (2014).
Qu, Y., Franchi, L., Nunez, G. & Dubyak, G.R. Nonclassical IL-1 beta secretion stimulated by P2X7 receptors is dependent on inflammasome activation and correlated with exosome release in murine macrophages. J. Immunol. 179, 1913–1925 (2007).
Kadiu, I., Narayanasamy, P., Dash, P.K., Zhang, W. & Gendelman, H.E. Biochemical and biologic characterization of exosomes and microvesicles as facilitators of HIV-1 infection in macrophages. J. Immunol. 189, 744–754 (2012).
Perez-Gonzalez, R., Gauthier, S.A., Kumar, A. & Levy, E. The exosome secretory pathway transports amyloid precursor protein carboxyl-terminal fragments from the cell into the brain extracellular space. J. Biol. Chem. 287, 43108–43115 (2012).
Thery, C., Amigorena, S., Raposo, G. & Clayton, A. Isolation and characterization of exosomes from cell culture supernatants and biological fluids. Curr. Protoc. Cell Biol. Ch. 3, Unit 3.22 (2006).
Trajkovic, K. et al. Ceramide triggers budding of exosome vesicles into multivesicular endosomes. Science 319, 1244–1247 (2008).
Brown, G.C. & Neher, J.J. Microglial phagocytosis of live neurons. Nat. Rev. Neurosci. 15, 209–216 (2014).
Ittner, L.M. et al. Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer's disease mouse models. Cell 142, 387–397 (2010).
Clavaguera, F. et al. Brain homogenates from human tauopathies induce tau inclusions in mouse brain. Proc. Natl. Acad. Sci. USA 110, 9535–9540 (2013).
Lasagna-Reeves, C.A. et al. Alzheimer brain-derived tau oligomers propagate pathology from endogenous tau. Sci. Rep. 2, 700 (2012).
Agosta, F. et al. Myeloid microvesicles in cerebrospinal fluid are associated with myelin damage and neuronal loss in mild cognitive impairment and Alzheimer disease. Ann. Neurol. 76, 813–825 (2014).
Lasagna-Reeves, C.A. et al. Identification of oligomers at early stages of tau aggregation in Alzheimer's disease. FASEB J. 26, 1946–1959 (2012).
Théry, C., Ostrowski, M. & Segura, E. Membrane vesicles as conveyors of immune responses. Nat. Rev. Immunol. 9, 581–593 (2009).
Lu, Z. et al. Phagocytic activity of neuronal progenitors regulates adult neurogenesis. Nat. Cell Biol. 13, 1076–1083 (2011).
Santacruz, K. et al. Tau suppression in a neurodegenerative mouse model improves memory function. Science 309, 476–481 (2005).
Castillo-Carranza, D.L. et al. Passive immunization with Tau oligomer monoclonal antibody reverses tauopathy phenotypes without affecting hyperphosphorylated neurofibrillary tangles. J. Neurosci. 34, 4260–4272 (2014).
Danzer, K.M. et al. Exosomal cell-to-cell transmission of alpha synuclein oligomers. Mol. Neurodegener. 7, 42 (2012).
Alvarez-Erviti, L. et al. Lysosomal dysfunction increases exosome-mediated alpha-synuclein release and transmission. Neurobiol. Dis. 42, 360–367 (2011).
Arellano-Anaya, Z.E. et al. Prion strains are differentially released through the exosomal pathway. Cell. Mol. Life Sci. 72, 1185–1196 (2015).
Phinney, A.L. et al. Cerebral amyloid induces aberrant axonal sprouting and ectopic terminal formation in amyloid precursor protein transgenic mice. J. Neurosci. 19, 8552–8559 (1999).
Yamamoto, M., Kiyota, T., Walsh, S.M. & Ikezu, T. Kinetic analysis of aggregated amyloid-beta peptide clearance in adult bone-marrow-derived macrophages from APP and CCL2 transgenic mice. J. Neuroimmune Pharmacol. 2, 213–221 (2007).
Lewis, J. et al. Neurofibrillary tangles, amyotrophy and progressive motor disturbance in mice expressing mutant (P301L) tau protein. Nat. Genet. 25, 402–405 (2000).
Jicha, G.A., Bowser, R., Kazam, I.G. & Davies, P. Alz-50 and MC-1, a new monoclonal antibody raised to paired helical filaments, recognize conformational epitopes on recombinant tau. J. Neurosci. Res. 48, 128–132 (1997).
Otvos, L. Jr. et al. Monoclonal antibody PHF-1 recognizes tau protein phosphorylated at serine residues 396 and 404. J. Neurosci. Res. 39, 669–673 (1994).
Butovsky, O. et al. Targeting miR-155 restores abnormal microglia and attenuates disease in SOD1 mice. Ann. Neurol. 77, 75–99 (2015).
Butovsky, O. et al. Identification of a unique TGF-β-dependent molecular and functional signature in microglia. Nat. Neurosci. 17, 131–143 (2014).
Vosshall, L.B., Wong, A.M. & Axel, R. An olfactory sensory map in the fly brain. Cell 102, 147–159 (2000).
Hama, H. et al. Scale: a chemical approach for fluorescence imaging and reconstruction of transparent mouse brain. Nat. Neurosci. 14, 1481–1488 (2011).
Tyler, W.A. & Haydar, T.F. Multiplex genetic fate mapping reveals a novel route of neocortical neurogenesis, which is altered in the Ts65Dn mouse model of Down syndrome. J. Neurosci. 33, 5106–5119 (2013).
Kiyota, T. et al. CCL2 accelerates microglia-mediated Aβ oligomer formation and progression of neurocognitive dysfunction. PLoS ONE 4, e6197 (2009).
Kiyota, T., Ingraham, K.L., Jacobsen, M.T., Xiong, H. & Ikezu, T. FGF2 gene transfer restores hippocampal functions in mouse models of Alzheimer's disease and has therapeutic implications for neurocognitive disorders. Proc. Natl. Acad. Sci. USA 108, E1339–E1348 (2011).
Kiyota, T. et al. AAV serotype 2/1-mediated gene delivery of anti-inflammatory interleukin-10 enhances neurogenesis and cognitive function in APP+PS1 mice. Gene Ther. 19, 724–733 (2012).
Beaudoin, G.M. III et al. Culturing pyramidal neurons from the early postnatal mouse hippocampus and cortex. Nat. Protoc. 7, 1741–1754 (2012).
Flach, K. et al. Tau oligomers impair artificial membrane integrity and cellular viability. J. Biol. Chem. 287, 43223–43233 (2012).
Blasi, E., Barluzzi, R., Bocchini, V., Mazzolla, R. & Bistoni, F. Immortalization of murine microglial cells by a v-raf/v-myc carrying retrovirus. J. Neuroimmunol. 27, 229–237 (1990).
Ellman, G.L., Courtney, K.D., Andres, V. Jr. & Feather-Stone, R.M. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. 7, 88–95 (1961).
Roccaro, A.M. et al. BM mesenchymal stromal cell-derived exosomes facilitate multiple myeloma progression. J. Clin. Invest. 123, 1542–1555 (2013).
Freilich, R.W., Woodbury, M.E. & Ikezu, T. Integrated expression profiles of mRNA and miRNA in polarized primary murine microglia. PLoS ONE 8, e79416 (2013).
Tabatadze, N. et al. Inhibition of neutral sphingomyelinase-2 perturbs brain sphingolipid balance and spatial memory in mice. J. Neurosci. Res. 88, 2940–2951 (2010).
Acknowledgements
The authors thank M. Ericsson (Electron Microscopy Facility, Harvard Medical School) for electron microscopic imaging services; P. Davies (Albert Einstein College of Medicine) for providing the MC1, CP13 and PHF1 antibodies; R. Kayed (University of Texas Medical Branch) for providing the T22 polyclonal antibody; Plexxikon, Inc. for providing PLX3397 and control chows; and M. Hasselmo and S. Przedborski for critical reading of the manuscript. This work is supported in part by grants from Alzheimer's Association (T.I.), Alzheimer's Art Quilt Initiative (T.I.), Boston University Alzheimer's Disease Center (P30AG013846, T.I.), BrightFocus Foundation (H.A.) and Coins for Alzheimer's Research Trust (T.I.).
Author information
Authors and Affiliations
Contributions
T.I. and H.A. designed the AAV-GFP/tau injection mouse model and initiated the study. M.M. and J.L. performed field recording electrophysiology and analyses; S.I. and H.A. cultured primary neuronal cells; H.A., S.I. and T.I. purified exosomes for electron microscopy and biochemical analyses; T.H. performed two-photon imaging and laser-scanning confocal microscopy; O.B. generated and provided the Pr2ry12 antibody, performed data analysis and edited the manuscript; B.W. provided tau antibodies, performed data analysis and wrote the manuscript; S.K. generated and provided AAV vectors, performed data analysis and edited the manuscript; and H.A., S.I., J.L., S.T., M.M. and T.I. designed and performed experiments and data analyses and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 AAV-GFP injection in the MEC of the mouse brain
C57Bl/6 mice at 4 months of age were injected with AAV-GFP into the MEC and sacrificed at 7 days post injection (dpi). (a) Brains were sectioned with 0.5-mm thickness, followed by 4M urea containing Scale solution treatment to make brain transparent. (c) Green fluorescence protein (GFP) was detected in MEC injected site. (d) Immunofluorescence of GFP (green) with GFAP (astrocytic marker, red) (e) Iba1 (mononuclear phagocyte maker, red) and (f) NeuN (neuron marker, red) in the MEC of injected mouse brain; Scale bars: 25 μm. (Scheme in b adapted from The Mouse Brain in Stereotaxic Coordinates 2nd ed (2001); p.333).
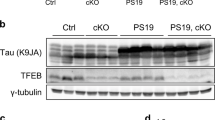
Supplementary Figure 2 Cytotoxic changes of tau-bearing neurons in the DG and reduction of changes by microglial depletion or nSMase2 inhibition in two different tau mouse models
(a) Cleaved caspase-3 (green), AT8 (pTau, red), and Dapi (blue) staining in the dentate granule cell layer (GCL) of AAV-GFP/tau mice at 28 dpi. Scale bar: 20 μm. GFP signal was quenched by methanol/acetone treatment of tissue sections prior to the immunostaining. (b,c) AAV-GFP/tau mice or PS19 mice were treated for microglial depletion by feeding mice with PLX3397 chow (upper panel) or nSMase2 inhibition by ip injection of GW4869 (lower panel). The frozen tissue sections were immunostained for cleaved caspase-3 (red) and Dapi (blue) in the GCL of AAV-GFP/tau mice at 28 dpi (A) or PS19 tau mice at 3.5 months of age (B); scale bars: 10 μm.
Supplementary Figure 3 Microglial density after AAV-GFP/tau injection into the MEC and depletion of microglia by clodronate liposome or PLX3397
(a,b) AAV-GFP or AAV-GFP/tau mice are subjected to immunofluorescence of Iba1 (mononuclear phagocyte marker, red) and Dapi (blue) in the DG at 7 or 28 dpi. (b) Quantification of microglial density in the DG. N.D.: No statistical difference between AAV-GFP and AAV-GFP/tau mice at 7 or 28 dpi as determined by one-way ANOVA (p>0.999, t(32)=0.0, n=3, 17 sections per group for 7 dpi; p=0.3231, t(42)=0.999, n=3, 22 sections mice per group for 28 dpi). Scale bar: 50 μm (c) C57BL/6 mice are pre-treated with clodronate liposome (CL-Lip) or PBS liposome (PBS-Lip) through a cannula implanted into the lateral ventricle at the time of AAV-GFP/tau injection until 28 dpi (a total of 4 week treatment, see Supplementary Figure 6 for details). PBS-Lip was injected in the control group. For PLX3397 study, C57BL/6 mice are pre-fed with the control or PLX-containing chow for 4 weeks prior to the AAV-GFP/tau injection, and maintained in the same chow until 28 dpi (a total of 8 week treatment). immunofluorescence of P2ry12 (microglia-specific marker, green) and CD169 (infiltrating monocytes marker, red) in the DG of AAV-GFP/tau mice at 28 dpi. Scale bar: 50 μm.
Supplementary Figure 4 Colocalization of pTau within Iba1-positive microglia
(a) Sequential imaging of confocal microscopy in the hippocampal area of the 6 month-old PS19 mouse brain. Green; AT8 (red), Iba1 (green). Scale bar: 10 μm (b) Double-immunogold labeling and electron microscopy in the hippocampal area of the 9-month-old PS19 mouse brain. 15-nm gold particles bind to Iba1 and 10-nm gold particles bind to PHF1 (pTau at pSer396/Ser404). Scale bars: 100 nm.
Supplementary Figure 5 Microglial depletion by clodronate liposome
(a) Cannula coordinate and time point for the CL-liposome ICV injection. (b) CL or PBS-Lip was ICV injected once a week for 4 weeks through the implanted cannula for one month after the AAV-GFP/tau injection. (c) Iba1 and Dapi staining in periventricular zone (top panels) and hippocampus (bottom panels). Scale bars: top panels: 25 μm; bottom panels: 50 μm (Scheme in a adapted from The Mouse Brain in Stereotaxic Coordinates second edition (2001), p. 83).
Supplementary Figure 6 Quantification of hTau in the MEC of AAV-GFP/tau-injected mice and PLX treatment and gene expression profile of immune molecules in the hippocampus
PLX3397 (or control) chow-fed C57BL/6 mice were injected with AAV-GFP/tau into the MEC and hippocampal regions were isolated at 28 dpi. (a) Quantification of hTau in the MEC using hTau specific ELISA. No statistical difference between control- and PLX-chow fed groups (p=0.8515, t(4)=0.1996, n=3 per group). (b) Gene expression profiles of pro-inflammatory cytokines (Tnfa, Il1b, and Il6) and anti-inflammatory cytokines (Il10 and Tgfb1) in the hippocampus of control or PLX chow-fed mice with AAV-GFP/tau injection. Each column represents ΔΔCT value vs. age-matched untreated C57BL/6 mice. p<0.0001, F(1,20)=77.29, n= 3 per group as determined by two-way ANOVA and multiple comparison tests. t(20)=2.987 (Tnfa), 2.877 (Il1b), 5.422 (Il6), 4.852 (Il10), and 3.610 (Tgfb1). *P < 0.05, **P < 0.01 and ***P < 0.001 between control and PLX group as determined by two-way ANOVA and multiple comparison tests (n=3 per group).
Supplementary Figure 7 Aggregation of purified hTau and microglial phagocytosis in vitro.
(a) Recombinant hTau protein was aggregated in the presence of heparin for 0-24 hrs as described in methods, and subjected to western blotting using HT7 (anti-hTau mAb). High molecular weight tau bands (120kDa and above) are visible even at 0 time point. (b) Quantification of tau oligomers by dot-blot analysis of aggregated tau protein for 0-72 hours. Tau oligomerization is increased after 3 hr incubation and is saturated by 24 hrs. (c) Murine primary microglia (MG) are treated with aggregated tau ± 1μM cytochalasin D (CyD, phagocytosis inhibitor) for 30 min, and the cells were washed with PBS and fixed with 4% paraformaldehyde for immunofluorescence using HT7 (green) and Dapi (blue); scale bar: 50μm. (d) After the phagocytosis assay of MG or BV-2 cells (murine microglial cell line), the cells were trypsinized to remove extracellular tau, and subjected to hTau ELISA. MG: p=0.0005, F(2,6)=34.93, q(6)=11.82 (MG no hTau vs. MG hTau), 5.781 (MG no hTau vs. MG hTau+CyD), and 6.039 (MG hTau vs. MG hTau+CyD). BV2: p=0.0005, F(2,6)=34.94, q(6)=11.80 (BV2 no hTau vs. BV2 hTau), 5.285 (BV2 no hTau vs. BV2 hTau+CyD), 6.517 (BV2 hTau vs. BV2+CyD). *P < 0.05, **P < 0.01 and ***P < 0.001 as determined by one-way ANOVA and Tukey post hoc.
Supplementary Figure 8 nSMase2 knockdown and purified tau-containing exosomes injected into the OML of mouse brain
(a) Neutral sphingomyeliase-2 (nSMase2) mRNA expression levels in mouse primary microglia treated with siRNA against murine nSMase2 or scramble siRNA. (b) Purified tau-containing exosomes from hTau-phagocytosed microglia was DiI-labeled. (c) One μl of the exosomal fraction from microglia with hTau+LPS+ATP+ or hTau-LPS-ATP+ treatment, and 1 to 50 ng/μl of aggregated recombinant hTau were blotted with HT7 or Tsg101. Full-length blots/gels are presented in Supplementary Figure 10. (d) Immunofluorescence of of HT7 (green), DiI (exosome, red), Dapi (blue) of mouse brain sections after injection of tau containing exosomes to the OML of the DG of C57BL/6 mice. Scale bar: 200 μm.
Supplementary Figure 9 Quantification of hTau in the MEC of AAV-GFP/tau injected mice and GW4869 treatment and gene expression profile of immune molecules in the hippocampus
C57BL/6 mice were injected with AAV-GFP/tau into the MEC, had daily ip injection of 1.25 mg/kg of GW4869 or 200μl of 5% DMSO in saline (control vehicle) from 0 to 28 dpi, and the MEC and hippocampal regions were isolated at 28 dpi. (a) Quantification of hTau in the MEC using hTau specific ELISA. No statistical difference between DMSO- and GW4869-treated groups (p=0.9295, t(4)=0.0942, n=3 per group). (b) Gene expression profiles of pro-inflammatory cytokines (Tnfa, Il1b, and Il6) and anti-inflammatory cytokines (Il10 and Tgfb1) in the hippocampus of DMSO or GW4869-treated AAV-GFP/tau mice. Each column represents ΔΔCT value vs. age-matched untreated C57BL/6 mice. p<0.0001, F(1,20)=28.89, t(20)=2.819 (Tnfa), 1.535 (Il1b), 1.114 (Il6), 4.725 (Il10), and 1.826 (Tgfb1) groups as determined by two-way ANOVA and multiple comparison tests (n=3 per group). *** P < 0.001 between DMSO and GW4869.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–10 (PDF 2997 kb)
Rights and permissions
About this article
Cite this article
Asai, H., Ikezu, S., Tsunoda, S. et al. Depletion of microglia and inhibition of exosome synthesis halt tau propagation. Nat Neurosci 18, 1584–1593 (2015). https://doi.org/10.1038/nn.4132
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nn.4132
This article is cited by
-
Cell type-specific roles of APOE4 in Alzheimer disease
Nature Reviews Neuroscience (2024)
-
Neuropathogenesis-on-chips for neurodegenerative diseases
Nature Communications (2024)
-
P2X7 Receptor: an Emerging Target in Alzheimer’s Disease
Molecular Neurobiology (2024)
-
Exosomes: A Cellular Communication Medium That Has Multiple Effects On Brain Diseases
Molecular Neurobiology (2024)
-
Integrating TSPO PET imaging and transcriptomics to unveil the role of neuroinflammation and amyloid-β deposition in Alzheimer’s disease
European Journal of Nuclear Medicine and Molecular Imaging (2024)