Abstract
Asymmetric dimethylarginine (ADMA) and monomethyl arginine (L-NMMA) are endogenously produced amino acids that inhibit all three isoforms of nitric oxide synthase (NOS)1. ADMA accumulates in various disease states, including renal failure, diabetes and pulmonary hypertension, and its concentration in plasma is strongly predictive of premature cardiovascular disease and death2,3,4. Both L-NMMA and ADMA are eliminated largely through active metabolism by dimethylarginine dimethylaminohydrolase (DDAH)5 and thus DDAH dysfunction may be a crucial unifying feature of increased cardiovascular risk. However, despite considerable interest in this pathway and in the role of ADMA as a cardiovascular risk factor, there is little evidence to support a causal role of ADMA in pathophysiology. Here we reveal the structure of human DDAH-1 and probe the function of DDAH-1 both by deleting the DDAH1 gene in mice and by using DDAH-specific inhibitors which, as we demonstrate by crystallography, bind to the active site of human DDAH-1. We show that loss of DDAH-1 activity leads to accumulation of ADMA and reduction in NO signaling. This in turn causes vascular pathophysiology, including endothelial dysfunction, increased systemic vascular resistance and elevated systemic and pulmonary blood pressure. Our results also suggest that DDAH inhibition could be harnessed therapeutically to reduce the vascular collapse associated with sepsis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Accession codes
References
Vallance, P., Leone, A., Calver, A., Collier, J. & Moncada, S. Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet 339, 572–575 (1992).
Schnabel, R. et al. Asymmetric dimethylarginine and the risk of cardiovascular events and death in patients with coronary artery disease: results from the AtheroGene study. Circ. Res. 97, e53–e59 (2005).
Ravani, P. et al. Asymmetrical dimethylarginine predicts progression to dialysis and death in patients with chronic kidney disease: a competing risks modeling approach. J. Am. Soc. Nephrol. 16, 2449–2455 (2005).
Cooke, J.P. Asymmetric dimethylarginine: the uber marker? Circulation 109, 1813–1819 (2004).
Vallance, P. & Leiper, J. Blocking NO synthesis: how, where and why? Nat. Rev. Drug Discov. 1, 939–950 (2002).
McBride, A.E. & Silver, P.A. State of the arg: protein methylation at arginine comes of age. Cell 106, 5–8 (2001).
Rossiter, S. et al. Selective substrate-based inhibitors of mammalian dimethylarginine dimethylaminohydrolase. J. Med. Chem. 48, 4670–4678 (2005).
Murray-Rust, J. et al. Structural insights into the hydrolysis of cellular nitric oxide synthase inhibitors by dimethylarginine dimethylaminohydrolase. Nat. Struct. Biol. 8, 679–683 (2001).
Leiper, J., Murray-Rust, J., McDonald, N. & Vallance, P. S-nitrosylation of dimethylarginine dimethylaminohydrolase regulates enzyme activity: further interactions between nitric oxide synthase and DDAH. Proc. Natl. Acad. Sci. USA 99, 13527–13532 (2002).
Ichinose, F., Roberts, J.D. & Zapol, W.M. Inhaled nitric oxide a selective pulmonary vasodilator, current use and therapeutic potential. Circulation 109, 3106–3111 (2004).
Pullamsetti, S. et al. Increased levels and reduced catabolism of asymmetric and symmetric dimethylarginine in pulmonary hypertension. FASEB J. 19, 1175–1177 (2005).
Arrigoni, F.I., Vallance, P., Haworth, S.G. & Leiper, J.M. Metabolism of asymmetric dimethylarginines is regulated in the lung developmentally and with pulmonary hypertension induced by hypobaric hypoxia. Circulation 107, 1195–1201 (2003).
Millatt, L.J. et al. Evidence for dysregulation of dimethylarginine dimethylaminohydrolase I in chronic hypxia-induced pulmonary hypertension. Circulation 108, 1493–1498 (2003).
Smith, C.L., Anthony, S., Hubank, M., Leiper, J.M. & Vallance, P. Effects of ADMA upon gene expression: an insight into the pathophysiological significance of raised plasma ADMA. PLoS Med. 2, e264 (2005).
Lane, K.B. et al. Heterozygous germline mutations in BMPR2, encoding a TGF beta receptor, cause familial primary pulmonary hypertension. Nat. Genet. 26, 81–84 (2000).
Tran, C.T., Fox, M.F., Vallance, P. & Leiper, J.M. Chromosomal localization, gene structure, and expression of DDAH-1: comparison with DDAH-2 and implications for evolutionary origins. Genomics 68, 101–105 (2000).
Collaborative Computational Project, Number 4. The CCP4 suite: programs for protein crystallography. Acta Crystallogr. D Biol. Crystallogr. 50, 760–763 (1994).
Emsley, P. & Cowtan, K. Coot: model-building tools for molecular graphics. Acta Crystallogr. D Biol. Crystallogr. 60, 2126–2132 (2004).
Teerlink, T., Nijveldt, R.J., de Jong, S. & Leeuwen, P.A. Determination of arginine, asymmetric dimethylarginine and symmetric dimethylarginine in human plasma and other biological samples by high-performance liquid chromatography. Anal. Biochem. 303, 131–137 (2002).
Hollenberg, S.M. et al. Characterization of a hyperdynamic murine model of resuscitated sepsis using echocardiography. Am. J. Respir. Crit. Care Med. 164, 891–895 (2001).
Nandi, M. et al. Pulmonary hypertension in a GTP-cyclohydrolase 1-deficient mouse. Circulation 111, 2086–2090 (2005).
Acknowledgements
We thank the following for experimental assistance: L. Newman, S. Jey, S. Thakker, H. Gill, V. Taylor and A. Cole. This work was funded by grants from the British Heart Foundation (PG20007 and PG/02/165/14797), the Wellcome Trust (065612/Z/01) and Medical Research Council (G0000002). P.V., J.L. and M.N. are part of the European Vascular Genomics Network funded by the European Union (contract number LSHM-CT-2003-503254). This study received financial support from the European Commission under the 6th Framework Programme (contract number LSHM-CT-2005-018725, PULMOTENSION). N.Q.M. and J.M.-R. are funded by Cancer Research UK.
Author information
Authors and Affiliations
Contributions
J.L. generated the Ddah1 gene–deleted mice, oversaw all molecular and cellular studies and was involved in every aspect of the work reported in this paper. M.N. undertook experiments and oversaw all aspects of functional phenotyping and pharmacological experiments. M.N., R.S. and A.R. contributed to the in vivo cardiovascular experiments. M. Malaki., B.T., M.M. and S.A. contributed to the ex vivo cardiovascular experiments. C.S. helped characterize the molecular phenotype of the mice. B.W.-S. undertook experiments on pulmonary endothelial cells. S.R. designed and synthesied the DDAH inhibitors with D.S. B.O'H. expressed, purified and crystallised DDAH-1 and collected the X-ray data. J.M.-R. solved, built and refined all structures. N.Q.M. supervised the structural biology aspects of the project. P.V. was involved in formulating the hypothesis, and in the design, analysis and interpretation of all experiments. P.V., J.L., M.N., J.M.-R. and N.Q.M. wrote the final manuscript.
Corresponding author
Ethics declarations
Competing interests
UCL holds patents on DDAH and the chemical structures identified in this manuscript. The funding agencies (BHF and Wellcome Trust) and UCL and Birkbeck College stand to gain financially from these patents. Since this work was completed, P.V. left UCL and is now a full-time employee of GSK and holds shares in GSK. GSK has had no input into the work and has no financial interest in the work described in this paper.
Supplementary information
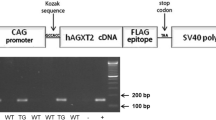
Supplementary Fig. 1
Construct development for DDAH-1 knockout mice and biochemical characterisation of DDAH1+/− mice. (PDF 170 kb)
Supplementary Fig. 2
Effect of DDAH inhibitors on NOS activity in vitro (PDF 22 kb)
Supplementary Fig. 3
Effect of L-291 on endothelium denuded rat aorta (PDF 10 kb)
Supplementary Fig. 4
Effects of i.v. administration of L-291 on mouse plasma levels. (PDF 11 kb)
Supplementary Fig. 5
Dimethylarginine levels and nitrite release from cultured primary pulmonary endothelial cells from mice. (PDF 14 kb)
Supplementary Fig. 6
Functional reactivity to calcium ionophore in isolated vessels from DDAH1+/− mice or mice treated with L-291 (PDF 25 kb)
Supplementary Fig. 7
Ex vivo analysis of pulmonary vasculature from DDAH1 +/− mice (PDF 313 kb)
Supplementary Fig. 8
Schematic summarising the main findings of study. (PDF 380 kb)
Supplementary Table 1
Crystallographic data collection and refinement (PDF 21 kb)
Supplementary Table 2
EC50 values from functional studies on isolated mouse aortic rings. (PDF 13 kb)
Rights and permissions
About this article
Cite this article
Leiper, J., Nandi, M., Torondel, B. et al. Disruption of methylarginine metabolism impairs vascular homeostasis. Nat Med 13, 198–203 (2007). https://doi.org/10.1038/nm1543
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm1543
This article is cited by
-
Knock-out of the critical nitric oxide synthase regulator DDAH1 in mice impacts amphetamine sensitivity and dopamine metabolism
Journal of Neural Transmission (2023)
-
A new perspective on NO pathway in sepsis and ADMA lowering as a potential therapeutic approach
Critical Care (2022)
-
An organ-on-chip model of pulmonary arterial hypertension identifies a BMPR2-SOX17-prostacyclin signalling axis
Communications Biology (2022)
-
Mechanical force promotes dimethylarginine dimethylaminohydrolase 1-mediated hydrolysis of the metabolite asymmetric dimethylarginine to enhance bone formation
Nature Communications (2022)
-
Love is in the hair: arginine methylation of human hair proteins as novel cardiovascular biomarkers
Amino Acids (2022)