Abstract
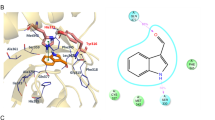
Astrocytes have important roles in the central nervous system (CNS) during health and disease. Through genome-wide analyses we detected a transcriptional response to type I interferons (IFN-Is) in astrocytes during experimental CNS autoimmunity and also in CNS lesions from patients with multiple sclerosis (MS). IFN-I signaling in astrocytes reduces inflammation and experimental autoimmune encephalomyelitis (EAE) disease scores via the ligand-activated transcription factor aryl hydrocarbon receptor (AHR) and the suppressor of cytokine signaling 2 (SOCS2). The anti-inflammatory effects of nasally administered interferon (IFN)-β are partly mediated by AHR. Dietary tryptophan is metabolized by the gut microbiota into AHR agonists that have an effect on astrocytes to limit CNS inflammation. EAE scores were increased following ampicillin treatment during the recovery phase, and CNS inflammation was reduced in antibiotic-treated mice by supplementation with the tryptophan metabolites indole, indoxyl-3-sulfate, indole-3-propionic acid and indole-3-aldehyde, or the bacterial enzyme tryptophanase. In individuals with MS, the circulating levels of AHR agonists were decreased. These findings suggest that IFN-Is produced in the CNS function in combination with metabolites derived from dietary tryptophan by the gut flora to activate AHR signaling in astrocytes and suppress CNS inflammation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Allen, N.J. et al. Astrocyte glypicans 4 and 6 promote formation of excitatory synapses via GluA1 AMPA receptors. Nature 486, 410–414 (2012).
Alvarez, J.I. et al. The Hedgehog pathway promotes blood–brain barrier integrity and CNS immune quiescence. Science 334, 1727–1731 (2011).
Chung, W.S. et al. Astrocytes mediate synapse elimination through MEGF10 and MERTK pathways. Nature 504, 394–400 (2013).
Khakh, B.S. & Sofroniew, M.V. Diversity of astrocyte functions and phenotypes in neural circuits. Nat. Neurosci. 18, 942–952 (2015).
Molofsky, A.V. et al. Astrocyte-encoded positional cues maintain sensorimotor circuit integrity. Nature 509, 189–194 (2014).
Obermeier, B., Daneman, R. & Ransohoff, R.M. Development, maintenance and disruption of the blood–brain barrier. Nat. Med. 19, 1584–1596 (2013).
Rieckmann, P. & Engelhardt, B. Building up the blood–brain barrier. Nat. Med. 9, 828–829 (2003).
Sofroniew, M.V. Astrocyte barriers to neurotoxic inflammation. Nat. Rev. Neurosci. 16, 249–263 (2015).
Tsai, H.H. et al. Regional astrocyte allocation regulates CNS synaptogenesis and repair. Science 337, 358–362 (2012).
Lassmann, H. Mechanisms of white matter damage in multiple sclerosis. Glia 62, 1816–1830 (2014).
Mayo, L. et al. Regulation of astrocyte activation by glycolipids drives chronic CNS inflammation. Nat. Med. 20, 1147–1156 (2014).
Shao, W. et al. Suppression of neuroinflammation by astrocytic dopamine D2 receptors via αB-crystallin. Nature 494, 90–94 (2013).
Berer, K. et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479, 538–541 (2011).
Furusawa, Y. et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 504, 446–450 (2013).
Smith, P.M. et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341, 569–573 (2013).
Baruch, K. et al. Aging. Aging-induced type I interferon response at the choroid plexus negatively affects brain function. Science 346, 89–93 (2014).
Ivashkiv, L.B. & Donlin, L.T. Regulation of type I interferon responses. Nat. Rev. Immunol. 14, 36–49 (2014).
Sandler, N.G. et al. Type I interferon responses in rhesus macaques prevent SIV infection and slow disease progression. Nature 511, 601–605 (2014).
Yan, Y. et al. CNS-specific therapy for ongoing EAE by silencing IL-17 pathway in astrocytes. Mol. Ther. 20, 1338–1348 (2012).
Quintana, F.J. & Sherr, D.H. Aryl hydrocarbon receptor control of adaptive immunity. Pharmacol. Rev. 65, 1148–1161 (2013).
Stockinger, B., Di Meglio, P., Gialitakis, M. & Duarte, J.H. The aryl hydrocarbon receptor: multitasking in the immune system. Annu. Rev. Immunol. 32, 403–432 (2014).
Prinz, M. et al. Distinct and nonredundant in vivo functions of IFNAR on myeloid cells limit autoimmunity in the central nervous system. Immunity 28, 675–686 (2008).
Fitzgerald, D.C. et al. Suppressive effect of IL-27 on encephalitogenic TH17 cells and the effector phase of experimental autoimmune encephalomyelitis. J. Immunol. 179, 3268–3275 (2007).
Mitsdoerffer, M. & Kuchroo, V. New pieces in the puzzle: how does interferon-β really work in multiple sclerosis? Ann. Neurol. 65, 487–488 (2009).
Mascanfroni, I.D. et al. Metabolic control of type 1 regulatory T cell differentiation by AHR and HIF1-α. Nat. Med. 21, 638–646 (2015).
Mascanfroni, I.D. et al. IL-27 acts on DCs to suppress the T cell response and autoimmunity by inducing expression of the immunoregulatory molecule CD39. Nat. Immunol. 14, 1054–1063 (2013).
Apetoh, L. et al. The aryl hydrocarbon receptor interacts with c-Maf to promote the differentiation of type 1 regulatory T cells induced by IL-27. Nat. Immunol. 11, 854–861 (2010).
Yeste, A., Nadeau, M., Burns, E.J., Weiner, H.L. & Quintana, F.J. Nanoparticle-mediated co-delivery of myelin antigen and a tolerogenic small molecule suppresses experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA 109, 11270–11275 (2012).
Weidemann, A. et al. The glial cell response is an essential component of hypoxia-induced erythropoiesis in mice. J. Clin. Invest. 119, 3373–3383 (2009).
Jessen, K.R. & Mirsky, R. Glial cells in the enteric nervous system contain glial fibrillary acidic protein. Nature 286, 736–737 (1980).
Kim, R.Y. et al. Astrocyte CCL2 sustains immune cell infiltration in chronic experimental autoimmune encephalomyelitis. J. Neuroimmunol. 274, 53–61 (2014).
Mc Guire, C., Prinz, M., Beyaert, R. & van Loo, G. Nuclear factor kappa B (NF-κB) in multiple sclerosis pathology. Trends Mol. Med. 19, 604–613 (2013).
van Loo, G. et al. Inhibition of transcription factor NF-κB in the central nervous system ameliorates autoimmune encephalomyelitis in mice. Nat. Immunol. 7, 954–961 (2006).
Boverhof, D.R. et al. 2,3,7,8-tetrachlorodibenzo-p-dioxin induces suppressor of cytokine signaling 2 in murine B cells. Mol. Pharmacol. 66, 1662–1670 (2004).
Zadjali, F. et al. Socs2 deletion protects against hepatic steatosis but worsens insulin resistance in high-fat-diet-fed mice. FASEB J. 26, 3282–3291 (2012).
Axtell, R.C. et al. T helper type 1 and 17 cells determine efficacy of interferon-β in multiple sclerosis and experimental encephalomyelitis. Nat. Med. 16, 406–412 (2010).
Borden, E.C. et al. Interferons at age 50: past, current and future impact on biomedicine. Nat. Rev. Drug Discov. 6, 975–990 (2007).
Ross, T.M. et al. Intranasal administration of interferon-β bypasses the blood–brain barrier to target the central nervous system and cervical lymph nodes: a non-invasive treatment strategy for multiple sclerosis. J. Neuroimmunol. 151, 66–77 (2004).
Yona, S. et al. Fate mapping reveals origins and dynamics of monocytes and tissue macrophages under homeostasis. Immunity 38, 79–91 (2013).
Farez, M.F. et al. Melatonin contributes to the seasonality of multiple sclerosis relapses. Cell 162, 1338–1352 (2015).
Gandhi, R. et al. Activation of the aryl hydrocarbon receptor induces human type 1 regulatory T cell–like and Foxp3+ regulatory T cells. Nat. Immunol. 11, 846–853 (2010).
Li, Y. et al. Exogenous stimuli maintain intraepithelial lymphocytes via aryl hydrocarbon receptor activation. Cell 147, 629–640 (2011).
Wikoff, W.R. et al. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc. Natl. Acad. Sci. USA 106, 3698–3703 (2009).
Zelante, T. et al. Tryptophan catabolites from microbiota engage aryl hydrocarbon receptor and balance mucosal reactivity via interleukin-22. Immunity 39, 372–385 (2013).
Schroeder, J.C. et al. The uremic toxin 3-indoxyl sulfate is a potent endogenous agonist for the human aryl hydrocarbon receptor. Biochemistry 49, 393–400 (2010).
Palace, J., Leite, M.I., Nairne, A. & Vincent, A. Interferon-β treatment in neuromyelitis optica: increase in relapses and aquaporin 4 antibody titers. Arch. Neurol. 67, 1016–1017 (2010).
Khorooshi, R. et al. Induction of endogenous type I interferon within the central nervous system plays a protective role in experimental autoimmune encephalomyelitis. Acta Neuropathol. 130, 107–118 (2015).
Dann, A. et al. Cytosolic RIG-I-like helicases act as negative regulators of sterile inflammation in the CNS. Nat. Neurosci. 15, 98–106 (2012).
Ejlerskov, P. et al. Lack of neuronal IFN-β–IFNAR causes Lewy body– and Parkinson's disease–like dementia. Cell 163, 324–339 (2015).
Goldmann, T. et al. USP18 lack in microglia causes destructive interferonopathy of the mouse brain. EMBO J. 34, 1612–1629 (2015).
Quintana, F.J. et al. Control of Treg and TH17 cell differentiation by the aryl hydrocarbon receptor. Nature 453, 65–71 (2008).
Quintana, F.J. et al. An endogenous aryl hydrocarbon receptor ligand acts on dendritic cells and T cells to suppress experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA 107, 20768–20773 (2010).
Veldhoen, M. et al. The aryl hydrocarbon receptor links TH17 cell–mediated autoimmunity to environmental toxins. Nature 453, 106–109 (2008).
Bessede, A. et al. Aryl hydrocarbon receptor control of a disease tolerance defense pathway. Nature 511, 184–190 (2014).
Opitz, C.A. et al. An endogenous tumor-promoting ligand of the human aryl hydrocarbon receptor. Nature 478, 197–203 (2011).
Monteleone, I. et al. Aryl-hydrocarbon-receptor-induced signals upregulate IL-22 production and inhibit inflammation in the gastrointestinal tract. Gastroenterology 141, 237–248, 248.e1 (2011).
Atarashi, K. et al. TH17 cell induction by adhesion of microbes to intestinal epithelial cells. Cell 163, 367–380 (2015).
Lee, Y.K., Menezes, J.S., Umesaki, Y. & Mazmanian, S.K. Proinflammatory T cell responses to gut microbiota promote experimental autoimmune encephalomyelitis. Proc. Natl. Acad. Sci. USA 108, 4615–4622 (2011).
Ochoa-Repáraz, J. et al. Central nervous system demyelinating disease protection by the human commensal Bacteroides fragilis depends on polysaccharide A expression. J. Immunol. 185, 4101–4108 (2010).
Viaud, S. et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 342, 971–976 (2013).
Prinz, M., Priller, J., Sisodia, S.S. & Ransohoff, R.M. Heterogeneity of CNS myeloid cells and their roles in neurodegeneration. Nat. Neurosci. 14, 1227–1235 (2011).
Trapnell, C. et al. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat. Protoc. 7, 562–578 (2012).
Jack, C.S. et al. TLR signaling tailors innate immune responses in human microglia and astrocytes. J. Immunol. 175, 4320–4330 (2005).
Alvarez, J.I. et al. Focal disturbances in the blood–brain barrier are associated with formation of neuroinflammatory lesions. Neurobiol. Dis. 74, 14–24 (2015).
Townsend, M.K. et al. Reproducibility of metabolomic profiles among men and women in two large cohort studies. Clin. Chem. 59, 1657–1667 (2013).
Acknowledgements
This work was supported by the National Institutes of Health (NIH) grants AI075285 (F.J.Q.) and AI093903 (F.J.Q.), the National Multiple Sclerosis Society grant RG4111A1 (F.J.Q.), the International Progressive MS Alliance grants PA0069 (F.J.Q.) and PA-1501-02847 (F.J.Q.), an educational grant from Mallinckrodt Pharmaceuticals (A219074; V.R.), a fellowship from the German Research Foundation (DFG RO4866 1/1; V.R.), postdoctoral fellowships from the National Multiple Sclerosis Society (FG 2036-A1/1 (I.D.M) and FG1941A1/2 (L.M.)), a fellowship from the International Academy of Life Sciences (L.B.), a postdoctoral Research Abroad Program award from the Ministry of Science and Technology, Taiwan (104-2917-I-564 -024; C.-C.C.) and a fellowship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil (BEX 0571/15-6; M.C.T.). Cx3cr1-CreERT2 mice were a kind gift from S. Jung (Weizmann Institute of science). The pLenti-Gfap-eGFP-mir30-shAct1 vector was a gift from G.-X. Zhang.
Author information
Authors and Affiliations
Contributions
V.R., I.D.M., L.B., M.C.T., J.E.K., L.M., C.-C.C., H.K., J.I.A., M.B. and C.B.C. performed in vitro and in vivo experiments; B.P., R.Y., N.O. and N.P. performed bioinformatics analysis; N.A., G.I., C.B.C., A.P., S.J., M.P. and J.A. provided unique reagents, and discussed and/or interpreted findings; V.R. and F.J.Q. wrote the manuscript; and F.J.Q. designed and supervised the study and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7 and Supplementary Table 1–4 (PDF 6268 kb)
Rights and permissions
About this article
Cite this article
Rothhammer, V., Mascanfroni, I., Bunse, L. et al. Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor. Nat Med 22, 586–597 (2016). https://doi.org/10.1038/nm.4106
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4106
This article is cited by
-
The involvement of α-synucleinopathy in the disruption of microglial homeostasis contributes to the pathogenesis of Parkinson’s disease
Cell Communication and Signaling (2024)
-
Gut microbiota-host lipid crosstalk in Alzheimer’s disease: implications for disease progression and therapeutics
Molecular Neurodegeneration (2024)
-
Dietary fibre directs microbial tryptophan metabolism via metabolic interactions in the gut microbiota
Nature Microbiology (2024)
-
Myeloid cell-associated aromatic amino acid metabolism facilitates CNS myelin regeneration
npj Regenerative Medicine (2024)
-
Dubosiella newyorkensis modulates immune tolerance in colitis via the L-lysine-activated AhR-IDO1-Kyn pathway
Nature Communications (2024)