Abstract
Head and neck squamous cell carcinoma (HNSCC) is characterized by aggressive behavior with a propensity for metastasis and recurrence. Here we report a comprehensive analysis of the molecular and clinical features of HNSCC that govern patient survival. We find that TP53 mutation is frequently accompanied by loss of chromosome 3p and that the combination of these events is associated with a surprising decrease in survival time (1.9 years versus >5 years for TP53 mutation alone). The TP53-3p interaction is specific to chromosome 3p and validates in HNSCC and pan-cancer cohorts. In human papillomavirus (HPV)-positive tumors, in which HPV inactivates TP53, 3p deletion is also common and is associated with poor outcomes. The TP53-3p event is modified by mir-548k expression, which decreases survival further, and is mutually exclusive with mutations affecting RAS signaling. Together, the identified markers underscore the molecular heterogeneity of HNSCC and enable a new multi-tiered classification of this disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Leemans, C.R., Braakhuis, B.J.M. & Brakenhoff, R.H. The molecular biology of head and neck cancer. Nat. Rev. Cancer 11, 9–22 (2011).
Mroz, E.A. et al. High intratumor genetic heterogeneity is related to worse outcome in patients with head and neck squamous cell carcinoma: Genetic Heterogeneity and HNSCC Outcome. Cancer 119, 3034–3042 (2013).
Stransky, N. et al. The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160 (2011).
Chung, C.H. et al. Molecular classification of head and neck squamous cell carcinomas using patterns of gene expression. Cancer Cell 5, 489–500 (2004).
Walter, V. et al. Molecular subtypes in head and neck cancer exhibit distinct patterns of chromosomal gain and loss of canonical cancer genes. PLoS ONE 8, e56823 (2013).
Pickering, C.R. et al. Integrative genomic characterization of oral squamous cell carcinoma identifies frequent somatic drivers. Cancer Discov. 3, 770–781 (2013).
Temam, S. et al. Epidermal growth factor receptor copy number alterations correlate with poor clinical outcome in patients with head and neck squamous cancer. J. Clin. Oncol. 25, 2164–2170 (2007).
Lui, V.W.Y. et al. Frequent mutation of the PI3K pathway in head and neck cancer defines predictive biomarkers. Cancer Discov. 3, 761–769 (2013).
Perez, F. & Granger, B.E. IPython: a system for interactive scientific computing. Comput. Sci. Eng. 9, 21–29 (2007).
Poeta, M.L. et al. TP53 mutations and survival in squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 357, 2552–2561 (2007).
Ohta, M. et al. The FHIT gene, spanning the chromosome 3p14.2 fragile site and renal carcinoma–associated t(3;8) breakpoint, is abnormal in digestive tract cancers. Cell 84, 587–597 (1996).
Rosin, M.P. et al. Use of allelic loss to predict malignant risk for low-grade oral epithelial dysplasia. Clin. Cancer Res. 6, 357–362 (2000).
Partridge, M., Emilion, G. & Langdon, J.D. LOH at 3p correlates with a poor survival in oral squamous cell carcinoma. Br. J. Cancer 73, 366–371 (1996).
Meredith, S.D. et al. Chromosome 11q13 amplification in head and neck squamous cell carcinoma. Association with poor prognosis. Arch. Otolaryngol. Head Neck Surg. 121, 790–794 (1995).
Partridge, M. et al. The prognostic significance of allelic imbalance at key chromosomal loci in oral cancer. Br. J. Cancer 79, 1821–1827 (1999).
Ciriello, G., Cerami, E., Sander, C. & Schultz, N. Mutual exclusivity analysis identifies oncogenic network modules. Genome Res. 22, 398–406 (2012).
Bredel, M. et al. A network model of a cooperative genetic landscape in brain tumors. J. Am. Med. Assoc. 302, 261–275 (2009).
Thomas, M., Pim, D. & Banks, L. The role of the E6-p53 interaction in the molecular pathogenesis of HPV. Oncogene 18, 7690–7700 (1999).
Marur, S., D'Souza, G., Westra, W.H. & Forastiere, A.A. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol. 11, 781–789 (2010).
Cancer Genome Atlas Research Network. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 45, 1113–1120 (2013).
Song, Y. et al. Identification of genomic alterations in oesophageal squamous cell cancer. Nature 509, 91–95 (2014).
Lawrence, M.S. et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 505, 495–501 (2014).
Xing, F. et al. Concurrent loss of the PTEN and RB1 tumor suppressors attenuates RAF dependence in melanomas harboring V600EBRAF. Oncogene 31, 446–457 (2012).
Cibulskis, K. et al. Sensitive detection of somatic point mutations in impure and heterogeneous cancer samples. Nat. Biotechnol. 31, 213–219 (2013).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Liberzon, A. et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics 27, 1739–1740 (2011).
Mermel, C.H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, R41 (2011).
Mell, L.K. et al. Predictors of competing mortality in advanced head and neck cancer. J. Clin. Oncol. 28, 15–20 (2010).
Farshadpour, F. et al. Survival analysis of head and neck squamous cell carcinoma: influence of smoking and drinking. Head Neck 33, 817–823 (2011).
Cox, D.R. Analysis of Survival Data (Chapman and Hall, London, New York, 1984).
Benjamini, Y. & Hochberg, Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. B 57, 289–300 (1995).
Acknowledgements
The results published here are based upon data generated by the TCGA Research Network. We thank K. Messer and A. Tward for helpful discussions. We gratefully acknowledge support for this study from the US National Institutes of Health (P50 GM085764, U24 CA184427 and P41 GM103504 to T.I.; T32 DC000028 to R.K.O.; Burroughs Welcome Fund CAMS to Q.T.N.; P50 CA097190 and The American Cancer Society to J.R.G.; K07 CA137140 to A.M.E.; DP5 OD017937-01 to H.C.). J.P.S. is supported in part by grants from the Marsha Rivkin Center for Ovarian Cancer Research and a Conquer Cancer Foundation of the American Society of Clinical Oncology Young Investigator Award.
Author information
Authors and Affiliations
Contributions
A.M.G., R.K.O., Q.T.N. and T.I. conceived the study. A.M.G. carried out most analyses. R.K.O., J.P.S., M.C., C.S.C., E.E.C., S.M.L., Q.T.N. and D.N.H. provided expertise. M.H. and H.C. aided in bioinformatics analysis. A.M.E. and J.R.G. collected and compiled clinical follow-up data for the UPMC cohort. A.M.G. and T.I. wrote the manuscript with assistance from other authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Integration and selection of cancer events in HNSCC.
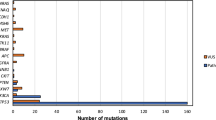
(a) Tumor data first pass an integration step in which knowledge of pathway or chromosomal structure is used to create meta features. Data are then filtered on the basis of event frequency across tumor samples or comparison with matched normal samples, yielding a pool of candidate cancer-associated events. (b) Example of the integration step in which sparse mutations to the SOS1/RAS pathway (Reactome 524) are combined to derive (c) a single pathway mutation marker for each patient. In b, green bars indicate that a patient (column) has a mutation in a particular pathway gene (row). (d) Example integration of mRNA expression on a pathway, in which principal-component analysis (PCA) is applied to the gene-by-patient expression matrix. Shown are the gene loadings for PCA of the PIP3 signaling pathway (mSigDB M1315). (e) In each patient, the first principal component is used to represent the consensus expression value of the pathway. Here the blue bars represent patients for whom this value is above the threshold and for whom the pathway is scored as ‘upregulated’.
Supplementary Figure 2 Characterization of patient age and HPV status in the TCGA HNSCC cohort.
(a) Distribution of patient ages across the 378 patients in the cohort. (b) Kaplan-Meier survival curves for the different age cutoffs used in this study. (c) Distribution of HPV-positive and HPV-negative tumors across different tumor subdivisions. (d) Kaplan-Meier survival curves comparing HPV-positive and HPV-negative patients.
Supplementary Figure 3 Exploration of the 3p chromosomal arm.
Number of patients with heterozygous loss (top) and association with patient survival (bottom) for genes along the 3p chromosomal arm in TCGA discovery cohort patients with HPV-negative (a) and HPV-positive (b) tumors.
Supplementary Figure 4 Exploration of TP53 mutation in the context of chromosomal instability.
Violin plots showing the effect of TP53 mutation on deletion (a) and amplification (b) rates. P values indicate significance from a Kruskal-Wallis test.
Supplementary Figure 5 Exploration of TP53-3p interaction with respect to patient survival.
(a) Number of patients surviving or deceased for various time intervals. (b) Statistical models fit using logistic regression. CIN indicates chromosomal instability, measured by the fraction of deleted genes per tumor genome. (c,d) Performance of each logistic regression model in leave-one-out cross-validation to assess the ability of different combinations of genomic variables to predict patient outcomes. For a description of regression formulation, see the Online Methods. For multivariate Cox analysis of the best model, m5, using the full censored data set, see Supplementary Table 7.
Supplementary Figure 6 Subtypes in the context of clinical stage and grade.
(a) Frequency and (b) prognostic effect of the TP53-3p aggregate event across different stage groups. (c) Frequency and (d) prognostic effect of the TP53-3p aggregate event across different grade groups. P values indicate significance from a Kruskal-Wallis test assessing association of the TP53-3p event with increasing stage or grade.
Supplementary Figure 7 Analysis of clinical covariates with molecular subtypes.
(a) Hazard ratios (x axis) for each component (y axis) of a multivariate Cox model of patient survival, including the TP53-3p event and clinical variables. All hazard ratios are relative to the absence of the clinical or molecular event. Stepwise feature selection was performed to reduce the model to informative clinical variables only. See Supplementary Table 1 for more information on clinical variables. (b–d) Re-creation of the main prognostic associations from this study in a clinically homogenous cohort of 175 patients with a history of smoking who were under 75 years of age.
Supplementary Figure 8 Pan-cancer analysis.
(a) Kaplan-Meier survival plots, (b) median survival and (c) 5-year survival for TCGA cancers (error bars indicate 95% CI). Cancer acronyms are defined as follows: BRCA, breast invasive carcinoma; UCEC, uterine corpus endometrioid carcinoma; KIRP, Kidney renal papillary cell carcinoma; CESC, cervical squamous cell carcinoma and endocervical adenocarcinoma; LGG, brain lower grade glioma; COAD, colon adenocarcinoma; KIRC, Kidney renal clear cell carcinoma; SKCM, skin cutaneous melanoma; SARC, sarcoma; READ, rectum adenocarcinoma; LUSC, lung squamous cell carcinoma; HNSC, head and neck squamous cell carcinoma; BLCA, bladder urothelial carcinoma; LIHC, liver hepatocellular carcinoma; LUAD, lung adenocarcinoma; STAD, stomach adenocarcinoma; OV, ovarian serous cystadenocarcinoma; LAML, acute myeloid leukemia.
Supplementary Figure 9 Characterization of miR-548k in patients with the TP53-3p event.
(a) miR-548k expression levels in tumor and normal tissues. (b) Comparison of miR-548k copy number with expression. (c) Kaplan-Meier survival curves of different combinations of high and low mR-548k expression and amplification of its chromosomal segment.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–9 (PDF 33073 kb)
Supplementary tables 1-8
Supplementary Tables 1–8 (XLSX 602 kb)
Rights and permissions
About this article
Cite this article
Gross, A., Orosco, R., Shen, J. et al. Multi-tiered genomic analysis of head and neck cancer ties TP53 mutation to 3p loss. Nat Genet 46, 939–943 (2014). https://doi.org/10.1038/ng.3051
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3051
This article is cited by
-
Gene alterations as predictors of radiation-induced toxicity in head and neck squamous cell carcinoma
Journal of Translational Medicine (2021)
-
In-gel digestion coupled with mass spectrometry (GeLC-MS/MS)-based salivary proteomic profiling of canine oral tumors
BMC Veterinary Research (2020)
-
Genomic and human papillomavirus profiling of an oral cancer cohort identifies TP53 as a predictor of overall survival
Cancers of the Head & Neck (2019)
-
Identification of genomic copy number variations associated with specific clinical features of head and neck cancer
Molecular Cytogenetics (2018)
-
RETRACTED ARTICLE: Periostin secreted by cancer-associated fibroblasts promotes cancer stemness in head and neck cancer by activating protein tyrosine kinase 7
Cell Death & Disease (2018)