Abstract
The contribution of lncRNAs to tumour progression and the regulatory mechanisms driving their expression are areas of intense investigation. Here, we characterize the binding of heterogeneous nuclear ribonucleoprotein E1 (hnRNP E1) to a nucleic acid structural element located in exon 12 of PNUTS (also known as PPP1R10) pre-RNA that regulates its alternative splicing. HnRNP E1 release from this structural element, following its silencing, nucleocytoplasmic translocation or in response to TGFβ, allows alternative splicing and generates a non-coding isoform of PNUTS. Functionally the lncRNA-PNUTS serves as a competitive sponge for miR-205 during epithelial–mesenchymal transition (EMT). In mesenchymal breast tumour cells and in breast tumour samples, the expression of lncRNA-PNUTS is elevated and correlates with levels of ZEB mRNAs. Thus, PNUTS is a bifunctional RNA encoding both PNUTS mRNA and lncRNA-PNUTS, each eliciting distinct biological functions. While PNUTS mRNA is ubiquitously expressed, lncRNA-PNUTS appears to be tightly regulated dependent on the status of hnRNP E1 and tumour context.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Accession codes
Change history
13 November 2017
In this Addendum, the authors include western blot data using a C-terminal PNUTS antibody. This is important in that an annotation of the alternative spliced form of PNUTS, denoted in the UCSC genome browser (https://genome.ucsc.edu/), depicts it as a non-coding RNA. However, downstream of the alternative splice site is an alternative AUG located in frame in the PNUTS ORF at position 1039. The potential for a protein product of ∼61 kDa being generated from this AUG was examined experimentally using a C-terminal raised antibody to PNUTS to exclude the possibility that the N-terminal deletion of the splice isoform was not the reason that the predicted 61-kDa protein was not detected in cells using an N-terminal generated antibody. The results presented here confirm our previous results using the N-terminal PNUTS antibody and originally presented in Supplementary Fig. 2b of the Article; namely, that this predicted ∼61-kDa product is not detectable in cells under the conditions used, even under conditions of overexpression. Figure (see PDF): lncRNA-PNUTS does not encode for a N-terminal truncated-protein product. The result of a western blot analysis of PNUTS protein expression in CaCo-2 cells upon transient lncRNA-PNUTS expression (3 days) or TGFβ treatment (1 day) is shown. The C-terminal antibody used was EPR11706 (Abcam: Ab173285; clone PPP1R10; 1/1000 dilution) raised against the C-terminal region of the PNUTS protein (amino acids 550–650). The western blot protocol and extracts used in this experiment were identical to those described in Supplementary Fig. 2 of the original Article.
References
Jemal, A. et al. Global cancer statistics. CA. Cancer J. Clin. 61, 69–90 (2011).
Chaffer, C. L. & Weinberg, R. A. A perspective on cancer cell metastasis. Science 331, 1559–1564 (2011).
Gupta, G. P. & Massagué, J. Cancer metastasis: building a framework. Cell 127, 679–695 (2006).
Weigelt, B., Peterse, J. L. & van’t Veer, L. J. Breast cancer metastasis: markers and models. Nat. Rev. Cancer 5, 591–602 (2005).
Dhamija, S. & Diederichs, S. From junk to master regulators of invasion: lncRNA functions in migration, EMT and metastasis. Int. J. Cancer 139, 269–280 (2016).
Malone, C. D. & Hannon, G. J. Small RNAs as guardians of the genome. Cell 136, 656–668 (2009).
Batista, P. J. & Chang, H. Y. Long noncoding RNAs: cellular address codes in development and disease. Cell 152, 1298–1307 (2013).
Yuan, J. et al. A long noncoding RNA activated by TGF-β promotes the invasion-metastasis cascade in hepatocellular carcinoma. Cancer Cell 25, 666–681 (2014).
Leone, S. & Santoro, R. Challenges in the analysis of long noncoding RNA functionality. FEBS Lett. 590, 2342–2353 (2016).
Thomson, D. W. & Dinger, M. E. Endogenous microRNA sponges: evidence and controversy. Nat. Rev. Genet. 17, 272–283 (2016).
Smith, B. N. & Bhowmick, N. A. Role of EMT in metastasis and therapy resistance. J. Clin. Med. 5, 17 (2016).
Ye, X. & Weinberg, R. A. Epithelial–mesenchymal plasticity: a central regulator of cancer progression. Trends Cell Biol. 25, 675–686 (2015).
Chaudhury, A. et al. TGF-β-mediated phosphorylation of hnRNP E1 induces EMT via transcript-selective translational induction of Dab2 and ILEI. Nat. Cell Biol. 12, 286–293 (2010).
Grelet, S. et al. The human NANOS3 gene contributes to lung tumour invasion by inducing epithelial—mesenchymal transition. J. Pathol. 237, 25–37 (2015).
Hussey, G. S. et al. Identification of an mRNP complex regulating tumorigenesis at the translational elongation step. Mol. Cell 41, 419–431 (2011).
Chaudhury, A., Chander, P. & Howe, P. H. Heterogeneous nuclear ribonucleoproteins (hnRNPs) in cellular processes: focus on hnRNP E1’s multifunctional regulatory roles. RNA 16, 1449–1462 (2010).
Wang, E. T. et al. Alternative isoform regulation in human tissue transcriptomes. Nature 456, 470–476 (2008).
Zhang, T. et al. PCBP-1 regulates alternative splicing of the CD44 gene and inhibits invasion in human hepatoma cell line HepG2 cells. Mol. Cancer 9, 72 (2010).
Akker, S. A. et al. Pre-spliceosomal binding of U1 small nuclear ribonucleoprotein (RNP) and heterogenous nuclear RNP E1 is associated with suppression of a growth hormone receptor pseudoexon. Mol. Endocrinol. 21, 2529–2540 (2007).
Minn, A. J. et al. Genes that mediate breast cancer metastasis to lung. Nature 436, 518–524 (2005).
Desmet, F.-O. et al. Human splicing finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 37, e67 (2009).
Brown, A. S., Mohanty, B. K. & Howe, P. H. Identification and characterization of an hnRNP E1 translational silencing motif. Nucleic Acids Res. 44, 5892–5907 (2016).
Tennyson, C. N., Klamut, H. J. & Worton, R. G. The human dystrophin gene requires 16 hours to be transcribed and is cotranscriptionally spliced. Nat. Genet. 9, 184–190 (1995).
Gregory, P. A. et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat. Cell Biol. 10, 593–601 (2008).
Chao, C.-H. et al. MicroRNA-205 signaling regulates mammary stem cell fate and tumorigenesis. J. Clin. Invest. 124, 3093–3106 (2014).
Mani, S. A. et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133, 704–715 (2008).
Al-Hajj, M., Wicha, M. S., Benito-Hernandez, A., Morrison, S. J. & Clarke, M. F. Prospective identification of tumorigenic breast cancer cells. Proc. Natl Acad. Sci. USA 100, 3983–3988 (2003).
Yang, L. Splicing noncoding RNAs from the inside out. Wiley Interdiscip. Rev. RNA 6, 651–660 (2015).
Ulveling, D., Francastel, C. & Hubé, F. Identification of potentially new bifunctional RNA based on genome-wide data-mining of alternative splicing events. Biochimie 93, 2024–2027 (2011).
Brabletz, S. & Brabletz, T. The ZEB/miR-200 feedback loop—a motor of cellular plasticity in development and cancer? EMBO Rep. 11, 670–677 (2010).
Li, Y. et al. Metastatic heterogeneity of breast cancer cells is associated with expression of a heterogeneous TGFβ-activating miR424-503 gene cluster. Cancer Res. 74, 6107–6118 (2014).
Oshimori, N., Oristian, D. & Fuchs, E. TGF-β promotes heterogeneity and drug resistance in squamous cell carcinoma. Cell 160, 963–976 (2015).
Kornblihtt, A. R. et al. Alternative splicing: a pivotal step between eukaryotic transcription and translation. Nat. Rev. Mol. Cell Biol. 14, 153–165 (2013).
Geisler, S. & Coller, J. RNA in unexpected places: long non-coding RNA functions in diverse cellular contexts. Nat. Rev. Mol. Cell Biol. 14, 699–712 (2013).
West, J. A. et al. The long noncoding RNAs NEAT1 and MALAT1 bind active chromatin sites. Mol. Cell 55, 791–802 (2014).
Xing, Z. et al. lncRNA directs cooperative epigenetic regulation downstream of chemokine signals. Cell 159, 1110–1125 (2014).
Carter, M. S. et al. A regulatory mechanism that detects premature nonsense codons in T-cell receptor transcripts in vivo is reversed by protein synthesis inhibitors in vitro. J. Biol. Chem. 270, 28995–29003 (1995).
Laury-Kleintop, L. D., Tresini, M. & Hammond, O. Compartmentalization of hnRNP-K during cell cycle progression and its interaction with calponin in the cytoplasm. J. Cell. Biochem. 95, 1042–1056 (2005).
Fischer, K. R. et al. Epithelial-to-mesenchymal transition is not required for lung metastasis but contributes to chemoresistance. Nature 527, 472–476 (2015).
Hu, Y. et al. miRNA-205 targets VEGFA and FGF2 and regulates resistance to chemotherapeutics in breast cancer. Cell Death Dis. 7, e2291 (2016).
Li, J., Liu, H., Yu, J. & Yu, H. Chemoresistance to doxorubicin induces epithelial-mesenchymal transition via upregulation of transforming growth factor β signaling in HCT116 colon cancer cells. Mol. Med. Rep. 12, 192–198 (2015).
Li, Q.-Q. et al. Twist1-mediated adriamycin-induced epithelial-mesenchymal transition relates to multidrug resistance and invasive potential in breast cancer cells. Clin. Cancer Res. 15, 2657–2665 (2009).
Gu, S., Jin, L., Zhang, F., Sarnow, P. & Kay, M. A. Biological basis for restriction of microRNA targets to the 3′ untranslated region in mammalian mRNAs. Nat. Struct. Mol. Biol. 16, 144–150 (2009).
Vanharanta, S. & Massagué, J. Origins of metastatic traits. Cancer Cell 24, 410–421 (2013).
Wan, L., Pantel, K. & Kang, Y. Tumor metastasis: moving new biological insights into the clinic. Nat. Med. 19, 1450–1464 (2013).
Hu, Y. & Smyth, G. K. ELDA: extreme limiting dilution analysis for comparing depleted and enriched populations in stem cell and other assays. J. Immunol. Methods 347, 70–78 (2009).
Acknowledgements
The authors are grateful to M. Gooz for help with the microscopic analysis. We also thank Y. Shao for histopathological analysis and K. Gibbs (Charleston, South Carolina USA—Biorepository & Tissue Analysis Shared Resource at Medical University of South Carolina) for providing the human tumour samples. We thank M. Bidyut for his assistance with the cloning and K. Noguchi for his help with hnRNP E1 plasmid constructs and J. Isaacs for her precious help concerning hypoxia experiments. This work was supported in part by the Cell & Molecular Imaging, Small Animal Imaging, and the Biorepository & Tissue Analysis Shared Resources, Hollings Cancer Center, Medical University of South Carolina (P30 CA138313), and the Shared Instrumentation Grant S10 OD018113. This work was also supported by grants CA555536 and CA154664 from the National Cancer Institute to P.H.H.
Author information
Authors and Affiliations
Contributions
The study was supervised by P.H.H. The conception and design were made by S.G. and P.H.H. The methodology was developed by S.G. and P.H.H. Acquisition and interpretation of the data was carried out by S.G. and P.H.H. The Affymetrix experiment and care of the mice was provided by B.H. Mice injections and dissection were performed by S.G., L.A.L. and C.O. The manuscript was written by S.G. and P.H.H. and all the authors contributed to its reviewing. V.P., V.K.G. and J.A.D. provided critical discussion.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Characterization of the EMT induced by hnRNP E1 knockdown and validation of the splicing model in mouse.
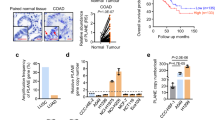
(a) EMT induction following shRNA-mediated silencing of hnRNP E1 in NMuMG cells. Imaging of cells reveals a significant morphological change in cellular phenotype from an epithelial-like to a mesenchymal-like phenotype. EMT was validated by immunoblotting analysis using antibodies to the mesenchymal marker vimentin and the epithelial markers ZO2 and E-cadherin. Scale bar, 100 μM. (b) Quantitative RT–PCR analysis of mRNA-PNUTS, ZEB-1 and ZEB-2 expression in 24 human breast tumor samples. Relative expression levels of transcripts were calculated using the ΔCt method normalizing to GAPDH. Correlations between transcript expression levels were then evaluated using Pearson correlation coefficient test. (Linear regression, df = 24–2, a Pearson score >0.515 and P < 0.05 was considered as significant). Source data are available in Supplementary Table 2. (c) Sanger sequencing result of the lower band obtained by end-point RT–PCR in Fig. 1h. (d) Identification of an alternative splice product corresponding to the lncRNA-PNUTS in NMuMG cells. Sequence alignment of human and murine genomes indicates that exon-11 of the murine genome matches with exon 12 of the human genome. RT–PCR amplification of exon10-exon11 junction demonstrates a potential alternative splice product. The lower band was cloned and then sequenced using Sanger technology. (e) Sequencing results indicate a splicing pseudosite located 86 nucleotides downstream of the regular splicing site (Top). Schematic representation of the alternative splice region of the PNUTS variants based on Sanger sequencing results (Bottom). (f) Secondary structure of the BAT-like element located in the alternative splicing site of murine PNUTS RNA as predicted using the Mfold algorithm (ΔG = −2.10 kcal mol−1). (g) Extended time course experiment using RT–PCR analysis of PNUTS gene processing following addition of TGFβ in A549. GAPDH was used as a loading control.
Supplementary Figure 2 The predicted lncRNA-PNUTS does not encode protein, is both nuclear and cytoplasmic and colocalizes with miRNA-205.
(a) In silico prediction of PNUTS alternative splicing sites. Lower case: intronic sequences; Upper case: exonic sequences; Bold characters: natural acceptor splice site; Bold italicized characters: newly identified pseudosite. (b) Western-blot (top) analysis of PNUTS protein expression upon PNUTS predicted-lncRNA transient overexpression (3 days) or TGFβ treatment (1 day) in A549, MCF7 and CaCO2 cell lines. RT–PCR analysis (bottom) was used to monitor the PNUTS predicted-lncRNA overexpression. ∗indicates the PNUTS protein band. The fact that the lncRNA does not appear upregulated in this experiment is due to the time point assayed (24 h TGFβ treatment) (see Supplementary Fig. 1g). (c) Fluorescence in situ hybridization analysis (FISH) of the endogenous form of lncRNA-PNUTS, mRNA-PNUTS and miR-205 was performed using selective probes labeled with ATTO dyes. Images at 300× magnifications, obtained by using confocal microscopy. Scale bar, 10 μM.
Supplementary Figure 3 The lncRNA-PNUTS silencing or splicing inhibition prevents both TGF-ß and E1KD-mediated EMT.
(a) The alternative splicing oligo (ASO) designed to block alternative splicing of PNUTS was used to inhibits TGFß-induced EMT in A549 cells (24 h TGFß treatment). The mesenchymal marker Vimentin was used to monitor the EMT induced by TGFß. (b) siRNA selectively targeting the lncRNA-PNUTS isoform was used to prevent TGFß-induced EMT in A549 cells or EMT occurring following transient hnRNP E1 knockdown in HMLE cells in c. Vimentin (mesenchymal marker) and E-cadherin (epithelial marker) were used to monitor the EMT induced by TGFß in A549 cells or by E1KD in HMLE cells. (d) Changes in cells morphologies were assessed by bright-field microscopy and quantified by determining the cell circularity index of the cells with a decrease in cell circularity reflecting the acquisition of a more mesenchymal phenotype. Cellular circularity was measured using ImageJ software according to the following formula: ‘circularity = 4π (area/perimeter2)’. Data are from a single experiment, where 35, 35, 35 and 61 cells were scored per condition. Scale bar, 50 μM. Source data are available in Supplementary Table 2. (e) The impact of the ASO on TGF-ß induced EMT was monitored on A549 cells migration. We observed that ASO transfection significantly impaired the TGF-ß induced 2D migration of the cells. (mean ± s.d., n = 5 fields quantified, pooled from 2 independent experiments, two-tailed Student t test, ∗∗P < 0.01; ∗∗∗P < 0.001, NS, not significant). Scale bar, 200 μM. Source data are available in Supplementary Table 2. Unprocessed original scans of blots are shown in Supplementary Fig. 7.
Supplementary Figure 4 The lncRNA-PNUTS regulates ZEB-1 3’UTR through its control of miRNA-205.
A Renilla reporter containing 3′-UTR of ZEB2 cloned downstream of Renilla was transfected into A549 and NMuMG cells overexpressing wild-type (lncRNA) or mutated (lncRNAS1-6M) constructs of lncRNA-PNUTS and treated ± synthetic miR-205 mimic. For each condition, Renilla luciferase activity was normalized to Firefly luciferase reporter. Data shown are from two experiments with a bar representing the mean.
Supplementary Figure 5 Impact and regulation of the lncRNA on stem cell properties.
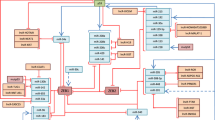
(a) (Top) Cell morphology of control and lncRNA overexpressing HMLE cells were assessed by phase-contrast microscopy and lncRNA-PNUTS overexpression was validated by RT–PCR. Scale bar, 50 μM. (Bottom) Histogram analysis related to FACS analysis presented in Fig. 6g. (b) Flow cytometry analysis of CD24 cell surface expression levels in MDA231-LM2 control (Scr-ShRNA) and shRNA-lncRNA-PNUTS. (c) Graphical abstract of the study. hnRNP E1 inhibits the alternative splicing of PNUTS by directly binding to the alternative splicing site. Loss of binding following hnRNP E1 knockdown, phosphorylation or its translocation to the cytoplasm allows for alternative splicing of PNUTS and thus generates lncRNA-PNUTS. This lncRNA competes for miR-205 and thus contributes to the EMT by allowing expression of mesenchymal markers such as Zeb1, normally targeted by this miRNA.
Supplementary Figure 6 Primers and probes design.
(a) Design of the splice-specific primers used either in end-point RT–PCR or quantitative RT–PCR. Primers were designed to overcome primer competition in order to analyze the specific expression of either mRNA-PNUTS or lncRNA-PNUTS isoforms. (b) Design of the primers used in competitive end-point RT–PCR to analyze the relative expression between mRNA-PNUTS, lncRNA-PNUTS and preRNA-PNUTS on the same PCR reaction. (c) Validation of the reliability of the primer sets presented in a and b by end-point RT–PCR (d) Design of the probes used for Northern-blot experiments to discriminate mRNA-PNUTS from lncRNA-PNUTS. (e) Design of siRNA or shRNA used to selectively target the lncRNA isoform of PNUTS. Probes were designed to target the new exon11/exon12 splice junction specific to the lncRNA-PNUTS.
Supplementary information
Supplementary Information
Supplementary Information (PDF 47326 kb)
Supplementary Table 1
Supplementary Information (XLSX 37 kb)
Supplementary Table 2
Supplementary Information (XLSX 44 kb)
Rights and permissions
About this article
Cite this article
Grelet, S., Link, L., Howley, B. et al. A regulated PNUTS mRNA to lncRNA splice switch mediates EMT and tumour progression. Nat Cell Biol 19, 1105–1115 (2017). https://doi.org/10.1038/ncb3595
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncb3595