Abstract
Which genetic alterations drive tumorigenesis and how they evolve over the course of disease and therapy are central questions in cancer biology. Here we identify 44 recurrently mutated genes and 11 recurrent somatic copy number variations through whole-exome sequencing of 538 chronic lymphocytic leukaemia (CLL) and matched germline DNA samples, 278 of which were collected in a prospective clinical trial. These include previously unrecognized putative cancer drivers (RPS15, IKZF3), and collectively identify RNA processing and export, MYC activity, and MAPK signalling as central pathways involved in CLL. Clonality analysis of this large data set further enabled reconstruction of temporal relationships between driver events. Direct comparison between matched pre-treatment and relapse samples from 59 patients demonstrated highly frequent clonal evolution. Thus, large sequencing data sets of clinically informative samples enable the discovery of novel genes associated with cancer, the network of relationships between the driver events, and their impact on disease relapse and clinical outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Accession codes
Data deposits
CLL8 WES data is deposited in dbGaP under accession code phs000922.v1.p1.
References
Quesada, V. et al. Exome sequencing identifies recurrent mutations of the splicing factor SF3B1 gene in chronic lymphocytic leukemia. Nature Genet. 44, 47–52 (2012)
Puente, X. S. et al. Whole-genome sequencing identifies recurrent mutations in chronic lymphocytic leukaemia. Nature 475, 101–105 (2011)
Landau, D. A. et al. Evolution and impact of subclonal mutations in chronic lymphocytic leukemia. Cell 152, 714–726 (2013)
Schuh, A. et al. Monitoring chronic lymphocytic leukemia progression by whole genome sequencing reveals heterogeneous clonal evolution patterns. Blood 120, 4191–4196 (2012)
Lawrence, M. S. et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 505, 495–501 (2014)
Hallek, M. et al. Addition of rituximab to fludarabine and cyclophosphamide in patients with chronic lymphocytic leukaemia: a randomised, open-label, phase 3 trial. Lancet 376, 1164–1174 (2010)
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013)
Edelmann, J. et al. High-resolution genomic profiling of chronic lymphocytic leukemia reveals new recurrent genomic alterations. Blood 120, 4783–4794 (2012)
De Paoli, L. et al. MGA, a suppressor of MYC, is recurrently inactivated in high risk chronic lymphocytic leukemia. Leuk. Lymphoma 54, 1087–1090 (2013)
Schlosser, I. et al. Dissection of transcriptional programmes in response to serum and c-Myc in a human B-cell line. Oncogene 24, 520–524 (2005)
Jiang, X. et al. Critical role of SHP2 (PTPN11) signaling in germinal center-derived lymphoma. Haematologica 99, 1834–1845 (2014)
Zhang, J. & Chen, Q. M. Far upstream element binding protein 1: a commander of transcription, translation and beyond. Oncogene 32, 2907–2916 (2013)
Tiacci, E. et al. BRAF mutations in hairy-cell leukemia. N. Engl. J. Med. 364, 2305–2315 (2011)
Brastianos, P. K. et al. Exome sequencing identifies BRAF mutations in papillary craniopharyngiomas. Nature Genet. 46, 161–165 (2014)
Heidorn, S. J. et al. Kinase-dead BRAF and oncogenic RAS cooperate to drive tumor progression through CRAF. Cell 140, 209–221 (2010)
Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014)
Yang, H. et al. RG7204 (PLX4032), a selective BRAFV600E inhibitor, displays potent antitumor activity in preclinical melanoma models. Cancer Res. 70, 5518–5527 (2010)
Jebaraj, B. M. et al. BRAF mutations in chronic lymphocytic leukemia. Leuk. Lymphoma 54, 1177–1182 (2013)
Landau, D. A. & Wu, C. J. Chronic lymphocytic leukemia: molecular heterogeneity revealed by high-throughput genomics. Genome Med. 5, 47 (2013)
Sashida, G. et al. ELF4/MEF activates MDM2 expression and blocks oncogene-induced p16 activation to promote transformation. Mol. Cell. Biol. 29, 3687–3699 (2009)
Park, J. et al. Dyrk1A phosphorylates p53 and inhibits proliferation of embryonic neuronal cells. J. Biol. Chem. 285, 31895–31906 (2010)
Gazda, H. T. et al. Ribosomal protein L5 and L11 mutations are associated with cleft palate and abnormal thumbs in Diamond-Blackfan anemia patients. Am. J. Hum. Genet. 83, 769–780 (2008)
Ferreiros-Vidal, I. et al. Genome-wide identification of Ikaros targets elucidates its contribution to mouse B-cell lineage specification and pre-B-cell differentiation. Blood 121, 1769–1782 (2013)
Billot, K. et al. Deregulation of Aiolos expression in chronic lymphocytic leukemia is associated with epigenetic modifications. Blood 117, 1917–1927 (2011)
Nückel, H. et al. The IKZF3 (Aiolos) transcription factor is highly upregulated and inversely correlated with clinical progression in chronic lymphocytic leukaemia. Br. J. Haematol. 144, 268–270 (2009)
Beà, S. et al. Genetic imbalances in progressed B-cell chronic lymphocytic leukemia and transformed large-cell lymphoma (Richter’s syndrome). Am. J. Pathol. 161, 957–968 (2002)
Carter, S. L. et al. Absolute quantification of somatic DNA alterations in human cancer. Nature Biotechnol. 30, 413–421 (2012)
Papaemmanuil, E. et al. Clinical and biological implications of driver mutations in myelodysplastic syndromes. Blood 122, 3616–3627 (2013)
Wang, J. et al. Tumor evolutionary directed graphs and the history of chronic lymphocytic leukemia. Elife 3, (2014)
Stilgenbauer, S. et al. Gene mutations and treatment outcome in chronic lymphocytic leukemia: results from the CLL8 trial. Blood 123, 3247–3254 (2014)
Rossi, D. et al. Integrated mutational and cytogenetic analysis identifies new prognostic subgroups in chronic lymphocytic leukemia. Blood 121, 1403–1412 (2013)
Damm, F. et al. Acquired initiating mutations in early hematopoietic cells of CLL patients. Cancer Discov. 4, 1088–1101 (2014)
Winkelmann, N. et al. Low frequency mutations independently predict poor treatment-free survival in early stage chronic lymphocytic leukemia and monoclonal B-cell lymphocytosis. Haematologica 100, e237–e239 (2015)
Puente, X. S. & Lopez-Otin, C. The evolutionary biography of chronic lymphocytic leukemia. Nature Genet. 45, 229–231 (2013)
Nowak, M. A. et al. The role of chromosomal instability in tumor initiation. Proc. Natl Acad. Sci. USA 99, 16226–16231 (2002)
Bozic, I. et al. Accumulation of driver and passenger mutations during tumor progression. Proc. Natl Acad. Sci. USA 107, 18545–18550 (2010)
Davoli, T. et al. Cumulative haploinsufficiency and triplosensitivity drive aneuploidy patterns and shape the cancer genome. Cell 155, 948–962 (2013)
Hallek, M. Chronic lymphocytic leukemia: 2015 Update on diagnosis, risk stratification, and treatment. Am. J. Hematol. 90, 446–460 (2015)
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500, 415–421 (2013)
Vogelstein, B. et al. Cancer genome landscapes. Science 339, 1546–1558 (2013)
Acknowledgements
We thank all members of the Broad Institute’s Biological Samples, Genetic Analysis and Genome Sequencing Platforms, who made this work possible (NHGRI-U54HG003067). We further thank all patients and their physicians for CLL8 trial participation and donation of samples; M. Mendila, N. Valente, S. Zurfluh, M. Wenger and J. Wingate for their support in conception and conduct of the CLL8 trial. D.A.L. is supported by an ACS Postdoctoral Fellowship, ASH Scholar Award, and the Burroughs Wellcome Fund Career Award for Medical Scientists and by the NIH Big Data to Knowledge initiative (BD2K, 1K01ES025431-01). J.G.R. was supported by the European Research Council (ERC) start grant 279307: Graph Games, Austrian Science Fund (FWF) grant no. P23499-N23, and FWF NFN grant no S11407-N23 RiSE. S.B. is supported by the German Jose Carreras Leukemia Foundation (project R 06/03v). M.H. is supported by the Deutsche Forschungsgemeinschaft (KFO 286, Project 6). S.S. is supported by the Else Kröner-Fresenius-Stiftung (2010_Kolleg24, 2012_A146), Virtual Helmholtz Institute (VH-VI-404), CLL Global Research Foundation (Alliance), and Deutsche Forschungsgemeinschaft (SFB 1074 projects B1, B2). C.J.W. acknowledges support from the Blavatnik Family Foundation, AACR (SU2C Innovative Research Grant), and NIH/NCI (1R01CA182461-02, 1R01CA184922-01, 1U10CA180861-01).
Author information
Authors and Affiliations
Contributions
All authors contributed extensively to the work presented in this paper. D.A.L., D.N., G.G., E.T., S.S. and C.J.W. contributed to study conception and design. E.T., S.B., J.E., S.K., M.K., M.R., A.F., K.F., H.D., M.H. and S.S. performed patient selection, provided the DNA samples, and prior matched clinical and genetic data sets. C.L.S., S.G. and E.S.L. enabled sample sequencing. D.A.L., A.N.T., C.S., M.L., K.C., M.R., J.M.H., S.L.C. and G.G. contributed to the computational genomics analysis. D.A.L., E.T., J.G.R., J.B., S.K., I.B., D.M., M.A.N., D.N., G.G., S.S. and C.J.W. contributed to additional data analysis as well as manuscript preparation. All authors contributed to the writing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
S.B., S.S. and M.H. have received research support and honoraria from F. Hoffmann-La Roche. S.B. is a recipient of honoraria and research support from AbbVie and of research support from Celgene. All other authors have no conflicts of interest.
Extended data figures and tables
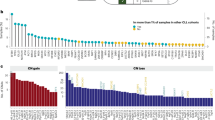
Extended Data Figure 1 Candidate CLL cancer genes discovered in the combined cohort of 538 primary CLL samples.
Significantly mutated genes identified in 538 primary CLL. Top panel: the rate of coding mutations (mutations per megabase) per sample. Centre panel: detection of individual genes found to be mutated (sSNVs or sIndels) in each of the 538 patient samples (columns), colour-coded by type of mutation. Only one mutation per gene is shown if multiple mutations from the same gene were found in a sample. Right panel: Q-values (red, Q < 0.1; purple dashed, Q < 0.25) and Hugo symbol gene identification. New candidate CLL genes are marked with asterisks. Left panel: the percentages of samples affected with mutations (sSNVs and sIndels) in each gene. Bottom panel: plots showing allelic fractions and the spectrum of mutations (sSNVs and sIndels) for each sample.
Extended Data Figure 2 Cellular networks and processes affected by putative CLL drivers.
Putative CLL cancer genes cluster in pathways that are central to CLL biology such as Notch signalling, inflammatory response and B-cell receptor signalling. In addition, proteins that participate in central cellular processes such as DNA damage repair, chromatin modification and mRNA processing, export and translation are also recurrently affected. New CLL subpathways highlighted by the current driver discovery effort are shown in yellow boxes. Red circles indicate putative driver genes previously identified3; purple circles indicate genes newly identified in the current study.
Extended Data Figure 3 RNA-seq expression data for candidate CLL genes and targeted candidate driver validation.
a, Matched RNA-seq and WES data were available for 156 CLLs (103 CLLs previously reported3 and 53 CLLs from the ICGC studies1). From the WES of these 156 cases, we identified 318 driver mutations (sSNVs and sIndels). For each site, we quantified the number of alternative reads corresponding to the somatic mutation in matched RNA-seq data. We subsequently counted the number of instances in which a mutation was detected (‘detected’) and compared it to the number of instances in which mutation detection had >90% power based on the allelic fraction in the WES and the read depth in the RNA-seq data (‘powered’). Overall, we detected 78.1% of putative CLL gene mutations at sites that had >90% power for detection in RNA-seq data. b, Targeted orthogonal validation (Access Array System, Fluidigm) was performed for 71 mutations (sSNVs and sIndels) in putative CLL genes, affecting 47 CLLs from the CLL8 cohort (selected on the basis of sample availability). With a mean depth of coverage of 7,472×, 65 of the 71 mutations (91.55%) validated, with a higher variant allele fraction compared with normal sample DNA (binomial P < 0.01).
Extended Data Figure 4 Gene mutation maps for candidate CLL genes.
a–v, Individual gene mutation maps are shown for all newly identified candidate CLL cancer genes not included in Fig. 2. The plots show mutation subtype (for example, missense, nonsense) and position along the gene.
Extended Data Figure 5 CLL copy number profiles.
Copy number profile across 538 CLLs detected from WES data from primary samples (see Supplementary Methods).
Extended Data Figure 6 Annotation of drivers based on clinical characteristics and co-occurrence patterns.
a, Putative drivers affecting greater than 10 patients were assessed for enrichment in IGHV mutated versus unmutated CLL subtype (Fisher’s exact test, magenta line denotes P = 0.05). b, Putative drivers affecting greater than 10 patients were assessed for enrichment in samples that received therapy before sampling (Fisher’s exact test). Putative drivers affecting greater than 10 patients were tested for co-occurrence. c, d, Significantly high (c) or low (d) co-occurrences are shown (Q < 0.1, Fisher’s exact test with Benjamini Hochberg, false discovery rate, after accounting for prior therapy and IGHV mutation status, see Supplementary Methods).
Extended Data Figure 7 Mutation spectrum analysis, clonal versus subclonal sSNVs.
The spectrum of mutation is shown for the clonal and subclonal subsets of coding somatic sSNVs across WES of 538 samples. The rate is calculated by dividing the number of trinucleotides with the specified sSNVs by the covered territory containing the specified trinucleotide. Both clonal and subclonal sSNVs were similarly dominated by C > T transitions at CpG sites. Thus, this mutational process that was previously associated with ageing39 not only predates oncogenic transformation (since clonal mutations will be highly enriched in mutations that precede the malignant transformation40) but also is the dominant mechanism of malignant diversification after transformation in CLL.
Extended Data Figure 8 The CLL driver landscape in the CLL8 cohort.
Somatic mutation information shown across the 55 candidate CLL cancer genes and recurrent somatic CNAs (rows) for 278 CLL samples collected from patients enrolled on the CLL8 clinical trial primary that underwent WES (columns). Recurrent somatic CNA labels are listed in blue, candidate CLL cancer genes are listed in bold if previously identified in Landau et al.3, and with an asterisk if newly identified in the current study.
Extended Data Figure 9 CLL8 patient cohort clinical outcome (from 278 patients) information by CLL cancer gene.
Kaplan–Meier analysis (with logrank P values) for putative drivers not associated with significant impact on progression-free survival (PFS) or overall survival (OS) in the cohort of 278 patients that were treated as part of the CLL8 trial. For candidate CLL genes tested here for the first time regarding impact on outcome, a Bonferroni P value is also shown.
Extended Data Figure 10 Comparison of pre-treatment and relapse cancer cell fraction (CCF) for non-silent mutations in candidate CLL genes across 59 CLLs.
For each CLL gene mutated across the 59 CLLs that were sampled longitudinally, the modal CCF is compared between the pre-treatment and relapse samples. CCF increases (red), decreases (blue) or stable CCF (grey) over time are shown (in addition to CLL genes shown in Fig. 5). A significant change in CCF over time (red or blue) was determined if the 95% CI of the CCF in the pre-treatment and relapse samples did not overlap.
Supplementary information
Supplementary Information
This file contains Supplementary Tables 1, 5, 7, 8 and 9, Supplementary Methods and a Supplementary Bibliography. (PDF 386 kb)
Supplementary Data
This file contains Supplementary Table 2. (XLSX 328 kb)
Supplementary Data
This file contains Supplementary Table 3. (XLSX 2452 kb)
Supplementary data
This file contains Supplementary Table 4. (XLSX 19704 kb)
Supplementary Data
This file contains Supplementary Table 6. (XLSX 49 kb)
Supplementary Data
This file contains Supplementary Table 10. (XLSX 246 kb)
Rights and permissions
About this article
Cite this article
Landau, D., Tausch, E., Taylor-Weiner, A. et al. Mutations driving CLL and their evolution in progression and relapse. Nature 526, 525–530 (2015). https://doi.org/10.1038/nature15395
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature15395
This article is cited by
-
Activation-induced cytidine deaminase causes recurrent splicing mutations in diffuse large B-cell lymphoma
Molecular Cancer (2024)
-
CXCR4 overexpression in chronic lymphocytic leukemia associates with poorer prognosis: A prospective, single-center, observational study
Genes & Immunity (2024)
-
Alternative splicing in prostate cancer progression and therapeutic resistance
Oncogene (2024)
-
AIOLOS-Associated Inborn Errors of Immunity
Journal of Clinical Immunology (2024)
-
Immuno-regulatory malignant B cells contribute to Chronic Lymphocytic Leukemia progression
Cancer Gene Therapy (2023)