Abstract
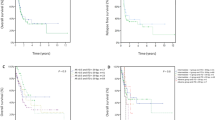
Recurrent molecular markers have been routinely used in acute myeloid leukemia (AML) for risk assessment at diagnosis, whereas their post-induction monitoring still represents a debated issue. We evaluated the prognostic value and biological impact of minimal residual disease (MRD) and of the allelic ratio (AR) of FLT3-internal-tandem duplication (ITD) in childhood AML. We retrospectively screened 494 children with de novo AML for FLT3-ITD mutation, identifying 54 harboring the mutation; 51% of them presented high ITD-AR at diagnosis and had worse event-free survival (EFS, 19.2 versus 63.5% for low ITD-AR, <0.05). Forty-one percent of children with high levels of MRD after the 1st induction course, measured by a patient-specific real-time-PCR, had worse EFS (22.2 versus 59.4% in low-MRD patients, P<0.05). Next, we correlated these parameters with gene expression, showing that patients with high ITD-AR or persistent MRD had characteristic expression profiles with deregulated genes involved in methylation and acetylation. Moreover, patients with high CyclinA1 expression presented an unfavorable EFS (20.3 versus 51.2% in low CyclinA1 group, P<0.01). Our results suggest that ITD-AR levels and molecular MRD should be considered in planning clinical management of FLT3-ITD patients. Different transcriptional activation of epigenetic and oncogenic profiles may explain variability in outcome among these patients, for whom novel therapeutic approaches are desirable.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Accession codes
References
Pigazzi M, Masetti R, Bresolin S, Beghin A, Di Meglio A, Gelain S et al. MLL partner genes drive distinct gene expression profiles and genomic alterations in pediatric acute myeloid leukemia: an AIEOP study. Leukemia 2011; 25: 560–563.
Pigazzi M, Manara E, Bisio V, Aveic S, Masetti R, Menna G et al. Screening of novel genetic aberrations in pediatric acute myeloid leukemia: a report from the AIEOP AML-2002 study group. Blood 2012; 120: 3860–3862.
Sandahl JD, Coenen Ea, Forestier E, Harbott J, Johansson B, Kerndrup G et al. T(6;9)(p22;q34)/DEK-NUP214-rearranged pediatric myeloid leukemia: an international study of 62 patients. Haematologica 2014; 99: 865–872.
Masetti R, Pigazzi M, Togni M, Astolfi A, Indio V, Manara E et al. CBFA2T3-GLIS2 fusion transcript is a novel common feature in pediatric, cytogenetically normal AML, not restricted to FAB M7 subtype. Blood 2013; 121: 3469–3472.
Gruber Ta, Larson Gedman A, Zhang J, Koss CS, Marada S, Ta HQ et al. An Inv(16)(p13.3q24.3)-encoded CBFA2T3-GLIS2 fusion protein defines an aggressive subtype of pediatric acute megakaryoblastic leukemia. Cancer Cell 2012; 22: 683–697.
Pession A, Masetti R, Rizzari C, Putti MC, Casale F, Fagioli F et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood 2013; 122: 170–178.
Grimwade D, Freeman SD . Defining minimal residual disease in acute myeloid leukemia: which platforms are ready for ‘Prime Time’? Blood 2014; 124: 222–233.
Takahashi S . Downstream molecular pathways of FLT3 in the pathogenesis of acute myeloid leukemia: biology and therapeutic implications. J Hematol Oncol 2011; 4: 13.
Hayakawa F, Towatari M, Kiyoi H, Tanimoto M, Kitamura T, Saito H et al. Tandem-duplicated Flt3 constitutively activates STAT5 and MAP kinase and introduces autonomous cell growth in IL-3-dependent cell lines. Oncogene 2000; 19: 624–631.
Mizuki M, Fenski R, Halfter H, Matsumura I, Schmidt R, Müller C et al. Flt3 mutations from patients with acute myeloid leukemia induce transformation of 32D cells mediated by the Ras and STAT5 pathways. Blood 2000; 96: 3907–3914.
Kondo M, Horibe K, Takahashi Y, Matsumoto K, Fukuda M, Inaba J et al. Prognostic value of internal tandem duplication of the FLT3 gene in childhood acute myelogenous leukemia. Med Pediatr Oncol 1999; 33: 525–529.
Nakao M, Yokota S, Iwai T, Kaneko H, Horiike S, Kashima K et al. Internal tandem duplication of the flt3 gene found in acute myeloid leukemia. Leukemia 1996; 10: 1911–1918.
Abu-Duhier FM, Goodeve AC, Wilson GA, Gari MA, Peake IR, Rees DC et al. FLT3 internal tandem duplication mutations in adult acute myeloid leukaemia define a high-risk group. Br J Haematol 2000; 111: 190–195.
Kottaridis PD . The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood 2001; 98: 1752–1759.
Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: Association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002; 99: 4326–4335.
Levis M, Small D . FLT3: ITDoes matter in leukemia. Leukemia 2003; 17: 1738–1752.
Meshinchi S, Alonzo Ta, Stirewalt DL, Zwaan M, Zimmerman M, Reinhardt D et al. Clinical implications of FLT3 mutations in pediatric AML. Blood 2006; 108: 3654–3661.
Daver N, Cortes J, Ravandi F, Patel KP, Burger Ja, Konopleva M et al. Review article secondary mutations as mediators of resistance to targeted therapy in leukemia. Blood 2015; 125: 10–20.
Kern W, Haferlach T, Schoch C, Löffler H, Gassmann W, Sauerland MC et al. Early blast clearance by remission induction therapy is a major independent prognostic factor for both achievement of complete remission and long-term outcome in acute myeloid leukemia: data from the German AMLCooperative Group (AMLCG) 1992 Trial. Blood 2003; 101: 64–70.
Chen X, Xie H, Wood BL, Walter RB, Pagel JM, Becker PS et al. Relation of clinical response and minimal residual disease and their prognostic impact on outcome in acute myeloid leukemia. J Clin Oncol 2015; 33: 1268–1264.
Schlenk RF, Kayser S, Bullinger L, Kobbe G, Casper J, Ringhoffer M et al. Differential impact of allelic ratio and insertion site in FLT3-ITD-positive AML with respect to allogeneic transplantation. Blood 2014; 124: 3441–3449.
Meshinchi S, Stirewalt DL, Alonzo TA, Boggon TJ, Gerbing RB, Rocnik JL et al. Structural and numerical variation of FLT3 / ITD in pediatric AML Brief report Structural and numerical variation of FLT3 / ITD in pediatric AML. Blood 2012; 111: 4930–4933.
Locatelli F, Masetti R, Rondelli R, Zecca M, Fagioli F, Rovelli A et al. Outcome of children with high-risk acute myeloid leukemia given autologous or allogeneic hematopoietic cell transplantation in the aieop AML-2002/01 study. Bone Marrow Transplant 2014; 50: 181–188.
Pigazzi M, Manara E, Bresolin S, Tregnago C, Beghin A, Baron E et al. MicroRNA-34b promoter hypermethylation induces CREB overexpression and contributes to myeloid transformation. Haematologica 2013; 98: 602–610.
Zhao M, Sun J, Zhao Z . TSGene: a web resource for tumor suppressor genes. Nucleic Acids Res 2013; 41: D970–D976.
Zhan M, Riordon DR, Yan B, Tarasova YS, Bruweleit S, Tarasov KV et al. The B-MYB transcriptional network guides cell cycle progression and fate decisions to sustain self-renewal and the identity of pluripotent stem cells. PLoS ONE 2012; 7: e42350.
Paganin M, Zecca M, Fabbri G, Polato K, Biondi A, Rizzari C et al. Minimal residual disease is an important predictive factor of outcome in children with relapsed ‘high-risk’ acute lymphoblastic leukemia. Leukemia 2008; 22: 2193–2200.
Grimwade D, Jovanovic JV, Hills RK, Nugent EA, Patel Y, Flora R et al. Prospective minimal residual disease monitoring to predict relapse of acute promyelocytic leukemia and to direct pre-emptive arsenic trioxide therapy. J Clin Oncol 2009; 27: 3650–3658.
Pigazzi M, Manara E, Buldini B, Beqiri V, Bisio V, Tregnago C et al. Minimal residual disease monitored after induction therapy by RQ-PCR can contribute to tailor treatment of patients with t(8;21) RUNX1-RUNX1T1 rearrangement. Haematologica 2015; 100: e99–101.
Inaba H, Coustan-Smith E, Cao X, Pounds SB, Shurtleff Sa, Wang KY et al. Comparative analysis of different approaches to measure treatment response in acute myeloid leukemia. J Clin Oncol 2012; 30: 3625–3632.
Kayser S, Schlenk RF, Grimwade D, Yosuico VE, Walter RB . Evidence-based focused review minimal residual disease—directed therapy in acute myeloid leukemia. Blood 2015; 125: 2331–2336.
Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S et al. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood 1999; 93: 3074–3080.
Zwaan CM, Kolb Ea, Reinhardt D, Abrahamsson J, Adachi S, Aplenc R et al. Collaborative efforts driving progress in pediatric acute myeloid leukemia. J Clin Oncol 2015; 33: 2949–2962.
Gill S, Tasian SK, Ruella M, Shestova O, Li Y, Porter DL et al. Preclinical targeting of human acute myeloid leukemia and myeloablation using chimeric antigen receptor-modified T cells. Blood 2014; 123: 2343–2354.
Cauchy P, James SR, Zacarias-Cabeza J, Ptasinska A, Imperato MR, Assi SA et al. Chronic FLT3-ITD signaling in acute myeloid leukemia is connected to a specific chromatin signature. Cell Rep 2015; 12: 821–836.
Bali P, George P, Cohen P, Tao J, Guo F, Sigua C et al. Superior activity of the combination of histone deacetylase inhibitor LAQ824 and the FLT-3 kinase inhibitor PKC412 against human acute myelogenous leukemia cells with mutant FLT-3. Clin Cancer Res 2004; 10: 4991–4997.
Nishioka C, Ikezoe T, Yang J, Takeuchi S, Phillip Koeffler H, Yokoyama A . MS-275, a novel histone deacetylase inhibitor with selectivity against HDAC1, induces degradation of FLT3 via inhibition of chaperone function of heat shock protein 90 in AML cells. Leuk Res 2008; 32: 1382–1392.
Pietschmann K, Bolck HA, Buchwald M, Spielberg S, Polzer H, Spiekermann K et al. Breakdown of the FLT3-ITD/STAT5 axis and synergistic apoptosis induction by the histone deacetylase inhibitor panobinostat and FLT3-specific inhibitors. Mol Cancer Ther 2012; 11: 2373–2383.
Liao C, Wang XY, Wei HQ, Li SQ, Merghoub T, Pandolfi PP et al. Altered myelopoiesis and the development of acute myeloid leukemia in transgenic mice overexpressing cyclin A1. Proc Natl Acad Sci USA 2001; 98: 6853–6858.
Li Y, Zhu X, Gu J, Hu H, Dong D, Yao J et al. Anti-miR-21 oligonucleotide enhances chemosensitivity of leukemic HL60 cells to arabinosylcytosine by inducing apoptosis. Hematology 2010; 15: 215–221.
Hong L, Han Y, Zhang Y, Zhang H, Zhao Q, Wu K et al. MicroRNA-21: a therapeutic target for reversing drug resistance in cancer. Expert Opin Ther Targets 2013; 17: 1073–1080.
Rommer A, Steinleitner K, Hackl H, Schneckenleithner C, Engelmann M, Scheideler M et al. Overexpression of primary microRNA 221/222 in acute myeloid leukemia. BMC Cancer 2013; 13: 364.
Garofalo M, Quintavalle C, Romano G, Croce CM, Condorelli G . miR221/222 in cancer: their role in tumor progression and response to therapy. Curr. Mol. Med. 2012; 12: 27–33.
Ekberg J, Landberg G, Holm C, Richter J, Wolgemuth DJ, Persson JL . Regulation of the cyclin A1 protein is associated with its differential subcellular localization in hematopoietic and leukemic cells. Oncogene 2004; 23: 9082–9089.
Acknowledgements
This work was supported by CARIPARO Istituto di Ricerca Pediatrica-Fondazione Città della Speranza to GB, EM, MZ; Università degli Studi di Padova to CT, VB, BB, MP, and by the special grant 5 × 1.000 of AIRC (Associazione Italiana Ricerca sul Cancro) to FL.
Author contributions
EM, CT, VB, MF, MZ, BB and GC performed experiments; KP, RM, GC, BB, RR, GM, FG, AB, AP, FL, PM and GB collected samples in AIEOP centers; EM, RR and RM performed the statistical analysis; EM, GB, FL, MP designed the research, analyzed and interpreted data, and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Manara, E., Basso, G., Zampini, M. et al. Characterization of children with FLT3-ITD acute myeloid leukemia: a report from the AIEOP AML-2002 study group. Leukemia 31, 18–25 (2017). https://doi.org/10.1038/leu.2016.177
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2016.177
This article is cited by
-
Outcomes and prognosis of haploidentical haematopoietic stem cell transplantation in children with FLT3-ITD mutated acute myeloid leukaemia
Bone Marrow Transplantation (2024)
-
NUP98-fusion transcripts characterize different biological entities within acute myeloid leukemia: a report from the AIEOP-AML group
Leukemia (2017)