Abstract
Thalidomide and the immunomodulatory drug, lenalidomide, are therapeutically active in hematological malignancies. The ubiquitously expressed E3 ligase protein cereblon (CRBN) has been identified as the primary teratogenic target of thalidomide. Our studies demonstrate that thalidomide, lenalidomide and another immunomodulatory drug, pomalidomide, bound endogenous CRBN and recombinant CRBN–DNA damage binding protein-1 (DDB1) complexes. CRBN mediated antiproliferative activities of lenalidomide and pomalidomide in myeloma cells, as well as lenalidomide- and pomalidomide-induced cytokine production in T cells. Lenalidomide and pomalidomide inhibited autoubiquitination of CRBN in HEK293T cells expressing thalidomide-binding competent wild-type CRBN, but not thalidomide-binding defective CRBNYW/AA. Overexpression of CRBN wild-type protein, but not CRBNYW/AA mutant protein, in KMS12 myeloma cells, amplified pomalidomide-mediated reductions in c-myc and IRF4 expression and increases in p21WAF-1 expression. Long-term selection for lenalidomide resistance in H929 myeloma cell lines was accompanied by a reduction in CRBN, while in DF15R myeloma cells resistant to both pomalidomide and lenalidomide, CRBN protein was undetectable. Our biophysical, biochemical and gene silencing studies show that CRBN is a proximate, therapeutically important molecular target of lenalidomide and pomalidomide.
Similar content being viewed by others
Introduction
In multiple myeloma, myelodysplastic syndrome and lymphomas, thalidomide and/or the structurally analogous compound lenalidomide, are antiproliferative, increase immune surveillance and decrease stromal cell support.1, 2, 3, 4 Lenalidomide has a different spectrum of preclinical and clinical activities from thalidomide, including increased efficacy in tumor and immune cells.5, 6 The chemically related immunomodulatory drug candidate, pomalidomide, has a distinct and heightened antiproliferative potency compared with lenalidomide and demonstrates clinical efficacy in settings of lenalidomide resistance.7, 8
The mechanism of action of lenalidomide has been explored in tumor cells, myeloid cells and stromal cells.9, 10, 11 In myeloma lines, lenalidomide has cell-type and cell-context dependent pleiotropic effects.1, 2, 3, 4, 12, 13, 14, 15 These include G0/G1 arrest associated with the upregulation of the cyclin-dependent kinase inhibitor p21WAF-1, and downregulation of the expression of interferon regulatory factor 4 (IRF4) in both multiple myeloma lines and bone marrow samples from lenalidomide-treated myeloma patients.12, 13, 14 Lenalidomide decreases the expression of anti-apoptotic and translation checkpoint proteins Bcl2 and eIF4E15 and modulates activation of RhoGTPases in T cells,16 an effect critical for actin hyperpolymerization and immune synapse formation.17 In addition, lenalidomide co-stimulates T cell proliferation and cytokine production3 and inhibits angiogenesis and bone marrow stromal cell growth factor production.18, 19
Following more than a decade of research on the mechanism of action of thalidomide, preclinical studies identified E3 ligase protein cereblon (CRBN) as a direct molecular target for the teratogenecity of thalidomide. CRBN binds directly to thalidomide analog affinity beads and is linked to the teratogenic effects of thalidomide in zebrafish and chicks.20 CRBN is highly conserved from plants to mammals and the mRNA for human, rat and mouse is ubiquitously expressed.21 A truncating mutation at R419, deleting the C terminus results in a familial syndrome of mild mental retardation.22, 23 CRBN binds to a calcium-activated potassium channel in the brain, a chloride channel in the retina,24, 25, 26 and to AMP kinase, a critical sensor/transducer protein regulating metabolic pathways in eukaryotic cells.27 CRBN and DNA damage binding protein-1 (DDB1) form a functional E3 ligase complex with Cul4A and Roc1. The CRBN autoubiquitination activity of this complex was inhibited by thalidomide.20
The current study, undertaken to explore the potential role of CRBN as a therapeutic target, provides biophysical, biochemical and additional functional evidence that human CRBN is a direct target of lenalidomide and pomalidomide.
Materials and methods
Cell culture
Cell lines NCI-H929 and U266 were obtained from ATCC (American Type Culture Collection, Manassas, VA, USA). DF15 cells were obtained from John Shaughnessy (University of Arkansas, Little Rock, AR, USA). Cells were grown in RPMI-I640 medium containing 10% (V/V) heat-inactivated fetal bovine serum (Gibco, Grand Island, NY, USA) supplemented with 2 mM glutamine. To produce lenalidomide resistant cell lines, NCI-H929 cells were treated continuously (fresh lenalidomide was added every 3–4 days) with control (final 0.1% dimethyl sulfoxide (DMSO)) or low-dose lenalidomide (1 μM) for 2 months until the proliferation of cells was no longer inhibited by lenalidomide (1 μM), as determined by cell viability (Vi-cell XR cell viability analyzer, Beckman Coulter, Indianapolis, IN, USA), cell proliferation by flow cytometry and cell cycle analysis (propidium iodide staining). After acquisition of resistance to 1 μM, the resistant H929 cell lines were treated with lenalidomide (10 μM) for a further 4 months. After this period of time, the cell cultures achieved fully establish resistance up to high-dose lenalidomide (30 μM). Prior to the experiments described here, H929 lenalidomide-resistant cells were taken out of culture with compounds for 5–7 days before use. DF15 cells were made resistant to pomalidomide by continuous culture in the presence of increasing concentrations of pomalidomide (0.1–100 μM) for at least 5 months to achieve stable pomalidomide resistance. Prior to the experiments described here, DF15R pomalidomide-resistant cells were taken out of culture with compounds for 5–7 days before use.
CRBN anti-sera production, validation, immunoblot and immunofluorescence analyses
See online Supplemental Methods section.
Cloning, expression and purification of human CRBN and DDB1
See online Supplemental Methods section.
Fluorescence thermal melt assay to measure binding of compounds to recombinant CRBN
Thermal stabilities of CRBN–DDB1 in the presence or absence of phthalimide, thalidomide, lenalidomide and pomalidomide were done in the presence of Sypro Orange in a microplate format according to Pantoliano et al.28 Two μg of protein in 20 μl of assay buffer (25 mM Tris HCl, pH 8.0, 150 mM NaCl, 2 μM Sypro Orange) were subjected to stepwise increase of temperature from 20 to 70 °C and the fluorescence was read at every 1 °C on an ABIPrism 7900HT (Applied Biosystems, Carlsbad, CA, USA). Compounds were dissolved in DMSO (1% final in assay) and tested in quadruplicate at a concentration range between 30 nM to 1000 μM; controls contained 1% DMSO only.
Thalidomide analog bead assay to measure compound binding to endogenous CRBN
Coupling of thalidomide analog to FG-magnetic nanoparticle beads (structure shown in Figure 1b) from Tamagawa Seiko Co. Tokyo, Japan was carried out as described20 and myeloma extract binding assays to these beads were performed with minor modifications. U266, DF15 or DF15R myeloma cell extracts or HEK293T extracts were prepared in NP 40 lysis buffer (0.5% NP40, 50 mM Tris HCl (pH 8.0)), 150 mM NaCl, 0.5 mM dithiothreitol, 0.25 mM phenylmethanesulfonylfluoride, 1x protease inhibitor mix (Roche, Indianapolis, IN, USA) at approximately 2 × 108 cells per ml (20 mg protein/ml). Cell debris and nucleic acids were cleared by centrifugation (14 000 r.p.m. 30 min 4 °C). In competition experiments 0.5 ml (3–5 mg protein) aliquots of the resulting extracts were preincubated (15 min room temperature) with 5 μl DMSO (control) or 5 μl compound at varying concentrations in DMSO. Thalidomide analog-coupled beads (0.3–0.5 mg) were added to protein extracts and samples rotated (2 h, 4 °C). Beads were washed three times with 0.5 ml NP40 buffer and then bound proteins were eluted with sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS–PAGE) sample buffer. In bead elution experiments, HEK293T extracts were not preincubated with compounds but final elution was with 1 mM phthalimide, 1 mM glutarimide (final 1% DMSO) or 1% DMSO in NP40 lysis buffer. Samples were subjected to SDS–PAGE and immunoblot analysis performed (as described in Supplementary Methods) using anti-CRBN 65–76 (1:10 000 dilution) for all studies except HEK293T and KMS12-PE studies in which a mouse monoclonal anti-CRBN 1–18 was utilized; other antisera dilutions were DDB1 (1:2000 dilution) or β-actin (1:10 000 dilution). In thalidomide affinity bead competition assays, a LI-COR Odessey system was used to quantify CRBN band density and relative amounts of CRBN were determined by averaging at least three DMSO controls and expressing CRBN in each competition sample as percent inhibition of CRBN protein relative to the averaged controls as 100% binding. Approximate IC50 values were determined by GraFit (Erithacus software, Surrey, UK).
Binding of lenalidomide and pomalidomide to CRBN within the CRBN–DDB1 complex. (a) Fluorescence-based thermal shift assay of binding of lenalidomide (▪), pomalidomide (▴) and thalidomide (○) but not pthalimide (•) to a recombinant human CRBN–DDB1 complex. Representative curves from one of two independent experiments with similar results. (b) Structures of compounds utilized in these studies and thalidomide analog magnetic affinity beads (FG beads). The glutarimide moiety in each compound is highlighted in red. (c) Immunoblot analyses of rabbit anti-hCRBN and mouse anti-hDDB1 from U266 myeloma cell extract bound to thalidomide analog beads; In=U266 total protein input before affinity bead binding; DMSO=U266 extract control (1% DMSO preincubation); Len=U266 extract preincubated with lenalidomide (100 μM), Pom=U266 extract preincubated with pomalidomide (100 μM). Fluorescent labeled donkey anti-mouse antisera (green, DDB1) and goat anti-rabbit (red, CRBN) were used to identify proteins. Representative immunoblot from at least five independent experiments with similar results. (d) Immunoblot analysis of HEK293T extracts incubated with thalidomide analog affinity beads and eluted with 1 mM of thalidomide, phthalimide or glutarimide. Input extract before bead purification =In. (e) Immunoblot analysis of HEK293T extracts pre-incubated with thalidomide (Thal), lenalidomide (Len) or pomalidomide (Pom) at indicated concentrations and bound to thalidomide analog affinity beads, washed and eluted with SDS buffer as described in Materials and Methods. Input extract before bead purification (In) also shown in the immunoblot. (f) CRBN binding dose–response to lenalidomide in U266 extracts; Insert shows immunoblot of CRBN of dose–response competition of U266 extract CRBN by preincubation of varying concentrations of lenalidomide. (g) U266 extract CRBN binding dose–response of pomalidomide. Insert shows immunoblot of CRBN of dose–response competition of U266 extract CRBN by preincubation with varying concentrations of pomalidomide. Data for Figure 1f and g are representative of two similar dose–response experiments with IC50 values of ∼1 and ∼2 μM, respectively.
Cellular ubiquitination assay
HEK293T cells stably expressing FLAG-HA-tagged (FH)-CRBN or FH-CRBNYW/AA were treated for 3 h before harvest with the proteasome inhibitor MG132 (10 μM) or left untreated. Lysates were prepared as described20 and incubated with anti-FLAG (M2, Sigma, St Louis, MO, USA) agarose beads. FH-CRBN was eluted with SDS–PAGE buffer and SDS–PAGE separated proteins immunoblotted with anti-HA antibody (3F10, Roche). Unless otherwise indicated, compounds were added to cells 3 h before addition of MG132.
Short hairpin RNA of CRBN knockdown studies
See online Supplemental Methods section.
T cell isolation and activity assays
T cells were isolated from human leukocytes (Blood Center of New Jersey, East Orange, NJ, USA) by centrifugation through Ficoll following the ‘RosetteSep’ protocol (Stem Cell Technologies, Vancouver, BC, Canada). Purified T cells were treated with 1 μg/ml PHA-L at 37°C for 24 h and then subjected to small interfering RNA (siRNA) transfection (300 nM siRNA of CRBN (siCRBN-1)/100 μl/ 2 × 106 cells/cuvette) using Amaxa Human T-cell Nucleofector kit (Lonza, Basel, Switzerland) with T-20 program. Control low GC content negative siRNA was also transfected. Transfected cells were cultured in RPMI containing 10% fetal bovine serum at 37 °C for 24 h. Cells (1 × 106) were collected for measuring knockdown efficiency by quantitative reverse transcription-PCR. The remaining transfected cells were seeded on prebound OKT3 (3 μg/ml) 96-well TC plates at 1.25 × 106 cells/200 μl per well and treated with DMSO or compounds in duplicate at 37 °C for 48 h. After 48 h the supernatants of drug-treated cells were collected and interleukin-2 or tumor necrosis factor-α production measured by enzyme-linked immunosorbent assay (Thermo Scientific, Rockford, IL, USA) according to the manufacturer’s directions. The siCRBN 1-transfected T cells were harvested at 72 h post transfection and CRBN protein reduction was determined by immunoblot analysis using the CRBN 65–76 antisera. Low GC siRNA-transfected cells were used as a negative control.
Statistical analyses
Analyses for the multiple group comparisons were performed with 1-way analysis of variance followed Dunnett’s posttest. P<0.05 was considered significant.
Results
Thalidomide, lenalidomide and pomalidomide bind to CRBN in vitro
Recombinant human ZZ-tagged CRBN and full length DDB1 expression plasmids were co-expressed in Sf9 cells. A complex containing both CRBN and DDB1 was purified from these cells (Supplementary Figure S1) and fluorescent thermal melt shift studies were performed on the purified complex in the presence of thalidomide, lenalidomide, the functionally related compound pomalidomide or phthalimide (a fragment of thalidomide not containing glutarimide) (Figures 1a and b). The purified ZZ-CRBN-DDB1 complex had greater stability and solubility than CRBN alone. Dose-dependent interaction with the CRBN-DDB1 complex was observed with thalidomide, lenalidomide and pomalidomide, with IC50 values of ∼30 μM, ∼3 μM and ∼3 μM, respectively (Figure 1a), while phthalimide (inactive in immunomodulatory and antiproliferative assays) showed no appreciable thermal melt shift with the CRBN–DDB1 complex.
To study lenalidomide and pomalidomide binding to CRBN in extracts from myeloma cells, we used thalidomide analog-coupled affinity beads prepared as previously described.20 Preincubation of U266 myeloma cell extracts with either lenalidomide (100 μM) or pomalidomide (100 μM) (Figure 1c) prevented CRBN and DDB1 binding to the thalidomide analog-coupled beads, as determined by immunoblot analysis of proteins selectively bound to the beads (CRBN antibody validation in Supplementary Figure S2). The U266 extract input appeared to express more DDB1 than CRBN, but CRBN protein was concentrated on the beads as observed in control (DMSO preincubation) eluates. To complement these competitive binding studies HEK293T CRBN prebound to the affinity beads was eluted with compounds thalidomide and glutarimide but not phthalimide (Figures 1b and d). Preincubation of HEK293T cell extracts with lenalidomide or pomalidomide, inhibited CRBN binding to the affinity beads with similar apparent potency, and both showed greater potency than thalidomide (Figure 1e). Thalidomide analog bead binding to endogenous CRBN in U266 myeloma extracts was dose-dependently inhibited by preincubation with either lenalidomide or pomalidomide with IC50 values of ∼2 μM (Figures 1f and g). Thus in two different cell lines, CRBN binding to thalidomide analog affinity beads were competitively inhibited by lenalidomide and pomalidomide. Notably glutarimide, but not phthalimide eluted CRBN from affinity beads.
CRBN short hairpin RNA reduces the effects of lenalidomide and pomalidomide in myeloma cells
Lentiviral vectors expressing CRBN short hairpin RNAs generated stably-transduced U266 cell lines with either 60 or 75% reduced expression of CRBN protein (insert Figure 2a) compared with the parental U266 line. These reduced CRBN expression cells (U266-CRBN60 and U266-CRBN75) were less responsive than the parental cells to antiproliferative effects lenalidomide across a dose–response range of 0.01 to 10 μM, and the reduction in response related directly to the level of reduction of CRBN (Figure 2a). The U266 cell lines with stably reduced CRBN expression (U266-CRBN60 and U266-CRBN75) retained greater sensitivity to inhibition of proliferation by pomalidomide but required higher concentrations for inhibition than the parental cells (Figure 2b). Expression of the tumor suppressor p21WAF-1 was increased in the parental U266 cells approximately threefold, by incubation with lenalidomide or pomalidomide for 48 h, but these increases were attenuated approximately 35% in U266-CRBN75 cells (Figures 2c and d). In contrast, abundance of IRF4, a protein critical for myeloma proliferation, was decreased approximately 1.7 fold by lenalidomide or pomalidomide in the parental U266 cells and compound-induced decreases were attenuated approximately 30% in U266-CRBN75 cells (Figures 2c and d).
Reduction of CRBN gene expression in U266 myeloma cells modulates antiproliferative response to lenalidomide and pomalidomide. (a) Lenalidomide dose–response inhibition of proliferation parental U266 versus lentiviral 60 and 75% CRBN-reduced cell lines. All points are average of quadruplicates. CRBN immunoblot of parental U266 cells and two clones of lentiviral transduced CRBN short hairpin RNA cells (insert Figure 2a). (b) Pomalidomide dose–response inhibition of proliferation of parental versus lentiviral 60 and 75% CRBN-reduced cell line. All points are average of quadruplicates. (c) Immunoblot analysis of CRBN, p21WAF-1 IRF4 and β-actin protein expression in U266-CRBN60 and U266-CRBN75 treated with DMSO (0.1%), 1 μM pomalidomide (Pom) or 10 μM lenalidomide (Len) for 48 h. (d) Percent change in expression of p21 (green bars) and IRF4 (red/orange bars) proteins from compound-treated cells to control-treated baselines were determined by densitometry of bands relative to β-actin in parental U266 and CRBN75 cells (as indicated in graph).
Binding incompetent CRBN abrogates thalidomide, lenalidomide and pomalidomide effects on autoubiquitination and prevents pomalidomide effects on protein abundance
As thalidomide was previously shown to inhibit autoubiquitination of CRBN,20 we evaluated the ability of lenalidomide and pomalidomide to inhibit CRBN autoubiquitination in HEK293T cells transfected with either FH-CRBN, or a mutant FH-CRBNYW/AA incompetent in its ability to bind thalidomide.20 HEK293T cells stably expressing wild-type FH-CRBN or FH-CRBNYW/AA were preincubated with compounds before the addition of the proteasome inhibitor MG132 to facilitate accumulation of ubiquitinated proteins20 (Figures 3a and b). While thalidomide, lenalidomide and pomalidomide were all effective dose-dependent inhibitors of wild-type FH-CRBN autoubiquitination (Figure 3a), they were unable to inhibit autoubiquitination of the binding defective mutant (Figure 3b).
Expression of FH-CRBNYW/AA prevents pomalidomide, lenalidomide or thalidomide inhibition of CRBN autoubiquitination in HEK293 cells and pomalidomide induction of protein changes in KMS12 cells. (a) Pomalidomide, lenalidomide and thalidomide inhibit autoubiquitination of CRBN. HEK293T cells stably expressing FLAG-HA CRBN (FH)-CRBN were established by lentiviral transduction. Cells were treated with the indicated concentrations of compounds for 3 h before harvest. FH-CRBN was immunoprecipitated (IP) with anti-FLAG antibody under stringent wash conditions and immunoblotted (IB) with anti-HA antibody. (b) HEK293T cells stably expressing FLAG-HA CRBN or FH-CRBNYW/AA were treated and processed as in Figure 3a. (c) Cartoon of CRBN E3 ligase complex. CRBN is bound to the adapter protein DDB1 that binds to Cul4A a scaffold protein for Roc1 and the E2 ubiquitin-conjugating enzyme. E2 adds ubiquitin protein either to CRBN itself (autoubiquitination) or to a putative substrate protein (S) that binds CRBN. X marks the inhibition of autoubiquitination of CRBN by thalidomide, lenalidomide or pomalidomide. (d) KMS12 cells constitutively expressing FH-CRBN or FH-CRBNYW/AA were established by lentiviral transduction and expression of CRBN determined in whole-cell extracts by immunoblot analysis with mouse anti-CRBN. (e) Control KMS12 cells (−) or cells stably expressing wild-type FH-CRBN or FH-CRBNYW/AA were treated with the indicated concentrations of pomalidomide and incubated for 48 h before extract preparation, SDS–PAGE and immunoblotting for c-myc or IRF4. (f) Control KMS12 cells or cells stably expressing FH-CRBNYW/AA were treated with the indicated concentrations of pomalidomide and incubated for 48 h before extract preparation, SDS–PAGE and immunoblotting for p21WAF-1 (p21).
The model cartoon of the CRBN E3 ligase complex in Figure 3c shows CRBN bound to the adaptor protein DDB1 linking to Cul4A, Roc1 and an E2 ubiquitin-conjugating enzyme. E2 ligase adds ubiquitin either to CRBN itself (autoubiquitination) or to a substrate protein (S) that binds CRBN. The inhibition of autoubiquitination of CRBN by thalidomide, lenalidomide or pomalidomide is indicated by an X. Other substrates ubiquitinated by the CRBN E3 ligase are not yet reported. It has not been clarified if these compounds’ effects are antagonistic or agonistic to the E3 ligase ubiquitination of putative additional substrates.
We also investigated effects of expression of the wild-type FH-CRBN versus the binding incompetent FH-CRBNYW/AA mutant in KMS12 myeloma cells. The expression levels of wild-type FH-CRBN and FH-CRBNYW/AA were determined to be approximately twofold and fourfold higher than endogenous CRBN, respectively (Figure 3d). Treatment ofwild-type FH-CRBN KMS12 cells with pomalidomide resulted in measurable decreases in c-myc and IRF4 namely, 57 and 45% (signal change by 100 nM pomalidomide relative to non-treated parental non-transfected KMS12 corrected for actin) (Figure 3e) and an increase in p21WAF-1 (Figure 3f) in parental cells namely 77% (signal change by 10 nM pomalidomide relative to non-treated parental non-transfected KMS12 corrected for actin) consistent with previous reports in other myeloma lines.12, 13, 14 In cells expressing the binding incompetent CRBN, pomalidomide-induced decreases in c-myc and IRF4, namely 13 and 6%, (signal change by 100 nM pomalidomide relative to non-treated parental non-transfected KMS12 corrected for actin) (Figure 3e) and increase in p21WAF-1 (Figure 3f), namely −3% (signal change by 10 nM pomalidomide relative to non-treated parental non-transfected KMS12 corrected for actin) were highly attenuated.
CRBN expression level modulates T-cell response to lenalidomide and pomalidomide
The stimulation of interleukin-2 production in activated T cells was much greater with the S- compared with the R-enantiomer of methyl-pomalidomide (Figure 4a), with IC50 values of 0.02 and >10 μM, respectively (Figure 4b). Competition of these methyl-pomalidomide enantiomers for CRBN binding to the thalidomide analog affinity beads correlated with the rank order of functional difference; IC50 values were ∼10 μM for the active S enantiomer and >300 μM for the inactive R enantiomer (Figure 4c). To complement the findings in multiple myeloma lines, we investigated the impact of reducing CRBN in activated human T cells by siCRBN treatment and confirmed a significant decrease in CRBN protein by immunoblot analysis (Figure 4d). Effects of lenalidomide or pomalidomide to induce T-cell production of interleukin-2 (5–23-fold) (Figure 4e) and tumor necrosis factor-α (a 5–10-fold) (Figure 4f) were significantly reduced by siCRBN.
Effects of S and R enantiomers of methyl-pomalidomide on T-cell cytokine production and U266 cell CRBN binding to thalidomide analog affinity beads. (a) Structures of S methyl-pomalidomide and R methyl-pomalidomide. (b) T cell activation of interleukin-2 production by S or R methyl-pomalidomide enantiomers; (?) S methyl-pomalidomide (Me-PomS) (•) R methyl-pomalidomide (Me-PomR). (c) CRBN immunoblot quantitation of S or R methyl-pomalidomide competition for thalidomide analog bead binding to CRBN from U266 extracts; (?) S methyl-pomalidomide (•) R methyl-pomalidomide; (d) Immunoblot of T cell CRBN protein reduction by siCRBN treatment for 72 h. (e) Activated T-cell interleukin-2-induction and (f) tumor necrosis factor-α-induction by lenalidomide and pomalidomide at the indicated concentrations in the presence of control siRNA or CRBN siRNA for 72 h.
Acquired resistance to lenalidomide is accompanied by decreased CRBN
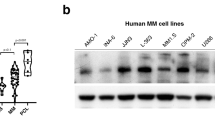
H929 myeloma cells were treated in cell culture with increasing concentrations of lenalidomide (L) or control vehicle DMSO (D) for extended durations to select for resistance to the antiproliferative effects of lenalidomide. CRBN mRNA expression was observed to decrease in cultures exposed continuously (6 months) to lenalidomide 1 μM, and also in cultures sequentially treated with 1 μM (2 months) followed by 10 μM lenalidomide for 4 months (Figure 5a; data for H929 R10-4 cells). CRBN protein was shown to be decreased in our independently generated lenalidomide-resistant H929 cell lines compared with the parental H929 cell line (Figure 5b). All these lenalidomide-resistant H929 cell lines had a 50% CRBN gene copy reduction (data not shown). These CRBN-reduced cell lines showed marked resistance to the antiproliferative effects of lenalidomide (Figure 5c), yet remained sensitive to inhibition of proliferation by pomalidomide, although higher concentrations of compound are required than for parental H929 cells (Figure 5d).
Prolonged exposure of myeloma cells in culture to high-dose lenalidomide induces resistance to antiproliferative effect of lenalidomide correlating with decreases in CRBN. (a) Time course of acquisition of lenalidomide resistance in H929 cells and concurrent reduction in CRBN mRNA determined by reverse transcription--PCR (data for one clone R10-4 is shown, representative of generation of four independent lenalidomide resistant cells lines, H929 R10-1, R10-2, R10-3 and R10-4 ). H929 cells were treated with control (final 0.1% DMSO) (D) or lenalidomide (1 μM) (L1) for 2 months until the proliferation of cells was no longer inhibited by 1 μM lenalidomide. The lenalidomide treated cultures were subsequently treated with 10 μM lenalidomide for a further 4 months to fully establish resistance to high-dose lenalidomide (30 μM). Arbitary units for CRBN mRNA are shown. (b) Immunoblot of CRBN in H929 cells treated with DMSO for 6 months (H929/D1) and H929 lenalidomide-resistant cells lines (R10-1, R 10-2, R 10-3 and R 10-4). (c) Dose-dependent inhibition of proliferation of parental H929 cells (•) and H929/D1 cells grown continuously in 0.1% DMSO (▪) cells by lenalidomide. Lack of inhibition of proliferation by lenalidomide, up to 10 μM concentration, of four H929 cell lines (R10-1, R10-2, R10-3, R10-4; ○, □,∇, ◊) made resistant to high-dose lenalidomide over 6 months in culture. (d) Dose-dependent inhibition of proliferation of parental H929 cells (•) and H929/D1 cells grown continuously in 0.1% DMSO (▪) cells by pomalidomide. Dose-dependent inhibition of proliferation by pomalidomide of four H929 cell lines made resistant to high-dose lenalidomide over 6 months in culture.
Acquired resistance to pomalidomide is accompanied by major decrease of CRBN protein
DF15 myeloma cells sensitive to proliferation inhibition by lenalidomide and pomalidomide (Figure 6a), expressed CRBN protein (Figure 6A, insert). DF15R cells made resistant to antiproliferative effects of pomalidomide and lenalidomide by continuous culture in increasing concentration of pomalidomide (up to100 μM) had minimal detectable CRBN protein (Figure 6A, insert). CRBN was shown to be distributed predominantly in the cytoplasm of DF15 cells (Figure 6B). Consistent with the immunoblot data, DF15 cells showed CRBN immunofluorescence in both the cytoplasm and the nucleus, while minimal CRBN immunofluorescence was observed in DF15R cells (Figure 6B). Preincubation of DF15 myeloma cell extracts with excess lenalidomide (100 μM) prevented CRBN and DDB1 binding to thalidomide analog affinity beads (Figure 6C). Protein extracts from DF15R cells had abundant DDB1 but undetectable CRBN (In) (Figure 6C). Despite the potential for CRBN to be concentrated by thalidomide analog bead binding, as observed in DF15 extracts (Figure 6C; DF15, DMSO lane), no CRBN was observed in bead eluates from DF15R extracts preincubated with DMSO. Although DDB1 was abundant in the DF15R input extract (In), DDB1 did not bind to the affinity beads, confirming the previous observation that binding is dependent on CRBN (Figure 6C).20 We investigated the possibility that CRBN was mutated or CRBN gene copy number was decreased in DF15R cells. There was no evidence of mutation or change in copy number of the CRBN gene in DF15R cells relative to parental DF15 (data not shown).
Comparison of lenalidomide and pomalidomide effects in DF15 and DF15R myeloma cells. (A) Dose-dependent inhibition of proliferation of parental DF15 cells by lenalidomide (•) and pomalidomide (▪). No proliferation inhibition of DF15R cells by lenalidomide (○) or pomalidomide (□). Insert is immunoblot analysis of protein lysates from DF15 and DF15R cells demonstrating minimal CRBN protein in DF15R compared with DF15 cells. (B) CRBN analysis in DF15 and DF15R cells by immunofluorescence confocal microscopy in the absence (panels a) or presence (panels b) of anti-CRBN blocking peptide (Supplemental Figure S2). Images were obtained using a Nikon E800 confocal microscope (Nikon Instruments, Melville, NY, USA) at a 60 × magnification. CRBN immunofluorescence is shown as green color and DAPI blue staining identifies the nucleus of cells. (C) Immunoblot of thalidomide analog affinity bead binding to CRBN in DF15 and DF15R cell extracts. Lane description in order left to right: In=DF15 input before bead purification; DMSO=DF15 extract control (1% DMSO preincubation); Len=DF15 extract preincubated with lenalidomide (100 μM); In=DF15R input before bead purification; DMSO=DF15R control (1% DMSO preincubation); Len=DF15R extract preincubated with lenalidomide (100 μM). Representative immunoblot from two independent experiments with similar results.
Discussion
The immunomodulatory drug lenalidomide has pleiotropic activities in distinct cell types and temporal contexts, which result in direct antitumor effects on cancer cells, inhibition of stromal growth factor support and enhancement of host anticancer immunity.5, 6, 7 This broad range of activities has historically challenged the concept of a single target for these compounds, raising possibilities for either promiscuous interactions with a number of targets, or, as supported by the findings presented here, direct interaction with a specific target that has a central role in orchestrating a range of subsequent cellular events. The observation that CRBN, which is part of an E3 ligase complex with DDB1, is the target for thalidomide-based teratogenicity led us to formally evaluate the role of CRBN as a target for the known clinical activities of lenalidomide and pomalidomide.
Using complementary and independent biophysical methods, we show that in addition to thalidomide, both lenalidomide and pomalidomide bind human CRBN and that these compounds also inhibit the autoubiquitination of CRBN. The binding and expression of CRBN in myeloma cell lines were shown to be functionally linked to well-known clinically relevant cellular activities of these compounds. All observations are consistent with direct interaction between these immunomodulatory compounds and CRBN within the DDB1-containing E3 ligase complex. Notably, elution studies using thalidomide analog beads demonstrated that CRBN binds to the glutarimide moiety of these compounds, but not to the phthalimide moiety. Additionally, inhibition of CRBN autoubiquitination by thalidomide, lenalidomide or pomalidomide was abrogated in a binding defective mutant CRBN (FH-CRBNYW/AA). The functional consequences of the binding of the immunomodulatory compounds to CRBN were investigated in U266 cells in which CRBN had been reduced either 60 or 75% by lentivial transduction. CRBN reduction decreased the antiproliferative potency of both lenalidomide and pomalidomide and significantly prevented compound-mediated induction of the cell cycle progression inhibitor p21WAF-1 and the suppression of IRF4, a gene critical for myeloma cell growth. A similar effect on pomalidomide-induced protein changes was seen in KSM12 myeloma cells, by the presence of the CRBN mutant (FH-CRBNYW/AA).
To determine the role of CRBN in acquired resistance to lenalidomide, H929 resistant cell lines were selected by prolonged exposure to increasing doses of lenalidomide. The final concentration of 10 μM lenalidomide was higher than maximum clinically achievable plasma concentrations of lenalidomide.29 CRBN mRNA expression decreased concurrently with increased antiproliferative resistance to lenalidomide; pomalidomide maintained efficacy, albeit at higher concentrations, in these lenalidomide-resistant cells. The observation of decreased CRBN expression correlating with acquisition of lenalidomide resistance in cells was consistent with published data30 showing a reduction in CRBN mRNA (20–90%) in eight out of nine multiple myeloma patients with clinically-acquired lenalidomide resistance.
Differential potency and resistance of myeloma cells lines to lenalidomide and pomalidomide led us to address whether CRBN binding affinity of these compounds could explain their different spectra of activity. Pomalidomide shows approximately 10-fold higher potency than lenalidomide in a number of cellular systems, activity in lenalidomide-resistant preclinical models31 and also myeloma patients refractory and resistant to lenalidomide show clinical responses to pomalidomide.7, 8, 9 In addition, our results show that reduction of CRBN expression was associated with a greater loss of the antiproliferative potency of lenalidomide than that of pomalidomide. Apparent CRBN-binding affinities of lenalidomide and pomalidomide were similar in myeloma cell lysates and in fluorescent thermal melt assays performed with the recombinant CRBN–DDB1 complexes. In these studies, the cellular context, such as organelle localization (nuclear versus cytoplasmic) or peripheral membrane association, is lost. Such context may alter apparent potency of these compounds against the CRBN complex. In the affinity binding experiments, we coupled the beads through the phthalimide portion and this might affect the interaction of lenalidomide and pomalidomide with the CRBN complex. Indeed, the fact that the potency of lenalidomide is more shifted than that of pomalidomide in CRBN-reduced cells suggests that there may be other proteins that modulate the effects of pomalidomide. The clinical potency of these compounds reflects their cellular potencies where pomalidomide is more potent than lenalidomide, which in turn is more potent than thalidomide. In vivo other aspects including metabolism, distribution and bioavailability may also affect the relative efficacy of these compounds in patients.
Extending beyond roles in multiple myeloma, CRBN was shown to be required for lenalidomide- and pomalidomide-mediated induction of the cytokines, interleukin-2 and tumor necrosis factor-α, in human T cells. Knockdown of CRBN expression by siCRBN treatment of activated T cells resulted in decreased compound-induced cytokines. Inhibition of T cell cytokine production and CRBN binding to thalidomide analog affinity beads showed strong enantiomeric selectivity for S-methyl-pomalidomide over the R isomer. This is consistent with the thesis that binding of immunomodulatory compounds to CRBN is a proximal event in subsequent functional outcomes.
There are some species differences in teratogenicity between thalidomide, lenalidomide and pomalidomide. Thalidomide does not cause limb malformations in rodents but does in rabbits.32 There are reports of other types of developmental defects, for example, vertebral column, rib and eye malformations, when thalidomide was given to pregnant rats.33 Lenalidomide did not have teratogenic effects in rats or rabbits, but produced limb malformations in fetuses of cynomolgus monkeys (lenalidomide food and drug administration product label and Celgene unpublished data). Pomalidomide was teratogenic to both rats and rabbits, with limb malformations observed in rabbits and visceral defects in rats (Celgene, unpublished data). There is very strong conservation of the CRBN sequence between these species and both mouse and human CRBN bind selectively to thalidomide analog affinity beads and binding is competed by thalidomide,20 lenalidomide or pomalidomide. It is possible that there may be differences between rodents, rabbits and primates in the importance of CRBN and/or protein substrates modified by CRBN activity during embryonic development.
Our characterization of CRBN as the target of lenalidomide and pomalidomide, in addition to thalidomide, leaves a number of important questions unanswered. These include the cellular importance of compound-modulation of CRBN autoubiquitination, compound effects on ubiquitination of physiological substrates of the CRBN- E3 ligase, and how these compounds may modify the abundance, localization and activity of CRBN E3 ligase substrate proteins. In addition, we need to understand what other factors influence the cellular and functional differentiation of the antitumor effects of thalidomide, lenalidomide and pomalidomide. Our data linking CRBN expression to response and resistance to immunomodulatory compounds in myeloma cells provide a firm basis for future studies to define the role of the CRBN E3 ligase complex and downstream substrates in the pleiotropic effects of these compounds. Further dissection of the mechanism of action of immunomodulatory compounds at the molecular level, may not only result in discovery of novel antitumor protein targets within the CRBN pathway, but also pave the way for new approaches to other E3 ubiquitin ligase systems as therapeutic targets.
References
Bartlett JB, Dredge K, Dalgleish AG . The evolution of thalidomide and its IMiD derivatives as anticancer agents. Nat Rev Cancer 2004; 4: 314–322.
Teo SK . Properties of thalidomide and its analogues: implications for anticancer therapy. AAPS J 2005; 7: E14–E19.
Davies FE, Raje N, Hideshima T, Lentzsch S, Young G, Tai YT et al. Thalidomide and immunomodulatory derivatives augment natural killer cell cytotoxicity in multiple myeloma. Blood 2001; 98: 210–216.
Dredge K, Marriott JB, Macdonald CD, Man HW, Chen R, Muller GW et al. Novel thalidomide analogues display anti-angiogenic activity independently of immunomodulatory effects. Br J Cancer 2002; 87: 1166–1172.
Zeldis JB, Knight R, Hussein M, Chopra R, Muller G . A review of the history, properties, and use of the immunomodulatory compound lenalidomide. Ann N Y Acad Sci 2011; 1222: 76–82.
Richardson P, Mitsiades C, Lauback J, Schlossman R, Ghobrial I, Hideshima T et al. Lenalidomide in multiple myeloma: an evidence-based review of its role in therapy. Core Evid 2009; 4: 215–245.
Schey S, Ramasamy K . Pomalidomide therapy for myeloma. Expert Opin Investig Drugs 2011; 20: 691–700.
Lacy MQ, Hayman SR, Gertz MA, Dispenzieri A, Buadi F, Kumar S et al. Pomalidomide (CC4047) plus low-dose dexamethasone as therapy for relapsed multiple myeloma. J Clin Oncol 2009; 27: 5008–5014.
Li S, Gill N, Lentzsch S . Recent advances of IMiDs in cancer therapy. Curr Opin Oncol 2010; 22: 579–585.
D’Amato RJ, Loughnan MS, Flynn E, Folkman J . Thalidomide is an inhibitor of angiogenesis. Proc Natl Acad Sci U S A 1994; 91: 4082–4085.
De Luisi A, Ferrucci A, Coluccia AM, Ria R, Moschetta M, de Luca E et al. Lenalidomide restrains motility and overangiogenic potential of bone marrow endothelial cells in patients with active multiple myeloma. Clin Cancer Res 2011; 17: 1935–1946.
Verhelle D, Corral LG, Wong K, Mueller JH, Moutouh-de Parseval L, Jensen-Pergakes K et al. Lenalidomide and CC-4047 inhibit the proliferation of malignant B cells while expanding normal CD34+ progenitor cells. Cancer Res 2007; 6: 746–755.
Escoubet-Lozach L, Lin IL, Jensen-Pergakes K, Brady HA, Gandhi AK, Schafer PH et al. Pomalidomide and lenalidomide induce p21 WAF-1 expression in both lymphoma and multiple myeloma through a LSD1-mediated epigenetic mechanism. Cancer Res 2009; 69: 7347–7356.
Lopez-Girona A, Heintel D, Zhang LH, Mendy D, Gaidarova S, Brady H et al. Lenalidomide downregulates the cell survival factor, interferon regulatory factor-4, providing a potential mechanistic link for predicting response. Br J Haematol 2011; 154: 325–336.
Li S, Pal R, Monaghan SA, Schafer P, Ouyang H, Mapara M et al. IMiD immunomodulatory compounds block C/EBP{beta} translation through eIF4E down-regulation resulting in inhibition of MM. Blood 2011; 117: 5157–5165.
Xu Y, Li J, Ferguson GD, Mercurio F, Khambatta G, Morrison L et al. Immunomodulatory drugs reorganize cytoskeleton by modulating Rho GTPases. Blood 2009; 114: 338–345.
Ramsay AG, Johnson AJ, Lee AM, Gorgun G, Le Dieu R, Blum W et al. Chronic lymphocytic leukemia T cells show impaired immunological synapse formation that can be reversed with an immunomodulating drug. J Clin Invest 2008; 118: 2427–2437.
Gorgun G, Calabrese E, Soydan E, Hideshima T, Perrone G, Bandi M et al. Immunomodulatory effects of lenalidomide and pomalidomide on interaction of tumor and bone marrow accessory cells in multiple myeloma. Blood 2010; 116: 3227–3237.
Lu L, Payvandi F, Wu L, Zhang LH, Hariri RJ, Man HW et al. The anti-cancer drug lenalidomide inhibits angiogenesis and metastasis via multiple inhibitory effects on endothelial cell function in normoxic and hypoxic conditions. Microvasc Res 2009; 77: 78–86.
Ito T, Ando H, Suzuki T, Ogura T, Hotta K, Imamura Y et al. Identification of a primary target of thalidomide teratogenicity. Science 2010; 327: 1345–1350.
Higgins JJ, Tal AL, Sun X, Hauck SC, Hao J, Kosofosky BE et al. Temporal and spatial mouse brain expression of cereblon, an ionic channel regulator involved in human intelligence. J Neurogenet 2004; 24: 18–26.
Higgins JJ, Hao J, Kosofsky BE, Rajadhyaksha AM . Dysregulation of large-conductance Ca2+-activated K+ channel expression in nonsyndromal mental retardation due to a cereblon p.R419X mutation. Neurogenetics 2008; 9: 219–223.
Aizawa M, Abe Y, Ito T, Handa H, Nawa H . mRNA distribution of the thalidomide binding protein cereblon in adult mouse brain. Neurosci Res 2011; 69: 343–347.
Jo S, Lee KH, Song S, Jung YK, Park CS . Identification and functional characterization of cereblon as a binding protein for large-conductance calcium-activated potassium channel in rat brain. J Neurochem 2005; 94: 1212–1224.
Hohberger B, Enz R . Cereblon is expressed in the retina and binds to voltage-gated chloride channels. FEBS Lett 2009; 583: 633–637.
Xin W, Xiaohua N, Peilin C, Xin C, Yaqiong S, Qihan W . Primary function analysis of human mental retardation related gene CRBN. Mol Biol Rep 2008; 35: 251–256.
Lee KM, Jo S, Kim H, Lee J, Park CS . Functional modulation of AMP-activated protein kinase by cereblon. Biochim Biophys Acta 2011; 1813: 448–455.
Pantoliano MW, Petrella EC, Kwasnoski JD, Lobanov VS, Myslik J, Graf E et al. High-density miniaturized thermal shift assays as a general strategy for drug discovery. J Biomol Screen 2001; 6: 429–440.
Chen N, Lau H, Kong L, Kumar G, Zeldis JB, Knight R et al. Pharmacokinetics of lenalidomide in subjects with various degrees of renal impairment and in subjects on hemodialysis. J Clin Pharmacol 2007; 47: 1466–1475.
Zhu YX, Braggio E, Shi CX, Bruins LA, Schmidt JE, Van Wier S et al. Cereblon expression is required for the anti-myeloma activity of lenalidomide and pomalidomide. Blood 2011; 118: 4771–4779.
Rychak E, Mendy D, Miller K, Schafer P, Chopra R, Daniel TO et al. Overcoming resistance; the use of pomalidomide (Pom) and dexamethasone (DEX) in re-sensitizing lenalidomide (len)-resistant multiple myeloma cells. Haematologica 2011; 96: P–328.
Fratta ID, Sigg EB, Maiorana K . Teratogenic effects of thalidomide in rabbits, rats, hamsters and mice. Tox Applied Pharm 1965; 7: 268–280.
Parkhie M, Webb M . Embryotoxicity and teratogenicity of Thalidomide in rats. Teratology 1983; 27: 327–332.
Acknowledgements
We thank John Shaughnessy (University of Arkansas, Little Rock, AR, USA) for the DF15 cell line. We thank Kentaro Hotta (Tokyo Institute of Technology) for his technical support, and also thank colleagues at Celgene who have assisted in this project in particular Helen Brady, Normand Richard, Julia Hui, James Hartke, Laurie LeBrun, Kyle Hughes, Mark Nagy, Veronique Plantevin-Krenitsky, Philip Chamberlin, Flora Huynh, Kirsten Blumeyer and especially George Muller for insightful discussions on the chemistry of these compounds.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
All authors except TI, SK and HH, are, or were, employees of Celgene and all Celgene employees except JFE hold stock options in Celgene.
Additional information
Supplementary Information accompanies the paper on the Leukemia website
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Lopez-Girona, A., Mendy, D., Ito, T. et al. Cereblon is a direct protein target for immunomodulatory and antiproliferative activities of lenalidomide and pomalidomide. Leukemia 26, 2326–2335 (2012). https://doi.org/10.1038/leu.2012.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2012.119
Keywords
This article is cited by
-
G protein-biased LPAR1 agonism of prototypic antidepressants: Implication in the identification of novel therapeutic target for depression
Neuropsychopharmacology (2024)
-
Efficacy and safety of pomalidomide, bortezomib, and dexamethasone combination chemotherapy for newly diagnosed multiple myeloma: POMACE Phase II Study
Blood Cancer Journal (2023)
-
Clinical evidence for immune-based strategies in early-line multiple myeloma: current challenges in decision-making for subsequent therapy
Blood Cancer Journal (2023)
-
SUMOylation inhibition enhances multiple myeloma sensitivity to lenalidomide
Cancer Gene Therapy (2023)
-
Mechanism and therapeutic implications of pomalidomide-induced immune surface marker upregulation in EBV-positive lymphomas
Scientific Reports (2023)