Abstract
Objective
Polycaprolactone (PCL) is a widely applied biomaterial in bone tissue engineering (BTE) due to its superior mechanical properties and biodegradability. However, the high hydrophobicity and low cell adhesion properties of PCL show limited cell interactions. Herein, we prepared the porous PCL/DBP composites with improved cell adhesion through the addition of demineralized bone powder (DBP). Three-dimensional scaffolds were fabricated by mixing various concentrations of DBP with PCL and applying non-solvent-induced phase separation (NIPS) and thermal-induced phase separation (TIPS) (N-TIPS) and solvent casting and particulate leaching (SCPL) to impart porosity.
Methods
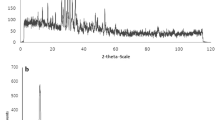
A characteristic evaluation was performed through X-ray diffraction (XRD), morphological analysis, physicochemical analysis, bioactivity test, and mechanical test. Upon culture with mouse bone marrow stem cells (mBMSCs), proliferation and osteogenic differentiation of mBMSC were evaluated using quantitative dsDNA analysis and alkaline phosphatase (ALP) activity, respectively.
Results
The addition of DBP improved the physicochemical and mechanical properties of the scaffold and formed a large amount of hydroxyapatite (HAp). Also, cell proliferation and differentiation were increased by enhancing cell adhesion.
Conclusion
The porous PCL/DBP scaffolds could provide a favorable microenvironment for cell adhesion and be a promising biomaterial model for bone tissue engineering.
Graphical abstract







Similar content being viewed by others
References
Ho-Shui-Ling A, et al. Bone regeneration strategies: engineered scaffolds, bioactive molecules and stem cells current stage and future perspectives. Biomaterials. 2018;180:143–62. https://doi.org/10.1016/j.biomaterials.2018.07.017.
Oryan A, et al. Bone regenerative medicine: classic options, novel strategies, and future directions. J Orthop Surg Res. 2014;9(1):1–27. https://doi.org/10.1186/1749-799X-9-18.
Almubarak S, et al. Tissue engineering strategies for promoting vascularized bone regeneration. Bone. 2016;83:197–209. https://doi.org/10.1016/j.bone.2015.11.011.
Shin SR, Tornetta P III. Donor site morbidity after anterior iliac bone graft harvesting. J Orthop Trauma. 2016;30(6):340–3.
Sohn H-S, Oh J-K. Review of bone graft and bone substitutes with an emphasis on fracture surgeries. Biomater Res. 2019;23(1):1–7. https://doi.org/10.1186/s40824-019-0157-y.
Stratton S, et al. Bioactive polymeric scaffolds for tissue engineering. Bioactive Mater. 2016;1(2):93–108. https://doi.org/10.1016/j.bioactmat.2016.11.001.
Zhang Y, et al. Polymer fiber scaffolds for bone and cartilage tissue engineering. Adv Func Mater. 2019;29(36):1903279. https://doi.org/10.1002/adfm.201903279.
Donnaloja F, et al. Natural and synthetic polymers for bone scaffolds optimization. Polymers. 2020;12(4):905. https://doi.org/10.3390/polym12040905.
Bharadwaz A, Jayasuriya AC. Recent trends in the application of widely used natural and synthetic polymer nanocomposites in bone tissue regeneration. Mater Sci Eng, C. 2020;110:110698. https://doi.org/10.1016/j.msec.2020.110698.
Shao H, et al. Effect of PCL concentration on PCL/CaSiO3 porous composite scaffolds for bone engineering. Ceram Int. 2020;46(9):13082–7. https://doi.org/10.1016/j.ceramint.2020.02.079.
Unagolla JM, Jayasuriya AC. Enhanced cell functions on graphene oxide incorporated 3D printed polycaprolactone scaffolds. Mater Sci Eng, C. 2019;102:1–11. https://doi.org/10.1016/j.msec.2019.04.026.
Huong K-H, Teh C-H, Amirul A. Microbial-based synthesis of highly elastomeric biodegradable poly (3-hydroxybutyrate-co-4-hydroxybutyrate) thermoplastic. Int J Biol Macromol. 2017;101:983–95. https://doi.org/10.1016/j.ijbiomac.2017.03.179.
Dwivedi R, et al. Polycaprolactone as biomaterial for bone scaffolds: review of literature. J Oral biol Craniofacial Res. 2020;10(1):381–8. https://doi.org/10.1016/j.jobcr.2019.10.003.
Thitiset T, et al. Development of collagen/demineralized bone powder scaffolds and periosteum-derived cells for bone tissue engineering application. Int J Mol Sci. 2013;14(1):2056–71. https://doi.org/10.3390/ijms14012056.
Yuan B, et al. In vitro and in vivo study of a novel nanoscale demineralized bone matrix coated PCL/β-TCP scaffold for bone regeneration. Macromol Biosci. 2021;21(3):2000336. https://doi.org/10.1002/mabi.202000336.
Chen I, et al. Preparation and characterization of moldable demineralized bone matrix/calcium sulfate composite bone graft materials. J Function Biomater. 2021;12(4):56. https://doi.org/10.3390/jfb12040056.
Aghdasi B, et al. A review of demineralized bone matrices for spinal fusion: the evidence for efficacy. The Surgeon. 2013;11(1):39–48. https://doi.org/10.1016/j.surge.2012.08.001.
Lee S-Y, et al. The effect of titanium with heparin/BMP-2 complex for improving osteoblast activity. Carbohyd Polym. 2013;98(1):546–54. https://doi.org/10.1016/j.carbpol.2013.05.095.
Russell N, et al. In-vivo performance of seven commercially available demineralized bone matrix fiber and putty products in a rat posterolateral fusion model. Front Surg. 2020;7:10. https://doi.org/10.3389/fsurg.2020.00010.
Dechwongya P, et al. Preparation and characterization of demineralized bone matrix/chitosan composite scaffolds for bone tissue engineering. Chulalongkorn Med J. 2019;63(2):119–26.
Cho HH, et al. Comparative study on the effect of the different harvesting sources of demineralized bone particles on the bone regeneration of a composite gellan gum scaffold for bone tissue engineering applications. ACS Appl Bio Mater. 2021;4(2):1900–11. https://doi.org/10.1021/acsabm.0c01549.
Dadgar N, et al. Bioartificial injectable cartilage implants from demineralized bone matrix/PVA and related studies in rabbit animal model. J Biomater Appl. 2021;35(10):1315–26. https://doi.org/10.1177/0885328220976552.
Jung JT, et al. Understanding the non-solvent induced phase separation (NIPS) effect during the fabrication of microporous PVDF membranes via thermally induced phase separation (TIPS). J Membr Sci. 2016;514:250–63. https://doi.org/10.1016/j.memsci.2016.04.069.
Jin TT, Zhao ZP, Chen KC, Preparation of a poly (vinyl chloride) ultrafiltration membrane through the combination of thermally induced phase separation and non‐solvent‐induced phase separation. Journal of Applied Polymer Science, 2016. 133(5). https://doi.org/10.1002/app.42953
Szustakiewicz K, et al. The influence of hydroxyapatite content on properties of poly (L-lactide)/hydroxyapatite porous scaffolds obtained using thermal induced phase separation technique. Eur Polymer J. 2019;113:313–20. https://doi.org/10.1016/j.eurpolymj.2019.01.073.
Sola A, et al. Development of solvent-casting particulate leaching (SCPL) polymer scaffolds as improved three-dimensional supports to mimic the bone marrow niche. Mater Sci Eng, C. 2019;96:153–65. https://doi.org/10.1016/j.msec.2018.10.086.
Abzan N, et al. Modulation of the mechanical, physical and chemical properties of polyvinylidene fluoride scaffold via non-solvent induced phase separation process for nerve tissue engineering applications. Eur Polymer J. 2018;104:115–27. https://doi.org/10.1016/j.eurpolymj.2018.05.004.
Abbasi N, et al. Porous scaffolds for bone regeneration. J Sci: Adv Mater Device. 2020;5(1):1–9.
Grgurevic L, Pecina M, Vukicevic S, Marshall R. Urist and the discovery of bone morphogenetic proteins. Int Orthop. 2017;41(5):1065–9. https://doi.org/10.1007/s00264-017-3402-9.
Liu S, et al. Fabrication of polycaprolactone nanofibrous scaffolds by facile phase separation approach. Mater Sci Eng, C. 2014;44:201–8. https://doi.org/10.1016/j.msec.2014.08.012.
Yang F, Wolke J, Jansen J. Biomimetic calcium phosphate coating on electrospun poly (ɛ-caprolactone) scaffolds for bone tissue engineering. Chem Eng J. 2008;137(1):154–61. https://doi.org/10.1016/j.cej.2007.07.076.
Meurer SK, et al. Isolation of mature (peritoneum-derived) mast cells and immature (bone marrow-derived) mast cell precursors from mice. PLoS ONE. 2016;11(6):e0158104. https://doi.org/10.1371/journal.pone.0158104.
Dávila J. et al. Fabrication of PCL/β‐TCP scaffolds by 3D mini‐screw extrusion printing. Journal of Applied Polymer Science, 2016. 133(15). https://doi.org/10.1002/app.43031.
Nicoletti A, et al. Incorporation of nanostructured hydroxyapatite and poly (N-isopropylacrylamide) in demineralized bone matrix enhances osteoblast and human mesenchymal stem cell activity. Biointerphases. 2015;10(4):041001. https://doi.org/10.1116/1.4931882.
Dozza B, et al. When size matters: differences in demineralized bone matrix particles affect collagen structure, mesenchymal stem cell behavior, and osteogenic potential. J Biomed Mater Res, Part A. 2017;105(4):1019–33. https://doi.org/10.1002/jbm.a.35975.
Figueiredo M, et al. Influence of hydrochloric acid concentration on the demineralization of cortical bone. Chem Eng Res Des. 2011;89(1):116–24. https://doi.org/10.1016/j.cherd.2010.04.013.
Cheng M-Q, et al. A novel open-porous magnesium scaffold with controllable microstructures and properties for bone regeneration. Sci Rep. 2016;6(1):1–14. https://doi.org/10.1038/srep24134.
Lin T-H, et al. Osteochondral tissue regeneration using a tyramine-modified bilayered PLGA scaffold combined with articular chondrocytes in a porcine model. Int J Mol Sci. 2019;20(2):326. https://doi.org/10.3390/ijms20020326.
Yoon S-J, et al. The cocktail effect of BMP-2 and TGF-β1 loaded in visible light-cured glycol chitosan hydrogels for the enhancement of bone formation in a rat tibial defect model. Mar Drugs. 2018;16(10):351. https://doi.org/10.3390/md16100351.
Zhang K, et al. Effect of microporosity on scaffolds for bone tissue engineering. Regenerative Biomater. 2018;5(2):115–24. https://doi.org/10.1093/rb/rby001.
Sousa I, et al. Collagen surface modified poly (ε-caprolactone) scaffolds with improved hydrophilicity and cell adhesion properties. Mater Lett. 2014;134:263–7. https://doi.org/10.1016/j.matlet.2014.06.132.
Ambekar RS, Kandasubramanian B. Progress in the advancement of porous biopolymer scaffold: tissue engineering application. Ind Eng Chem Res. 2019;58(16):6163–94. https://doi.org/10.1021/acs.iecr.8b05334.
Adachi T, et al. Framework for optimal design of porous scaffold microstructure by computational simulation of bone regeneration. Biomaterials. 2006;27(21):3964–72. https://doi.org/10.1016/j.biomaterials.2006.02.039.
Zhang Q, et al. Characterization of polycaprolactone/collagen fibrous scaffolds by electrospinning and their bioactivity. Int J Biol Macromol. 2015;76:94–101. https://doi.org/10.1016/j.ijbiomac.2015.01.063.
Kang M-H, et al. Biomimetic porous Mg with tunable mechanical properties and biodegradation rates for bone regeneration. Acta Biomater. 2019;84:453–67. https://doi.org/10.1016/j.actbio.2018.11.045.
Chavan PN, et al. Study of nanobiomaterial hydroxyapatite in simulated body fluid: formation and growth of apatite. Mater Sci Eng, B. 2010;168(1–3):224–30. https://doi.org/10.1016/j.mseb.2009.11.012.
Al-Munajjed AA, et al. Development of a biomimetic collagen-hydroxyapatite scaffold for bone tissue engineering using a SBF immersion technique. J Biomed Mater Res Part B: App Biomater: An Off J Soc Biomater, Japanese Soc Biomater Australian Soc Biomater Korean Soc Biomater. 2009;90(2):584–91. https://doi.org/10.1002/jbm.b.31320.
Zhang J, et al. Three-dimensional printing of strontium-containing mesoporous bioactive glass scaffolds for bone regeneration. Acta Biomater. 2014;10(5):2269–81. https://doi.org/10.1016/j.actbio.2014.01.001.
Shahriarpanah S, Nourmohammadi J, Amoabediny G. Fabrication and characterization of carboxylated starch-chitosan bioactive scaffold for bone regeneration. Int J Biol Macromol. 2016;93:1069–78. https://doi.org/10.1016/j.ijbiomac.2016.09.045.
Zhang L-J, et al. Hydroxyapatite/collagen composite materials formation in simulated body fluid environment. Mater Lett. 2004;58(5):719–22. https://doi.org/10.1016/j.matlet.2003.07.009.
Lei X, et al. Comparative evaluation of the physicochemical properties of nano-hydroxyapatite/collagen and natural bone ceramic/collagen scaffolds and their osteogenesis-promoting effect on MC3T3-E1 cells. Regenerative Biomater. 2019;6(6):361–71. https://doi.org/10.1093/rb/rbz026.
Yu L, Wei M. Biomineralization of collagen-based materials for hard tissue repair. Int J Mol Sci. 2021;22(2):944. https://doi.org/10.3390/ijms22020944.
Datta N, et al. Effect of bone extracellular matrix synthesized in vitro on the osteoblastic differentiation of marrow stromal cells. Biomaterials. 2005;26(9):971–7. https://doi.org/10.1016/j.biomaterials.2004.04.001.
Cai Y, et al. Collagen grafted 3D polycaprolactone scaffolds for enhanced cartilage regeneration. J Mater Chem B. 2013;1(43):5971–6. https://doi.org/10.1039/C3TB20680G.
Mauney J, et al. Mechanical stimulation promotes osteogenic differentiation of human bone marrow stromal cells on 3-D partially demineralized bone scaffolds in vitro. Calcif Tissue Int. 2004;74(5):458–68. https://doi.org/10.1007/s00223-003-0104-7.
Mauney JR, et al. Osteogenic differentiation of human bone marrow stromal cells on partially demineralized bone scaffolds in vitro. Tissue Eng. 2004;10(1–2):81–92. https://doi.org/10.1089/107632704322791727.
Tomoaia G, Pasca R-D. On the collagen mineralization. A Rev Clujul Med. 2015;88(1):15. https://doi.org/10.15386/cjmed-359.
Funding
This research was supported by the bilateral cooperation Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2019K2A9A1A06098563).
Author information
Authors and Affiliations
Contributions
S.I.K. and N.E.K. are equally contributed as first author. S.I.K., N.E.K., S.J.P., and J.H.C. designed and conceived the study. S.J.P. helped write the manuscript. Y.G.L. and G.Y.J. fabricated and characterized the material. S.I.K. and N.E.K. performed the in vitro study. J.E.S. and G.K. gave feedback and opinion on the study. G.K. contributed in reagents and materials and supervised overall study.
Corresponding author
Ethics declarations
Consent to participate
All authors agree to their participation in this study.
Consent for publication
All authors approve the publication of the manuscript in its present form.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, S.i., Kim, N.E., Park, S. et al. Characterization of non-solvent- and thermal-induced phase separation applied polycaprolactone/demineralized bone matrix scaffold for bone tissue engineering. In vitro models 1, 197–207 (2022). https://doi.org/10.1007/s44164-022-00018-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s44164-022-00018-9