Abstract
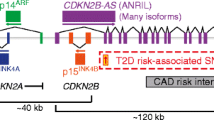
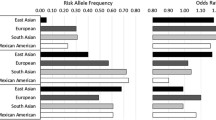
Diabetes Mellitus, being a polygenic disorder, have a set of risk genes involved in the onset of the insulin resistance, obesity and impaired insulin synthesis. Recent genome wide association studies (GWAS) shows the intimacy of CDK5 regulatory subunit Associated protein 1-Like 1 (Cdkal1) with the pathophysiology of the diabetes mellitus and its complications, although the exact molecular relation is still unknown. In this short review, we have summarized all the diverse biological roles of Cdkal1 in relation to the onset of diabetes mellitus. Variations in the Cdkal1 transcript are responsible for the accumulation of misfolded insulin and thus generating oxidative and ER stress in the pancreatic β-cells, leading to their destruction. Recent studies have shown that Cdkal1 has an intrinsic thiomethyl transferase activity, which is essential for proper posttranslational processing of pre-proinsulin to produce mature insulin. Moreover, Cdkal1 has also been claimed as an endogenous inhibitor of cdk5, which prevents the cdk5-induced interruption in insulin synthesis through PDX1 translocation from nucleus to cytosol. Recent clinical studies have identified the risk single nucleotide polymorphisms (SNPs) of Cdkal1 as one of the root causes for the onset of diabetic complications. To the best of our knowledge, it is the first comprehensive review which elaborates most of the potential Cdkal1-dependent molecular mechanisms studied yet. In this review, we present a compiled and concise summary about all the diverse roles of Cdkal1 in the context of type 2 diabetes mellitus and its associated complications. This review will be helpful to target Cdkal1 as a potential option for the management of type 2 diabetes mellitus in future.
Graphical abstract





Similar content being viewed by others
References
Who. c2020. World Health Organization. [Online]. [5 July 2020]. Available from: https://www.who.int/news-room/fact-sheets/detail/diabetes
Gerich JE. Is reduced first-phase insulin release the earliest detectable abnormality in individuals destined to develop type 2 diabetes? Diabetes. 2002;51(suppl 1):S117–21. https://doi.org/10.2337/diabetes.51.2007.S117.
Wei FY, Tomizawa K. tRNA modifications and islet function. Diabetes Obes Metab. 2018 Sep;20:20–7. https://doi.org/10.1111/dom.13405.
Ohara-Imaizumi M, Yoshida M, Aoyagi K, Saito T, Okamura T, Takenaka H, et al. Deletion of CDKAL1 affects mitochondrial ATP generation and first-phase insulin exocytosis. PLoS One. 2010;5(12):e15553. https://doi.org/10.1371/journal.pone.0015553.
Watanabe S, Wei FY, Tomizawa K. Functional characterization of Cdkal1, a risk factor of type 2 diabetes, and the translational opportunities. Drug Discov Today Dis Models. 2013;10(2):e65–9. https://doi.org/10.1016/j.ddmod.2012.12.001.
Groenewoud MJ, Dekker JM, Fritsche A, Reiling E, Nijpels G, Heine RJ, et al. Variants of CDKAL1 and IGF2BP2 affect first-phase insulin secretion during hyperglycaemic clamps. Diabetologia. 2008;51(9):1659–63. https://doi.org/10.1007/s00125-008-1083-z.
Yonghong L, Wilson L, Monica C, Steven JS, Nam B, Joseph JC, et al. Further genetic evidence for three psoriasis-risk genes: ADAM33, CDKAL1, and PTPN22. J Invest Dermatol. 2009;129(3):629–34. https://doi.org/10.1038/jid.2008.297.
Nan L, Junfen M, Kai L, Changlong G, Liang M. Different contributions of CDKAL 1, KIF21B, and LRRK2/MUC19 polymorphisms to SAPHO syndrome, rheumatoid arthritis, Ankylosing spondylitis, and Seronegative Spondyloarthropathy. Genet Test Mol Biomarkers. 2017;21(2):122–6. https://doi.org/10.1089/gtmb.2016.0112.
Nikhil K, Sharan S, Chakraborty A, Roy P. Pterostilbene-isothiocyanate conjugate suppresses growth of prostate cancer cells irrespective of androgen receptor status. PLoS One. 2014;9(4):e93335. https://doi.org/10.1371/journal.pone.0093335.
Varshney R, Gupta S, Roy P. Cytoprotective effect of kaempferol against palmitic acid-induced pancreatic β-cell death through modulation of autophagy via AMPK/mTOR signaling pathway. Mol Cell Endocrinol. 2017;15(448):1–20. https://doi.org/10.1016/j.mce.2017.02.033.
Varshney R, Mishra R, Das N, Sircar D, Roy P. A comparative analysis of various flavonoids in the regulation of obesity and diabetes: an in vitro and in vivo study. J Funct Foods. 2019 Aug;1(59):194–205. https://doi.org/10.1016/j.jff.2019.05.004.
Arragain S, Handelman SK, Forouhar F, Wei FY, Tomizawa K, Hunt JF, et al. Identification of eukaryotic and prokaryotic methylthiotransferase for biosynthesis of 2-methylthio-N6-threonylcarbamoyladenosine in tRNA. J Biol Chem. 2010;285(37):28425–33. https://doi.org/10.1074/jbc.m110.106831.
Wang H, Wei L, Li C, Zhou J, Li Z. CDK5RAP1 deficiency induces cell cycle arrest and apoptosis in human breast cancer cell line by the ROS/JNK signaling pathway. Oncol Rep. 2015;33(3):1089–96. https://doi.org/10.3892/or.2015.3736.
Ubeda M, Rukstalis JM, Habener JF. Inhibition of cyclin-dependent kinase 5 activity protects pancreatic beta cells from glucotoxicity. J Biol Chem. 2006;281(39):28858–64. https://doi.org/10.1074/jbc.m604690200.
Wei FY, Nagashima K, Ohshima T, Saheki Y, Lu YF, Matsushita M, et al. Cdk5-dependent regulation of glucose-stimulated insulin secretion. Nat Med. 2005;11(10):1104–8. https://doi.org/10.1038/nm1299.
Suzuki K, Hata S, Kawabata Y, Sorimachi H. Structure, activation, and biology of calpain. Diabetes. 2004;53(suppl 1):S12–8. https://doi.org/10.2337/diabetes.53.2007.s12.
Ong SB, Lee WH, Shao NY, Ismail NI, Katwadi K, Lim MM, et al. Calpain inhibition restores autophagy and prevents mitochondrial fragmentation in a human iPSC model of diabetic endotheliopathy. Stem Cell Reports. 2019;12(3):597–610. https://doi.org/10.1016/j.stemcr.2019.01.017.
Ahmed D, Sharma M. Cyclin-dependent kinase 5/p35/p39: a novel and imminent therapeutic target for diabetes mellitus. Int. J Endocrinol. 2011. https://doi.org/10.1155/2011/530274.
Johnson AD. Single-nucleotide polymorphism bioinformatics: a comprehensive review of resources. Circ Cardiovasc Genet. 2009;2(5):530–6. https://doi.org/10.1161/2FCIRCGENETICS.109.872010.
Bethesda MD SNP FAQ Archive: National Center for Biotechnology Information (US).
Rung J, Cauchi S, Albrechtsen A, Shen L, Rocheleau G, Cavalcanti-Proença C, et al. Genetic variant near IRS1 is associated with type 2 diabetes, insulin resistance and hyperinsulinemia. Nat Genet. 2009 Oct;41(10):1110. https://doi.org/10.1038/ng.443.
Zeggini E, Scott LJ, Saxena R, Voight BF, Marchini JL, Hu T, et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet. 2008;40(5):638–45. https://doi.org/10.1038/ng.120.
Lasram K, Ben Halim N, Benrahma H, Mediene Benchekor S, Arfa I, Hsouna S, et al. Contribution of CDKAL1 rs7756992 and IGF2BP2 rs4402960 polymorphisms in type 2 diabetes, diabetic complications, obesity risk and hypertension in the T unisian population. J Diabetes. 2015 Jan;7(1):102–13. https://doi.org/10.1111/1753-0407.12147.
Saxena R, Voight BF, Lyssenko V, Burtt NP, de Bakker PI, Chen H, et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science. 2007;316(5829):1331–6. https://doi.org/10.1126/science.1142358.
Wellcome Trust Case Control Consortium. Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature. 2007;447(7145):661. https://doi.org/10.1038/nature05911.
Zhou B, Wei FY, Kanai N, Fujimura A, Kaitsuka T, Tomizawa K. Identification of a splicing variant that regulates type 2 diabetes risk factor CDKAL1 level by a coding-independent mechanism in human. Hum Mol Genet. 2014;23(17):4639–50. https://doi.org/10.1093/hmg/ddu184.
Wei FY, Tomizawa K. Functional loss of Cdkal1, a novel tRNA modification enzyme, causes the development of type 2 diabetes. Endocr J .2011: 1109050614-1109050614; https://doi.org/10.1507/endocrj.ej11-0099.
Steiner DF, Park SY, Støy J, Philipson LH, Bell GI. A brief perspective on insulin production. Diabetes Obes Metab. 2009;11:189–96. https://doi.org/10.1111/j.1463-1326.2009.01106.x.
Støy J, Steiner DF, Park SY, Ye H, Philipson LH, Bell GI. Clinical and molecular genetics of neonatal diabetes due to mutations in the insulin gene. Rev Endocr Metab Disord. 2010;11(3):205–15. https://doi.org/10.1007/11154-010-9151-3.
Brambillasca S, Altkrueger A, Colombo SF, Friederich A, Eickelmann P, Mark M, et al. CDK5 regulatory subunit-associated protein 1-like 1 (CDKAL1) is a tail-anchored protein in the endoplasmic reticulum (ER) of insulinoma cells. J Biol Chem. 2012;287(50):41808–19. https://doi.org/10.1074/jbc.m112.376558.
Okamura T, Yanobu-Takanashi R, Takeuchi F, Isono M, Akiyama K, Shimizu Y, et al. Deletion of CDKAL1 affects high-fat diet–induced fat accumulation and glucose-stimulated insulin secretion in mice, indicating relevance to diabetes. PLoS One. 2012;7(11):e49055. https://doi.org/10.1371/journal.pone.0049055.
Back SH, Scheuner D, Han J, Song B, Ribick M, Wang J, et al. Translation attenuation through eIF2α phosphorylation prevents oxidative stress and maintains the differentiated state in β cells. Cell Metab. 2009;10(1):13–26. https://doi.org/10.1016/j.cmet.2009.06.002.
Frakes AE, Dillin A. The UPRER: sensor and coordinator of organismal homeostasis. Mol Cell. 2017;66(6):761–71. https://doi.org/10.1016/j.molcel.2017.05.031.
Sun J, Cui J, He Q, Chen Z, Arvan P, Liu M. Proinsulin misfolding and endoplasmic reticulum stress during the development and progression of diabetes☆. Mol Asp Med. 2015;1(42):105–18. https://doi.org/10.1016/j.mam.2015.01.001.
Hasnain SZ, Prins JB, McGuckin MA. Oxidative and endoplasmic reticulum stress in b-cell dysfunction in diabetes. J Mol Endocrinol. 2016;56(2):33–54. https://doi.org/10.1530/jme-15-0232.
Dos S, Maria CF, Cole PA, Susanne N, Kimberly BZ, Steven JR, et al. Irp2 regulates insulin production through iron-mediated Cdkal1-catalyzed tRNA modification. Nat Commun. 2020;11(1):1–16. https://doi.org/10.1038/s41467-019-14004-5.
Fan-Yan W, Kazuhito T. Development of type 2 diabetes caused by a deficiency of a tRNAlys modification. Islets. 2012;4(1):71–3. https://doi.org/10.4161/isl.18262.
Randal JK. Beta-cell failure, stress, and type 2 diabetes. N Engl J Med. 2011;365(20):1931–3. https://doi.org/10.1056/NEJMcibr1109442.
Zeng H, Guo M, Zhou T, Tan L, Chong CN, Zhang T, et al. An isogenic human ESC platform for functional evaluation of genome-wide-association-study-identified diabetes genes and drug discovery. Cell Stem Cell. 2016;19(3):326–40. https://doi.org/10.1016/j.stem.2016.07.002.
Guo M, Zhang T, Dong X, Xiang JZ, Lei M, Evans T, et al. Using hESCs to probe the interaction of the diabetes-associated genes CDKAL1 and MT1E. Cell Rep. 2017;19(8):1512–21. https://doi.org/10.1016/j.celrep.2017.04.070.
Dehwah MA, Wang M, Huang QY. CDKAL1 and type 2 diabetes: a global meta-analysis. Genet Mol Res. 2010;9(2):1109–20. https://doi.org/10.4238/vol9-2gmr802.
Desai BM, Oliver-Krasinski J, De Leon DD, Farzad C, Hong N, Leach SD, et al. Preexisting pancreatic acinar cells contribute to acinar cell, but not islet β cell, regeneration. J Clin Invest. 2007;117(4):971–7. https://doi.org/10.1172/jci29988.
Xiao X, Chen Z, Shiota C, Prasadan K, Guo P, El-Gohary Y, et al. No evidence for β cell neogenesis in murine adult pancreas. J Clin Invest. 2013;123(5):2207–17. https://doi.org/10.1172/jci66323.
Liu KC, Leuckx G, Sakano D, Seymour PA, Mattsson CL, Rautio L, et al. Inhibition of Cdk5 promotes β-cell differentiation from ductal progenitors. Diabetes. 2018;67(1):58–70. https://doi.org/10.2337/db16-1587.
Mehmet ZK, Gulali A, Edip E, Ozgur MY, Tuba TD, Burcin MA, Haluk S. Neuregulin-4 is associated with plasma glucose and increased risk of type 2 diabetes mellitus. Swiss Med Wkly. 2019; 149, no. 4344; https://doi.org/10.4414/smw.2019.20139
Mehmet ZK, Gulali A, Burcin MA, Tuba TD, Ozgur MY, Edip E, et al. Is Neuregulin-4 a predictive marker of microvascular complications in type 2 diabetes mellitus? Eur J Clin Investig. 2020;50(3):e13206. https://doi.org/10.1111/eci.13206.
Gulali A, Aytekin A, Mehmet T, Serkan O, Mehmet FO, Haluk S, et al. Diabetes mellitus increases plasma CARDIOTHROPHIN-1 levels independently of heart failure and hypertension. 2013.
Tuba TD, Gulali A, Burcin MA, Mehmet ZK, Edip E, Haluk S. Neutrophil to lymphocyte ratio as an indicative of diabetic control level in type 2 diabetes mellitus. Afr Health Sci. 2019;19(1):1602–6. https://doi.org/10.4314/ahs.v19i1.35.
Gulali A, Mehmet ZK, Tuba TD, Edip E, Burcin MA, Mustafa S, et al. Mean platelet volume (MPV) as an inflammatory marker in type 2 diabetes mellitus and obesity. Bali Med J. 2018;7(3):650–3. https://doi.org/10.15562/bmj.v7i3.806.
Pinar S, Brendon S, Paola L, Claudio L, Marco S, Roberto P, et al. Inflammation and frailty in the elderly: a systematic review and meta-analysis. Ageing Res Rev. 2016;31:1–8. https://doi.org/10.1016/j.arr.2016.08.006.
Satilmis B, Gulali A, Ozge K, Burcin MA, Tuba TD. Edmonton frail score is associated with diabetic control in elderly type 2 diabetic subjects. J Diabetes Metab. 2020;19(1):511. https://doi.org/10.1007/2Fs40200-020-00542-z.
Bilgin S, Aktas G, Kahveci G, Atak MB, Kurtkulagi O, Duman TT. Does mean platelet volume/lymphocyte count ratio associate with frailty in type 2 diabetes mellitus? Bratisl Lek Listy. 2021;122(2):116–9. https://doi.org/10.4149/bll_2021_017.
Mehmet ZK, Gulali A, Edip E, Tuba TD, Burcin MA, Haluk S. Mean platelet volume to lymphocyte ratio as a novel marker for diabetic nephropathy. J Coll Physicians Surg Pak. 2018;28(11):844–7.
Mehmat ZK, Gulali A, Edip E, Isa S, Burcin MA, Tuba TD. Serum uric acid to HDL-cholesterol ratio is a strong predictor of metabolic syndrome in type 2 diabetes mellitus. Rev Assoc Med Bras. 2019;65:9–15. https://doi.org/10.1590/1806-9282.65.1.9.
Jeong-Ah S, Jin-Hee L, Sun-Young L, Hee-Sung H, Hyuk-Sang K, Yong-Moon P, et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig. 2013;4(4):334–43. https://doi.org/10.1111/jdi.12075.
Gulali A, Mehmet ZK, Satilmis B, Burcin MA, Tuba TD, Ozge K. Uric acid to HDL cholesterol ratio is a strong predictor of diabetic control in men with type 2 diabetes mellitus. The Aging Male. 2020;23(5):1098–102. https://doi.org/10.1080/13685538.2019.1678126.
Mehmet ZK, Gulali A, Tuba TD, Burcin MA, Haluk S. Is uric acid elevation a random finding or a causative agent of diabetic nephropathy? Rev Assoc Med Bras. 2019;65:1155–60. https://doi.org/10.1590/1806-9282.65.9.1156.
Aktas G, Alcelik A, Ozlu MT, Tekce BK, Savli H, Tekce H, et al. Association between omentin levels and insulin resistance in pregnancy. Exp Clin Endocrinol Diabetes. 2014;122(03):163–6. https://doi.org/10.1055/s-0034-1370917.
Mohan RD, Sridevi D, Samuel P, Ishwarlal J. Increased toll-like receptor (TLR) activation and TLR ligands in recently diagnosed type 2 diabetic subjects. Diabetes Care. 2010;33(4):861–8. https://doi.org/10.2337/dc09-1799.
Husam G, Priya M, Rupali D, Ching LS, Kelly K, Sanaa A, et al. Acute modulation of toll-like receptors by insulin. Diabetes Care. 2008;31(9):1827–31. https://doi.org/10.2337/dc08-0561.
Xiao-Ming M, Hao L, Xiao-Jun T, Guo-Ping Y, Qian L, Shu-Kui W. Independent anti-inflammatory effect of insulin in newly diagnosed type 2 diabetes. Diabetes Metab Res Rev. 2009;25(5):435–41. https://doi.org/10.1002/dmrr.968.
Take K, Waki H, Sun W, Wada T, Yu J, Nakamura M, et al. CDK5 regulatory subunit-associated protein 1-like 1 negatively regulates adipocyte differentiation through activation of Wnt signaling pathway. Sci Rep. 2017;7(1):1–1. https://doi.org/10.1038/s41598-017-06469-5.
Xie P, Wei FY, Hirata S, Kaitsuka T, Suzuki T, Suzuki T, et al. Quantitative PCR measurement of tRNA 2-methylthio modification for assessing type 2 diabetes risk. Clin Chem. 2013;59(11):1604–12. https://doi.org/10.1373/clinchem.2013.210401.
Choi JH, Banks AS, Estall JL, Kajimura S, Boström P, Laznik D, et al. Anti-diabetic drugs inhibit obesity-linked phosphorylation of PPARγ by Cdk5. Nature. 2010;466(7305):451–6. https://doi.org/10.1038/nature09291.
Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes. 2011;29(3):116–22. https://doi.org/10.2337/diaclin.26.2.77.
Vithian K, Hurel S. Microvascular complications: pathophysiology and management. Clin Med (Lond). 2010;10(5):505. https://doi.org/10.7861/clinmedicine.10-5-505.
Chen G, Xu Y, Lin Y, Lai X, Yao J, Huang B, et al. Association study of genetic variants of 17 diabetes-related genes/loci and cardiovascular risk and diabetic nephropathy in the Chinese she population (中国畲族人群 17 个糖尿病相关基因位点的遗传变异与心血管风险和糖尿病肾病的相关性). J Diabetes. 2013;5(2):136–45. https://doi.org/10.1111/1753-0407.12025.
Liu NJ, Xiong Q, Wu HH, Li YL, Yang Z, Tao XM, et al. The association analysis polymorphism of CDKAL1 and diabetic retinopathy in Chinese Han population. Int J Ophthalmol. 2016;9(5):707. https://doi.org/10.18240/ijo.2016.05.12.
Peng D, Wang J, Zhang R, Jiang F, Tam CH, Jiang G, et al. CDKAL1 rs7756992 is associated with diabetic retinopathy in a Chinese population with type 2 diabetes. Sci Rep. 2017;7(1):1–7. https://doi.org/10.1038/s41598-017-09010-w.
Pablo Y, José DL, Emilio A, Aylén S, Ana LG, Claudio PJ, et al. The rs4712527 Polymorphism in the CDKAL1 Gene: A Protective Factor for Proliferative Diabetic Retinopathy Progress in Type 2 Diabetes. J Vitreoretin Dis. 2018;2(4):200–7. https://doi.org/10.1177/2F2474126418777405.
Nai-Jia L, Qian X, Hui-Hui W, Yan-Liang L, Zhen Y, Xiao-Ming T, et al. The association analysis polymorphism of CDKAL1 and diabetic retinopathy in Chinese Han population. Int J Ophthalmol. 2016;9(5):707. https://doi.org/10.18240/2Fijo.2016.05.12.
Yanni T, Jing X, Ting H, Jiaqi C, Wei Z, Wei S, et al. A novel polymorphism (rs35612982) in CDKAL1 is a risk factor of type 2 diabetes: a case-control study. Kidney Blood Press Res. 2019;44(6):1313–26. https://doi.org/10.1159/000503175.
Lu J, Luo Y, Wang J, Hu C, Zhang R, Wang C, et al. Association of type 2 diabetes susceptibility loci with peripheral nerve function in a Chinese population with diabetes. J Diabetes Investig. 2017 Jan;8(1):115–20. https://doi.org/10.1111/jdi.12546.
Prabodha LB, Sirisena ND, Dissanayake VH. Susceptible and prognostic genetic factors associated with diabetic peripheral neuropathy: a comprehensive literature review. Int J Endocrinol 2018 15; https://doi.org/10.1155/2018/8641942.
Pascoe L, Tura A, Patel SK, Ibrahim IM, Ferrannini E, Zeggini E, et al. Common variants of the novel type 2 diabetes genes CDKAL1 and HHEX/IDE are associated with decreased pancreatic β-cell function. Diabetes. 2007;56(12):3101–4. https://doi.org/10.2337/db07-0634.
Shigi N. Sulfur modifications in tRNA: function and implications for human disease. In: Modified nucleic acids in biology and medicine. Cham: Springer; 2016. p. 55–71. https://doi.org/10.1007/978-3-319-34175-0_3.
Locke JM, Wei FY, Tomizawa K, Weedon MN, Harries LW. A cautionary tale: the non-causal association between type 2 diabetes risk SNP, rs7756992, and levels of non-coding RNA, CDKAL1-v1. Diabetologia. 2015;58(4):745–8. https://doi.org/10.1007/s00125-015-3508-9.
Herder C, Rathmann W, Strassburger K, Finner H, Grallert H, Huth C, et al. Variants of the PPARG, IGF2BP2, CDKAL1, HHEX, and TCF7L2 genes confer risk of type 2 diabetes independently of BMI in the German KORA studies. Horm Metab Res. 2008;40(10):722–6. https://doi.org/10.1055/s-2008-1078730.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
All the authors have contributed in the following manner: CG, ND and TK made the substantial contribution in conceptualizing, designing and writing the article; SS, DS and PR drafted the article and revised it for critically important intellectual contents; and finally, PR approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ghosh, C., Das, N., Saha, S. et al. Involvement of Cdkal1 in the etiology of type 2 diabetes mellitus and microvascular diabetic complications: a review. J Diabetes Metab Disord 21, 991–1001 (2022). https://doi.org/10.1007/s40200-021-00953-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-021-00953-6