Abstract
Background
In this work, we aimed to identify molecular epidermal growth factor receptor (EGFR) tissue biomarkers in patients with ovarian cancer who were treated within the phase III randomized European Organisation for Research and Treatment of Cancer-Gynaecological Cancer Group (EORTC-GCG) 55041 study comparing erlotinib with observation in patients with no evidence of disease progression after first-line platinum-based chemotherapy.
Methods
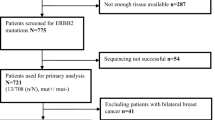
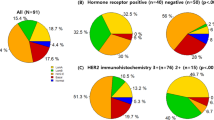
Somatic mutations in KRAS, BRAF, NRAS, PIK3CA, EGFR, and PTEN were determined in 318 (38 %) and expression of EGFR, pAkt, pMAPK, E-cadherin and Vimentin, and EGFR and HER2 gene copy numbers in 218 (26 %) of a total of 835 randomized patients. Biomarker data were correlated with progression-free survival (PFS) and overall survival (OS).
Results
Only 28 mutations were observed among KRAS, BRAF, NRAS, PIK3CA, EGFR, and PTEN (in 7.5 % of patients), of which the most frequent were in KRAS and PIK3CA. EGFR mutations occurred in only three patients. When all mutations were pooled, patients with at least one mutation in KRAS, NRAS, BRAF, PIK3CA, or EGFR had longer PFS (33.1 versus 12.3 months; HR 0.57; 95 % CI 0.33 to 0.99; P = 0.042) compared to those with wild-type tumors. EGFR overexpression was detected in 93 of 218 patients (42.7 %), and 66 of 180 patients (36.7 %) had EGFR gene amplification or high levels of copy number gain. Fifty-eight of 128 patients had positive pMAPK expression (45.3 %), which was associated with inferior OS (38.9 versus 67.0 months; HR 1.81; 95 % CI 1.11 to 2.97; P = 0.016). Patients with positive EGFR fluorescence in situ hybridization (FISH) status had worse OS (46.1 months) than those with negative status (67.0 months; HR 1.56; 95 % CI 1.01 to 2.40; P = 0.044) and shorter PFS (9.6 versus 16.1 months; HR 1.57; 95 % CI 1.11 to 2.22; P = 0.010). None of the investigated biomarkers correlated with responsiveness to erlotinib.
Conclusions
In this phase III study, increased EGFR gene copy number was associated with worse OS and PFS in patients with ovarian cancer. It remains to be determined whether this association is purely prognostic or is also predictive.




Similar content being viewed by others
References
Ciardiello F, Tortora G (2008) EGFR antagonists in cancer treatment. N Engl J Med 358(11):1160–74. doi:10.1056/NEJMra0707704
Yarden Y, Sliwkowski MX (2001) Untangling the ErbB signalling network. Nat Rev Mol Cell Biol 2(2):127–37
Skirnisdóttir I, Sorbe B, Seidal T (2001) The growth factor receptors HER-2/neu and EGFR, their relationship, and their effects on the prognosis in early stage (FIGO I-II) epithelial ovarian carcinoma. Int J Gynecol Cancer 11(2):119–29
Fischer-Colbrie J, Witt A, Heinzl H, Speiser P, Czerwenka K, Sevelda P, Zeillinger R (1997) EGFR and steroid receptors in ovarian carcinoma: comparison with prognostic parameters and outcome of patients. Anticancer Res 17(1B):613–9
Berchuck A, Rodriguez GC, Kamel A, Dodge RK, Soper JT, Clarke-Pearson DL, Bast RC Jr (1991) Epidermal growth factor receptor expression in normal ovarian epithelium and ovarian cancer. I. Correlation of receptor expression with prognostic factors in patients with ovarian cancer. Am J Obstet Gynecol 164(2):669–74
Baekelandt M, Kristensen GB, Tropé CG, Nesland JM, Holm R (1999) Epidermal growth factor receptor expression has no independent prognostic significance in advanced ovarian cancer. Anticancer Res 19(5C):4469–74
Elie C, Geay JF, Morcos M, Le Tourneau A, Girre V, Broët P, Marmey B, Chauvenet L, Audouin J, Pujade-Lauraine E, Camilleri-Broët S, GINECO Group (2004) Lack of relationship between EGFR-1 immunohistochemical expression and prognosis in a multicentre clinical trial of 93 patients with advanced primary ovarian epithelial cancer (GINECO group). Br J Cancer 91(3):470–5
Gordon AN, Finkler N, Edwards RP, Garcia AA, Crozier M, Irwin DH, Barrett E (2005) Efficacy and safety of erlotinib HCl, an epidermal growth factor receptor (HER1/EGFR) tyrosine kinase inhibitor, in patients with advanced ovarian carcinoma: results from a phase II multicenter study. Int J Gynecol Cancer 15(5):785–92
Blank SV, Christos P, Curtin JP, Goldman N, Runowicz CD, Sparano JA, Liebes L, Chen HX, Muggia FM (2010) Erlotinib added to carboplatin and paclitaxel as first-line treatment of ovarian cancer: a phase II study based on surgical reassessment. Gynecol Oncol 119(3):451–6. doi:10.1016/j.ygyno.2010.08.008
Hirte H, Oza A, Swenerton K, Ellard SL, Grimshaw R, Fisher B, Tsao M, Seymour L (2010) A phase II study of erlotinib (OSI-774) given in combination with carboplatin in patients with recurrent epithelial ovarian cancer (NCIC CTG IND.149). Gynecol Oncol 118(3):308–12. doi:10.1016/j.ygyno.2010.05.005
Schilder RJ, Sill MW, Chen X, Darcy KM, Decesare SL, Lewandowski G, Lee RB, Arciero CA, Wu H, Godwin AK (2005) Phase II study of gefitinib in patients with relapsed or persistent ovarian or primary peritoneal carcinoma and evaluation of epidermal growth factor receptor mutations and immunohistochemical expression: a Gynecologic Oncology Group Study. Clin Cancer Res 11(15):5539–48
Posadas EM, Liel MS, Kwitkowski V, Minasian L, Godwin AK, Hussain MM, Espina V, Wood BJ, Steinberg SM, Kohn EC (2007) A phase II and pharmacodynamic study of gefitinib in patients with refractory or recurrent epithelial ovarian cancer. Cancer 109(7):1323–30
Wagner U, du Bois A, Pfisterer J, Huober J, Loibl S, Lück HJ, Sehouli J, Gropp M, Stähle A, Schmalfeldt B, Meier W, Jackisch C, AGO Ovarian Cancer Study Group (2007) Gefitinib in combination with tamoxifen in patients with ovarian cancer refractory or resistant to platinum-taxane based therapy–a phase II trial of the AGO Ovarian Cancer Study Group (AGO-OVAR 2.6). Gynecol Oncol 105(1):132–7
Pautier P, Joly F, Kerbrat P, Bougnoux P, Fumoleau P, Petit T, Rixe O, Ringeisen F, Carrasco AT, Lhommé C (2010) Phase II study of gefitinib in combination with paclitaxel (P) and carboplatin (C) as second-line therapy for ovarian, tubal or peritoneal adenocarcinoma (1839IL/0074). Gynecol Oncol 116(2):157–62. doi:10.1016/j.ygyno.2009.10.076
Schilder RJ, Pathak HB, Lokshin AE, Holloway RW, Alvarez RD, Aghajanian C, Min H, Devarajan K, Ross E, Drescher CW, Godwin AK (2009) Phase II trial of single agent cetuximab in patients with persistent or recurrent epithelial ovarian or primary peritoneal carcinoma with the potential for dose escalation to rash. Gynecol Oncol 113(1):21–7. doi:10.1016/j.ygyno.2008.12.003
Secord AA, Blessing JA, Armstrong DK, Rodgers WH, Miner Z, Barnes MN, Lewandowski G, Mannel RS, Gynecologic Oncology Group (2008) Phase II trial of cetuximab and carboplatin in relapsed platinum-sensitive ovarian cancer and evaluation of epidermal growth factor receptor expression: a Gynecologic Oncology Group study. Gynecol Oncol 108(3):493–9. doi:10.1016/j.ygyno.2007.11.029
Cannistra SA (2004) Cancer of the ovary. N Engl J Med 351(24):2519–29
Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ (2002) Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a meta-analysis. J Clin Oncol 20(5):1248–59
Cappuzzo F, Hirsch FR, Rossi E, Bartolini S, Ceresoli GL, Bemis L, Haney J, Witta S, Danenberg K, Domenichini I, Ludovini V, Magrini E, Gregorc V, Doglioni C, Sidoni A, Tonato M, Franklin WA, Crino L, Bunn PA Jr, Varella-Garcia M (2005) Epidermal growth factor receptor gene and protein and gefitinib sensitivity in non-small-cell lung cancer. J Natl Cancer Inst 97(9):643–55
Hirsch FR, Varella-Garcia M, McCoy J, West H, Xavier AC, Gumerlock P, Bunn PA Jr, Franklin WA, Crowley J, Gandara DR, Southwest Oncology Group (2005) Increased epidermal growth factor receptor gene copy number detected by fluorescence in situ hybridization associates with increased sensitivity to gefitinib in patients with bronchioloalveolar carcinoma subtypes: a Southwest Oncology Group Study. J Clin Oncol 23(28):6838–45
Chung KY, Shia J, Kemeny NE, Shah M, Schwartz GK, Tse A, Hamilton A, Pan D, Schrag D, Schwartz L, Klimstra DS, Fridman D, Kelsen DP, Saltz LB (2005) Cetuximab shows activity in colorectal cancer patients with tumors that do not express the epidermal growth factor receptor by immunohistochemistry. J Clin Oncol 23(9):1803–10
Paez JG, Jänne PA, Lee JC, Tracy S, Greulich H, Gabriel S, Herman P, Kaye FJ, Lindeman N, Boggon TJ, Naoki K, Sasaki H, Fujii Y, Eck MJ, Sellers WR, Johnson BE, Meyerson M (2004) EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science 304(5676):1497–500
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA (2004) Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med 350(21):2129–39
Pao W, Miller V, Zakowski M, Doherty J, Politi K, Sarkaria I, Singh B, Heelan R, Rusch V, Fulton L, Mardis E, Kupfer D, Wilson R, Kris M, Varmus H (2004) EGF receptor gene mutations are common in lung cancers from "never smokers" and are associated with sensitivity of tumors to gefitinib and erlotinib. Proc Natl Acad Sci U S A 101(36):13306–11
Hirsch FR, Varella-Garcia M, Bunn PA Jr, Di Maria MV, Veve R, Bremmes RM, Barón AE, Zeng C, Franklin WA (2003) Epidermal growth factor receptor in non-small-cell lung carcinomas: correlation between gene copy number and protein expression and impact on prognosis. J Clin Oncol 21(20):3798–807
Moroni M, Veronese S, Benvenuti S, Marrapese G, Sartore-Bianchi A, Di Nicolantonio F, Gambacorta M, Siena S, Bardelli A (2005) Gene copy number for epidermal growth factor receptor (EGFR) and clinical response to antiEGFR treatment in colorectal cancer: a cohort study. Lancet Oncol 6(5):279–86
Cappuzzo F, Finocchiaro G, Rossi E, Jänne PA, Carnaghi C, Calandri C, Bencardino K, Ligorio C, Ciardiello F, Pressiani T, Destro A, Roncalli M, Crino L, Franklin WA, Santoro A, Varella-Garcia M (2008) EGFR FISH assay predicts for response to cetuximab in chemotherapy refractory colorectal cancer patients. Ann Oncol 19(4):717–23
Sartore-Bianchi A, Moroni M, Veronese S, Carnaghi C, Bajetta E, Luppi G, Sobrero A, Barone C, Cascinu S, Colucci G, Cortesi E, Nichelatti M, Gambacorta M, Siena S (2007) Epidermal growth factor receptor gene copy number and clinical outcome of metastatic colorectal cancer treated with panitumumab. J Clin Oncol 25(22):3238–45
Di Nicolantonio F, Martini M, Molinari F, Sartore-Bianchi A, Arena S, Saletti P, De Dosso S, Mazzucchelli L, Frattini M, Siena S, Bardelli A (2008) Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol 26(35):5705–12. doi:10.1200/JCO.2008.18.0786
Frattini M, Saletti P, Romagnani E, Martin V, Molinari F, Ghisletta M, Camponovo A, Etienne LL, Cavalli F, Mazzucchelli L (2007) PTEN loss of expression predicts cetuximab efficacy in metastatic colorectal cancer patients. Br J Cancer 97(8):1139–45
De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V, Papamichael D, Laurent-Puig P, Penault-Llorca F, Rougier P, Vincenzi B, Santini D, Tonini G, Cappuzzo F, Frattini M, Molinari F, Saletti P, De Dosso S, Martini M, Bardelli A, Siena S, Sartore-Bianchi A, Tabernero J, Macarulla T, Di Fiore F, Gangloff AO, Ciardiello F, Pfeiffer P, Qvortrup C, Hansen TP, Van Cutsem E, Piessevaux H, Lambrechts D, Delorenzi M, Tejpar S (2010) Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol 11(8):753–62
Linardou H, Dahabreh IJ, Kanaloupiti D, Siannis F, Bafaloukos D, Kosmidis P, Papadimitriou CA, Murray S (2008) Assessment of somatic k-RAS mutations as a mechanism associated with resistance to EGFR-targeted agents: a systematic review and meta-analysis of studies in advanced non-small-cell lung cancer and metastatic colorectal cancer. Lancet Oncol 9(10):962–72. doi:10.1016/S1470-2045(08)70206-7
Van Cutsem E, Köhne CH, Láng I, Folprecht G, Nowacki MP, Cascinu S, Shchepotin I, Maurel J, Cunningham D, Tejpar S, Schlichting M, Zubel A, Celik I, Rougier P, Ciardiello F (2011) Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol 29(15):2011–9. doi:10.1200/JCO.2010.33.5091
Massarelli E, Varella-Garcia M, Tang X, Xavier AC, Ozburn NC, Liu DD, Bekele BN, Herbst RS, Wistuba II (2007) KRAS mutation is an important predictor of resistance to therapy with epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. Clin Cancer Res 13(10):2890–6
Godin-Heymann N, Ulkus L, Brannigan BW, McDermott U, Lamb J, Maheswaran S, Settleman J, Haber DA (2008) The T790M "gatekeeper" mutation in EGFR mediates resistance to low concentrations of an irreversible EGFR inhibitor. Mol Cancer Ther 7(4):874–9. doi:10.1158/1535-7163.MCT-07-2387
Cappuzzo F, Ligorio C, Toschi L, Rossi E, Trisolini R, Paioli D, Magrini E, Finocchiaro G, Bartolini S, Cancellieri A, Hirsch FR, Crino L, Varella-Garcia M (2007) EGFR and HER2 gene copy number and response to first-line chemotherapy in patients with advanced non-small cell lung cancer (NSCLC). J Thorac Oncol 2(5):423–9
Daniele L, Macrì L, Schena M, Dongiovanni D, Bonello L, Armando E, Ciuffreda L, Bertetto O, Bussolati G, Sapino A (2007) Predicting gefitinib responsiveness in lung cancer by fluorescence in situ hybridization/chromogenic in situ hybridization analysis of EGFR and HER2 in biopsy and cytology specimens. Mol Cancer Ther 6(4):1223–9
Cappuzzo F, Varella-Garcia M, Shigematsu H, Domenichini I, Bartolini S, Ceresoli GL, Rossi E, Ludovini V, Gregorc V, Toschi L, Franklin WA, Crino L, Gazdar AF, Bunn PA Jr, Hirsch FR (2005) Increased HER2 gene copy number is associated with response to gefitinib therapy in epidermal growth factor receptor-positive non-small-cell lung cancer patients. J Clin Oncol 23(22):5007–18
Hirsch FR, Varella-Garcia M, Cappuzzo F (2009) Predictive value of EGFR and HER2 overexpression in advanced non-small-cell lung cancer. Oncogene 28(Suppl 1):S32–7. doi:10.1038/onc.2009.199
Yonesaka K, Zejnullahu K, Okamoto I, Satoh T, Cappuzzo F, Souglakos J, Ercan D, Rogers A, Roncalli M, Takeda M, Fujisaka Y, Philips J, Shimizu T, Maenishi O, Cho Y, Sun J, Destro A, Taira K, Takeda K, Okabe T, Swanson J, Itoh H, Takada M, Lifshits E, Okuno K, Engelman JA, Shivdasani RA, Nishio K, Fukuoka M, Varella-Garcia M, Nakagawa K, Jänne PA (2011) Activation of ERBB2 signaling causes resistance to the EGFR-directed therapeutic antibody cetuximab. Sci Transl Med 3(99):99ra86. doi:10.1126/scitranslmed.3002442
Martin V, Landi L, Molinari F, Fountzilas G, Geva R, Riva A, Saletti P, De Dosso S, Spitale A, Tejpar S, Kalogeras KT, Mazzucchelli L, Frattini M, Cappuzzo F (2013) HER2 gene copy number status may influence clinical efficacy to anti-EGFR monoclonal antibodies in metastatic colorectal cancer patients. Br J Cancer 108(3):668–75. doi:10.1038/bjc.2013.4
Frederick BA, Helfrich BA, Coldren CD, Zheng D, Chan D, Bunn PA Jr, Raben D (2007) Epithelial to mesenchymal transition predicts gefitinib resistance in cell lines of head and neck squamous cell carcinoma and non-small cell lung carcinoma. Mol Cancer Ther 6(6):1683–91
Uramoto H, Iwata T, Onitsuka T, Shimokawa H, Hanagiri T, Oyama T (2010) Epithelial-mesenchymal transition in EGFR-TKI acquired resistant lung adenocarcinoma. Anticancer Res 30(7):2513–7
Vergote IB, Jimeno A, Joly F, Katsaros D, Coens C, Despierre E, Marth C, Hall M, Steer CB, Colombo N, Lesoin A, Casado A, Reinthaller A, Green J, Buck M, Ray-Coquard I, Ferrero A, Favier L, Reed NS, Curé H, Pujade-Lauraine E (2014) Randomized phase III study of erlotinib versus observation in patients with no evidence of disease progression after first-line platin-based chemotherapy for ovarian carcinoma: a European Organisation for Research and Treatment of Cancer-Gynaecological Cancer Group, and Gynecologic Cancer Intergroup study. J Clin Oncol 32(4):320–6. doi:10.1200/JCO.2013.50.5669
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–16
Vergote I, Rustin GJ, Eisenhauer EA, Kristensen GB, Pujade-Lauraine E, Parmar MK, Friedlander M, Jakobsen A, Vermorken JB (2000) Re: new guidelines to evaluate the response to treatment in solid tumors [ovarian cancer]. Gynecologic Cancer Intergroup. J Natl Cancer Inst 92(18):1534–5
Varella-Garcia M (2006) Stratification of non-small cell lung cancer patients for therapy with epidermal growth factor receptor inhibitors: the EGFR fluorescence in situ hybridization assay. Diagn Pathol 1:19
Forbes SA, Bindal N, Bamford S, Cole C, Kok CY, Beare D, Jia M, Shepherd R, Leung K, Menzies A, Teague JW, Campbell PJ, Stratton MR, Futreal PA (2011) COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res 39(Database issue):D945–50. doi:10.1093/nar/gkq929
Li H, Durbin R (2009) Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25(14):1754–60. doi:10.1093/bioinformatics/btp324
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, Garimella K, Altshuler D, Gabriel S, Daly M, DePristo MA (2010) The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res 20(9):1297–303. doi:10.1101/gr.107524.110
Albers CA, Lunter G, MacArthur DG, McVean G, Ouwehand WH, Durbin R (2011) Dindel: accurate indel calls from short-read data. Genome Res 21(6):961–73. doi:10.1101/gr.112326.110
Reumers J, De Rijk P, Zhao H, Liekens A, Smeets D, Cleary J, Van Loo P, Van Den Bossche M, Catthoor K, Sabbe B, Despierre E, Vergote I, Hilbush B, Lambrechts D, Del-Favero J (2011) Optimized filtering reduces the error rate in detecting genomic variants by short-read sequencing. Nat Biotechnol 30(1):61–8. doi:10.1038/nbt.2053
Lassus H, Sihto H, Leminen A, Joensuu H, Isola J, Nupponen NN, Butzow R (2006) Gene amplification, mutation, and protein expression of EGFR and mutations of ERBB2 in serous ovarian carcinoma. J Mol Med (Berl) 84(8):671–81
Acknowledgments
We thank all patients for their participation in the EORTC-GCG 55041 trial. In addition, the active commitment of the EORTC, the study coordinators, and investigators providing tumor tissue is gratefully acknowledged, as it enabled this translational study. We are grateful to Mrs. Katrien Drijkoningen and Mrs. Godelieve Verbist for their expert technical support. This publication was supported by the EORTC Charitable Trust and by an unrestricted educational grant from Roche. Evelyn Despierre was supported by a grant for the NOCI project “Pharmacogenomic and immunohistochemical evaluation of the EGFR pathway in ovarian cancer in patients treated with erlotinib: combined prognostic and predictive assessment on the EORTC 55041-study,” which was competitively selected during the EORTC Groups Annual Meeting in 2009. FISH analyses were supported in part by NCI grant CCSG P30 CA046934 to the University of Colorado Comprehensive Cancer Center.
We acknowledge all collaborators who actively contributed to this study, including C. Abraham (Hôpital André Mignot, Le Chesnay, France), F. Amant (University Hospital Leuven, Leuven, Belgium), R. Anderson (University of Colorado, Boulder, CO, USA), A. Azzedine (Centre Hospitalier, Avignon, France), C. Benedetto (University of Turin, Turin, Italy), G. Bertelli (Singelton Hospital, Swansea, UK), P. Berteloot (University Hospital Leuven, Leuven, Belgium), D. Berton-Rigaud (Centre René Gauducheau, Saint-Herblain, France), N. Biglia (University of Turin, Turin, Italy), N. Bonichon-Lamichhane (Clinique Tivoli, Bordeaux, France), P. Bougnoux (Centre Hospitalier Universitaire [CHU], Tours, France), E. Bourbouloux (Centre René Gauducheau, Saint-Herblain, France), C. Bourcier (Centre Hospitalier Départemental [CHD] Les Oudairies, La Roche-Sur-Yon, France), M. Buck (Sir Charles Gairdner Hospital, Nedlands, Australia), M. Campone (Centre René Gauducheau, Saint-Herblain, France), E.M. Canuto (University of Turin, Turin, Italy), A. Casado Herraez (Hospital Universitario San Carlos, Madrid, Spain), I. Cauvin (Centre Hospitalier, Chambéry, France), L. Chauvenet (Hôpital Hôtel-Dieu, Paris, France), A. Chevalier-Place (Centre Oscar Lambret, Lille, France), P.-H. Cottu (Institut Curie, Paris, France), J. Cretin (Clinique de Valdegour, Nîmes, France), I. Cumin (Centre Hospitalier de Bretagne Sud, Lorient, France), H. Curé (Institut Jean Godinot, Reims, France), F. Dalenc (Institut Claudius Régaud, Toulouse, France), S. Danese (University of Turin, Turin, Italy), A. Davis (The Canberra Hospital, Garran (woden), Australia), P. Debruyne (AZ St. Augustinus, Kortrijk, Belgium), G. Delplanque (Groupe Hospitalier Saint-Joseph, Paris, France), R. Delva (Centre Paul Papin, Angers, France), De Valk (Onze Lieve Vrouw Gasthuis, Amsterdam), V. D'Hondt (Hôpitaux Universitaires Jules Bordet), D. Dramais (Centre Hospitalier, Valence, France), X. Durando (Centre Jean Perrin, Clermont-Ferrand, France), C. El Kouri (Centre Catherine de Sienne, Nantes, France), C. Esteban (Hospital Virgen de la Salud, Toledo, Spain), M. Fabbro (Institut du Cancer de Montpellier Val d'Aurelle, Montpellier, France), C. Falandry (Centre Hospitalier Lyon Sud, Pierre-Bénite, France), B. Filleul (Hopital de Jolimont, Haine-Saint-Paul, Belgium), A. Floquet (Institut Bergonie, Bordeaux, France), P. Fumoleau (Centre Georges François Leclerc, Dijon, France), M. Garcia-Varella (University of Colorado, Boulder, CO, USA), C. Garnier (Groupe Hospitalier Mutualiste, Institut Daniel Hollard, Grenoble, France), E. Gilby (Royal United Hospital, Bath, UK), L. Gladieff (Centre Claudius Regaud, Toulouse, France), F. Goffin (Centre Hospitalier Regional de la Citadelle, Liège, Belgium), M.-C. Gouttebel (Centre Hospitalier, Valence, France), J.A. Green (Clatterbridge Cancer Centre NHS Foundation Trust, Bebington, Wirral, UK), J.-P. Guastalla (Centre Léon Bérard, Lyon, France), A.-C. Hardy-Bessard (Clinique Armoricaine de Radiologie, Saint-Brieuc, France), F. Hirsch (University of Colorado, Boulder, CO, USA), A. Hughes (Gateshead Hospitals, Queen Elizabeth Hospital, Gateshead, UK), D. Jaubert (Clinique Tivoli, Bordeaux, France), M.-C. Kaminsky (Centre Alexis Vautrin, Vandoeuvre-lès-Nancy, France), D. Katsaros (Clinica Universita, Torino, Italy), Frederic Kridelka (Centre Hospitalier Regional de la Citadelle, Liège, Belgium), R. Largillier (Centre Antoine Lacassagne, Nice, France), D. Lebrun-Jezekova (Institut Jean Godinot, Reims, France), B. Leduc (Centre Hospitalier, Brive-la-Gaillarde, France), M. Leheurteur (Centre Jean Perrin, Clermont-Ferrand, France), A. Lesoin (Centre Oscar Lambret, Lille, France), K. Leunen (University Hospital Leuven, Leuven, Belgium), N. Levasseur (Groupe Hospitalier Saint-Joseph, Paris, France), C. Leyronnas (Groupe Hospitalier Mutualiste, Institut Daniel Hollard, Grenoble, France), J.-F. Llory (Institut d'Oncologie Hartmann, Levallois Perret, France), A. Lortholary (Centre Catherine de Sienne, Nantes, France), F. Mayer (Centre Georges Francois Leclerc, Dijon, France), D. Mayeur (Hôpital André Mignot, Le Chesnay, France), C. Mendiola (Hospital Universitario 12 de Octubre, Madrid, Spain), L. Mignot (Institut Curie, Paris, France), J. Morgan (Ipswich Hospital NHS Trust, Ipswich, Suffolk, UK), M.-A. Mouret-Reynier (Centre Jean Perrin, Clermont-Ferrand, France), P. Neven (University Hospital Leuven, Leuven, Belgium), Paola Modaffari (Ospedale Mauriziano Umberto I, Torino, Italy),T. Petit (Centre Paul Strauss, Strasbourg, France),E. Picardo (University of Turin, Turin, Italy), J. Plaza (Centre Hospitalier Général, Montbelliard, France), M. Pluvio-Coronado (Universitario San Carlos Madrid, Madrid, Spain), F. Priou (CHD Les Oudairies, La Roche-Sur-Yon, France), E. Pujade-Lauraine (Hôpital Hôtel-Dieu, Paris, France), I. Ray Coquard (Centre Leon Berard, Lyon, France), N. Reed (NHS Greater Glasgow and Clyde Beatson West of Scotland Cancer Centre-Gartnavel General Hospital, Glasgow, UK), I. Rigault de la Longrais (University of Turin, Turin, Italy), S. Scholl (Institut Curie, Paris, France), I. Sillet-Bach (Centre Hospitalier, Brive-La-Gaillarde, France),C. Steer (Murray Valley Private Hospital, Wodonga, Australia), J. Summers (Mid Kent Oncology Centre, Maidstone, Kent, UK), V. Trillet-Lenoir (Centre Hospitalier Lyon Sud, Pierre-Bénite, France), P. Van Dam (AZ St. Augustinus, Wilrijk, Belgium), M.E.L. Van Der Burg (Erasmus Medical Center, Rotterdam, the Netherlands), E. Vanlerenberghe (Centre Oscar Lambret, Lille, France), J.-M. Vannetzel (Institut d'Oncologie Hartmann, Levallois Perret, France),I. Vergote (University Hospital Leuven, Leuven, Belgium), J.A. Vidart Aragon (Universitario San Carlos Madrid, Madrid, Spain), J. Waters (East Kent Hospitals University NHS Foundation Trust, Queen Elizabeth The Queen Mother Hospital, Margate, UK), B. Weber (Centre Alexis Vautrin, Vandoeuvre-Les-Nancy, France), G. Yazbek (Institut Jean Godinot, Reims, France), P. Zola (Ospedale Mauriziano Umberto I, Torino, Italy).
Conflict of Interest
Marileila Varella-Garcia is co-inventor on a patent held by the University of Colorado to use EGFR copy number as biomarker for selection of lung cancer patients for targeted therapy. Evelyn Despierre, Ignace Vergote, Ryan Anderson, Corneel Coens, Dionyssios Katsaros, Fred R. Hirsch, Bram Boeckx, Annamaria Ferrero, Isabelle Ray-Coquard, Els MJJ Berns, Antonio Casado, Diether Lambrechts, and Antonio Jimeno declare no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Online Resource 1
(DOCX 50 kb)
Online Resource 2
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Despierre, E., Vergote, I., Anderson, R. et al. Epidermal Growth Factor Receptor (EGFR) Pathway Biomarkers in the Randomized Phase III Trial of Erlotinib Versus Observation in Ovarian Cancer Patients with No Evidence of Disease Progression after First-Line Platinum-Based Chemotherapy. Targ Oncol 10, 583–596 (2015). https://doi.org/10.1007/s11523-015-0369-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-015-0369-6