Abstract
Purpose
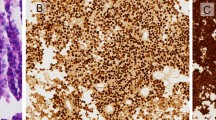
Silent corticotroph adenomas (SCAs) are clinically silent and non-secreting, but exhibit positive adrenocorticotropic hormone (ACTH) immunostaining. We characterized a single center cohort of SCA patients, compared the SCAs to silent gonadotroph adenomas (SGAs), identified predictors of recurrence, and reviewed and compared the cohort to previously published SCAs cases.
Methods
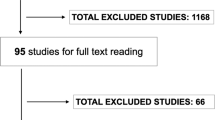
Retrospective review of SCA and SGA surgically resected patients over 10 years and 6 years, respectively. Definitions; SCA—no clinical or biochemical evidence of Cushing’s syndrome and ACTH positive immunostaining, and SGA—steroidogenic factor (SF-1) positive immunostaining. A systematic literature search was undertaken using Pubmed and Scopus.
Results
Review revealed 814 pituitary surgeries, 39 (4.8%) were SCAs. Mean follow-up was 6.4 years (range 0.5–23.8 years). Pre-operative magnetic resonance imaging demonstrated sphenoid and/or cavernous sinus invasion in 44%, 33% were > 50% cystic, and 28% had high ACTH levels pre-operatively. Compared to SGAs (n = 70), SCAs were of similar size and invasiveness (2.5 vs. 2.9 cm, p = 0.2; 44 vs. 41%, p = 0.8, respectively), but recurrence rate was higher (36 vs. 10%, p = 0.001) and more patients received radiation therapy (18 vs. 3%, p = 0.006). Less cystic tumors (0 vs. 50%, p < 0.001) and higher pre-operative ACTH levels (54 vs. 28 pg/ml, p = 0.04) were predictors of recurrence for SCAs.
Conclusion
This review is unique; a strict definition of SCA was used, and single center SCAs were compared with SGAs and with SCAs literature reviewed cases. We show that SCAs are aggressive and identify predictors of recurrence. Accurate initial diagnosis, close imaging and biochemical follow up are warranted.

Similar content being viewed by others
References
Horvath E, Kovacs K, Killinger DW, Smyth HS, Platts ME, Singer W (1980) Silent corticotropic adenomas of the human pituitary gland: a histologic, immunocytologic, and ultrastructural study. Am J Pathol 98(3):617–638
Kovacs K, Horvath E, Bayley TA, Hassaram ST, Ezrin C (1978) Silent corticotroph cell adenoma with lysosomal accumulation and crinophagy. A distinct clinicopathologic entity. Am J Med 64(3):492–499
Saeger W, Ludecke DK, Buchfelder M, Fahlbusch R, Quabbe HJ, Petersenn S (2007) Pathohistological classification of pituitary tumors: 10 years of experience with the German Pituitary Tumor Registry. Eur J Endocrinol 156(2):203–216
Cooper O (2015) Silent corticotroph adenomas. Pituitary 18(2):225–231
Scheithauer BW, Jaap AJ, Horvath E, Kovacs K, Lloyd RV, Meyer FB, Laws ER Jr, Young WF Jr (2000) Clinically silent corticotroph tumors of the pituitary gland. Neurosurgery 47(3):723–729
Webb KM, Laurent JJ, Okonkwo DO, Lopes MB, Vance ML, Laws ER (2003) Clinical characteristics of silent corticotrophic adenomas and creation of an internet-accessible database to facilitate their multi-institutional study. Neurosurgery 53(5):1076–1085
Cho HY, Cho SW, Kim SW, Shin CS, Park KS, Kim SY (2010) Silent corticotroph adenomas have unique recurrence characteristics compared with other nonfunctioning pituitary adenomas. Clin Endocrinol 72(5):648–653
Bradley KJ, Wass JA, Turner HE (2003) Non-functioning pituitary adenomas with positive immunoreactivity for ACTH behave more aggressively than ACTH immunonegative tumours but do not recur more frequently. Clin Endocrinol 58(1):59–64
Baldeweg SE, Pollock JR, Powell M, Ahlquist J (2005) A spectrum of behaviour in silent corticotroph pituitary adenomas. Br J Neurosurg 19(1):38–42
Abe M, Sawabe Y, Mochizuki Y, Sunaga S, Izumiyama H, Matsumoto K, Kushima M, Taniyama M, Ban Y, Sano T (2001) Corticotroph cell adenoma without typical manifestations of Cushing’s disease presenting with cavernous sinus syndrome following pituitary apoplexy. Endocr J 48(4):503–507
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F, Asa SL, Zadeh G (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir 154(8):1493–1498
Al-Sarraj S, King A, Harris P, Lantos P (2002) Atypical pituitary adenoma (silent corticotroph pituitary adenoma). Neuropathol Appl Neurobiol 28(2):157–158
Ambrosi B, Colombo P, Bochicchio D, Bassetti M, Masini B, Faglia G (1992) The silent corticotropinoma: is clinical diagnosis possible? J Endocrinol Invest 15(6):443–452
Benaiges D, Puig J, Lafuente J, Gimeno J, Prados M, Sagarra E, Flores-Le-Roux J (2012) Biochemical behaviour of an incidentally diagnosed silent corticotroph adenoma. Neuro Endocrinol Lett 33(3):290–293
Bordo G, Duong H, McLaughlin N, Cornell R, Findling J, Kelly D (2012) Case report: silent corticotroph adenoma progressing to cushing’s disease then to pituitary carcinoma with dramatic treatment response. J Neurol Surg Part B 73:02
Braithwaite SS, Clasen RA, D’Angelo CM (1997) Silent corticotroph adenoma: case report and literature review. Endocr Pract 3(5):297–301
Brown RL, Wollman R, Weiss RE (2007) Transformation of a pituitary macroadenoma into to a corticotropin-secreting carcinoma over 16 years. Endocr Pract 13(5):463–471
Cazabat L, Dupuy M, Boulin A, Bernier M, Baussart B, Foubert L, Raffin-Sanson ML, Caron P, Bertherat J, Gaillard S (2014) Silent, but not unseen: multimicrocystic aspect on T2-weighted MRI in silent corticotroph adenomas. Clin Endocrinol 81(4):566–572
Chen SC, Chung WY (2015) Progression rate of silent corticotroph adenomas after stereotactic radiosurgery. In regard to Xu et al. Int J Radiat Oncol Biol Phys 91(5):1113–1114
Coire CI, Horvath E, Kovacs K, Smyth HS, Sasano H, Iino K, Feig DS (1998) A composite silent corticotroph pituitary adenoma with interspersed adrenocortical cells: case report. Neurosurgery 42(3):650–654
Cooper ME, Murray RM, Kalnins R, Woodward J, Jerums G (1987) The development of Cushing’s syndrome from a previously silent pituitary tumour. Aust N Z J Med 17(2):249–251
Cooper O, Ben-Shlomo A, Bonert V, Bannykh S, Mirocha J, Melmed S (2010) Silent corticogonadotroph adenomas: clinical and cellular characteristics and long-term outcomes. Horm Cancer 1(2):80–92
Fang H, Tian R, Wu H, Xu J, Fan H, Zhou J, Zhong L (2015) Cushing disease after treatment of nonfunctional pituitary adenoma: a case report and literature review. Medicine 94(51):e2134
Farrell WE, Coll AP, Clayton RN, Harris PE (2003) Corticotroph carcinoma presenting as a silent corticotroph adenoma. Pituitary 6(1):41–47
Felix I, Asa SL, Kovacs K, Horvath E (1991) Changes in hormone production of a recurrent silent corticotroph adenoma of the pituitary: a histologic, immunohistochemical, ultrastructural, and tissue culture study. Hum Pathol 22(7):719–721
Gheri RG, Boddi W, Ammannati F, Olivotto J, Nozzoli C, Franchi A, Bordi L, Luisi ML, Mennonna P (1997) Two-step development of a pituitary adenoma: from hyperprolactinemic syndrome to Cushing’s disease. J Endocrinol Invest 20(4):240–244
Ghervan C (2014) Silent corticotroph adenoma transformed in secreting adenoma with severe Cushing’s disease after two pituitary surgeries. Acta Endocrinol 10(2):283–292
Gibson S, Ray DW, Crosby SR, Dornan TL, Jennings AM, Bevan JS, Davis JR, White A (1996) Impaired processing of proopiomelanocortin in corticotroph macroadenomas. J Clin Endocrinol Metab 81(2):497–502
Gogel EL, Salber PR, Tyrrell JB, Rosenblum ML, Findling JW (1983) Cushing’s disease in a patient with a ‘nonfunctioning’ pituitary tumor: spontaneous development and remission. Arch Intern Med 143(5):1040–1042
Guttenberg KB, Mayson SE, Sawan C, Kharlip J, Lee JY, Martinez-Lage M, Loevner LA, Ewanichak J, Grady MS, Snyder PJ (2016) Prevalence of clinically silent corticotroph macroadenomas. Clin Endocrinol 85(6):874–880
He L, Forbes JA, Carr K, Highfield Nickols H, Utz A, Moots P, Weaver K (2016) Response of silent corticotroph pituitary carcinoma to chemotherapy: case report. J Neurosurg Sci 60(2):272–280
Ikeda H, Yoshimoto T, Kovacs K, Horvath E (1995) Cushing’s disease due to female gonadotroph adenoma of the pituitary. Clin Endocrinol 43(3):383–386
Ioachimescu AG, Eiland L, Chhabra VS, Mastrogianakis GM, Schniederjan MJ, Brat D, Pileggi AV, Oyesiku NM (2012) Silent corticotroph adenomas: Emory University cohort and comparison with ACTH-negative nonfunctioning pituitary adenomas. Neurosurgery 71(2):296–303
Jahangiri A, Wagner JR, Pekmezci M, Hiniker A, Chang EF, Kunwar S, Blevins L, Aghi MK (2013) A comprehensive long-term retrospective analysis of silent corticotrophic adenomas vs hormone-negative adenomas. Neurosurgery 73(1):8–17
Kojima Y, Suzuki S, Yamamura K, Ohhashi G, Yamamoto I (2002) Comparison of ACTH secretion in Cushing’s adenoma and clinically silent corticotroph adenoma by cell immunoblot assay. Endocr J 49(3):285–292
Iino K, Oki Y, Matsushita F, Yamashita M, Hayashi C, Miura K, Nishizawa S, Nakamura H (2007) Immunohistochemical properties of silent corticotroph adenoma and Cushing’s disease. Pituitary 10(1):35–45
Lipatenkova A, Dzeranova L, Pigarova E, Ektova A (2014) Clinical case: silent corticotroph pituitary macroadenoma transforming into Cushing disease. Endocr Abstr. doi:10.1530/endoabs.35.P915
Lopez JA, Kleinschmidt-Demasters BK, Sze C-I, Woodmansee WW, Lillehei KO (2004) Silent corticotroph adenomas: Further clinical and pathological observations. Hum Pathol 35(9):1137–1147
Matsuno A, Okazaki R, Oki Y, Nagashima T (2004) Secretion of high-molecular-weight adrenocorticotropic hormone from a pituitary adenoma in a patient without Cushing stigmata: case report. J Neurosurg 101(5):874–877
Mindermann T, Kovacs K, Wilson CB (1994) Changes in the immunophenotype of recurrent pituitary adenomas. Neurosurgery 35(1):39–44
Moshkin O, Syro LV, Scheithauer BW, Ortiz LD, Fadul CE, Uribe H, Gonzalez R, Cusimano M, Horvath E, Rotondo F, Kovacs K (2011) Aggressive silent corticotroph adenoma progressing to pituitary carcinoma: the role of temozolomide therapy. Hormones 10(2):162–167
Ohta S, Nishizawa S, Oki Y, Yokoyama T, Namba H (2002) Significance of absent prohormone convertase 1/3 in inducing clinically silent corticotroph pituitary adenoma of subtype I–immunohistochemical study. Pituitary 5(4):221–223
Pawlikowski M, Kunert-Radek J, Radek M (2008) “Silent" corticotropinoma. Neuro Endocrinol Lett 29(3):347–350
Psaras T, Honegger J, Buslei R, Saeger W, Klein D, Capper D, Meyermann R, Mittelbronn M (2007) Atypical type II silent corticotrophic adenoma developing into Cushing’s disease upon second recurrence. Exp Clin Endocrinol Diabetes 115(9):610–615
Raverot G, Wierinckx A, Jouanneau E, Auger C, Borson-Chazot F, Lachuer J, Pugeat M, Trouillas J (2010) Clinical, hormonal and molecular characterization of pituitary ACTH adenomas without (silent corticotroph adenomas) and with Cushing’s disease. Eur J Endocrinol 163(1):35–43
Reincke M, Allolio B, Saeger W, Kaulen D, Winkelmann W (1987) A pituitary adenoma secreting high molecular weight adrenocorticotropin without evidence of Cushing’s disease. J Clin Endocrinol Metab 65(6):1296–1300
Righi A, Faustini-Fustini M, Morandi L, Monti V, Asioli S, Mazzatenta D, Bacci A, Foschini MP (2017) The changing faces of corticotroph cell adenomas: the role of prohormone convertase 1/3. Endocr 56(2):286–297
Sakaguchi H, Koshiyama H, Sano T, Inoue D, Hashimoto N, Aoki N, Nakao K (1997) A case of nonfunctioning pituitary adenoma resembling so-called silent corticotroph adenoma. Endocr J 44(2):329–333
Sano T, Kovacs K, Asa SL, Yamada S, Sanno N, Yokoyama S, Takami H (2002) Pituitary adenoma with “honeycomb Golgi” appearance showing a phenotypic change at recurrence from clinically nonfunctioning to typical Cushing disease. Endocr Pathol 13(2):125–130
Scheithauer BW, Gaffey TA, Lloyd RV, Sebo TJ, Kovacs KT, Horvath E, Yapıcıer Ö, Young WF, Meyer FB, Kuroki T, Riehle DL, Laws ER (2006) Pathobiology of pituitary adenomas and carcinomas. Neurosurgery 59(2):341–353
Serri O, Robert F, Pelletier G, Beauregard H, Hardy J (1987) Hyperprolactinemia associated with clinically silent adenomas: endocrinologic and pathologic studies; a report of two cases. Fertil Steril 47(5):792–796
Tan EU, Ho MS, Rajasoorya CR (2000) Metamorphosis of a non-functioning pituitary adenoma to Cushing’s disease. Pituitary 3(2):117–122
Tateno T, Izumiyama H, Doi M, Akashi T, Ohno K, Hirata Y (2007) Defective expression of prohormone convertase 1/3 in silent corticotroph adenoma. Endocr J 54(5):777–782
Tateno T, Kato M, Tani Y, Oyama K, Yamada S, Hirata Y (2009) Differential expression of somatostatin and dopamine receptor subtype genes in adrenocorticotropin (ACTH)-secreting pituitary tumors and silent corticotroph adenomas. Endocr J 56(4):579–584
Ueyama T, Tamaki N, Kondoh T, Kurata H (1998) Large and invasive silent corticotroph-cell adenoma with elevated serum ACTH: a case report. Surg Neurol 50(1):30–31
Walsh MT, Couldwell WT (2010) Symptomatic cystic degeneration of a clinically silent corticotroph tumor of the pituitary gland. Skull Base 20(5):367–370
Yamada S, Ohyama K, Taguchi M, Takeshita A, Morita K, Takano K, Sano T (2007) A study of the correlation between morphological findings and biological activities in clinically nonfunctioning pituitary adenomas. Neurosurgery 61(3):580–584
Yamakita N, Murai T, Kawamura S, Teramachi H, Matsuhisa T, Hirata T, Ikeda T, Morita H, Mune T, Yasuda K (1999) High molecular weight corticotropin measured with immunoradiometric assay in a patient with asymptomatic pituitary corticotropinoma. Endocr J 46(4):563–571
Yokoyama S, Kawahara Y, Sano T, Nakayama M, Kitajima S, Kuratsu J (2001) A case of non-functioning pituitary adenoma with Cushing’s syndrome upon recurrence. Neuropathology 21(4):288–293
Zoli M, Faustini-Fustini M, Mazzatenta D, Marucci G, De Carlo E, Bacci A, Pasquini E, Lanzino G, Frank G (2015) ACTH adenomas transforming their clinical expression: report of 5 cases. Neurosurg Focus 38(2):E15
Barr K, Pillinger DA, Miller CR, Wan Y, Sharpless JL (2016) ACTH staining does not predict retx in silent acth adenomas. Poster presentation, Endocrine Society Meeting SUN-487
Bonner RA, Mukai K, Oppenheimer JH (1979) Two unusual variants of Nelson’s syndrome. J Clin Endocrinol Metab 49(1):23–29
Petrossians P, Ronci N, Valdes Socin H, Kalife A, Stevenaert A, Bloch B, Tabarin A, Beckers A (2001) ACTH silent adenoma shrinking under cabergoline. Eur J Endocrinol 144(1):51–57
Sahli R, Christ ER, Seiler R, Kappeler A, Vajtai I (2006) Clinicopathologic correlations of silent corticotroph adenomas of the pituitary: report of four cases and literature review. Pathol Res Pract 202(6):457–464
Salgado LR, Machado MC, Cukiert A, Liberman B, Kanamura CT, Alves VA (2006) Cushing’s disease arising from a clinically nonfunctioning pituitary adenoma. Endocr Pathol 17(2):191–199
Asano S, Ooka H, Okazaki R, Ishikawa T, Ochiai H, Nakashima M, Ide F, Hasegawa I, Miyawaki S, Nakaguchi H, Murakami M, Ogino Y, Takano K, Matsuno A (2007) Long-term remission of cyclic Cushing’s disease that was diagnosed and treated surgically in non-active phase. Endocr J 54(3):407–412
Popovic V, Micic D, Nesovic M, Howlett T, Doniach I, Kendereski A, Djordjevic P, Manojlovic D, Micic J, Besser M (1990) Cushing’s disease cycling over ten years. Exp Clin Endocrinol 96(2):143–148
Ceccato F, Lombardi G, Manara R, Emanuelli E, Denaro L, Milanese L, Gardiman MP, Bertorelle R, Scanarini M, D’Avella D, Occhi G, Boscaro M, Zagonel V, Scaroni C (2015) Temozolomide and pasireotide treatment for aggressive pituitary adenoma: expertise at a tertiary care center. J Neurooncol 122(1):189–196
Nishioka H, Hirano A, Asa SL (1992) Silent corticotroph adenoma with multiple cysts: Pars intermedia tumor? Endocr Pathol 3(1):47–51
Kasuki L, Ventura N, Wildemberg L, Cardão Chimelli L, Gadelha M (2017) Accuracy of microcystic aspect on T2-weighted magnetic resonance imaging for the diagnosis of silent corticotropinomas. Presented at the 99th Endocrine Society Meeting, Orlando, April 2017 SAT 469
Kovacs K, Lloyd R, Horvath E, Asa SL, Stefaneanu L, Killinger DW, Smyth HS (1989) Silent somatotroph adenomas of the human pituitary. A morphologic study of three cases including immunocytochemistry, electron microscopy, in vitro examination, and in situ hybridization. Am J Pathol 134(2):345–353
Cooper O, Melmed S (2012) Subclinical hyperfunctioning pituitary adenomas: the silent tumors. Best Pract Res Clin Endocrinol Metab 26(4):447–460
Sano T, Mader R, Asa SL, Qian ZR, Hino A, Yamada S (2003) “Honeycomb Golgi” in pituitary adenomas: not a marker of gonadotroph adenomas. Endocr Pathol 14(4):363–368
Jin L, Riss D, Ruebel K, Kajita S, Scheithauer BW, Horvath E, Kovacs K, Lloyd RV (2005) Galectin-3 expression in functioning and silent ACTH-producing adenomas. Endocr Pathol 16(2):107–114
Thodou E, Argyrakos T, Kontogeorgos G (2007) Galectin-3 as a marker distinguishing functioning from silent corticotroph adenomas. Hormones 6(3):227–232
Mete O, Hayhurst C, Alahmadi H, Monsalves E, Gucer H, Gentili F, Ezzat S, Asa SL, Zadeh G (2013) The role of mediators of cell invasiveness, motility, and migration in the pathogenesis of silent corticotroph adenomas. Endocr Pathol 24(4):191–198
Acknowledgements
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
The study was approved under an IRB approved data repository with waiver of consent.
Rights and permissions
About this article
Cite this article
Langlois, F., Lim, D.S.T., Yedinak, C.G. et al. Predictors of silent corticotroph adenoma recurrence; a large retrospective single center study and systematic literature review. Pituitary 21, 32–40 (2018). https://doi.org/10.1007/s11102-017-0844-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-017-0844-4