Abstract
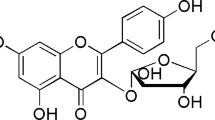
Chemotherapy-associated neurotoxicity is one of the principal side-effects for doxorubicin (DOX)-treated cancer patients. Despite its poor-penetration across the blood–brain barrier (BBB), DOX is linked to the induction of oxidative stress and neuroinflammation. Berberine (BEB) is a natural polyphenolic alkaloid, which exhibits unique antioxidant activity and anti-inflammatory potential. The present study was performed to investigate the neuroprotective potential of BEB in a rodent model of DOX-induced neurotoxicity. Neurotoxicity was induced in rats via a single acute dose of DOX (20 mg/kg/week, i.p.). BEB was administered at 50 mg/kg/day orally for 10 days before and 4 days after DOX administration. Brain acetylcholinesterase (AChE) activities were evaluated. Oxidative stress was investigated via the colorimetric determination of lipid peroxides, glutathione reduced (GSH) contents and catalase (CAT) activities in the brain tissue. In addition, DOX-induced genotoxicity was evaluated using comet assay. DOX produced a significant elevation in AChE activities. Additionally, DOX provoked oxidative stress as evidenced from the significant elevation in lipid peroxidation along with depletion in GSH contents and CAT activities. Moreover, DOX resulted in neuroinflammation as indicated by the elevation of pro-inflammatory mediator glial fibrillary acid protein (GFAP), as well as, the pro-apoptotic nuclear factor kappa B (NF-κB) and caspase-3 in brain tissue. Co-treatment with BEB significantly counteracted DOX-induced oxidative stress, neuroinflammation and genotoxicity. Histopathological and immunohistochemical examination supported the biochemical results. BEB demonstrated neuroprotective potential through exerting cholinergic, anti-oxidative, genoprotective, anti-inflammatory, and anti-apoptotic activities. Our findings present BEB as a promising “pre-clinical” neuroprotective agent against DOX-induced neurotoxicity during anti-neoplastic therapy.









Similar content being viewed by others
Data Availability
All data generated or analyzed during this study are included in this published article.
Abbreviations
- DOX:
-
Doxorubicin
- BBB:
-
Blood–brain barrier
- BEB:
-
Berberine
- AChE:
-
Acetylcholinesterase
- GSH:
-
Glutathione reduced
- CAT:
-
Catalase
- GFAP:
-
Glial fibrillary acid protein
- NF-κB:
-
Nuclear factor kappa B
- ROS:
-
Reactive oxygen species
- PUFAs:
-
Polyunsaturated fatty acids
References
Schultz L, Zurich MG, Culot M, da Costa A, Landry C et al (2015) Evaluation of drug-induced neurotoxicity based on metabolomics, proteomics and electrical activity measurements in complementary CNS in vitro models. Toxicol In Vitro 30(1):138–165
Borai IH, Ezz MK, Rizk MZ, Aly HF, El-Sherbiny M, Matloub AA, Fouad GI (2017) Therapeutic impact of grape leaves polyphenols on certain biochemical and neurological markers in AlCl3-induced Alzheimer’s disease. Biomed Pharmacother 93:837–851
Ibrahim Fouad G (2021) The neuropathological impact of COVID-19: a review. Bull Natl Res Cent 45(1):1–9
Ibrahim Fouad G (2020) Combination of omega 3 and coenzyme Q10 exerts neuroprotective potential against hypercholesterolemia-induced Alzheimer’s-like disease in rats. Neurochem Res 45(5):1142–1155. https://doi.org/10.1007/s11064-020-02996-2
Jordan B, Margulies A, Cardoso F, Cavaletti G, Haugnes HS et al (2020) Systemic anticancer therapy-induced peripheral and central neurotoxicity: ESMO–EONS–EANO Clinical Practice Guidelines for diagnosis, prevention, treatment and follow-up. Ann Oncol 31(10):1306–1319
Loghin ME, Kleiman A (2020) Medication-induced neurotoxicity in critically Ill cancer patients. In: Nates J, Price K (eds) Oncologic critical care. Springer, Cham, pp 319–334. https://doi.org/10.1007/978-3-319-74588-6_32
Cavaletti G (2014) Chemotherapy-induced peripheral neurotoxicity (CIPN): what we need and what we know. J Peripher Nerv Syst 19(2):66–76. https://doi.org/10.1111/jns5.12073
Prša P, Karademir B, Biçim G et al (2020) The potential use of natural products to negate hepatic, renal and neuronal toxicity induced by cancer therapeutics. Biochem Pharmacol 173:113551
Eide S, Feng ZP (2020) Doxorubicin chemotherapy-induced “chemo-brain”: Meta-analysis. Eur J Pharmacol 881:173078
Cavaletti G, Alberti P, Marmiroli P (2015) Chemotherapy-induced peripheral neurotoxicity in cancer survivors: an underdiagnosed clinical entity? Am Soc Clin Oncol Educ Book. https://doi.org/10.14694/EdBook_AM.2015.35.e553
Aluise CD, Sultana R, Tangpong J et al (2010) Chemo brain (chemo fog) as a potential side effect of doxorubicin administration: role of cytokine-induced, oxidative/nitrosative stress in cognitive dysfunction. Chemo Fog 678:147–156
Hayslip J, Dressler EV, Weiss H et al (2015) Plasma TNF-α and soluble TNF receptor levels after doxorubicin with or without co-administration of mesna—a randomized, cross-over clinical study. PloS One 10(4):e0124988
Sinha BK, Mason RP (2015) Is metabolic activation of topoisomerase II poisons important in the mechanism of cytotoxicity? J Drug Metab Toxicol 6(3):186
Aluise CD, Miriyala S, Noel T et al (2011) 2-Mercaptoethane sulfonate prevents doxorubicin-induced plasma protein oxidation and TNF-α release: implications for the reactive oxygen species-mediated mechanisms of chemobrain. Free Radic Biol Med 50(11):1630–1638
Brantley-Finley C, Lyle CS, Du L et al (2003) The JNK, ERK and p53 pathways play distinct roles in apoptosis mediated by the antitumor agents vinblastine, doxorubicin, and etoposide. Biochem Pharmacol 66(3):459–469
Cardinale D, Colombo A, Bacchiani G et al (2015) Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 131(22):1981–1988
Heeba GH, Mahmoud ME (2016) Dual effects of quercetin in doxorubicin-induced nephrotoxicity in rats and its modulation of the cytotoxic activity of doxorubicin on human carcinoma cells. Environ Toxicol 31(5):624–636
Guzel EE, Tektemur NK, Tektemur A (2021) Alpha-lipoic acid may ameliorate testicular damage by targeting dox-induced altered antioxidant parameters, mitofusin-2 and apoptotic gene expression. Andrologia 53:e13990
Liu X, Qiu Y, Liu Y et al (2021) Citronellal ameliorates doxorubicin-induced hepatotoxicity via antioxidative stress, antiapoptosis, and proangiogenesis in rats. Biochem Mol Toxicol 35(2):e22639
Wang S, Konorev EA, Kotamraju S, Joseph J et al (2004) Doxorubicin induces apoptosis in normal and tumor cells via distinctly different mechanisms: intermediacy of H2O2-and p53-dependent pathways. Biol Chem 279(24):25535–25543
Rashid S, Ali N, Nafees S et al (2013) Alleviation of doxorubicin-induced nephrotoxicity and hepatotoxicity by chrysin in Wistar rats. Toxicol Mech Method 23(5):337–345
Kuzu M, Kandemir FM, Yildirim S, Kucukler S et al (2018) Morin attenuates doxorubicin-induced heart and brain damage by reducing oxidative stress, inflammation and apoptosis. Biomed Pharmacother 106:443–453
Silverman DH, Dy CJ, Castellon SA, Lai J, Pio BS, Abraham L et al (2007) Altered frontocortical, cerebellar, and basal ganglia activity in adjuvant-treated breast cancer survivors 5–10 years after chemotherapy. Breast Cancer Res Treat 103(3):303–311
Salas-Ramirez KY, Bagnall C, Frias L et al (2015) Doxorubicin and cyclophosphamide induce cognitive dysfunction and activate the ERK and AKT signaling pathways. Behav Brain Res 292:133–141
Keeney JT, Ren X, Warrier G, Noel T et al (2018) Doxorubicin-induced elevated oxidative stress and neurochemical alterations in brain and cognitive decline: protection by MESNA and insights into mechanisms of chemotherapy-induced cognitive impairment (“chemobrain”). Oncotarget 9(54):30324
Merzoug S, Toumi ML, Boukhris N et al (2011) Adriamycin-related anxiety-like behavior, brain oxidative stress and myelotoxicity in male Wistar rats. Pharmacol Biochem Behav 99(4):639–647
Allen BD, Apodaca LA, Syage AR et al (2019) Attenuation of neuroinflammation reverses Adriamycin-induced cognitive impairments. Acta Neuropathol Commun 7(1):1–15
Janelsins MC, Kesler SR, Ahles TA, Morrow GR (2014) Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 26(1):102–113
Sardi I, la Marca G, Cardellicchio S, Giunti L, Malvagia S, Genitori L et al (2013) Pharmacological modulation of blood–brain barrier increases permeability of doxorubicin into the rat brain. Am J Cancer Res 3(4):424
Carrasco R, Ramirez MC, Nes K et al (2020) Prevention of doxorubicin-induced cardiotoxicity by pharmacological non-hypoxic myocardial preconditioning based on docosahexaenoic acid (DHA) and carvedilol direct antioxidant effects: study protocol for a pilot, randomized, double-blind, controlled trial (CarDHA trial). Trials 21(1):137
Sergazy S, Shulgau Z, Fedotovskikh G, Chulenbayeva L et al (2020) Cardioprotective effect of grape polyphenol extract against doxorubicin induced cardiotoxicity. Sci Rep 10(1):1–12
Mohamed RH, Karam RA, Amer MGMG (2011) Epicatechin attenuates doxorubicin-induced brain toxicity: critical role of TNF-α, iNOS and NF-κB. Brain Res Bull 86(1–2):22–28
Stankovic JSK, Selakovic D, Mihailovic V, Rosic G (2020) Antioxidant supplementation in the treatment of neurotoxicity induced by platinum-based chemotherapeutics—a review. Int J Mol Sci 21(20):7753
Mohammed A, Janakiram NB, Pant S, Rao CV (2015) Molecular targeted intervention for pancreatic cancer. Cancers 7(3):1499–1542
Yue Q, Gao G, Zou G, Yu H, Zheng X (2017) Natural products as adjunctive treatment for pancreatic cancer: recent trends and advancements. Biomed Res Int 2017:8412508
Li L, Leung PS (2014) Use of herbal medicines and natural products: an alternative approach to overcoming the apoptotic resistance of pancreatic cancer. Int J Biochem Cell Biol 53:224–236
Li B, Gan R, Yang Q, Huang J, Chen P, Wan L, Guo C (2015) Chinese herbal medicines as an adjunctive therapy for unresectable pancreatic cancer: a systematic review and meta-analysis. Evid-Based Complement Alter Med. https://doi.org/10.1155/2015/350730
Arayne MS, Sultana N, Bahadur SS (2007) The berberis story: Berberis vulgaris in therapeutics. Pak J Pharm Sci 20(1):83–92
Singh IP, Mahajan S (2013) Berberine and its derivatives: a patent review (2009–2012). Expert Opin Ther Pat 23(2):215–231
Abd El-Wahab AE, Ghareeb DA, Sarhan EE, Abu-Serie MM, El Demellawy MA (2013) In vitro biological assessment of Berberis vulgaris and its active constituent, berberine: antioxidants, anti-acetylcholinesterase, anti-diabetic and anticancer effects. BMC Complement Altern Med 13(1):1–12
Ghareeb DA, Khalil S, Hafez HS, Bajorath J, Ahmed HE et al (2015) Berberine reduces neurotoxicity related to nonalcoholic steatohepatitis in rats. Evid-Based Complement Altern Med. https://doi.org/10.1155/2015/361847
Ahmad S, Hussain A, Hussain A, Abdullah I, Ali MS et al (2019) Quantification of berberine in Berberis vulgaris L. root extract and its curative and prophylactic role in cisplatin-induced in vivo toxicity and in vitro cytotoxicity. Antioxidants 8(6):185
Chen X, Zhang Y, Zhu Z, Liu H, Guo H et al (2016) Protective effect of berberine on doxorubicin-induced acute hepatorenal toxicity in rats. Mol Med Rep 13(5):3953–3960
Colvin LA (2019) Chemotherapy-induced peripheral neuropathy (CIPN): where are we now? Pain 160(Suppl 1):S1
Hajra S, Patra AR, Basu A, Bhattacharya S (2018) Prevention of doxorubicin (DOX)-induced genotoxicity and cardiotoxicity: effect of plant derived small molecule indole-3-carbinol (I3C) on oxidative stress and inflammation. Biomed Pharmacother 101:228–243
Verma T, Mallik SB, Ramalingayya GV, Nayak PG et al (2017) Sodium valproate enhances doxorubicin-induced cognitive dysfunction in Wistar rats. Biomed Pharmacother 96:736–741
Mohammed HS, Hosny EN, Khadrawy YA, Magdy M et al (1866) (2020) Protective effect of curcumin nanoparticles against cardiotoxicity induced by doxorubicin in rat. Biochim et Biophys Acta (BBA)-Mol Basis Dis 5:165665
Sadraie S, Kiasalari Z, Razavian M et al (2019) Berberine ameliorates lipopolysaccharide-induced learning and memory deficit in the rat: insights into underlying molecular mechanisms. Metab Brain Dis 34:245–255. https://doi.org/10.1007/s11011-018-0349-5
Ohkawa H et al (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95(2):351–358
Beutler E, Duron O, Kelly BM (1963) An improved method for the determination of blood glutathione. J Lab Clin Med 61:882–888
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126. https://doi.org/10.1016/s0076-6879(84)05016-3
Singh NP, McCoy MT, Tice RR, Schneider EL (1988) A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res 175(1):184–191
Suvarna KS, Layton C, Bancroft JD (eds) (2018) Bancroft’s theory and practice of histological techniques E-Book. Elsevier Health Sciences, London
El-Shiekh RA, Ashour RM, Abd El-Haleim EA et al (2020) A potent natural neuroprotective agent for the prevention of streptozotocin-induced Alzheimer’s disease in mice. Biomed Pharmacother 128:110303
Park OK, Choi JH, Park JH, Kim IH, Yan BC, Ahn JH, Kwon SH, Lee JC, Kim YS, Kim M, Kang IJ, Kim JD, Lee YL, Won MH (2012) Comparison of neuroprotective effects of five major lipophilic diterpenoids from Danshen extract against experimentally induced transient cerebral ischemic damage. Fitoterapia 83:1666–1674
Youssef S, Abd-El-Aty OA, Mossalam M (2011) Effects of prenatal phenytoin toxicity on the expression of glial fibrillary acidic protein (GFAP) in the developing rat cerebellum. J Am Sci 7(8):139–152
Matsushita K, Wu Y, Qiu J, Lang-Lazdunski L et al (2000) Fas receptor and neuronal cell death after spinal cord ischemia. J Neurosci 20(18):6879–6887
Chin M, Yokoyama R, Sumi M, Okita H et al (2020) Multimodal treatment including standard chemotherapy with vincristine, doxorubicin, cyclophosphamide, ifosfamide, and etoposide for the Ewing sarcoma family of tumors in Japan: results of the Japan Ewing Sarcoma Study 04. Pediatr Blood Cancer 67(5):e28194
Leung WS, Kuo WW, Ju DT, Wang TD et al (2020) Protective effects of diallyl trisulfide (DATS) against doxorubicin-induced inflammation and oxidative stress in the brain of rats. Free Radic Biol Med 160:141–148
Pal S, Ahir M, Sil PC (2012) Doxorubicin-induced neurotoxicity is attenuated by a 43-kD protein from the leaves of Cajanus indicus L. via NF-κB and mitochondria dependent pathways. Free Radic Res 46(6):785–798
Khadrawy YA, Hosny EN, Mohammed HS (2021) Protective effect of nanocurcumin against neurotoxicity induced by doxorubicin in rat’s brain. NeuroToxicology 85:1
Patil S, Tawari S, Mundhada D, Nadeem S (2015) Protective effect of berberine, an isoquinoline alkaloid ameliorates ethanol-induced oxidative stress and memory dysfunction in rats. Pharmacol Biochem Behav 136:13–20
Hussien HM, Abd-Elmegied A, Ghareeb DA, Hafez HS et al (2018) Neuroprotective effect of berberine against environmental heavy metals-induced neurotoxicity and Alzheimer’s-like disease in rats. Food Chem Toxicol 111:432–444
Ji HF, Shen L (2012) Molecular basis of inhibitory activities of berberine against pathogenic enzymes in Alzheimer’s disease. Sci World J 2012:823201
Patel M (2016) Targeting oxidative stress in central nervous system disorders. Trends Pharmacol Sci 37(9):768–778
Islam MT (2017) Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol Res 39(1):73–82
Shaker FH, El-Derany MO, Wahdan SA, El-Demerdash E, El-Mesallamy HO (2021) Berberine ameliorates doxorubicin-induced cognitive impairment (chemobrain) in rats. Life Sci 269:119078
Tangpong J, Cole MP, Sultana R et al (2007) Adriamycin-mediated nitration of manganese superoxide dismutase in the central nervous system: insight into the mechanism of chemobrain. Neurochemistry 100(1):191–201
Mayer CA, Brunkhorst R, Niessner M, Pfeilschifter W et al (2013) Blood levels of glial fibrillary acidic protein (GFAP) in patients with neurological diseases. PloS ONE 8(4):e62101
Lei J, Gao G, Feng J, Jin Y et al (2015) Glial fibrillary acidic protein as a biomarker in severe traumatic brain injury patients: a prospective cohort study. Crit Care 19(1):1–12
Sofroniew MV (2015) Astrocyte barriers to neurotoxic inflammation. Nat Rev Neurosci 16(5):249–263
Siracusa R, Fusco R, Cuzzocrea S (2019) Astrocytes: role and functions in brain pathologies. Front Pharmacol 10:1114
Cardoso CV, de Barros MP, Bachi ALL, Bernardi MM et al (2020) Chemobrain in rats: behavioral, morphological, oxidative and inflammatory effects of doxorubicin administration. Behav Brain Res 378:112233
Ali MA, Menze ET, Tadros MG, Tolba MF (2020) Caffeic acid phenethyl ester counteracts doxorubicin-induced chemobrain in Sprague-Dawley rats: emphasis on the modulation of oxidative stress and neuroinflammation. Neuropharmacology 181:108334
Rizk HA, Masoud MA, Maher OW (2017) Prophylactic effects of ellagic acid and rosmarinic acid on doxorubicin-induced neurotoxicity in rats. J Biochem Mol Toxicol 31(12):e21977
Alhowail AH, Bloemer J, Majrashi M, Pinky PD et al (2019) Doxorubicin-induced neurotoxicity is associated with acute alterations in synaptic plasticity, apoptosis, and lipid peroxidation. Toxicol Mech Method 29(6):457–466
Quiles JL, Huertas JR, Batino M, Mataix J, Ramirez-Tortosa MC (2002) Antioxidants nutrients and adriamycin toxicity. Toxicology 180:79–95
Choi SS, Lee HJ, Lim I, Satoh JI, Kim SU (2014) Human astrocytes: secretome profiles of cytokines and chemokines. PloS One 9(4):e92325
Liu T, Zhang L, Joo D, Sun SC (2017) NF-κB signaling in inflammation. Signal Transduct Target Ther 2(1):1–9
Mattson MP, Kroemer G (2003) Mitochondria in cell death: novel targets for neuroprotection and cardioprotection. Trends Mol Med 9:196–205
Ongnok B, Chattipakorn N, Chattipakorn SC (2020) Doxorubicin and cisplatin induced cognitive impairment: the possible mechanisms and interventions. Exp Neurol 324:113118
Moneim AEA (2015) The neuroprotective effect of berberine in mercury-induced neurotoxicity in rats. Metab Brain Dis 30(4):935–942
Sadeghnia HR, Kolangikhah M, Asadpour E, Forouzanfar F et al (2017) Berberine protects against glutamate-induced oxidative stress and apoptosis in PC12 and N2a cells. Iran J Basic Med Sci 20(5):594
Zhang Z, Li X, Li FL (2016) An, Berberine alleviates postoperative cognitive dysfunction by suppressing neuroinflammation in aged mice. Int Immunopharmacol 38:426–433
Ren Z, He H, Zuo Z, Xu Z, Wei Z, Deng J (2019) The role of different SIRT1-mediated signaling pathways in toxic injury. Cell Mol Biol Lett 24:36
Zhang Q, Qian Z, Pan L, Li H, Zhu H (2012) Hypoxia-inducible factor 1 mediates the anti-apoptosis of berberine in neurons during hypoxia/ischemia. Acta Physiol Hung 99(3):311–323
Wu YZ, Zhang L, Wu ZX, Shan TT, Xiong C (2019) Berberine ameliorates doxorubicin-induced cardiotoxicity via a SIRT1/p66Shc-mediated pathway. Oxid Med Cell Longev 2019:2150394
Wang J, Zhang Y (2018) Neuroprotective effect of berberine agonist against impairment of learning and memory skills in severe traumatic brain injury via Sirt1/p38 MAPK expression. Mol Med Rep 17(5):6881–6886
Rausch CR, Jabbour EJ, Kantarjian HM, Kadia TM (2020) Optimizing the use of the hyperCVAD regimen: clinical vignettes and practical management. Cancer 126(6):1152–1160
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
GIF conceived and designed the research proposal, performed experiments, analyzed biochemical data, and wrote the original manuscript. KAA was responsible for methodology and writing of histopathological and immunohistochemical investigations and review of the original manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to the content of this article.
Ethical Approval
The animal protocol was adopted in accordance with the National Research Council’s Guide for the Care and Use of Laboratory Animals (NIH Publications No. 8023, revised 1978), and experimental procedures were approved by the Ethical Committee, National Research Centre (NRC), Egypt (Approval no. 19–313).
Consent to Participate
All authors gave their consent to participate in the present study.
Consent for Publication
All authors gave approval to publish the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ibrahim Fouad, G., Ahmed, K.A. Neuroprotective Potential of Berberine Against Doxorubicin-Induced Toxicity in Rat’s Brain. Neurochem Res 46, 3247–3263 (2021). https://doi.org/10.1007/s11064-021-03428-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-021-03428-5