Abstract
Introduction
Brain tumor treatment and survival information is generally limited in large-scale cancer datasets. We provide a clinical investigation of current patterns of care and survival estimates for central nervous system (CNS) tumors treated in the United States.
Methods
We analyzed the National Cancer Database from 2004–2015 for all patients with diagnosis of primary CNS tumors. We describe patient demographics, treatment modality, and analyzed survival estimates.
Results
512,168 patient tumor records were examined. The most common histology was meningioma (43.6%), followed by glioblastoma (22.0%), and nerve sheath tumors (10.6%). Patients had a median age of 60 years, with a female (57.9%), white (85.0%), and non-Hispanic (87.8%) predominance. Tumors were reported as World Health Organization (WHO) grade I for 55.9% of the patients, grade II for 5.9%, grade III for 4.4%, grade IV for 24.3%, and grade unknown or not applicable for 9.4%. Overall, 56% underwent surgical procedures, 30.4% received radiation, and 20.6% received chemotherapy. Radiation plus chemotherapy and surgery was the most common treatment modality in high-grade tumors (40.5% in WHO grade III and 49.3% in WHO grade IV), while surgery only or watchful waiting was preferred in low-grade tumors. Older age, male gender, non-Hispanic origin, higher number of comorbidities, and lower socioeconomic status were identified as risk factors for mortality.
Conclusions
Our analysis provides long-term survival estimates and initial treatment decisions for patients with CNS tumors in hospitals throughout the United States. Age, comorbidities, gender, ethnicity, and socioeconomic characteristics were determinants of survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system (CNS) tumors are a heterogeneous group of malignancies. Based on morphological features alone, over 100 histological subtypes are described [1], and these are further refined by molecular profiling [2]. The incidence of primary brain tumors in the United States is 23.03/100,000 population [3]. Both the prevalence and incidence are expected to rise due to an increasingly aging population, as well as advancing therapeutic and diagnostic strategies. This trend is demonstrated in the Global Burden of Disease Study, which shows increased prevalence and decreased mortality from 1990 to 2015 [4].
Primary brain tumors represent a major public health issue. They are the most common cause of cancer death in children, and the second most common cause of cancer death in young adults [3, 5]. They rank as 14th most common cause of cancer death in patients over 40 years of age [6], and the median survival for aggressive brain tumors such as glioblastoma is around 7 months in the United States [7]. The disability adjusted life-years for brain and nervous system cancer increased by 37.5% from 1990 to 2015, accounting for 3.0% of the overall burden of neurological disorders in 2015 [4]. Symptoms include focal neurological deficits, memory and cognition impairments, and difficulties performing activities of daily living [8, 9].
The main tumors comprising PBT include gliomas and meningiomas. Glioblastoma is the most common type of malignant CNS tumors, while meningioma is the most common type of non-malignant. Less common histology groups include nerve sheath tumors, ependymal tumors, craniopharyngioma, and embryonal tumors. Histological grading and molecular profiling predict biological behavior, with WHO grade being a major determinant of treatment decisions.
The Central Brain Tumor Registry of the United States (CBTRUS) provides population-based comprehensive information regarding incidence, and survival outcomes [3]. However, survival estimates by CBTRUS are estimated using SEER data with only close to 28% of the population, and thus, may not accurately represent observed mortality, particularly in light of the high variety of tumor growth rates and behavior based on molecular subtypes of primary brain tumors. Understanding treatment decisions in daily clinical practice using a large-scale hospital-based data source provides a unique opportunity to assess survival estimates and provide clinical evidence for future therapeutic hypotheses. We provide an updated descriptive investigation of current patterns of care and survival estimates using the National Cancer Database (NCDB), the largest source of hospital-based cancer patient information.
Methods
NCDB is a hospital-based dataset comprising data from over 1500 hospital cancer centers. It is supported by the American College of Surgeons Commission on Cancer (CoC) and the American Cancer Society, under well-established quality standards on collection methods [10, 11]. This database provides a unique opportunity to assess patterns of care with high-quality treatment information and survival estimates in a hospital-based setting, providing valuable information for primary CNS tumors [12]. A list of the CoC centers in the United States is available on the American College of Surgeons website (https://www.facs.org/search/cancer-programs) [13].
We used the 2015 NCDB brain and CNS participant user file, which includes patient data from 2004 to 2015. Tumor records were identified and defined using the International Classification of Disease for Oncology (ICD-0–3), third edition histology and topographical site codes1. Histology grouping was designed based on the categories used by CBTRUS [3] (Supplemental Table 1). Pituitary and pineal tumors are not consistently included within the NCDB brain/CNS file, as per the WHO classification [1], and were excluded from our analysis (4 pituitary and 27 pineal records). Additionally, patients with lymphomas and hematopoietic neoplasms were not included in our analyses, as they are included in a separate participant user file per NCDB.
To ensure the clinical relevance of our results, pilocytic astrocytomas and meningiomas without WHO grade stated were re-graded as WHO grade I, and all glioblastomas were re-graded as WHO grade IV. The following histology groups do not use WHO grade and were re-graded as “Not applicable”: primary melanocytic lesions, germ cell tumors, cysts, and heterotopias, hemangioma, other neoplasms related to the meninges, nerve sheath tumors (9561, 9570, and 9571), and other tumors of cranial and spinal nerves. Craniopharyngioma (9350, 9351, and 9352), ependymal tumors (9391 and 9394), nerve sheath tumors (9541, 9550, and 9560), and neuronal and mixed neuronal-glial tumors (8680, 8690, 8693, 9413, 9492, and 9493) were re-graded as WHO grade I. Embryonal tumors (9470, 9471, 9472, 9473, 9474, 9500, 9501, and 9508) were graded as WHO grade IV. Otherwise, WHO grade was stated as available in NDCB. Grade I–III gliomas grading is presented as reported to the NCDB due to the heterogeneity of this group and the difficulties in estimating grading without central pathology review and complete molecular profiling data. Demographic and clinical variables analyzed include age at diagnosis, sex, race, Hispanic origin, comorbidity score, histology, tumor location, primary payer status, median income, education, and area of residence (metropolitan, urban, or rural).
Molecular profiling characteristics such as 1p/19q co-deletion and O(6)-methylguanine-DNA methyltransferase (MGMT) gene promoter methylation status were included as available in NCDB. These characteristics are determined by each cancer-accredited center per their protocols and results are collect by the NCDB as reported in the patients’ records.
Comorbid conditions were assessed using Charlson/Deyo Score, a weighted score that ranges from 0 to 25, and is derived from the highest score calculated from reported ICD-9 or ICD-10 secondary diagnosis codes [14]. Charlson/Deyo comorbidity scores were available for diagnosis years 2006–2015.
Living area, as determined by residential zip code of the patient recorded at the time of diagnosis, was used to classify patients as metropolitan, urban, or rural, as defined by the United States Department of Agriculture Economic Research Service [15]. Metropolitan was defined as counties with a population of 250,000 or more; urban as a population of 2500 to less than 250,000; and rural as a population of less than 2500 inhabitants. Education was assessed by the percentage of non-high school graduates in the patient residential zip code at the time of diagnosis, categorized as ≤ 7%, 7–12.9%, 13–20.9%, ≥ 21%. Facility location and affiliation are suppressed by NCDB for pediatric and young adult cases to protect confidentiality given the smaller number of patients. Treatment received was assessed as first course of treatment at any CoC facility.
Age is summarized with median and interquartile range and all categorical variables are summarized by counts and percentages. The Wilcoxon Rank Sum test was used for comparisons for age and chi-square was employed for categorical variables. Survival analyses were calculated using Kaplan–Meier and Cox proportional hazard models are represented as forest plots. For all models, observed histologies were collapsed into the following groups: (1) Gliomas (Glioma malignant, NOS, unique astrocytoma variants, oligoastrocytic, diffuse astrocytoma, anaplastic astrocytoma, pilocytic astrocytoma, glioblastoma, oligodendroglioma, and anaplastic oligodendroglioma) (2) Meningiomas (Meningiomas and other neoplasm to meninges) (3) Nerve sheath tumors (4) Other (Other neuroepithelial, other tumors of cranial and spinal nerves, neoplasm, unspecified) (5) Mesenchymal (Mesenchymal and hemangioma) (6) Embryonal (Embryonal and germ cell tumors) (7) Choroid plexus (8) Ependymal (9) Craniopharyngioma (10) Primary melanocytic lesions, and (11) Neuronal and mixed neuronal-glial tumors. All analyses were performed with SAS software version 9.4 (SAS Statistical Institute, Cary, North Carolina).
RESULTS
Demographics and patients characteristics
A total of 512,168 patients were analyzed. Median age was 60 (IQR 47–72) years; 5.0% were younger than 20 years (Table 1, Fig. 1a, Supplemental Table 3). Patients were more commonly female (57.9%), white (85.2%), and non-Hispanic (87.5%). Blacks accounted for 9.2% of patients, with a higher representation in pediatric patients (Table 1).
The majority of patients had a Charlson/Deyo Score equal to zero (76.5%). Around 37% of cases were treated in academic facilities, and 36.3% in community centers. Among patients > 75 years old, 54% were treated in community centers.
Histology and tumor clinical characteristics
The most common histology was meningiomas (43.6%), followed by glioblastoma (21.9%), and nerve sheath tumors (10.6%) (Fig. 2, Supplemental Table 2). The number of cases diagnosed per year is available in Supplemental Table 4. Diagnosis was confirmed histologically in 67.5% and by imaging in 32.2% of patients. Distribution of histology groups by diagnostic confirmation modality is available in Supplemental Table 7. WHO grade I accounted for 55.9% of patients, WHO grade II for 5.9%, WHO grade III for 4.4%, and WHO grade IV for 24.3%. WHO grade was unknown/ not applicable for 9.4% of patients.
The WHO grade I group was mainly composed of meningiomas (73.4%) and nerve sheath tumors (18.2%). WHO grade II included meningiomas (38.8%), diffuse astrocytoma (24.4%), and oligodendrogliomas (19.3%). WHO grade III included anaplastic astrocytoma (44.3%) and diffuse astrocytoma (14.7%). WHO grade IV consisted mainly of glioblastoma (90.3%), and embryonal tumors (4.8%) (Fig. 2, Supplemental Table 2).
WHO grade IV tumors had the smallest percentage of pediatrics cases (4.4%), and the highest percentage of elderly patients (25.3% > 65 years and 20.1% > 75 years). WHO grade I tumors had a significantly higher proportion of females compared to any other WHO grade. This was expected due to the known predominance of meningiomas in the WHO grade I group. In WHO grade I and II there was a higher frequency of blacks and Hispanics compared to high-grade lesions. Sex, race, and age group distribution varied by histology group (Supplemental Tables 5 and 6, Supplemental Fig. 1). Astrocytic, oligodendroglial, craniopharyngioma, ependymal tumors, and germ cell tumors were more frequent in males than females. Neuronal tumors, embryonal tumors, neuroepithelial tumors, choroid plexus tumors, pilocytic astrocytomas, and rare astrocytoma variants were more frequent in younger patients.
The most common primary site location was the meninges (42.7%), followed by the cerebrum (28.8%), and cranial nerves (7.9%) (Fig. 1b). Within the cerebrum, the most common location was the frontal lobe (11.4% of all tumor locations), and within cranial nerves the most common location was the auditory nerve (6.2% of all tumor locations). Pediatrics cases had a higher frequency of tumors in the optic nerve, ventricles, cerebellum, or brainstem compared to any other age group (Supplemental Table 2).
1p/19q co-deletion was determined in 9,872 (Supplemental Tables 8 and 9). 1p19q was co-deleted in 2816, non co-deleted in 5632, and incomplete (either 1p or 19q co-deleted) in 1,424. MGMT methylation status was determined in 13,656 (Supplemental Tables 10 and 11).
Treatment
Overall, 56.0% underwent surgical procedures, 30.4% received radiation, 20.6% received chemotherapy, and 30% did not receive any form of treatment (Table 2). The frequency of not receiving treatment increased progressively with increasing age, with over 57% of patients older than 75 years not receiving any form of treatment. This is likely associated with the high incidence of meningiomas in elderly patients.
Surgery only was the most common treatment in patients younger than 65 years of age, and was used in 34.3% of all primary brain tumors. WHO grade I tumors were more likely to be treated with surgery only (43.3%), or watchful waiting (no treatment) (41.4%). In patients where WHO grade was not reported or not applicable, over 43% were treated with watchful waiting. Radiation, plus chemotherapy, and surgery was the most common treatment modality in high-grade tumors (40.5% in WHO grade III, and 49.3% in WHO grade IV).
Patients with 1p/19q non co-deleted were more commonly treated with surgery plus chemotherapy and radiation, compared to co-deleted (50.4% versus 38.6%, respectively). Patients with MGMT methylated had a slightly higher use of chemotherapy compared to those with MGMT non-methylated (75.9% versus 72.3%, respectively).
Socioeconomic factors
The majority of the patients lived in metropolitan areas (81.4%). Annual income was reported as over $68,000 in 33.3% of cases. Private insurance (46.7%) was the most common type of insurance followed by Medicare (37.5%) (Table 1). The percentage of patients with Medicare was significantly higher in WHO grade I and IV tumors (40.5% and 40.8%, respectively), due to the elderly association with meningiomas and glioblastoma. Twenty-six percent lived in an area with less than 7% of non-High School graduates. The WHO grade IV group had a higher percentage of patients living in urban areas.
Survival
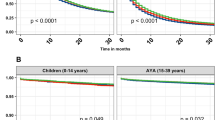
Median survival was approximately 13 years in WHO grade I tumors, 12 years in WHO grade II tumors, 3 years in WHO grade III, 10 months in WHO grade IV tumors, and 12 years in patients WHO grade N/A. Overall 5-year survival estimates were significantly higher in nerve sheath tumors (92.8%), and lowest in glioblastoma (6.0%) (Table 3). Survival varied by WHO grade, within histology groups. Five-year survival for WHO grade I meningiomas was 76.1% and 48.7% for WHO grade III.
Older age, male gender, lower income, glioma histology, and higher number of comorbidities were identified as risk factors for mortality for all primary brain tumors (Fig. 3). In low-grade tumors, older age, male gender, black race, higher comorbidities, and poorer socioeconomic status were associated with mortality (Supplemental Tables 12 and 13). However, in WHO grade III, age between 20 and 44 years was a protective factor for mortality compared to patients younger than 19 years of age (Supplemental Table 14). In WHO IV tumors, blacks had a decreased risk of mortality compared to whites (Supplemental Table 15). Other races were found to be a protective factor for mortality compared to whites in WHO grade III and WHO grade IV tumors. Hispanic origin was a protective factor for survival in every WHO grade.
Discussion
NCDB provides detailed, large-scale information on brain tumor distribution and survival patterns that are not available in other large databases, providing an optimal resource for evaluation of patterns of care as it collects over 70% of all cancer diagnoses in the United States. From these data, we present the largest clinical description of treatment and survival determinants for primary brain tumors.
Demographic characteristics were similar to those described by epidemiological studies [3], with a higher frequency of males, whites, non-Hispanics, and patients with an overall higher socioeconomic status. Blacks had a decreased risk of mortality in low-grade lesions, but the association shifted in WHO grade IV lesions. This may be partially explained by disparities in socioeconomic determinants and access to neuro-oncological care [16,17,18], as low-grade lesions with the highest survival benefits were treated with surgery only. Population-based and NCDB analyses have previously demonstrated survival benefit of blacks over whites in glioblastoma [6, 7, 19]. Although the number of cases of black patients was low, these studies showed that the benefit of black race persisted after receiving treatment. We believe that in part, these variances may be related to differences in tumor biology, molecular profiling, behavior, and treatment response that warrant further investigation [2].
Consistent with data from other countries, meningiomas are the most common primary brain and CNS tumor [3, 20,21,22,23]. Distribution differences are noted however, with a significantly higher percentage of high-grade lesions in the United States compared to other countries. Glioblastoma accounted for 21.9% of the patients in our analysis, and 14.7% in CBTRUS [3].
In our cohort, 32.2% were diagnosed by imaging modalities, which is significantly higher than the 8% reported in a similar hospital-based database in Japan [21], higher than reported by brain tumor registries in Austria, and France [22,23,24], and comparable to the 36.8% described by CBTRUS [3]. The rate of histological confirmation was higher in NCDB in comparison to CBTRUS for every histology group. The large inclusion of imaging-base diagnoses is mainly at the expense of meningiomas and provides the opportunity to assess mortality risk in a clinical setting, as at least 50% of these cases are diagnosed by imaging only. The higher number of pediatric cases with lesions in the optic nerve, ventricles, cerebellum, or brainstem likely reflects the presence of neurofibromatosis and other genetic predisposing factors in this age group [1].
Molecular profiling available in NCDB includes 1p/19q co-deletion and MGMT methylation status, which are some of the key predictive molecular markers in gliomas. Initial studies on the significance of 1p/19q co-deletion indicated an increased chemosensitivity to procarbazine, lomustine, and vincristine (PCV), and longer survival [25], and is now used to define oligodendrogliomas per 2016 classification [1]. Demographics and outcome results of 1p/19q co-deleted patients compared to non-co-deleted were similar to those described by the Cancer Genome Atlas Research Network [26], but in a larger sample size that includes 9872 patients.
MGMT is an intracellular DNA repair enzyme that can reverse the alkylating effect of temozolomide. Once the MGMT gene promoter is hypermethylated its effect is inactivated, and is therefore a prognostic marker [27, 28]. In NCDB, MGMT methylation was reported in 13,656 patients. To our knowledge, this is the largest demographic description of MGMT methylation in primary brain and CNS tumors. We found no demographic differences between MGMT methylated and non-methylated patients. MGMT methylation status is used in clinical decisions primarily in glioblastoma based on expected clinical benefit. Temozolomide confers higher survival benefits for MGMT methylated patients [27]. Among untreated patients, the survival between MGMT methylated and non-methylated glioblastoma is similar [29].
Histology group and expected tumor aggressiveness are the main clinical indicators of treatment received. Overall, surgery was the most common procedure (56%), followed by radiation (30.4%), and chemotherapy (20.6%). The use of surgical resection followed by concomitant radiation and chemotherapy has been the standard of care for glioblastoma since 2005 [30]. Overall, surgery plus chemoradiation was used in 18% of patients in Japan [21], compared to 14.7% in our analysis. However, in high-grade lesions, surgery followed by chemoradiation was preferred in 49.3% of the patients of NCDB, compared to 72–76% of patients in Japan [21]. This may reflect adherence to current standard of care for glioblastoma in the United States but a lower frequency compared to other industrialized countries.
Over 30% of patients did not receive any form of treatment, which correlates with the 31% of patients diagnosed by imaging. These patients are presumed to be low-grade meningiomas that are followed expectantly, as this tumor can be diagnosed by imaging [31]. Still, a proportion of these patients may have unresectable high-grade tumors, and/or contraindications for surgery. Of note, this is significantly lower than is reported by the Brain Tumor Registry of Japan (3%), and we believe it is likely because of the lack of inclusion of patients diagnosed by imaging, as they report only 7% of cases diagnosed by imaging [21]. The Brain Tumor Registry of Japan is an effort by the Japan Neurosurgical Society and this may limit their inclusion to patients that have contact with neurosurgeons at academic medical centers. Patterns of care have been described individually for meningiomas, low grade gliomas, and glioblastoma during this time frame in previous publications by our group [7, 12, 32, 33].
Survival estimates vary by age, WHO grade, tumor location, and -molecular profiling [2, 21, 34]. The 5-year survival rate for glioblastoma (6.0%) was significantly higher than described for Spain (3.7%), and slightly higher than described in CBTRUS (5.6%) [3]. However, it was significantly lower than described in Japan (10.1%) [21], despite similar treatment patterns. This may reflect differences in race or regional treatment responses. Interestingly, 5-year survival rates for benign tumors such as meningiomas was reported to be higher in European cohorts [34, 35], compared to 76.1% in our analysis, and 63.8% in CBTRUS [3]. While comparing benign but lesser common pathologies, such as craniopharyngioma, hemangioma, pilocytic astrocytoma, and neuronal and mixed neuronal-glial tumors, we found these histology groups to be more common in CBTRUS [3]. The 5-year survival rates for pilocytic astrocytoma, meningioma, neuronal and mixed neuronal-glial tumors were higher in CBTRUS. This may be explained by treatment in centers without CoC accreditation.
Some of the limitations of our analysis include the lack of availability of complete molecular profiling, especially isocitrate dehydrogenase (IDH) mutation, inability to obtain specific chemotherapy agent and cause of death, inability to analyze malignant and non-malignant histology due to the lack of behavioral code in the ICD-O-3 variable, and the percentage of missing data (over 10% for facility type and molecular profiling). Our analysis provides a large-scale, comprehensive evaluation on patterns of care for primary brain tumors with long-term survival estimates that complements current population-based analysis with molecular profiling information and treatment received.
References
Cavenee WK, Louis DN, Ohgaki H, Wiestler OD, International Agency for Research on Cancer (2016) WHO classification of tumours of the central nervous system. International Agency For Research On Cancer, Lyon
Verhaak RG, Hoadley KA, Purdom E, Wang V, Qi Y, Wilkerson MD, Miller CR, Ding L, Golub T, Mesirov JP, Alexe G, Lawrence M, O'Kelly M, Tamayo P, Weir BA, Gabriel S, Winckler W, Gupta S, Jakkula L, Feiler HS, Hodgson JG, James CD, Sarkaria JN, Brennan C, Kahn A, Spellman PT, Wilson RK, Speed TP, Gray JW, Meyerson M, Getz G, Perou CM, Hayes DN (2010) Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17:98–110. https://doi.org/10.1016/j.ccr.2009.12.020
Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS (2018) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2011–2015. Neuro-oncology 20:1–86. https://doi.org/10.1093/neuonc/noy131
Feigin VL, Abajobir AA, Abate KH, Abd-Allah F, Abdulle AM, Abera SF, Abyu GY, Ahmed MB, Aichour AN, Aichour I, Aichour MT (2017) Global, regional, and national burden of neurological disorders during 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol 16:877–897. https://doi.org/10.1016/s1474-4422(17)30299-5
Agbahiwe H, Rashid A, Horska A, Mahone EM, Lin D, McNutt T, Cohen K, Redmond K, Wharam M, Terezakis S (2017) A prospective study of cerebral, frontal lobe, and temporal lobe volumes and neuropsychological performance in children with primary brain tumors treated with cranial radiation. Cancer 123:161–168. https://doi.org/10.1002/cncr.30313
Ostrom QT, Cote DJ, Ascha M, Kruchko C, Barnholtz-Sloan JS (2018) Adult glioma incidence and survival by race or ethnicity in the United States from 2000 to 2014. JAMA Oncol 4:1254–1262. https://doi.org/10.1001/jamaoncol.2018.1789
Dressler EV, Liu M, Garcia CR, Dolecek TA, Pittman T, Huang B, Villano JL (2019) Patterns and disparities of care in glioblastoma. Neuro-oncol Pract 6:37–46. https://doi.org/10.1093/nop/npy014
Khan F, Amatya B (2013) Use of the International Classification of Functioning, Disability and Health (ICF) to describe patient-reported disability in primary brain tumour in an Australian community cohort. J Rehabil Med 45:434–445. https://doi.org/10.2340/16501977-1132
Mukand JA, Blackinton DD, Crincoli MG, Lee JJ, Santos BB (2001) Incidence of neurologic deficits and rehabilitation of patients with brain tumors. Am J Phys Med Rehabil 80:346–350
Surawicz TS, Davis F, Freels S, Laws ER Jr, Menck HR (1998) Brain tumor survival: results from the National Cancer Data Base. J Neuro-oncol 40:151–160
Boffa DJ, Rosen JE, Mallin K, Loomis A, Gay G, Palis B, Thoburn K, Gress D, McKellar DP, Shulman LN, Facktor MA, Winchester DP (2017) Using the national cancer database for outcomes research: a review. JAMA Oncol 3:1722–1728. https://doi.org/10.1001/jamaoncol.2016.6905
Liu M, Thakkar JP, Garcia CR, Dolecek TA, Wagner LM, Dressler EVM, Villano JL (2018) National cancer database analysis of outcomes in pediatric glioblastoma. Cancer Med. https://doi.org/10.1002/cam4.1404
Costa DB, Kobayashi S, Pandya SS, Yeo WL, Shen Z, Tan W, Wilner KD (2011) CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J Clin Oncol 29:e443–445. https://doi.org/10.1200/JCO.2010.34.1313
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Fekrazad MH, Ravindranathan M, Jones DV Jr (2007) Response of intracranial metastases to erlotinib therapy. J Clin Oncol 25:5024–5026. https://doi.org/10.1200/JCO.2007.13.3751
Dressler EV, Dolecek TA, Liu M, Villano JL (2017) Demographics, patterns of care, and survival in pediatric medulloblastoma. J Neuro-oncol 132:497–506. https://doi.org/10.1007/s11060-017-2400-5
Liu M, Thakkar JP, Garcia CR, Dolecek TA, Wagner LM, Dressler EVM, Villano JL (2018) National cancer database analysis of outcomes in pediatric glioblastoma. Cancer Med 7:1151–1159. https://doi.org/10.1002/cam4.1404
Rhome R, Fisher R, Hormigo A, Parikh RR (2016) Disparities in receipt of modern concurrent chemoradiotherapy in glioblastoma. J Neurooncol 128:241–250. https://doi.org/10.1007/s11060-016-2101-5
Bohn A, Braley A, de la Rodriguez PV, Zevallos JC, Barengo NC (2018) The association between race and survival in glioblastoma patients in the US: a retrospective cohort study. PLoS ONE 13:e0198581. https://doi.org/10.1371/journal.pone.0198581
Dho YS, Jung KW, Ha J, Seo Y, Park CK, Won YJ, Yoo H (2017) An updated nationwide epidemiology of primary brain tumors in Republic of Korea, 2013. Brain Tumor Res Treat 5:16–23. https://doi.org/10.14791/btrt.2017.5.1.16
Committee of Brain Tumor Registry of Japan (2017) Brain Tumor Registry of Japan (2005–2008). Neurol Medico-chir 57:9–102. https://doi.org/10.2176/nmc.sup.2017-0001
Wohrer A, Waldhor T, Heinzl H, Hackl M, Feichtinger J, Gruber-Mosenbacher U, Kiefer A, Maier H, Motz R, Reiner-Concin A, Richling B, Idriceanu C, Scarpatetti M, Sedivy R, Bankl HC, Stiglbauer W, Preusser M, Rossler K, Hainfellner JA (2009) The Austrian Brain Tumour Registry: a cooperative way to establish a population-based brain tumour registry. J Neuro-oncol 95:401–411. https://doi.org/10.1007/s11060-009-9938-9
Darlix A, Zouaoui S, Rigau V, Bessaoud F, Figarella-Branger D, Mathieu-Daude H, Tretarre B, Bauchet F, Duffau H, Taillandier L, Bauchet L (2017) Epidemiology for primary brain tumors: a nationwide population-based study. J Neuro-oncol 131:525–546. https://doi.org/10.1007/s11060-016-2318-3
Baldi I, Gruber A, Alioum A, Berteaud E, Lebailly P, Huchet A, Tourdias T, Kantor G, Maire JP, Vital A, Loiseau H (2011) Descriptive epidemiology of CNS tumors in France: results from the Gironde Registry for the period 2000–2007. Neuro-oncology 13:1370–1378. https://doi.org/10.1093/neuonc/nor120
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, Silver JS, Stark PC, Macdonald DR, Ino Y, Ramsay DA, Louis DN (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Brat DJ, Verhaak RG, Aldape KD, Yung WK, Salama SR, Cooper LA, Rheinbay E, Miller CR, Vitucci M, Morozova O, Robertson AG, Noushmehr H, Laird PW, Cherniack AD, Akbani R, Huse JT, Ciriello G, Poisson LM, Barnholtz-Sloan JS, Berger MS, Brennan C, Colen RR, Colman H, Flanders AE, Giannini C, Grifford M, Iavarone A, Jain R, Joseph I, Kim J, Kasaian K, Mikkelsen T, Murray BA, Neill BP, Pachter L, Parsons DW, Sougnez C, Sulman EP, Vandenberg SR, Van Meir EG, von Deimling A, Zhang H, Crain D, Lau K, Mallery D, Morris S, Paulauskis J, Penny R, Shelton T, Sherman M, Yena P, Black A, Bowen J, Dicostanzo K, Gastier-Foster J, Leraas KM, Lichtenberg TM, Pierson CR, Ramirez NC, Taylor C, Weaver S, Wise L, Zmuda E, Davidsen T, Demchok JA, Eley G, Ferguson ML, Hutter CM, Mills Shaw KR, Ozenberger BA, Sheth M, Sofia HJ, Tarnuzzer R, Wang Z, Yang L, Zenklusen JC, Ayala B, Baboud J, Chudamani S, Jensen MA, Liu J, Pihl T, Raman R, Wan Y, Wu Y, Ally A, Auman JT, Balasundaram M, Balu S, Baylin SB, Beroukhim R, Bootwalla MS, Bowlby R, Bristow CA, Brooks D, Butterfield Y, Carlsen R, Carter S, Chin L, Chu A, Chuah E, Cibulskis K, Clarke A, Coetzee SG, Dhalla N, Fennell T, Fisher S, Gabriel S, Getz G, Gibbs R, Guin R, Hadjipanayis A, Hayes DN, Hinoue T, Hoadley K, Holt RA, Hoyle AP, Jefferys SR, Jones S, Jones CD, Kucherlapati R, Lai PH, Lander E, Lee S, Lichtenstein L, Ma Y, Maglinte DT, Mahadeshwar HS, Marra MA, Mayo M, Meng S, Meyerson ML, Mieczkowski PA, Moore RA, Mose LE, Mungall AJ, Pantazi A, Parfenov M, Park PJ, Parker JS, Perou CM, Protopopov A, Ren X, Roach J, Sabedot TS, Schein J, Schumacher SE, Seidman JG, Seth S, Shen H, Simons JV, Sipahimalani P, Soloway MG, Song X, Sun H, Tabak B, Tam A, Tan D, Tang J, Thiessen N, Triche T Jr, Van Den Berg DJ, Veluvolu U, Waring S, Weisenberger DJ, Wilkerson MD, Wong T, Wu J, Xi L, Xu AW, Yang L, Zack TI, Zhang J, Aksoy BA, Arachchi H, Benz C, Bernard B, Carlin D, Cho J, DiCara D, Frazer S, Fuller GN, Gao J, Gehlenborg N, Haussler D, Heiman DI, Iype L, Jacobsen A, Ju Z, Katzman S, Kim H, Knijnenburg T, Kreisberg RB, Lawrence MS, Lee W, Leinonen K, Lin P, Ling S, Liu W, Liu Y, Liu Y, Lu Y, Mills G, Ng S, Noble MS, Paull E, Rao A, Reynolds S, Saksena G, Sanborn Z, Sander C, Schultz N, Senbabaoglu Y, Shen R, Shmulevich I, Sinha R, Stuart J, Sumer SO, Sun Y, Tasman N, Taylor BS, Voet D, Weinhold N, Weinstein JN, Yang D, Yoshihara K, Zheng S, Zhang W, Zou L, Abel T, Sadeghi S, Cohen ML, Eschbacher J, Hattab EM, Raghunathan A, Schniederjan MJ, Aziz D, Barnett G, Barrett W, Bigner DD, Boice L, Brewer C, Calatozzolo C, Campos B, Carlotti CG Jr, Chan TA, Cuppini L, Curley E, Cuzzubbo S, Devine K, DiMeco F, Duell R, Elder JB, Fehrenbach A, Finocchiaro G, Friedman W, Fulop J, Gardner J, Hermes B, Herold-Mende C, Jungk C, Kendler A, Lehman NL, Lipp E, Liu O, Mandt R, McGraw M, McLendon R, McPherson C, Neder L, Nguyen P, Noss A, Nunziata R, Ostrom QT, Palmer C, Perin A, Pollo B, Potapov A, Potapova O, Rathmell WK, Rotin D, Scarpace L, Schilero C, Senecal K, Shimmel K, Shurkhay V, Sifri S, Singh R, Sloan AE, Smolenski K, Staugaitis SM, Steele R, Thorne L, Tirapelli DP, Unterberg A, Vallurupalli M, Wang Y, Warnick R, Williams F, Wolinsky Y, Bell S, Rosenberg M, Stewart C, Huang F, Grimsby JL, Radenbaugh AJ, Zhang J (2015) Comprehensive, Integrative Genomic Analysis of diffuse lower-grade gliomas. N Engl J Med 372:2481–2498. https://doi.org/10.1056/NEJMoa1402121
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. https://doi.org/10.1056/NEJMoa043331
Esteller M, Garcia-Foncillas J, Andion E, Goodman SN, Hidalgo OF, Vanaclocha V, Baylin SB, Herman JG (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354. https://doi.org/10.1056/nejm200011093431901
Kessler T, Sahm F, Sadik A, Stichel D, Hertenstein A, Reifenberger G, Zacher A, Sabel M, Tabatabai G, Steinbach J, Sure U, Krex D, Grosu AL, Bewerunge-Hudler M, Jones D, Pfister SM, Weller M, Opitz C, Bendszus M, von Deimling A, Platten M, Wick W (2018) Molecular differences in IDH wildtype glioblastoma according to MGMT promoter methylation. Neuro-oncology 20:367–379. https://doi.org/10.1093/neuonc/nox160
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D, Cairncross JG, Eisenhauer E, Mirimanoff RO (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. https://doi.org/10.1056/NEJMoa043330
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, Niessen WJ, Breteler MM, van der Lugt A (2007) Incidental findings on brain MRI in the general population. N Engl J Med 357:1821–1828. https://doi.org/10.1056/NEJMoa070972
Garcia CR, Slone SA, Pittman T, St Clair WH, Lightner DD, Villano JL (2018) Comprehensive evaluation of treatment and outcomes of low-grade diffuse gliomas. PLoS ONE 13:e0203639. https://doi.org/10.1371/journal.pone.0203639
Garcia CR, Slone SA, Chau M, Neltner JH, Pittman T, Villano JL (2019) Initial management of meningiomas: analysis of the national cancer database. Cancer Epidemiol 60:16–22. https://doi.org/10.1016/j.canep.2019.02.018
Fuentes-Raspall R, Solans M, Roca-Barcelo A, Vilardell L, Puigdemont M, Del Barco S, Comas R, Garcia-Velasco A, Astudillo A, Carmona-Garcia MC, Marcos-Gragera R (2017) Descriptive epidemiology of primary malignant and non-malignant central nervous tumors in Spain: results from the Girona Cancer Registry (1994–2013). Cancer Epidemiol 50:1–8. https://doi.org/10.1016/j.canep.2017.07.005
Sant M, Minicozzi P, Lagorio S, Borge Johannesen T, Marcos-Gragera R, Francisci S (2012) Survival of European patients with central nervous system tumors. Int J Cancer 131:173–185. https://doi.org/10.1002/ijc.26335
Funding
Supported by the Biostatistics and Bioinformatics Shared Resource of the University of Kentucky Markey Cancer Center (P30CA177558).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal participants performed by any of the authors. Data is de-identified in NCDB and informed consent is not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Garcia, C.R., Slone, S.A., Dolecek, T.A. et al. Primary central nervous system tumor treatment and survival in the United States, 2004–2015. J Neurooncol 144, 179–191 (2019). https://doi.org/10.1007/s11060-019-03218-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03218-8