Abstract
Key developments in the understanding of the immune functions of milk and colostrum are reviewed, focusing on their proteinaceous components. The topics covered include the immunoglobulins, immune cells, immunomodulatory substances, and antimicrobial proteins. The contributions of new technologies and the introduction of fresh approaches from other fields are highlighted, as are the contributions that mammary biology research has made to the development of other fields. Finally, a summary of some current outstanding questions and likely future directions of the field are given.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept that milk, mammary secretions and the mammary gland have major roles in immune defense is an old one. The bactericidal property of milk was recorded in the scientific literature in the late nineteenth century [1, 2]. Moreover, observations at this time on the ability of milk to provide immunity to the newborn [3] played a key role in the development of modern immunology. The aim of this review is to provide a modern audience with a timeline for the key discoveries in milk immunology, illustrating how the current understanding of the immune function of milk evolved, and to offer some pointers for the future direction of the field.
This review is divided into three sections: the immunoglobulins and immune cells, immunomodulatory components, and antimicrobial components, covering elements of both innate and adaptive immunity, immune defenses in the mammary gland and the participation of the mammary gland in the mucosal defense system. In this we focus largely on the proteinaceous components of milk, some of which are depicted in Fig. 1. Reviews describing physical barriers, the role of probiotics, and the carbohydrate and lipid components of milk that have host defense functions have recently been presented elsewhere [4, 5].
Immunoglobulins in Milk
Today it is largely forgotten that the immune properties of milk helped lay the foundation of modern immunology. In 1892, Paul Ehrlich demonstrated that mice immunized against plant toxins passed immunity to the fetus in utero as well as via the milk. These observations were subsequently shown to be due to an ammonium sulfate precipitable substance, termed an antibody [6]. Ehrlich extended this work to develop the concept of passive and active immunisation via antibodies, for which he was awarded the Nobel Prize in 1908. Many other researchers made important contributions through this early period (see Campbell and Petersen [7] for an excellent review of the history of immune milk). For example, Famulener [8] showed that goats immunized prior to parturition could transmit this immunity to the sera of their offspring via colostrum and that this transfer could also take place if goat serum was fed. Further experiments around this time established the concept of passive immunisation through the transfer of milk-derived antibodies from the intestinal lumen into the bloodstream. Colostrum was shown to contain a greater concentration of antibodies than mature milk, and the origin of these substances from serum was confirmed [9]. The importance of colostrum in providing protection from bacterial infection was shown by Smith and Little [10] who reported that a calf deprived of colostrum lacks “something” which allowed intestinal bacteria to invade the body and multiply in various organs. Allied work showed that this “something” was specific agglutinins (substances causing agglutination of cells) in the blood, derived from the mother’s milk [11].
It was appreciated early on that there were significant differences between mammals in the immunological function of the mammary gland. For example, it was noted that colostrum was important for immune transfer to the newborn only in mammals with multi-layered placentae (for example the ungulates) [12–14]. In these species, the antibodies were shown to be absorbed into the bloodstream via the neonatal intestinal mucosa in the first 24–48 h of life [15]. Thus, by 1930, the role of the mammary gland in conferring protection to the neonate through the accumulation and secretion of agglutinating antibodies directed against pathogens was firmly established.
The bivalent structure of antibodies and the nature of their interaction with antigens were gradually elucidated through the 1940s. The highly specific nature of the antibodies in mammary secretions was demonstrated through analysis of the antibodies in colostrum fed to calves that had died from infections with different strains of E. coli [16]. While the presence of antibodies in milk and colostrum was indisputable, at this time there was still debate over their source and the nature of the therapeutic benefit that could be derived from them [7, 17].
The development of polyacrylamide gel electrophoresis and size-exclusion chromatography by the 1960s greatly accelerated the characterisation of the immune components of milk. These techniques led to the definition of individual classes of immunoglobulins (i.e. the agglutinating globulins) as well as comparisons between species. Thus, in sheep the predominant antibody in colostrum was shown to be IgG1 [18], while in humans it was IgA [19]. Moreover, mammary secretions and serum were shown to have distinct immunoglobulin compositions (see Table 1). Despite much additional data being accumulated, there were still questions about the fundamental reason for the difference in milk immunoglobulins between species.
In the 1960s, Campbell and Petersen [7] were enthusiastic advocates for the therapeutic benefits of colostrum and milk from immunized cows. In particular, and most controversially, systemic responses to oral consumption of immune milk were claimed, with beneficial effects on symptoms of arthritis and hay fever [7]. This work was commercialized by Ralph Stolle, whose company (http://www.smbimilk.com) still markets ‘hyperimmune milk’ to the present day.
The origin of the immunoglobulins in milk was the source of some controversy. Campbell and Petersen believed that the majority of antibodies in bovine mammary secretions were synthesized within the udder. They based this premise, in part, on their observation that ‘adequate’ numbers of plasma cells are present in the udder immediately before parturition [20]. However, later workers found only low levels of plasma cells [21]. These differences may have been due to differences in the health status of the gland between the experiments. Others favoured a humoral source of the immunoglobulins in colostrum and milk [17], based on the observed decrease in serum immunoglobulin levels before parturition and a corresponding increase in the udder [22]. While IgG was shown to be transported to the mammary gland from the serum, IgA was found to be synthesized within the mammary gland by plasma cells which had migrated into the gland from the gastrointestinal tract (see below). It was found that in species where IgG is transferred to the foetus prior to birth (e.g. humans), IgA is the predominant immunoglobulin in colostrum, whereas in those born with no circulating IgG (e.g. cattle and sheep), IgG is the predominant immunoglobulin in colostrum. A 10-fold increase in the IgG1:IgG2 ration in bovine colostrum over that in serum suggested a specific IgG1 transport mechanism [23].
By the 1970s, the mechanism for the transport of IgG into the mammary gland had been elucidated. The IgG receptor, FcRn, was identified and shown to be present on the apical surface of the gut of the suckling rat [24] as well as on the basolateral surface of the secretory epithelial cell during colostrogenesis [25]. Immunohistochemical analysis showed that FcRn expression coincided with Stage 1 lactogenesis (the onset of colostrogenesis) and was decreased during stage 2 lactogenesis (the onset of copious secretion; [26]).
The hormonal regulation of immunoglobulin transport into colostrum and milk has been investigated but remains incompletely described. Smith and co-workers [27] suggested that changing serum concentrations of estrogen and progesterone in late pregnancy exerted a controlling influence on the selective transport of IgG1 to bovine lacteal fluid and thus colostrum formation. However, others suggested that the rate of IgG1 transfer was a consequence of mammary gland development [28], which is itself under the control of estrogen and progesterone. Investigation into the role of prolactin in IgG transport showed that in the presence of the prolactin release inhibitor, bromoergocryptine, colostrum-like secretion continued post-partum for several days and mammary IgG1 receptor activity was maintained [26]. Addition of prolactin to mammary cells in culture resulted in down-regulation of the receptor [29]. Thus, it seems that prolactin plays a role in regulating the IgG1 receptor during Stage 2 lactogenesis. However, regulation of the induction of IgG receptor during Stage 1 lactogenesis remains poorly understood.
Advances in the knowledge of cellular immunity in mucosal tissues led to greater understanding of the origins of plasma cells in the mammary gland. These cells were shown to migrate into the mammary gland from the gut-associated lymphoid tissues (GALT) [30]. Adoptive transfer studies revealed that lymphocytes from the GALT populate many mucosal effector sites including the mammary gland. The precursors of plasma cells destined to produce IgA were shown to originate from GALT and traffic into the mammary gland near the time of parturition as well as in middle and late lactation [31]. In the late 1970s the concept of the ‘common mucosal immune system’ was proposed [32] in which the antigenic experience at one mucosal surface was deemed to lead to effector responses at a distant mucosal tissue, a concept that was supported by the discovery of cell surface receptors and cytokines. Thus, the idea emerged that cellular immune defense in the mammary gland is a local feature of an organism-wide integrated system.
In the mouse, T-cell migration to the mammary gland was shown to be mediated by mucosal addressin cell-adhesion molecule-1 (MAdCAM-1) expressed on the mammary vascular endothelium [33], while IgA plasma cell recruitment was found to be facilitated by vascular cell-adhesion molecule (VCAM-1) [34]. These adhesion molecules were found to be present in different proportions in the ruminant mammary gland [35], possibly accounting for some of the differences between species of the immunoglobulin isotypes in colostrum or milk. Recent studies have established a role for chemokines in directing immune cells to the mammary gland. Mouse mammary tissue has been shown to express the CCL28 (MEC) chemokine receptor, which binds to the CCR10 ligand on IgA lymphocytes [36]. Despite these advances, the nature of the stimulus for the trafficking of IgA plasma cells from the intestine to the mammary gland, particularly in late-pregnancy, is as yet unknown.
Transport of IgA from immune cells in the mammary gland into colostrum and milk has been elucidated. Key to this was the identification of the polymeric immunoglobulin receptor (pIgR), a transmembrane glycoprotein selectively expressed on mucosal and secretory epithelial basolateral cell surfaces. Earlier studies had identified a ‘secretory component’ that was linked to dimeric IgA following its secretion into mucosal fluids [37]. This secretory component was later identified as the extracellular domain of pIgR. The transport of IgA involved binding to pIgR at the basolateral membrane, passage to the apical membrane then release into the alveolar lumen by cleavage of the complex, with IgA remaining linked to secretory component [38]. The pIgR protein was found to function as a sacrificial receptor, with one molecule of pIgR synthesised for every molecule of immunoglobulin secreted. The production of pIgR appears to limit the amount of IgA that is transported. Transgenic mice overexpressing pIgR in their mammary glands had double the IgA concentration in their milk compared with non-transgenic mice [39]. The expression of pIgR was shown to be under endocrine control in some tissues [40]. Prolactin and glucocorticoids were shown to enhance mammary pIgR protein and mRNA levels during lactation in the sheep [41].
Secretory component was found to be important for the function of IgA. When bound to IgA, it conferred protection from proteolytic degradation in the intestine [42, 43], and its presence facilitated localization of IgA to mucus [44]. Free secretory component has antimicrobial properties in its own right. It was first isolated from bovine milk [45] and subsequent studies have demonstrated that it binds to fimbrial colonization factors on bacterial surfaces, thereby reducing their pathogenicity [46]. Free secretory component also binds the cytokine IL-8 thereby modifying the pro-inflammatory effects of this cytokine [47].
Immunomodulatory Properties of Milk
The immune cells in milk are an important aspect of the immunomodulatory activity of milk. The presence of cells in milk and their association with mammary infection was described in the early twentieth century [48, 49]. However, the types of cells, their origin and their role in prevention of infection within the gland were debated for many years, particularly in non-bovine species. Significant advances in immunological analytical techniques eventually led to characterisation of the cell types in milk of humans as well as several other species. It is now clear that the cells in mammary secretions of all species studied consist of neutrophils, macrophages, lymphocytes and a smaller percentage of epithelial cells. In general, macrophages are the major cell population in milk from the healthy lactating mammary gland, whereas neutrophils predominate during early inflammation. These cells play an important role in signalling the presence of pathogens to the systemic immune system and thereby mounting a local immune response against pathogens.
Neutrophils and macrophages also phagocytose and kill bacteria directly, and this activity is enhanced by opsonic immunoglobulins and complement present in milk. By the 1970s, most components of the complement system were described in human [50] and bovine milk and colostrum [51].
The immune cells in milk may also modulate the neonatal immune system. This idea was first raised as a result of observing an increased level of neutrophils in the colostrum of non-nursing mothers in the absence of infection [52]. Evidence of transfer of tuberculin sensitivity to suckling infants [53] was used to support this hypothesis, as was transfer of partial tolerance and graft-versus-host reactions in rodents [54]. Subsequent studies have confirmed that milk cells can traverse the neonatal intestinal epithelium in a range of species [55, 56]. However, other studies found no evidence for transfer of cells across the gut [57] or tuberculin-sensitivity via milk [58].
A more recent explanation for modulation of the neonatal immune system via the cells themselves, is the production of soluble immune mediators. These “lymphokines” were first described in the 1980s and shown to stimulate the immune cells in the suckling animal [58, 59]. Many studies have since revealed the large range of these proteins (now termed “cytokines”) present in human colostrum or milk. These include IL-1β, IL-6, IL-8, IL-10, IL-12, IL-18, IFN-γ, TNF-α, TGF-β, G-CSF, M-CSF, GM-CSF. These cytokines are thought to regulate the neonatal immune system in a variety of ways. For example, TGF-β has been proposed to reduce inflammatory reactions in the gut [60], to reduce allergy [61] and to stimulate intestinal IgA production [62]. Cyokines are also present in cow’s milk, with increased levels during infection (reviewed in [63]).
The advent of recombinant technology enabled the production of cytokines such as Il-1, IL-2, IFN-γ and GM-CSF which induce higher numbers of neutrophils and macrophages when infused into the bovine udder. This finding has led to the idea that cytokines may be used as immunotherapy for prevention of mastitis in cattle, but to date none have been commercialized for routine use.
In vitro studies carried out over the last 20 years suggest that the repertoire of immune factors in milk also includes immunomodulatory peptides derived from caseins or whey proteins. These peptides are receiving much attention as possible sources of ‘natural’ bioactivity with health benefits for the consumer (see [64]). Casein peptides have also been used to stimulate the innate immune system within the mammary gland and prevent infections within the udder of cows at drying off [65]. However, peptides from the A1 variant of β-casein have been proposed to be involved in the development of type 1 diabetes, an auto-immune related disease, largely on the basis of epidemiological evidence [66].
In the 1980s, nucleotides were found in milk and proposed as potential immune regulators. By the mid 1980s, dietary nucleotide/nucleosides were shown to modulate cell-mediated immunity and prevent infection in animals [67]. Since then several infant feeding studies using formula supplemented with nucleotides suggest they can influence immune cell development and reduce the incidence of diarrhea.
Long chain poly-unsaturated fatty acids (LC-PUFA) such as DHA (docosahexaenoic acids) and EPA (eicosapentaenoic acid) were also identified in the 1980s as possible candidates for immune modulation. This notion was based on the observation that the diets of Eskimo children have a high proportion of fish containing these fatty acids, as well as a low incidence of asthma [68]. Subsequent studies have shown that infants fed formula supplemented with DHA also have decreased incidence of bronchitis than infants fed un-supplemented formula [69]. Supplementation of a mother’s diet with LC-PUFA to enhance the immunomodulatory profile of breast milk is also receiving interest as a means to modify the infant’s immune system [70].
A common feature of the studies over the years is that human milk is a rich source of many of the above-mentioned immunomodulatory components. The elucidation of many of these compounds was driven by the idea that breast-feeding prevents gastrointestinal and respiratory infectious disease in infants, as initially documented in 1930s [71]. This concept has now been broadened to include potential role of immunomodulatory elements in development of atopic disease (allergy) in children. Concentrations of LCPUFA, cytokines, nucleotides and polyamines in breast milk have all been associated with development of atopy in infants. In addition, the proportion of neutrophils is significantly higher and macrophages is lower in milk from mothers with an infant suffering from atopic dermatitis [72]. As human milk cells are a major source of some of the cytokines, it is possible that this finding could explain the link between cytokines and allergy. In some studies, an infant’s risk of developing allergy has been linked to the mother, but not the father, having an allergy [73]. Thus, the association of a specific cytokine or fatty acid profile in breast milk with subsequent development of atopy in infants may simply relate to the mother’s history of atopy.
Interestingly, one study has suggested a reduction in atopic dermatitis in at risk infants (when at least one parent has an allergy) after 6 months feeding of a partially hydrolysed infant formula as opposed to breast milk [74]. In addition, it has been suggested that prolonged (>7.5 months) exclusive breast-feeding of high risk infants has been associated with increased risk of IgE mediated food allergy, asthma and atopy, and atopic dermatitis [75], although shorter periods of breast-feeding are likely to be protective [76]. These observations support the notion that the reduction in exposure of the infant’s immune system to foreign antigens at critical time points may be as important as the supply of immune factors from milk in the subsequent development of allergy in the infant. Much further work in these areas will be required to unravel the role of immune factors in colostrum and milk and development of mucosal immunity in infants.
Antimicrobial Proteins in Milk
Initial characterisation of the bactericidal components in milk was carried out in the 1920s. In 1922, Alexander Fleming [77] described a bacteriolytic activity which was present in a number of biological fluids, which he named lysozyme. Not long after, this activity was also described in milk [78]. About this time, what appeared to be a distinct antimicrobial action in milk was also described. This activity against streptococci was termed “lactenin” [79].
Improved techniques for protein analysis in the 1940s and 1950s led to the characterisation of these activities. The bactericidal activity of lysozyme was shown to be largely due to its ability to digest the complex polysaccharide component of the bacterial cell wall (reviewed in [80]). The isolation of lysozyme from human and cow’s milk was reported in the 1960s [81, 82], with human milk having by far the greater abundance. Milk was shown to contain at least two distinct lactenins [83]. One of these was an oxidase, termed lactoperoxidase [84], which had earlier been purified from cow’s milk [85]. Lactoperoxidase was subsequently shown to have antimicrobial activity against streptococci in the presence of peroxide and thiocyanate [86], thereby contributing to the antimicrobial activity of milk.
Other milk antimicrobial activities were also discovered. A fraction of cow’s milk with a distinctive red colour was described in 1939 [87] and iron-chelating activity in milk was noted in 1951 [88]. Later workers characterised the protein responsible and termed it red milk protein, lactotransferrin, lactosiderophilin or lactoferrin. Lactoferrin was shown to have a bacteriostatic effect against E. coli [89] as well as the fungus, Candida albicans [90]. The antimicrobial properties of lactoferrin were attributed to its ability to sequester iron from the surrounding solution, thereby depriving bacteria of a mineral necessary for its growth. Xanthine oxidoreductase activity was first reported in milk, in 1902 [91]. Its antimicrobial activity, when supplied with exogenous substrate, was demonstrated in 1943, and was attributed to the formation of peroxide [92, 93].
As a result of these studies, by the mid 1960s, there was an appreciation that the defense property of milk was more complicated than simply the presence of immunoglobulins [94, 95]. Nevertheless, immunoglobulin transfer to the neonate still dominated most studies on this topic at that time.
Further work in the 1970s provided more detail as to the function and biological role of antimicrobial milk proteins. Lactoferrin was found to be present in a number of additional secretions and fluids that are subject to pathogenic challenge [96], as well as in neutrophils [97], which play an important role in host defense. The level of lactoferrin in cow’s milk was shown to rise significantly during mastitis [98]. The iron binding properties, predominance of the apo form of the protein in milk and the iron sequestering mechanism for its bacteriostatic effect were all corroborated [99, 100]. Lactoferrin was also shown to have bactericidal as well as bacteriostatic activity, and that it could act on a wider range of microbes than just E. coli [101]. Its antimicrobial activity was found to be due in part to alternative mechanisms such as membrane disruption, which was attributed to proteolytic cleavage products of lactoferrin, termed lactoferricins [102]. Lactoferrin has also been shown to have activity against a range of viruses, an activity that appears largely due to its binding to viral particles, thereby blocking virus entry to the cell (reviewed in [103].
The bactericidal actions of the enzymes in milk have been characterised in greater detail. The substrates for lactoperoxidase, hydrogen peroxide and thiocyanate, were shown to be produced by streptococci and liver detoxification pathways acting on dietary glucosinolates, respectively [104]. Lactoperoxidase was shown to produce a range of highly reactive groups which were thought to react with and disrupt the bacterial cell membranes (reviewed in [105, 106]). In addition to streptococci, this antimicrobial system was also found to act against a range of coliforms and Pseudomonas species, providing there was a source of peroxide [107, 108]. Xanthine oxidoreductase was shown to contribute to the lactoperoxidase antimicrobial system by supplying it with hydrogen peroxide [109]. Further evidence for the host defense role of xanthine oxidoreductase included: its production of a range of potentially bactericidal reactive oxygen species [110]; its increased abundance in neutrophils during infection [111]; and its inhibition being associated with an increase in microbial activity [112]. Lysozyme was shown to attack the cell walls of Gram positive bacteria by cleaving the glycosidic bond of N-acetylmuramic acid within the peptidoglycan molecule [113]. Lysozyme was identified in the secretory granules of neutrophils [114], associated with lactoferrin [115]. Proteolytic fragments of the caseins in milk were also shown to have antimicrobial activity (reviewed in [116]), suggesting that the proteases in milk as well as the major milk proteins themselves may also play a role in host defense.
By the late 1990s, a considerable body of knowledge had been accumulated as to the composition and mode of action of a range of antimicrobial proteins in milk. Yet, the understanding of host defense in milk was essentially the same as in the 1960s. However, around this time significant new insights were gained into the nature of innate immunity in vertebrates. These included the extensive cross-talk between the innate and acquired immune system, the first elucidation of the molecular mechanisms for pathogen recognition and identification of components of the signal transduction cascade leading to specific effector responses (reviewed in [117]). Identification of some of the components of host defense mechanisms in plants, insects and amphibians led to the discovery of equivalent systems in mammals, including the β-defensin and cathelicidin families of cationic antimicrobial peptides (reviewed in [118, 119]). This rapid series of discoveries energized the field of mammalian innate immunity, and provided a fresh approach to investigating the host defense properties of milk.
As a result, additional immune components of milk were identified. Members of the β-defensin family were found to be expressed by mammary epithelial cells with expression of their genes induced during mastitis [120, 121]. Members of the β-defensin and cathelicidin families were also found in milk and some at elevated levels in colostrum [122, 123]. A variant of an acute phase protein, serum amyloid A3, was found to be expressed in mammary cells in response to pathogens or pathogen-derived lipoteichoic acid and to be present in milk during mastitis [124], suggesting a role for this milk protein in host defense.
The repertoire of putative immune factors in milk continues to grow. A member of the RNAse family of proteins, angiogenin, has been known to be present in milk since the 1980s [125]. More recently, a host defense role was claimed for this protein, based on the discovery that mouse and human angiogenins have antimicrobial activity [126]. This role in milk is still to be verified, but is supported by the observation that other members of the RNase family are found in neutrophils and have antimicrobial as well as antiviral activities [127, 128].
Future Directions
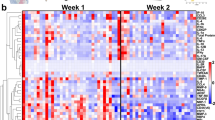
It is almost axiomatic that much remains to be discovered about the innate host defense system in the mammary gland and its secretions. The potential of the recently developed technologies of genomics, transcriptomics and proteomics to shed light on the biology of milk and the mammary gland have yet to be fully realised. Gene expression studies using microarrays and proteomics published to date have revealed a hitherto hidden complexity of the host defense-associated proteins in milk and the immune response of the mammary gland [129–134]. These techniques are likely to result in the identification of yet more components contributing to the host defense property of milk and colostrum.
A few fundamental questions remain to be answered. The regulation of the milk host defense system is not well understood. For example, the mechanisms responsible for differences in the composition of colostrum and milk between species and between stages of lactation have yet to be described. It is conceivable that these might involve epigenetic mechanisms. Also, the mechanisms by which pathogens are recognised by the host defense system is still a relatively unexplored area. Proteins such as Lipopolysaccharide Binding Protein (LBP) and Bactericidal/Permeability-Increasing Protein (BPI) have a key role in the systemic response to pathogens by binding to pathogen-derived compounds and presenting them to receptors on immune cells. It seems likely that an analogous system for pathogen recognition exists in milk, but to date this has not been described.
The biological roles of many of the known milk host defense components have still to be fully elucidated. The multifunctional nature of some of these has recently been suggested, for example the immunomodulatory properties of lactoferrin and some antimicrobial peptides known to be present in milk [135, 136]. To date most work on the proteins in mammary secretions has concentrated on the suppression of pathogens, while other possible functions have been under-represented in the literature. The immune system is known to play a role in mammary development and involution, as well as responding to neoplasia. It will be interesting to learn to what extent the proteins in milk contribute to these processes. Another current question is the extent of co-operativity and complementarity between the various components, as well as the nature of the mechanisms by which collectively they suppress the viability, growth, or virulence of pathogens of the mammary gland and neonatal GI tract. The possible synergies between the different proteins have not been thoroughly explored. Rather than consisting simply of immunoglobulins and a few minor milk proteins with inherent antimicrobial properties, it is now perhaps appropriate to view the defense system in mammary secretions as comprising a single integrated system. Thus in the future the application of a systems biology approach may be useful.
The host defense proteins in milk have many possible practical applications. The use of bovine milk extracts as natural food preservatives and functional food ingredients are two potential uses, and these are already beginning to be explored. One example of this is the supplementation of infant’s formula and other consumer milk-based products with lactoferrin. Individual components of milk are already being used therapeutically. For example, colostral IgG purified from cows immunised with E. coli is being marketed as a product to prevent travellers’ diarrhea. IgA has perhaps even more potential in this area, as it has better stability in the GI tract [137]. In the future, milk proteins with intrinsic bactericidal activity may be alternatives or supplements to traditional antibiotics, for which there is an increasing need [138]. It has also been suggested that the LPS-binding activity of lactoferrin could be used therapeutically [139]. Other potential uses are in dairying. For example, antimicrobial proteins have been expressed in cow’s milk, either through production of transgenic cattle or by transfection of mammary cells in vivo, thereby enhancing the animal’s resistance to mastitis [140, 141]. It is conceivable that in the future, the level of the endogenous host defense components in milk could be enhanced by inducing their over-expression through animal management approaches. Finally, detection of components of the host defense in milk could conceivably be used to detect mastitis in dairy cows. Similarly, their genes could be used as the basis for genetic selection for resistance to mastitis. Each of these applications has particular functional requirements that will need to be met. Future work will determine to what extent these potential uses are realised.
Abbreviations
- BPI:
-
bactericidal/permeability increasing protein
- DHA:
-
docosahexaenoic acids
- EPA:
-
eicosapentaenoic acid
- IgA:
-
immunoglobulin A
- IgG:
-
immunoglobulin G
- LBP:
-
lipopolysaccharide binding protein
- LC-PUFA:
-
long chain-polyunsaturated fatty acids
References
Kitasato S. Das Verhalten der Cholerabacterien in der Milch. Z Hyg Infektionskrankh 1889;5:491–6.
Fokker AP. Ueber bacterienvernichtende Eigenschaften der Milch. Z Hyg Infektionskrankh 1890;9:41–55.
Ehrlich P. Ueber Immunität durch Vererbung und Säugung. Z Hyg Infektionskr 1892;12:183–203.
Isaacs CE. The antimicrobial function of milk lipids. Adv Nutr Res 2001;10:271–85.
Newburg DS. Innate immunity and human milk. J Nutr 2005;135(5):1308–12.
Ehrlich P, Brieger L. Beiträge zur Kenntnis der Milch immunisirter Thiere. Z Hyg Infektionskr 1893;13:336–46.
Campbell B, Petersen WE. Immune milk—a historical survey. Dairy Sci Abst 1963;25(9):345–58.
Famulener LW. On the transmission of immunity from mother to offspring. J Infect Disease 1912;10:332–40.
Orcutt ML, Howe PE. The relation between the accumulation of globulins and the appearance of agglutinins in the blood of new-born calves. J Exp Med 1922;36:291–308.
Smith T, Little RB. The significance of colostrum to the new-born calf. J Exp Med 1922;36:181–98.
Little RB, Orcutt ML. The transmission of agglutinins of Bacillus abortus from cow to calf in the colostrum. J Exp Med 1922;35:161–71.
Ratner B, Jackson HC, Gruehl HL. Transmission of protein hypersensitiveness from mother to offspring: I. Critique of placental permeability. J Immunol 1927;14:249–65.
Ratner B, Jackson HC, Gruehl HL. Transmission of protein hypersensitiveness from mother to offspring: II. The role of colostrum. J Immunol 1927;14:267–74.
Ratner B, Jackson HC, Gruehl HL. Transmission of protein hypersensitiveness from mother to offspring: III. The rôle of milk. J Immunol 1927;14:275–90.
Smith T. The immunological significance of colostrum. I. The relationship between colostrum, serum, and the milk of cows normal and immunized towards B. coli. J Exp Med 1930;51:473–81.
Ingram PL, Lovell R, Wood PC, Aschaffenburg R, Bartlett S, Kon SK, et al. Bacterium coli antibodies in colostrum and their relation to calf survival. J Pathol Bacteriol 1956;72:561–8.
Lascelles AK. A review of the literature on some aspects of immune milk. Dairy Sci Abstr 1963;25(9):359–64.
Richards CB, Marrack JR. Sheep serum gamma globulin. In: Peeters H, editor. Protides of the biological fluids bruges. Amsterdam: Elsevier Science; 1963. p. 154–156.
Hanson LA. Comparative immunological studies of the immune globulins of human milk and of blood serum. Int Arch Allergy Appl Immunol 1961;18:241–67.
Campbell B, Porter RM, Petersen WE. Plasmacytosis of the bovine udder during colostrum secretion and experimental cessation of milking. Nature 1950;166(4230):913.
Lee CS, Lascelles AK. Antibody-producing cells in antigenically stimulated mammary glands and in the gastro-intestinal tract of sheep. Aust J Exp Biol Med Sci 1970;48(5):525–35.
Blakemore F, Garner RJ. The maternal transference of antibodies in the bovine. J Comp Pathol 1956;66(4):287–9.
Butler JE. Characteristics of bovine immunoglobulins and related molecules. Review of the bovine immunoglobulins. J Dairy Sci 1971;54(9):1315–6.
Jones EA, Waldmann TA. The mechanism of intestinal uptake and transcellular transport of IgG in the neonatal rat. J Clin Invest 1972;51(11):2916–27.
Kemler R, Mossmann H, Strohmaier U, Kickhofen B, Hammer DK. In vitro studies on the selective binding of IgG from different species to tissue sections of the bovine mammary gland. Eur J Immunol 1975;5(9):603–8.
Barrington GM, Besser TE, Gay CC, Davis WC, Reeves JJ, McFadden TB, et al. Regulation of the immunoglobulin G1 receptor: effect of prolactin on in vivo expression of the bovine mammary immunoglobulin G1 receptor. J Endocrinol 1999;163(1):25–31.
Smith KL, Muir LA, Ferguson LC, Conrad HR. Selective transport of IgGl into the mammary gland: role of estrogen and progesterone. J Dairy Sci 1971;54(12):1886–94.
Lascelles AK, McDowell GH. Localized humoral immunity with particular reference to ruminants. Transplant Rev 1974;19(0):170–208.
Barrington GM, Besser TE, Gay CC, Davis WC, Reeves JJ, McFadden TB. Effect of prolactin on in vitro expression of the bovine mammary immunoglobulin G1 receptor. J Dairy Sci 1997;80(1):94–100.
Roux ME, McWilliams M, Phillips-Quagliata JM, Weisz-Carrington P, Lamm ME. Origin of IgA-secreting plasma cells in the mammary gland. J Exp Med 1977;146(5):1311–22.
Weisz-Carrington P, Roux ME, Lamm ME. Plasma cells and epithelial immunoglobulins in the mouse mammary gland during pregnancy and lactation. J Immunol 1977;119(4):1306–7.
McDermott MR, Bienenstock J. Evidence for a common mucosal immunologic system. I. Migration of B immunoblasts into intestinal, respiratory, and genital tissues. J Immunol 1979;122(5):1892–8.
Tanneau GM, Oyant LHS, Chevaleyre CC, Salmon HP. Differential recruitment of T- and IgA B-lymphocytes in the developing mammary gland in relation to homing receptors and vascular addressins. J Histochem Cytochem 1999;47(12):1581–92.
Finke D, Acha-Orbea H. Differential migration of in vivo primed B and T lymphocytes to lymphoid and non-lymphoid organs. Eur J Immunol 2001;31(9):2603–11.
Hodgkinson AJ, Carpenter EA, Smith CS, Molan PC, Prosser CG. Adhesion molecule expression in the bovine mammary gland. Vet Immunol Immunopathol 2007;115(3–4):205–15.
Wilson E, Butcher EC. CCL28 controls immunoglobulin (Ig)A plasma cell accumulation in the lactating mammary gland and IgA antibody transfer to the neonate. J Exp Med 2004;200(6):805–9.
Crago SS, Kulhavy R, Prince SJ, Mestecky J. Secretory component of epithelial cells is a surface receptor for polymeric immunoglobulins. J Exp Med 1978;147(6):1832–7.
Apodaca G, Katz LA, Mostov KE. Receptor-mediated transcytosis of IgA in MDCK cells is via apical recycling endosomes. J Cell Biol 1994;125(1):67–86.
de Groot N, Van Kuik-Romeijn P, Lee SH, De Boer HA. Increased immunoglobulin A levels in milk by over-expressing the murine polymeric immunoglobulin receptor gene in the mammary gland epithelial cells of transgenic mice. Immunology 2000;101(2):218–24.
Rosato R, Jammes H, Belair L, Puissant C, Kraehenbuhl JP, Djiane J. Polymeric-Ig receptor gene expression in rabbit mammary gland during pregnancy and lactation: evolution and hormonal regulation. Mol Cell Endocrinol 1995;110(1–2):81–7.
Rincheval-Arnold A, Belair L, Djiane J. Developmental expression of pIgR gene in sheep mammary gland and hormonal regulation. J Dairy Res 2002;69(1):13–26.
Brown WR, Newcomb RW, Ishizaka K. Proteolytic degradation of exocrine and serum immunoglobulins. J Clin Invest 1970;49(7):1374–80.
Shuster J. Pepsin hydrolysis of IgA-delineation of two populations of molecules. Immunochemistry 1971;8(5):405–11.
Phalipon A, Cardona A, Kraehenbuhl JP, Edelman L, Sansonetti PJ, Corthesy B. Secretory component: a new role in secretory IgA-mediated immune exclusion in vivo. Immunity 2002;17(1):107–15.
Groves ML, Gordon WG. Isolation of a new glycoprotein-a and a gamma-G-globulin from individual cow milks. Biochemistry 1967;6(8):2388–94.
de Oliveira IR, de Araujo AN, Bao SN, Giugliano LG. Binding of lactoferrin and free secretory component to enterotoxigenic Escherichia coli. FEMS Microbiol Lett 2001;203(1):29–33.
Marshall LJ, Perks B, Ferkol T, Shute JK. IL-8 released constitutively by primary bronchial epithelial cells in culture forms an inactive complex with secretory component. J Immunol 2001;167(5):2816–23.
Breed RS. The sanitary significance of body cells in milk.. J Infect Dis. 1914;14:93–9.
Holm GC. The types of leucocytes in market milk as related to bovine mastitis. J Am Vet Med Assoc 1934;35:735–46.
Nakajima S, Baba AS, Tamura N. Complement system in human colostrum: presence of nine complement components and factors of alternative pathway in human colostrum. Int Arch Allergy Appl Immunol 1977;54(5):428–33.
Reiter B, Brock JH. Inhibition of Escherichia coli by bovine colostrum and post-colostral milk. I. Complement-mediated bactericidal activity of antibodies to a serum susceptible strain of E. coli of the serotype O 111. Immunology 1975;28(1):71–82.
Smith CW, Goldman AS. The cells of human colostrum .I. In vitro studies of morphology and functions. Pediatr Res 1968;2(2):103–9.
Mohr JA. The possible induction and-or acquisition of cellular hypersensitivity associated with ingestion of colostrum. J Pediatr 1973;82(6):1062–4.
Beer AE, Billington RE, Head JR. Natural transplantation of leukocytes during suckling. Transplant Proc 1975;7:399–402.
Weiler IJ, Hickler W, Sprenger R. Demonstration that milk cells invade the suckling neonatal mouse. Am J Reprod Immunol 1983;4(2):95–8.
Sheldrake RF, Husband AJ. Intestinal uptake of intact maternal lymphocytes by neonatal rats and lambs. Res Vet Sci 1985;39(1):10–5.
Miller SC. Failure to demonstrate morphologically the presence of colostral or milk cells in the wall of the gastrointestinal tract of the suckling neonatal mouse. J Reprod Immunol 1981;3(3):187–94.
Keller MA, Kidd RM, Bryson YJ, Turner JL, Carter J. Lymphokine production by human milk lymphocytes. Infect Immun 1981;32(2):632–6.
Lawton JW, Shortridge KF, Wong RL, Ng MH. Interferon synthesis by human colostral leucocytes. Arch Dis Child 1979;54(2):127–30.
Donnet-Hughes A, Duc N, Serrant P, Vidal K, Schiffrin EJ. Bioactive molecules in milk and their role in health and disease: the role of transforming growth factor-beta. Immunol Cell Biol 2000;78(1):74–9.
Penttilla IA. Effects of transforming growth factor-beta and formula feeding on systemic immune responses to dietary beta-lactoglobulin in allergy-prone rats. Pediatr Res 2006;59:650–5.
Stavnezer J. Regulation of antibody production and class switching by TGF-beta. J Immunol 1995;155(4):1647–51.
Sordillo LM, Shafer-Weaver K, DeRosa D. Immunobiology of the mammary gland. J Dairy Sci 1997;80(8):1851–65.
Gauthier SF, Pouliot Y, Saint-Sauveur D. Immunomodulatory peptides obtained by the enzymatic hydrolysis of whey proteins. Int Dairy J 2006;16:1315–1323.
Silanikove N, Shapiro F, Shamay A, Leitner G. Role of xanthine oxidase, lactoperoxidase, and NO in the innate immune system of mammary secretion during active involution in dairy cows: manipulation with casein hydrolyzates. Free Radic Biol Med 2005;38(9):1139–51.
Elliott RB, Harris DP, Hill JP, Bibby NJ, Wasmuth HE. Type I (insulin-dependent) diabetes mellitus and cow milk: casein variant consumption. Diabetologia 1999;42(3):292–6.
Yu WH. Scientific rationale and benefits of nucleotide supplementation of infant formula. J Paediatr Child Health 2002;38:543–9.
Horrobin E. Low prevalences of coronary heart disease (CHD), psoriasis, asthma and rheumatoid arthritis in Eskimos: are they caused by high dietary intake of ecosapentaenoic acid (EPA), a genetic variation of essential fatty acid (EPA) metabolism or a combination of both? Med Hypothesis 1987;22:388–96.
Pastor N, Soler B, Mitmesser SH, Ferguson P, Lifschitz C. Infants fed docosahexaenoic acid- and arachidonic acid-supplemented formula have decreased incidence of bronchiolitis/bronchitis the first year of life. Clin Pediatr (Phila) 2006;45(9):850–5.
Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, et al. Maternal fish oil supplementation in pregnancy reduces interleukin-13 levels in cord blood of infants at high risk of atopy. Clin Exp Allergy 2003;33(4):442–8.
Grulee CG, Sanford HN, Herron PH. Breast and artificial feeding: influences on morbidity and mortality of twenty thousand infants. J Am Med Assoc 1934;103:735–9.
Jarvinen KM, Suomalainen H. Leucocytes in human milk and lymphocyte subsets in cow’s milk-allergic infants. Pediatr Allergy Immunol 2002;13(4):243–54.
Ruiz RG, Kemeny DM, Price JF. Higher risk of infantile atopic dermatitis from maternal atopy than from paternal atopy. Clin Exp Allergy 1992;22(8):762–6.
Han Y-S, Park H-Y, Ahn K-M, Lee J-S, Choi H-M, Lee S-I. Short-term effect of partially hydrolysed formula on the prevention of development of atopic dermatitis in infants at high risk. J Korean Med Sci 2003;18:547–51.
Saarinen KM, Savilahti E. Infant feeding patterns affect the subsequent immunological features in cow’s milk allergy. Clin Exp Allergy 2000;30(3):400–6.
Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol 2001;45(4):520–7.
Fleming A. On a remarkable bacteriolytic element found in tissues and secretions. Proc Roy Soc Ser Biol Sci 1922;93:306–17.
Bordet J, Bordet M. Le pouvoir bacteriolytique du colostrum et du lait. Compt Rend 1924;179:1109–13.
Jones FS, Little RB. The bactericidal properties of cow’s milk. J Exp Med 1927;45:319–35.
Salton MR. The properties of lysozyme and its action on microorganisms. Bacteriol Rev 1957;21(2):82–100.
Jolles P, Jolles J. Lysozyme from human milk. Nature 1961;192:1187–1188.
Chandan RC, Shahani KM, Holly RG. Lysozyme content of human milk. Nature 1964;204:76–7.
Auclair JE. Studies on the antibacterial properties of cow’s milk. PhD Thesis, University of Reading 1953.
Wright RC, Tramer J. Factors influencing the activity of cheese starters. The role of milk peroxidase. J Dairy Res 1958;25:104–18.
Theorell H, Akeson A. Highly purified milk peroxidase. Ark Kemi Mineral Geol 1943;B17(7):1–6.
Jago GR, Morrison M. Anti-streptococcal activity of lactoperoxidase III. Proc Soc Exp Biol Med 1962;111:585–8.
Sorensen M, Sorensen SPL. The proteins in whey. C R Trav Lab Carlsberg 1939;23:55–99.
Schäfer KH. Elektrophoretische Untersuchengen zum Milchweissproblem. Monatsschr Kinderheilkd 1951;99:69.
Oram JD, Reiter B. Inhibition of bacteria by lactoferrin and other iron-chelating agents. Biochim Biophys Acta 1968;170(2):351–65.
Kirkpatrick CH, Green I, Rich RR, Schade AL. Inhibition of growth of Candida albicans by iron-unsaturated lactoferrin: relation to host-defense mechanisms in chronic mucocutaneous candidiasis. J Infect Dis 1971;124(6):539–44.
Schardinger F. Ueber das Verhalten der Kuhmilch gegen Methylenblau und seine Verwendung sur Unterscheidung von ungekochter und gekochter Milch. Z Unters Nahr Genussm 1902;5:1113–21.
Green DE, Pauli R. The antibacterial action of the xanthine oxidase system. Proc Soc Exp Biol Med 1943;54:148–50.
Lipmann F, Owen CR. The antibacterial effect of enzymatic xanthine oxidation. Science 1943;98:246–8.
Gyorgy P, Dhanamitta S, Steers E. Protective effects of human milk in experimental staphylococcus infection. Science 1962;137:338–40.
Reiter B, Oram J. Bacterial inhibitors in milk and other biological fluids. Nature 1967;216:328–30.
Masson PL, Heremans JF, Dive C. An iron-binding protein common to many external secretions. Clin Chim Acta 1966;14:735–739.
Masson PL, Heremans JF, Schonne E. Lactoferrin, an iron-binding protein in neutrophilic leukocytes. J Exp Med 1969;130(3):643–58.
Harmon RJ, Schanbacher FL, Ferguson LC, Smith KL. Concentration of lactoferrin in milk of normal lactating cows and changes occurring during mastitis. Am J Vet Res 1975;36(7):1001–7.
Masson PL, Heremans JF. Metal-combining properties of human lactoferrin (red milk protein). 1. The involvement of bicarbonate in the reaction. Eur J Biochem 1968;6(4):579–84.
Goldsmith SJ, Eitenmiller RR, Barnhart HM, Toledo RT, Rao VN. Unsaturated iron-binding capacity of human milk. J Food Sci 1982;47:1298–304.
Arnold RR, Brewer M, Gauthier JJ. Bactericidal activity of human lactoferrin: sensitivity of a variety of microorganisms. Infect Immun 1980;28(3):893–8.
Tomita M, Bellamy W, Takase M, Yamauchi K, Wakabayashi H, Kawase K. Potent antibacterial peptides generated by pepsin digestion of bovine lactoferrin. J Dairy Sci 1991;74(12):4137–42.
van der Strate BW, Beljaars L, Molema G, Harmsen MC, Meijer DK. Antiviral activities of lactoferrin. Antiviral Res 2001;52(3):225–39.
Reiter B. The lactoperoxidase-thiocyanate-hydrogen peroxide antibacterium system. Ciba Found Symp 1978;65:285–94.
de Wit JN, Hooydonk ACM. Structure, functions and applications of lactoperoxidase in natural antimicrobial systems. Neth Milk Dairy J 1996;50:227–44.
Kussendrager KD, van Hooijdonk AC. Lactoperoxidase: physico-chemical properties, occurrence, mechanism of action and applications. Br J Nutr. 2000;84(Suppl 1):S19–S25.
Bjorck L, Rosen C, Marshall V, Reiter B. Antibacterial activity of the lactoperoxidase system in milk against pseudomonads and other gram-negative bacteria. Appl Microbiol 1975;30(2):199–204.
Reiter B, Marshall VM, Bjorck L, Rosen CG. Nonspecific bactericidal activity of the lactoperoxidases-thiocyanate-hydrogen peroxide system of milk against Escherichia coli and some gram-negative pathogens. Infect Immun 1976;13(3):800–7.
Bjorck L, Claesson O. Xanthine oxidase as a source of hydrogen peroxide for the lactoperoxidase system in milk. J Dairy Sci 1979;62:1211–5.
Hunt J, Massey V. Purification and properties of milk xanthine dehydrogenase. J Biol Chem 1992;267(30):21479–85.
Tubaro E, Lotti B, Santiangeli C, Cavallo G. Xanthine oxidase increase in polymorphonuclear leucocytes and macrophages in mice in three pathological situations. Biochem Pharmacol 1980;29(3):1945–8.
Bungener W. Influence of allopurinol on the multiplication of rodent malaria parasites. Tropenmed Parasitol 1974;25(3):309–12.
Chipman DM, Sharon N. Mechanism of lysozyme action. Science 1969;165(892):454–65.
Cohn ZA, Hirsch JG. The isolation and properties of the specific cytoplasmic granules of rabbit polymorphonuclear leucocytes. J Exp Med 1960;112:983–1004.
Leffell MS, Spitznagel JK. Association of lactoferrin with lysozyme in granules of human polymorphonuclear leukocytes. Infect Immun 1972;6(5):761–5.
Lahov E, Regelson W. Antibacterial and immunostimulating casein-derived substances from milk: casecidin, isracidin peptides. Food Chem Toxicol 1996;34(1):131–45.
Medzhitov R, Janeway CA Jr. Innate immunity: impact on the adaptive immune response. Curr Opin Immunol 1997;9(1):4–9.
Lehrer RI, Ganz T. Defensins of vertebrate animals. Curr Opin Immunol 2002;14(1):96–102.
Zanetti M. Cathelicidins, multifunctional peptides of the innate immunity. J Leukoc Biol 2004;75(1):39–48.
Goldammer T, Zerbe H, Molenaar A, Schuberth HJ, Brunner RM, Kata SR, et al. Mastitis increases mammary mRNA abundance of beta-defensin 5, toll-like-receptor 2 (TLR2), and TLR4 but not TLR9 in cattle. Clin Diagn Lab Immunol 2004;11(1):174–85.
Swanson K, Gorodetsky S, Good L, Davis S, Musgrave D, Stelwagen K, et al. Expression of a beta-defensin mRNA, lingual antimicrobial peptide, in bovine mammary epithelial tissue is induced by mastitis. Infect Immun 2004;72(12):7311–4.
Armogida SA, Yannaras NM, Melton AL, Srivastava MD. Identification and quantification of innate immune system mediators in human breast milk. Allergy Asthma Proc 2004;25(5):297–304.
Murakami M, Dorschner RA, Stern LJ, Lin KH, Gallo RL. Expression and secretion of cathelicidin antimicrobial peptides in murine mammary glands and human milk. Pediatr Res 2005;57(1):10–5.
McDonald TL, Larson MA, Mack DR, Weber A. Elevated extrahepatic expression and secretion of mammary-associated serum amyloid A 3 (M-SAA3) into colostrum. Vet Immunol Immunopathol 2001;83(3–4):203–11.
Maes P, Damart D, Rommens C, Montreuil J, Spik G, Tartar A. The complete amino acid sequence of bovine milk angiogenin. FEBS Lett 1988;241(1–2):41–5.
Hooper LV, Stappenbeck TS, Hong CV, Gordon JI. Angiogenins: a new class of microbicidal proteins involved in innate immunity. Nat Immunol 2003;4(3):269–73.
Egesten A, Dyer KD, Batten D, Domachowske JB, Rosenberg HF. Ribonucleases and host defense: identification, localization and gene expression in adherent monocytes in vitro. Biochim Biophys Acta 1997;1358(3):255–60.
Rosenberg HF, Domachowske JB. Eosinophils, eosinophil ribonucleases, and their role in host defense against respiratory virus pathogens. J Leukoc Biol 2001;70(5):691–8.
Donaldson L, Vuocolo T, Gray C, Strandberg Y, Reverter A, McWilliam S, et al. Construction and validation of a bovine innate immune microarray. BMC Genomics 2005;6:135.
Swanson KM, Henderson HV, Farr VC, Davis SR, Oden K, Stelwagen K, et al. The use of microarrays to investigate gene regulation in the bovine mammary gland during Streptococcus uberis mastitis. Proc NZ Soc Anim Prod 2004;64:14–6.
Stein T, Morris JS, Davies CR, Weber-Hall SJ, Duffy MA, Heath VJ, et al. Involution of the mouse mammary gland is associated with an immune cascade and an acute-phase response, involving LBP, CD14 and STAT3. Breast Cancer Res 2004;6(2):R75–R91.
Clarkson RW, Wayland MT, Lee J, Freeman T, Watson CJ. Gene expression profiling of mammary gland development reveals putative roles for death receptors and immune mediators in post-lactational regression. Breast Cancer Res 2004;6(2):R92–R109.
Hogarth CJ, Fitzpatrick JL, Nolan AM, Young FJ, Pitt A, Eckersall PD. Differential protein composition of bovine whey: a comparison of whey from healthy animals and from those with clinical mastitis. Proteomics 2004;4(7):2094–100.
Smolenski G, Haines S, Kwan FY, Bond J, Farr V, Davis SR, et al. Characterisation of host defence proteins in milk using a proteomic approach. J Proteome Res 2007;6(1):207–15.
Takakura N, Wakabayashi H, Yamauchi K, Takase M. Influences of orally administered lactoferrin on IFN-gamma and IL-10 production by intestinal intraepithelial lymphocytes and mesenteric lymph-node cells. Biochem Cell Biol 2006;84(3):363–8.
Bowdish DM, Davidson DJ, Hancock RE. Immunomodulatory properties of defensins and cathelicidins. Curr Top Microbiol Immunol 2006;306:27–66.
Hodgkinson AJ, Cannon RD, Holmes AR, Fischer FJ, Willix-Payne DJ. Production from dairy cows of semi-industrial quantities of milk-protein concentrate (MPC) containing efficacious anti-Candida albicans IgA antibodies. J Dairy Res 2007;74(3):269–75.
Finlay BB, Hancock RE. Can innate immunity be enhanced to treat microbial infections? Nat Rev Microbiol 2004;2(6):497–504.
Caccavo D, Pellegrino NM, Altamura M, Rigon A, Amati L, Amoroso A, et al. Antimicrobial and immunoregulatory functions of lactoferrin and its potential therapeutic application. J Endotoxin Res 2002;8(6):403–17.
Kerr DE, Plaut K, Bramley AJ, Williamson CM, Lax AJ, Moore K, et al. Lysostaphin expression in mammary glands confers protection against staphylococcal infection in transgenic mice. Nat Biotechnol 2001;19(1):66–70.
Sun H-C, Xue F-M, Qian K, Fang H-X, Qiu H-L, Zhang X-Y, et al. Intramammary expression and therapeutic effect of a human lysozyme-expressing vector for treating bovine mastitis. J Zhejiang Univ Science B 2006;7:324–330.
Acknowledgement
The authors wish to acknowledge the efforts of Claire Miller and the staff at the AgResearch, Ruakura Information Services section in procuring the sometimes obscure original literature.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wheeler, T.T., Hodgkinson, A.J., Prosser, C.G. et al. Immune Components of Colostrum and Milk—A Historical Perspective. J Mammary Gland Biol Neoplasia 12, 237–247 (2007). https://doi.org/10.1007/s10911-007-9051-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10911-007-9051-7