Abstract
Background and Aims
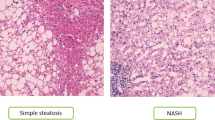
The prevalence of nonalcoholic fatty liver disease (NAFLD) and steatohepatitis (NASH) is increasing at an alarming rate. The role of bile acids in the development and progression of NAFLD to NASH and cirrhosis is poorly understood. This study aimed to quantify the bile acid metabolome in healthy subjects and patients with non-cirrhotic NASH under fasting conditions and after a standardized meal.
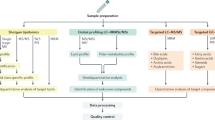
Methods
Liquid chromatography tandem mass spectroscopy was used to quantify 30 serum and 16 urinary bile acids from 15 healthy volunteers and 7 patients with biopsy-confirmed NASH. Bile acid concentrations were measured at two fasting and four post-prandial time points following a high-fat meal to induce gallbladder contraction and bile acid reabsorption from the intestine.
Results
Patients with NASH had significantly higher total serum bile acid concentrations than healthy subjects under fasting conditions (2.2- to 2.4-fold increase in NASH; NASH 2595–3549 µM and healthy 1171–1458 µM) and at all post-prandial time points (1.7- to 2.2-fold increase in NASH; NASH 4444–5898 µM and healthy 2634–2829 µM). These changes were driven by increased taurine- and glycine-conjugated primary and secondary bile acids. Patients with NASH exhibited greater variability in their fasting and post-prandial bile acid profile.
Conclusions
Results indicate that patients with NASH have higher fasting and post-prandial exposure to bile acids, including the more hydrophobic and cytotoxic secondary species. Increased bile acid exposure may be involved in liver injury and the pathogenesis of NAFLD and NASH.






Similar content being viewed by others
Abbreviations
- NAFLD:
-
Nonalcoholic fatty liver disease
- NASH:
-
Nonalcoholic steatohepatitis
- CA:
-
Cholate
- CDCA:
-
Chenodeoxycholate
- DCA:
-
Deoxycholate
- LCA:
-
Lithocholate
- HCA:
-
Hyocholate
- MCA:
-
Muricholate
- HDCA:
-
Hyodeoxycholate
- FXR:
-
Farnesoid X receptor
- PXR:
-
Pregnane X receptor
- NAS:
-
Nonalcoholic fatty liver disease activity score
- AUC:
-
Area under the curve
- OPLS-DA:
-
Orthogonal partial least squares-discriminant analysis
- HOMA-IR:
-
Homeostatic model for assessing insulin resistance
- BAAT:
-
Bile acid coenzyme A:amino acid N-acyltransferase
References
Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–1395.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609.
Perez MJ, Briz O. Bile-acid-induced cell injury and protection. World J Gastroenterol. 2009;15:1677–1689.
Neuman MG, French SW, French BA, et al. Alcoholic and non-alcoholic steatohepatitis. Exp Mol Pathol. 2014;97:492–510.
Trottier J, Bialek A, Caron P, Straka RJ, Milkiewicz P, Barbier O. Profiling circulating and urinary bile acids in patients with biliary obstruction before and after biliary stenting. PLoS One. 2011;6:e22094.
Mouzaki M, Comelli EM, Arendt BM, et al. Intestinal microbiota in patients with nonalcoholic fatty liver disease. Hepatology. 2013;58:120–127.
Ridlon JM, Kang DJ, Hylemon PB. Bile salt biotransformations by human intestinal bacteria. J Lipid Res. 2006;47:241–259.
Hofmann AF. Bile acids: the good, the bad, and the ugly. News Physiol Sci. 1999;14:24–29.
Jonker JW, Liddle C, Downes M. FXR and PXR: potential therapeutic targets in cholestasis. J Steroid Biochem Mol Biol. 2012;130:147–158.
Roberts RE, Glicksman C, Alaghband-Zadeh J, Sherwood RA, Akuji N, le Roux CW. The relationship between postprandial bile acid concentration, GLP-1, PYY and ghrelin. Clin Endocrinol. 2011;74:67–72.
Mudaliar S, Henry RR, Sanyal AJ, et al. Efficacy and safety of the farnesoid X receptor agonist obeticholic acid in patients with type 2 diabetes and nonalcoholic fatty liver disease. Gastroenterology. 2013;145:574–582.
Bechmann LP, Kocabayoglu P, Sowa JP, et al. Free fatty acids repress small heterodimer partner (SHP) activation and adiponectin counteracts bile acid-induced liver injury in superobese patients with nonalcoholic steatohepatitis. Hepatology. 2013;57:1394–1406.
Hardwick RN, Fisher CD, Canet MJ, Scheffer GL, Cherrington NJ. Variations in ATP-binding cassette transporter regulation during the progression of human nonalcoholic fatty liver disease. Drug Metab Dispos Biol Fate Chem. 2011;39:2395–2402.
Ferslew BC, Johnston CK, Tsakalozou E, et al. Altered morphine glucuronide and bile acid disposition in patients with non-alcoholic steatohepatitis. Clin Pharmacol Ther. 2015;97:419–427.
Jia X, Naito H, Yetti H, et al. Dysregulated bile acid synthesis, metabolism and excretion in a high fat-cholesterol diet-induced fibrotic steatohepatitis in rats. Dig Dis Sci. 2013;58:2212–2222.
Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146:1513–1524.
Kakiyama G, Hylemon PB, Zhou H, et al. Colonic inflammation and secondary bile acids in alcoholic cirrhosis. Am J Physiol Gastrointest Liver Physiol. 2014;306:G929–G937.
Kalhan SC, Guo L, Edmison J, et al. Plasma metabolomic profile in nonalcoholic fatty liver disease. Metab Clin Exp. 2011;60:404–413.
Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321.
Stone BG, Ansel HJ, Peterson FJ, Gebhard RL. Gallbladder emptying stimuli in obese and normal-weight subjects. Hepatology. 1992;15:795–798.
Xie G, Wang Y, Wang X, et al. Profiling of serum bile acids in a healthy Chinese population using UPLC-MS/MS. J Proteome Res. 2015;14:850–859.
Trottier J, Bialek A, Caron P, et al. Metabolomic profiling of 17 bile acids in serum from patients with primary biliary cirrhosis and primary sclerosing cholangitis: a pilot study. Dig Liver Dis. 2012;44:303–310.
Garcia-Canaveras JC, Donato MT, Castell JV, Lahoz A. Targeted profiling of circulating and hepatic bile acids in human, mouse, and rat using a UPLC-MRM-MS-validated method. J Lipid Res. 2012;53:2231–2241.
Tanaka N, Matsubara T, Krausz KW, Patterson AD, Gonzalez FJ. Disruption of phospholipid and bile acid homeostasis in mice with nonalcoholic steatohepatitis. Hepatology. 2012;56:118–129.
Aranha MM, Cortez-Pinto H, Costa A, et al. Bile acid levels are increased in the liver of patients with steatohepatitis. Eur J Gastroenterol Hepatol. 2008;20:519–525.
Russell DW. The enzymes, regulation, and genetics of bile acid synthesis. Annu Rev Biochem. 2003;72:137–174.
Lake AD, Novak P, Shipkova P, et al. Decreased hepatotoxic bile acid composition and altered synthesis in progressive human nonalcoholic fatty liver disease. Toxicol Appl Pharmacol. 2013;268:132–140.
Inagaki T, Moschetta A, Lee YK, et al. Regulation of antibacterial defense in the small intestine by the nuclear bile acid receptor. Proc Natl Acad Sci USA. 2006;103:3920–3925.
Thomas C, Gioiello A, Noriega L, et al. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10:167–177.
Watanabe M, Houten SM, Mataki C, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439:484–489.
Faubion WA, Guicciardi ME, Miyoshi H, et al. Toxic bile salts induce rodent hepatocyte apoptosis via direct activation of Fas. J Clin Investig. 1999;103:137–145.
Rodrigues CM, Fan G, Wong PY, Kren BT, Steer CJ. Ursodeoxycholic acid may inhibit deoxycholic acid-induced apoptosis by modulating mitochondrial transmembrane potential and reactive oxygen species production. Mol Med. 1998;4:165–178.
Spivey JR, Bronk SF, Gores GJ. Glycochenodeoxycholate-induced lethal hepatocellular injury in rat hepatocytes. Role of ATP depletion and cytosolic free calcium. J Clin Investig. 1993;92:17–24.
Rodrigues CM, Fan G, Ma X, Kren BT, Steer CJ. A novel role for ursodeoxycholic acid in inhibiting apoptosis by modulating mitochondrial membrane perturbation. J Clin Investig. 1998;101:2790–2799.
Bernstein H, Bernstein C, Payne CM, Dvorakova K, Garewal H. Bile acids as carcinogens in human gastrointestinal cancers. Mutat Res. 2005;589:47–65.
Baffy G, Brunt EM, Caldwell SH. Hepatocellular carcinoma in non-alcoholic fatty liver disease: an emerging menace. J Hepatol. 2012;56:1384–1391.
Larsson SC, Wolk A. Overweight, obesity and risk of liver cancer: a meta-analysis of cohort studies. Br J Cancer. 2007;97:1005–1008.
Larsson SC, Wolk A. Obesity and the risk of gallbladder cancer: a meta-analysis. Br J Cancer. 2007;96:1457–1461.
Reddy BS, Narasawa T, Weisburger JH, Wynder EL. Promoting effect of sodium deoxycholate on colon adenocarcinomas in germfree rats. J Natl Cancer Inst. 1976;56:441–442.
Zhang Y, Hagedorn CH, Wang L. Role of nuclear receptor SHP in metabolism and cancer. Biochim Biophys Acta. 1812;2011:893–908.
Acknowledgments
The authors would like to sincerely thank Drs. Nathan D. Pfeifer, Mary F. Paine, and Dhiren R. Thakker for insightful discussions throughout the development, conduct, and analysis of this study. The authors also would like to thank Kevin B. Harris and Dr. Eleftheria Tsakalozou for assistance with study conduct and data management, and Lisa Hardee for assistance performing FibroScan® measurements. Phoenix WinNonlin software was generously provided to the Division of Pharmacotherapy and Experimental Therapeutics, UNC Eshelman School of Pharmacy, by Certara as a member of the Pharsight Academic Center of Excellence Program. This project was supported in part by the National Institutes of Health, National Center for Advancing Translational Sciences (NCATS), through Award Number 1UL1TR001111, National Institute of General Medical Sciences through Award Number R01 GM041935 [K. L. R. B], an Amgen Predoctoral Fellowship in Pharmacokinetics and Drug Disposition [B. C. F.], and Quintiles Pharmacokinetics/Pharmacodynamics Fellowships [C. K. J.]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, Amgen or Quintiles.
Conflict of interest
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ferslew, B.C., Xie, G., Johnston, C.K. et al. Altered Bile Acid Metabolome in Patients with Nonalcoholic Steatohepatitis. Dig Dis Sci 60, 3318–3328 (2015). https://doi.org/10.1007/s10620-015-3776-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3776-8