Abstract
Background
Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are characterized by chronic intestinal inflammation due to immunological, microbial, and environmental factors in genetically predisposed individuals. Advances in the diagnosis, prognosis, and treatment of IBD require the identification of robust biomarkers that can be used for molecular classification of diverse disease presentations. We previously identified five genes, RELA, TNFAIP3 (A20), PIGR, TNF, and IL8, whose mRNA levels in colonic mucosal biopsies could be used in a multivariate analysis to classify patients with CD based on disease behavior and responses to therapy.
Aim
We compared expression of these five biomarkers in IBD patients classified as having CD or UC, and in healthy controls.
Results
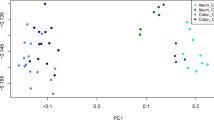
Patients with CD were characterized as having decreased median expression of TNFAIP3, PIGR, and TNF in non-inflamed colonic mucosa as compared to healthy controls. By contrast, UC patients exhibited decreased expression of PIGR and elevated expression of IL8 in colonic mucosa compared to healthy controls. A multivariate analysis combining mRNA levels for all five genes resulted in segregation of individuals based on disease presentation (CD vs. UC) as well as severity, i.e., patients in remission versus those with acute colitis at the time of biopsy.
Conclusion
We propose that this approach could be used as a model for molecular classification of IBD patients, which could further be enhanced by the inclusion of additional genes that are identified by functional studies, global gene expression analyses, and genome-wide association studies.


Similar content being viewed by others
References
Maher MM. Inflammatory bowel disease: review and future view. Front Biosci (Elite Ed). 2012;4:1638–1647.
Foersch S, Waldner MJ, Neurath MF. Innate and adaptive immunity in inflammatory bowel diseases. Dig Dis. 2013;31:317–320.
Van Assche G, Dignass A, Panes J, et al. The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohn’s Colitis. 2010;4:7–27.
Laass MW, Roggenbuck D, Conrad K. Diagnosis and classification of Crohn’s disease. Autoimmun Rev. 2014;13:467–471.
Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohn’s Colitis. 2012;6:965–990.
Conrad K, Roggenbuck D, Laass MW. Diagnosis and classification of ulcerative colitis. Autoimmun Rev. 2014;13:463–466.
Burisch J, Munkholm P. Inflammatory bowel disease epidemiology. Curr Opin Gastroenterol. 2013;29:357–362.
Feakins RM. Ulcerative colitis or Crohn’s disease? Pitfalls and problems. Histopathology. 2014;64:317–335.
Tontini GE, Vecchi M, Pastorelli L, et al. Differential diagnosis in inflammatory bowel disease colitis: state of the art and future perspectives. World J Gastroenterol. 2015;21:21–46.
Scaldaferri F, Correale C, Gasbarrini A, Danese S. Mucosal biomarkers in inflammatory bowel disease: key pathogenic players or disease predictors? World J Gastroenterol. 2010;16:2616–2625.
Vermeire S, Van Assche G, Rutgeerts P. Classification of inflammatory bowel disease: the old and the new. Curr Opin Gastroenterol. 2012;28:321–326.
Arsenescu R, Bruno ME, Rogier EW, et al. Signature biomarkers in Crohn’s disease: toward a molecular classification. Mucosal Immunol. 2008;1:399–411.
Eckmann L, Neish AS. NF-κB and mucosal homeostasis. Curr Top Microbiol Immunol. 2011;349:145–158. doi:10.1007/82_2010_103.
Pasparakis M. Role of NF-kappaB in epithelial biology. Immunol Rev. 2012;246:346–358.
Vereecke L, Sze M, Mc GC, et al. Enterocyte-specific A20 deficiency sensitizes to tumor necrosis factor-induced toxicity and experimental colitis. J Exp Med. 2010;207:1513–1523.
Kolodziej LE, Lodolce JP, Chang JE, et al. TNFAIP3 maintains intestinal barrier function and supports epithelial cell tight junctions. PLoS One. 2011;6:e26352.
Harhaj EW, Dixit VM. Regulation of NF-κB by deubiquitinases. Immunol Rev. 2012;246:107–124.
Ma A, Malynn BA. A20: linking a complex regulator of ubiquitylation to immunity and human disease. Nat Rev Immunol. 2012;12:774–785.
Rhee L, Murphy SF, Kolodziej LE, et al. Expression of TNFAIP3 in intestinal epithelial cells protects from DSS- but not TNBS-induced colitis. Am J Physiol Gastrointest Liver Physiol. 2012;303:G220–G227.
Shembade N, Harhaj EW. Regulation of NF-κB signaling by the A20 deubiquitinase. Cell Mol Immunol. 2012;9:123–130.
Johansen FE, Kaetzel CS. Regulation of the polymeric immunoglobulin receptor and IgA transport: new advances in environmental factors that stimulate pIgR expression and its role in mucosal immunity. Mucosal Immunol. 2011;4:598–602.
Frantz AL, Bruno ME, Rogier EW, et al. Multifactorial patterns of gene expression in colonic epithelial cells predict disease phenotypes in experimental colitis. Inflamm Bowel Dis. 2012;18:2138–2148.
Frantz AL, Rogier EW, Weber CR, et al. Targeted deletion of MyD88 in intestinal epithelial cells results in compromised antibacterial immunity associated with downregulation of polymeric immunoglobulin receptor, mucin-2, and antibacterial peptides. Mucosal Immunol. 2012;5:501–512.
Kaetzel CS. Cooperativity among secretory IgA, the polymeric immunoglobulin receptor, and the gut microbiota promotes host-microbial mutualism. Immunol Lett. 2014;162:10–21.
Rogier EW, Frantz AL, Bruno MEC, et al. Secretory antibodies in breast milk promote long-term intestinal homeostasis by regulating the gut microbiota and host gene expression. Proc Natl Acad Sci USA. 2014;111:3074–3079.
Slebioda TJ, Kmiec Z. Tumour necrosis factor superfamily members in the pathogenesis of inflammatory bowel disease. Mediat Inflamm. 2014;2014:325129.
Danese S, Colombel JF, Peyrin-Biroulet L, et al. Review article: the role of anti-TNF in the management of ulcerative colitis—past, present and future. Aliment Pharmacol Ther. 2013;37:855–866.
Oikonomopoulos A, van Deen WK, Hommes DW. Anti-TNF antibodies in inflammatory bowel disease: do we finally know how it works? Curr Drug Targets. 2013;14:1421–1432.
Goncalves NS, Ghaem-Maghami M, Monteleone G, et al. Critical role for tumor necrosis factor alpha in controlling the number of lumenal pathogenic bacteria and immunopathology in infectious colitis. Infect Immun. 2001;69:6651–6659.
Corredor J, Yan F, Shen CC, et al. Tumor necrosis factor regulates intestinal epithelial cell migration by receptor-dependent mechanisms. Am J Physiol Cell Physiol. 2003;284:C953–C961.
Bruno MEC, Kaetzel CS. Long-term exposure of the HT-29 human intestinal epithelial cell-line to TNF causes sustained up-regulation of the polymeric Ig receptor and pro-inflammatory genes through transcriptional and post-transcriptional mechanisms. J Immunol. 2005;174:7278–7284.
Dent G, Loweth SC, Hasan AM, Leslie FM. Synergic production of neutrophil chemotactic activity by colonic epithelial cells and eosinophils. Immunobiology. 2014;219:793–797.
Franke A, McGovern DP, Barrett JC, et al. Genome-wide meta-analysis increases to 71 the number of confirmed Crohn’s disease susceptibility loci. Nat Genet. 2010;42:1118–1125.
Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124.
Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a working party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005;19:5–36.
Bruno ME, Frantz AL, Rogier EW, et al. Regulation of the polymeric immunoglobulin receptor by the classical and alternative NF-κB pathways in intestinal epithelial cells. Mucosal Immunol. 2011;4:468–478.
Murthy AK, Dubose CN, Banas JA, et al. Contribution of polymeric immunoglobulin receptor to regulation of intestinal inflammation in dextran sulfate sodium-induced colitis. J Gastroenterol Hepatol. 2006;21:1372–1380.
Reikvam DH, Derrien M, Islam R, et al. Epithelial-microbial cross-talk in polymeric Ig receptor deficient mice. Eur J Immunol. 2012;42:2959–2970.
Acknowledgments
This work was supported by NIH/NIDCR Grant 5P20RR020145 to M.E.C.B. and R.I.A.; NIH Grant AI069027 (and an associated American Recovery and Reinvestment Act supplement) and a Senior Research Award from the Crohn’s and Colitis Foundation of America (CCFA) to C.S.K.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bruno, M.E.C., Rogier, E.W., Arsenescu, R.I. et al. Correlation of Biomarker Expression in Colonic Mucosa with Disease Phenotype in Crohn’s Disease and Ulcerative Colitis. Dig Dis Sci 60, 2976–2984 (2015). https://doi.org/10.1007/s10620-015-3700-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-015-3700-2