Abstract
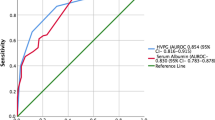
Background Patients with decompensated cirrhosis and acute liver failure have circulatory dysfunctions leading to high portal pressure and cardiac output (CO) and low systemic vascular resistance (SVR). Circulatory changes in acute-on-chronic liver failure (ACLF) patients have not been studied. We studied the portal, systemic, and pulmonary hemodynamics in patients with ACLF and compared them with compensated and decompensated cirrhotics. Patients and Methods Clinical features and hemodynamic profile were studied in patients with ACLF and compared with age- and sex-matched compensated and decompensated cirrhotics with portal hypertension. Results The study cohort comprised 144 patients categorized into one of three groups (ACLF, compensated cirrhosis, and decompensated cirrhosis), with 48 (33%) patients in each group. All values are given as the mean ± standard deviation, except for frequencies (%). The mean arterial pressure (MAP) and SVR were lower in the ACLF than the compensated group and were similar to those of the decompensated group (MAP 90 ± 16 vs. 99 ± 15 vs. 96 ± 16 mmHg; SVR 912 ± 435 vs. 1350 ± 449 vs. 891 ± 333 dyn s/cm5). The mean CO of the ACLF patients was higher than that of the compensated group and similar to that of the decompensated group (CO 8.9 ± 3.5 vs. 6.1 ± 1.7 vs. 9.0 ± 3.0 l/min). The pulmonary vascular resistance (PVR) and pulmonary capillary wedge pressures (PCWP) were similar in all the three groups (PVR 78 ± 48 vs. 109 ± 70 vs. 61 ± 47 dyn s/cm5; PCWP 8 ± 4 vs. 8 ± 4 vs. 10 ± 5 mmHg). The mean hepatic venous pressure gradient (HVPG) in the ACLF group was 15.1 ± 6.3 mmHg, which was significantly higher than that of the compensated group (11.7 ± 6.3 mmHg), but lower than that of the decompensated cirrhosis group (20.2 ± 6.0 mmHg). When patients of ACLF were categorized on the basis of their variceal size, the mean HVPG in ACLF patients with small varices was similar to that of compensated cirrhotics (13.7 ± 5.7 vs. 11.7 ± 6.3 mmHg; P = 0.146), while in the ACLF patients with large varices, the HVPG was comparable to that of the decompensated cirrhotics (18.7 ± 6.6 vs. 20.2 ± 6.0 mmHg; P = 0.442). Conclusions The systemic hemodynamics in patients with ACLF is similar to that in decompensated cirrhotics. The portal pressure in these patients is higher than that in the compensated cirrhotics, and in the subgroup with large varices, it becomes similar to that of decompensated cirrhotics.





Similar content being viewed by others
References
Sen S, Williams R, Jalan R (2002) The pathophysiological basis of acute-on-chronic liver failure. Liver 22[Suppl 2]:5–13. doi:10.1034/j.1600-0676.2002.00001.x
Ellis A, Wendon J (1996) Circulatory, respiratory, cerebral, and renal derangements in acute liver failure: Pathophysiology and management. Semin Liver Dis 16:379–388
Larsen FS, Ejlersen E, Hansen BA, Mogensen T, Tygstrup N, Secher NH (1995) Systemic vascular resistance during high-volume plasmapheresis in patients with fulminant hepatic failure: relationship with oxygen consumption. Eur J Gastroenterol Hepatol 7:887–892
Clemmesen JO, Larsen FS, Ejlersen E, Schiodt FV, Ott P, Hansen BA (1997) Haemodynamic changes after high-volume plasmapheresis in patients with chronic and acute liver failure. Eur J Gastroenterol Hepatol 9:55–60
Kowalski HJ, Abelmann WH (1953) The cardiac output at rest in Laennec’s cirrhosis. J Clin Invest 32:1025–1033. doi:10.1172/JCI102813
Kontos HA, Sharpiro W, Mauck HP, Patterson JL (1964) General and regional circulatory alterations in cirrhosis of the liver. Am J Med 37:526–535. doi:10.1016/0002-9343(64)90066-X
Henderson KM, Mackay GJ, Hooks M, Chezmar JL, Galloway JR, Dodson TF (1992) High cardiac output of advanced liver disease persists after orthotopic liver transplantation. Hepatology 15:258–262. doi:10.1002/hep. 1840150214
Newby DE, Jalan R, Masumori S, Hayes PC, Boon NA, Webb DJ (1998) Peripheral vascular tone in patients with cirrhosis: role of the renin-angiotensin and sympathetic nervous systems. Cardiovasc Res 38:221–228. doi:10.1016/S0008-6363(98)00008-X
Bosch J, Garcia-Pagan JC (2000) Complications of cirrhosis. I. Portal hypertension. J Hepatol 32[Suppl 1]:141–156. doi:10.1016/S0168-8278(00)80422-5
Navasa M, Garcia-Pagan JC, Bosch J, Riera JR, Banares R, Mas A et al (1992) Portal hypertension in acute liver failure. Gut 33:965–968. doi:10.1136/gut.33.7.965
de Franchis R (2005) Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol 43:167–176. doi:10.1016/j.jhep.2005.05.009
Wadhawan M, Dubey S, Sharma BC, Sarin SK, Sarin SK (2006) Hepatic venous pressure gradient in cirrhosis: correlation with the size of varices, bleeding, ascites, and child’s status. Dig Dis Sci 51:2264–2269. doi:10.1007/s10620-006-9310-2
Sarin SK, Lamba GS, Kumar M, Misra A, Murthy NS (1999) Comparison of endoscopic ligation and propranolol for the primary prevention of variceal bleeding. N Engl J Med 340:988–993. doi:10.1056/NEJM199904013401302
Groszmann RJ, Garcia-Tsao G, Bosch J, Grace ND, Burroughs AK, Planas R et al (2005) Portal Hypertension Collaborative Group. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med 353:2254–2261. doi:10.1056/NEJMoa044456
Groszmann RJ, Glickman M, Blei AT, Storer E, Conn HO (1979) Wedged and free hepatic venous pressure measured with a balloon catheter. Gastroenterology 76:253–258
Hoeper MM, Maier R, Tongers J, Niedermeyer J, Hohlfeld JM, Hamm M et al (1999) Determination of cardiac output by the Fick method, thermodilution, and acetylene rebreathing in pulmonary hypertension. Am J Respir Crit Care Med 160:535–541
Cardenas A, Gines P (2006) Hepatorenal syndrome. Clin Liver Dis 10:371–385. doi:10.1016/j.cld.2006.05.006
Groszmann RJ (1994) Vasodilatation and hyperdynamic circulatory state in chronic liver diseases. In: Bosch J, Groszmann RJ (eds) Portal hypertension: pathophysiology and treatment. Blackwell Science, Oxford, pp 17–26
Arroyo V, Jimenez W (2000) Complications of cirrhosis. II. Renal and circulatory dysfunction light. and shadows in an important clinical problem. J Hepatol 32[Suppl 1]:157–170. doi:10.1016/S0168-8278(00)80423-7
Schrier RW, Arroyo V, Bernardi M, Epstein M, Henriksen JH, Rodes J (1988) Peripheral arterial vasodilation hypothesis: a proposal for the initiation of renal sodium and water retention in cirrhosis. Hepatology 8:1151–1157. doi:10.1002/hep. 1840080532
Fernandez-Seara J, Prieto J, Quiroga J, Zozaya JM, Cobos MA, Rodriguez-Eire JL et al (1989) Systemic and regional hemodynamics in patients with liver cirrhosis and ascites with and without functional renal failure. Gastroenterology 97:1304–1312
Hadengue A, Lebrec D, Moreau R, Sogni P, Durand F, Gaudin C et al (1993) Persistence of systemic and splanchnic hyperkinetic circulation in liver transplant patients. Hepatology 17:175–178
Javle P, Yates J, Kynaston HG, Parsons KF, Jenkins SA (1998) Hepatosplanchnic haemodynamics and renal blood flow and function in rats with liver failure. Gut 43:272–279
Yu CH, Chen HL, Chen WT, Ni YH, Lin YL, Chang MH (2004) Portal hemodynamic changes after hepatocyte transplantation in acute hepatic failure. J Biomed Sci 11:756–763. doi:10.1007/BF02254360
Poynard T, Degott C, Munoz C, Lebrec D (1987) Relationship between degree of portal hypertension and liver histologic lesions in patients with alcoholic cirrhosis. Effect of acute alcoholic hepatitis on portal hypertension. Dig Dis Sci 32:337–343. doi:10.1007/BF01296284
Sen S, Mookerjee RP, Cheshire LM, Davies NA, Williams R, Jalan R (2005) Albumin dialysis reduces portal pressure acutely in patients with severe alcoholic hepatitis. J Hepatol 43:142–148. doi:10.1016/j.jhep. 2005.01.032
Catalina MV, Barrio J, Anaya F, Salcedo M, Rincon D, Clemente G et al (2003) Hepatic and systemic haemodynamic changes after MARS in patients with acute-on-chronic liver failure. Liver Int 23[Suppl 3]:39–43
Meyer RA, Duffy MC (1993) Spontaneous reactivation of chronic hepatitis B infection leading to fulminant hepatic failure. Report of two cases and review of the literature. J Clin Gastroenterol 17:231–234. doi:10.1097/00004836-199310000-00012
Bellis L, Castellacci R, Montagnese F, Festuccia F, Corvisieri P, Puoti C (2003) Hepatic venous pressure gradient determination in patients with hepatitis C virus-related and alcoholic cirrhosis. Eur J Gastroenterol Hepatol 15:1085–1089. doi:10.1097/00042737-200310000-00004
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kumar, A., Das, K., Sharma, P. et al. Hemodynamic Studies in Acute-on-Chronic Liver Failure. Dig Dis Sci 54, 869–878 (2009). https://doi.org/10.1007/s10620-008-0421-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-008-0421-9