Abstract
Purpose
To estimate the roles of extracellular vesicles (EVs) in tears and to determine whether their profiles are associated with the type of ocular disease.
Study design
Cross-sectional study.
Methods
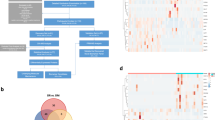
Tear EVs were extracted from 14 healthy participants and from 21 patients with retinal diseases (age-related macular degeneration [AMD] or diabetic macular edema [DME]). The surface marker expression of tear EVs was examined, and microRNAs (miRNAs) were extracted and profiled by use of real-time PCR array. The stability of the expression of the miRNAs was determined, and their functions were assessed by network analyses. Classification accuracy was evaluated by use of a random forest classifier and k-fold cross-validation.
Results
The miRNAs that were highly expressed in tear EVs were miR-323-3p, miR-548a-3p, and miR-516a-5p. The most stably expressed miRNAs independent of diseases were miR-520h and miR-146b-3p. The primary networks of the highly stably expressed endogenous miRNAs were annotated as regulation of organismal injury and abnormalities. The highly expressed miRNAs for severe retinal disease were miR-151-5p for AMD and miR-422a for DME, suggesting potential roles of tear EVs in liquid biopsy. Nine miRNAs (miR-25, miR-30d, miR-125b, miR-132, miR-150, miR-184, miR-342-3p, miR-378, and miR-518b) were identified as distinguishing individuals with AMD from healthy individuals with a classification accuracy of 91.9%.
Conclusions
The finding that tear EVs contain characteristic miRNA species indicates that they may help in maintaining homeostasis and serve as a potential tool for disease diagnosis.






Similar content being viewed by others
References
Cappello F, Logozzi M, Campanella C, Bavisotto CC, Marcilla A, Properzi F, et al. Exosome levels in human body fluids: a tumor marker by themselves? Eur J Pharm Sci. 2017;96:93–8.
Grigor’eva AE, Tamkovich SN, Eremina AV, Tupikin AE, Kabilov MR, Chernykh VV, et al. Exosomes in tears of healthy individuals: isolation, identification, and characterization. Biochem Moscow Suppl Ser B Biomed Chem. 2016;10:165–72.
Dilsiz N. Role of exosomes and exosomal microRNAs in cancer. Future Sci OA. 2020;6:FSO465.
Howitt J, Hill AF. Exosomes in the pathology of neurodegenerative diseases. J Biol Chem. 2016;291:26589–97.
Zamani P, Fereydouni N, Butler AE, Navashenaq JG, Sahebkar A. The therapeutic and diagnostic role of exosomes in cardiovascular diseases. Trends Cardiovasc Med. 2019;29:313–23.
Zhang Z, Liang X, Zhou J, Meng M, Gao Y, Yi G, et al. Exosomes in the pathogenesis and treatment of ocular diseases. Exp Eye Res. 2021;209:108626.
Thery C, Witwer KW, Aikawa E, Alcaraz MJ, Anderson JD, Andriantsitohaina R, et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles. 2018;7:1535750.
Yoshioka Y, Kosaka N, Konishi Y, Ohta H, Okamoto H, Sonoda H, et al. Ultra-sensitive liquid biopsy of circulating extracellular vesicles using ExoScreen. Nat Commun. 2014;5:3591.
Zhou L, Chen F, Ye J, Pan H. Selection of reliable reference genes for RT-qPCR analysis of Bursaphelenchus mucronatus gene expression from different habitats and developmental stages. Front Genet. 2018;9:269.
Pfaffl MW, Tichopad A, Prgomet C, Neuvians TP. Determination of stable housekeeping genes, differentially regulated target genes and sample integrity: BestKeeper–Excel-based tool using pair-wise correlations. Biotechnol Lett. 2004;26:509–15.
Silver N, Best S, Jiang J, Thein SL. Selection of housekeeping genes for gene expression studies in human reticulocytes using real-time PCR. BMC Mol Biol. 2006;7:33.
Vandesompele J, De Preter K, Pattyn F, Poppe B, Van Roy N, De Paepe A, et al. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol. 2002;3:RESEARCH0034.
Andersen CL, Jensen JL, Orntoft TF. Normalization of real-time quantitative reverse transcription-PCR data: a model-based variance estimation approach to identify genes suited for normalization, applied to bladder and colon cancer data sets. Cancer Res. 2004;64:5245–50.
Feng Z, Zhang C, Wu R, Hu W. Tumor suppressor p53 meets microRNAs. J Mol Cell Biol. 2011;3:44–50.
Tarasov V, Jung P, Verdoodt B, Lodygin D, Epanchintsev A, Menssen A, et al. Differential regulation of microRNAs by p53 revealed by massively parallel sequencing: miR-34a is a p53 target that induces apoptosis and G1-arrest. Cell Cycle. 2007;6:1586–93.
Zhang J, Sun Q, Zhang Z, Ge S, Han ZG, Chen WT. Loss of microRNA-143/145 disturbs cellular growth and apoptosis of human epithelial cancers by impairing the MDM2-p53 feedback loop. Oncogene. 2013;32:61–9.
Garibaldi F, Falcone E, Trisciuoglio D, Colombo T, Lisek K, Walerych D, et al. Mutant p53 inhibits miRNA biogenesis by interfering with the microprocessor complex. Oncogene. 2016;35:3760–70.
Redshaw N, Camps C, Sharma V, Motallebipour M, Guzman-Ayala M, Oikonomopoulos S, et al. TGF-beta/Smad2/3 signaling directly regulates several miRNAs in mouse ES cells and early embryos. PLoS ONE. 2013;8:e55186.
Du T, Zamore PD. microPrimer: the biogenesis and function of microRNA. Development. 2005;132:4645–52.
Men Y, Yelick J, Jin S, Tian Y, Chiang MSR, Higashimori H, et al. Exosome reporter mice reveal the involvement of exosomes in mediating neuron to astroglia communication in the CNS. Nat Commun. 2019;10:4136.
Nolte-’t Hoen EN, Buschow SI, Anderton SM, Stoorvogel W, Wauben MH. Activated T cells recruit exosomes secreted by dendritic cells via LFA-1. Blood. 2009;113:1977–81.
Zhang B, Wang M, Gong A, Zhang X, Wu X, Zhu Y, et al. HucMSC-exosome mediated-Wnt4 signaling is required for cutaneous wound healing. Stem Cells. 2015;33:2158–68.
Osaki M, Okada F. Exosomes and their role in cancer progression. Yonago Acta Med. 2019;62:182–90.
Deng ZB, Liu Y, Liu C, Xiang X, Wang J, Cheng Z, et al. Immature myeloid cells induced by a high-fat diet contribute to liver inflammation. Hepatology. 2009;50:1412–20.
Samaeekia R, Rabiee B, Putra I, Shen X, Park YJ, Hematti P, et al. Effect of human corneal mesenchymal stromal cell-derived exosomes on corneal epithelial wound healing. Invest Ophthalmol Vis Sci. 2018;59:5194–200.
Han KY, Tran JA, Chang JH, Azar DT, Zieske JD. Potential role of corneal epithelial cell-derived exosomes in corneal wound healing and neovascularization. Sci Rep. 2017;7:40548.
Han KY, Dugas-Ford J, Seiki M, Chang JH, Azar DT. Evidence for the involvement of MMP14 in MMP2 processing and recruitment in exosomes of corneal fibroblasts. Invest Ophthalmol Vis Sci. 2015;56:5323–9.
Weber JA, Baxter DH, Zhang S, Huang DY, Huang KH, Lee MJ, et al. The microRNA spectrum in 12 body fluids. Clin Chem. 2010;56:1733–41.
Danese E, Minicozzi AM, Benati M, Paviati E, Lima-Oliveira G, Gusella M, et al. Reference miRNAs for colorectal cancer: analysis and verification of current data. Sci Rep. 2017;7:8413.
Faraldi M, Gomarasca M, Sansoni V, Perego S, Banfi G, Lombardi G. Normalization strategies differently affect circulating miRNA profile associated with the training status. Sci Rep. 2019;9:1584.
Hermeking H. The miR-34 family in cancer and apoptosis. Cell Death Differ. 2010;17:193–9.
Huang W, Yan Y, Liu Y, Lin M, Ma J, Zhang W, et al. Exosomes with low miR-34c-3p expression promote invasion and migration of non-small cell lung cancer by upregulating integrin alpha2beta1. Signal Transduct Target Ther. 2020;5:39.
Kim YJ, Yeon Y, Lee WJ, Shin YU, Cho H, Sung YK, et al. Comparison of microRNA expression in tears of normal subjects and Sjögren syndrome patients. Invest Ophthalmol Vis Sci. 2019;60:4889–95.
Kapsogeorgou EK, Abu-Helu RF, Moutsopoulos HM, Manoussakis MN. Salivary gland epithelial cell exosomes: a source of autoantigenic ribonucleoproteins. Arthritis Rheum. 2005;52:1517–21.
Mitsias DI, Kapsogeorgou EK, Moutsopoulos HM. The role of epithelial cells in the initiation and perpetuation of autoimmune lesions: lessons from Sjogren’s syndrome (autoimmune epithelitis). Lupus. 2006;15:255–61.
Murad N, Kokkinaki M, Gunawardena N, Gunawan MS, Hathout Y, Janczura KJ, et al. miR-184 regulates ezrin, LAMP-1 expression, affects phagocytosis in human retinal pigment epithelium and is downregulated in age-related macular degeneration. FEBS J. 2014;281:5251–64.
Xu S, Li Y, Chen JP, Li DZ, Jiang Q, Wu T, et al. Oxygen glucose deprivation/re-oxygenation-induced neuronal cell death is associated with Lnc-D63785 m6A methylation and miR-422a accumulation. Cell Death Dis. 2020;11:816.
Acknowledgements
Ryu Uotani reports a relationship with the Japanese Ministry of Education, Science, and Culture that includes funding grants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Torimura, None; S. Kanei, None; Y. Shimizu, None; T. Baba, None; R. Uotani, None; S. Sasaki, None; D. Nagase, None; Y. Inoue, None; T. Ochiya, Patent application filed for the Exoscreen; D. Miyazaki, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Dai Miyazaki
About this article
Cite this article
Torimura, A., Kanei, S., Shimizu, Y. et al. Profiling miRNAs in tear extracellular vesicles: a pilot study with implications for diagnosis of ocular diseases. Jpn J Ophthalmol 68, 70–81 (2024). https://doi.org/10.1007/s10384-023-01028-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-023-01028-0