Abstract
Introduction
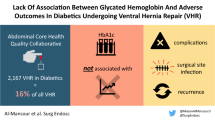
Numerous studies have identified diabetes mellites (DM) as a significant risk factor for postoperative wound morbidity, with suboptimal preoperative glycemic control (GC) posing an even greater risk. However, this data largely excludes ventral hernia patients. Our study examined the association between diabetes and preoperative GC and postoperative outcomes following open complex abdominal wall reconstruction (AWR).
Methods
We identified diabetic patients who had undergone open, elective, clean VHR with transversus abdominis release (TAR) and permanent synthetic mesh at the Cleveland Clinic Foundation between January 2014 and December 2023. Their 30-day outcomes were compared to non-diabetic patients undergoing the same procedure. Subsequently, diabetic patients were categorized based on GC. status: “Optimal GC” (HbA1c < 7%), “Sub-optimal GC” (HbA1c 7-8.4%), and “Poor GC” (HbA1c ≥ 8.5%) and their outcomes were compared.
Results
514 patients with DM who underwent clean elective TAR were identified, of which 431 met the inclusion criteria. GC was deemed optimal in 255 patients, sub-optimal in 128, and poor in 48 patients. Demographics were similar, except for anticoagulation treatment (p = 0.014). The entire study population exhibited significantly higher rates of wound morbidities and overall complications compared to non-diabetic patients. However, rates of surgical site infection (SSI), surgical site occurrence (SSO), SSO requiring procedural intervention (SSOPI), and reoperation did not differ significantly among the three cohorts of presurgical glycemic control (p = 0.82, p = 0.46, p = 0.51, p = 0.78), respectively. No occurrence of mesh removal was documented.
Conclusion
In general, diabetes is a marker for increased wound morbidity and complications following complex abdominal wall reconstruction. However, we could not establish a hard cutoff to justify withholding surgery in symptomatic patients based on an arbitrary HbA1C level. We believe this data is important for shared decision-making when considering AWR for symptomatic ventral hernias in diabetic patients.

Similar content being viewed by others
Data Availability
The data used in this study are available upon reasonable request to the corresponding author (Nir Messer). Requests will be considered on a case-by-case basis and may be subject to specific conditions.
References
National Diabetes Statistics Report (2020) Estimates of diabetes and its burden in the United States. 2020
Jones CE, Graham LA, Morris MS, Richman JS, Hollis RH, Wahl TS et al (2017) Association between Preoperative Hemoglobin A1c Levels, postoperative hyperglycemia, and readmissions following gastrointestinal surgery. JAMA Surg 152(11):1031–1038
Ata A, Lee J, Bestle SL, Desemone J, Stain SC (2010) Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg Chic Ill 1960 145(9):858–864
King JT, Goulet JL, Perkal MF, Rosenthal RA (2011) Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg 253(1):158–165
Noordzij PG, Boersma E, Schreiner F, Kertai MD, Feringa HHH, Dunkelgrun M et al (2007) Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur J Endocrinol 156(1):137–142
Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R et al (2016) Diabetes and risk of Surgical Site infection: a systematic review and Meta-analysis. Infect Control Hosp Epidemiol 37(1):88–99
Goodenough CJ, Liang MK, Nguyen MT, Nguyen DH, Holihan JL, Alawadi ZM et al Preoperative Glycosylated Hemoglobin and Postoperative Glucose Together Predict Major Complications after Abdominal Surgery. J Am Coll Surg [Internet]. 2015 Oct [cited 2024 Feb 28];221(4):854. https://journals.lww.com/journalacs/abstract/2015/10000/preoperative_glycosylated_hemoglobin_and.9.aspx
Moitra VK, Greenberg J, Arunajadai S, Sweitzer B The relationship between glycosylated hemoglobin and perioperative glucose control in patients with diabetes. Can J Anesth Can Anesth [Internet]. 2010 Apr 1 [cited 2024 Feb 28];57(4):322–9. https://doi.org/10.1007/s12630-010-9266-8
Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JRF, Askenasy EP et al (2017) Ventral Hernia Management: Expert Consensus guided by systematic review. Ann Surg 265(1):80–89
Zavlin D, Jubbal KT, Van Eps JL, Bass BL, Ellsworth WA, Echo A et al Safety of open ventral hernia repair in high-risk patients with metabolic syndrome: a multi-institutional analysis of 39,118 cases. Surg Obes Relat Dis [Internet]. 2018 Feb 1 [cited 2024 Feb 28];14(2):206–13. https://www.sciencedirect.com/science/article/pii/S1550728917309474
Messer N, Melland MS, Miller BT, Krpata DM, Beffa LRA, Zheng X et al (2023) Evaluating the impact of lifting mandatory smoking cessation prior to elective abdominal wall reconstruction. A single-center experience. Am J Surg. ;S0002-9610(23)00442-7.
Haskins IN, Horne CM, Krpata DM, Prabhu AS, Tastaldi L, Perez AJ et al A call for standardization of wound events reporting following ventral hernia repair. Hernia [Internet]. 2018 Oct [cited 2023 Apr 24];22(5):729–36. http://link.springer.com/https://doi.org/10.1007/s10029-018-1748-6
Mathias JM (1998) CDC updates guideline on surgical site infection. OR Manager 14(7):9–10
Kesler P (2022) Distressed Communities. Economic Innovation Group. Accessed October 18, https://eig.org/distressed-communities/
Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R (2014) Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care 37(3):611–616
Jehan F, Joseph B (2019) Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of HbA1c? J Trauma Acute Care Surg 86(2):379
Acott AA, Theus SA, Kim LT (2009) Long-term glucose control and risk of perioperative complications. Am J Surg [Internet]. Nov 1 [cited 2024 Mar 2];198(5):596–9. https://www.sciencedirect.com/science/article/pii/S0002961009004425
Rollins KE, Varadhan KK, Dhatariya K, Lobo DN Systematic review of the impact of HbA1c on outcomes following surgery in patients with diabetes mellitus. Clin Nutr [Internet]. 2016 Apr 1 [cited 2024 Mar 2];35(2):308–16. https://www.sciencedirect.com/science/article/pii/S0261561415000825
Polat A, Gumus F (2014) Elevated hemoglobin A1c is associated with readmission but not complications. Asian Cardiovasc Thorac Ann 22(7):885
Al-Mansour MR, Vargas M, Olson MA, Gupta A, Read TE, Algarra NN S-144 lack of association between glycated hemoglobin and adverse outcomes in diabetic patients undergoing ventral hernia repair: an ACHQC study. Surg Endosc [Internet]. 2023 Apr 1 [cited 2023 Oct 9];37(4):3180–90. https://doi.org/10.1007/s00464-022-09479-1
Soare AMS, Preda SD, Râmboiu S, Cârțu D, Pătrașcu Ștefan, Cazacu S et al (2023) Ventral hernia repair and diabetes Mellitus - A prospective, observational and comparative study of outcomes. Curr Health Sci J 49(2):263–272
Xu Z, Qu H, Kanani G, Guo Z, Ren Y, Chen X (2020) Update on risk factors of surgical site infection in colorectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis 35(12):2147–2156
Romero-Velez G, Lima DL, Pereira X, Farber BA, Friedmann P, Malcher F et al (2022) Risk factors for Surgical Site infection in the Undeserved Population after ventral hernia repair: a 3936 patient single-center study using National Surgical Quality Improvement Project. J Laparoendosc Adv Surg Tech A 32(9):948–954
Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P et al (2011) Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care 34(2):256–261
Tan DJH, Yaow CYL, Mok HT, Ng CH, Tai CH, Tham HY et al (2021) The influence of diabetes on postoperative complications following colorectal surgery. Tech Coloproctology 25(3):267–278
Swenne CL, Lindholm C, Borowiec J, Schnell AE, Carlsson M (2005) Peri-operative glucose control and development of surgical wound infections in patients undergoing coronary artery bypass graft. J Hosp Infect 61(3):201–212
Steely AM, Smith L, Callas PW, Nathan MH, Lahiri JE, Stanley AC et al (2017) Prospective Study of Postoperative Glycemic Control with a standardized insulin infusion protocol after Infrainguinal Bypass and Open Abdominal aortic aneurysm repair. Ann Vasc Surg 44:211–220
Gomes MB, Tang F, Chen H, Cid-Ruzafa J, Fenici P, Khunti K et al (2022) Socioeconomic factors Associated with Glycemic Measurement and poor HbA1c control in people with type 2 diabetes: The Global DISCOVER Study. Front Endocrinol 13:831676
Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A (2011) Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol 40(3):804–818
Kyrou I, Tsigos C, Mavrogianni C, Cardon G, Van Stappen V, Latomme J et al (2020) Sociodemographic and lifestyle-related risk factors for identifying vulnerable groups for type 2 diabetes: a narrative review with emphasis on data from Europe. BMC Endocr Disord 20(Suppl 1):134
Olah ME, Gaisano G, Hwang SW (2013) The effect of socioeconomic status on access to primary care: an audit study. Can Med Assoc J [Internet]. Apr 2 [cited 2023 Apr 6];185(6):E263–9. http://www.cmaj.ca/lookup/doi/https://doi.org/10.1503/cmaj.121383
Hausmann LRM, Jeong K, Bost JE, Ibrahim SA Perceived Discrimination in Health Care and Use of Preventive Health Services. J Gen Intern Med [Internet]. 2008 Oct [cited 2023 Apr 6];23(10):1679–84. http://link.springer.com/https://doi.org/10.1007/s11606-008-0730-x
Trivedi AN, Ayanian JZ Perceived discrimination and use of preventive health services. J Gen Intern Med [Internet]. 2006 Jun [cited 2023 Apr 6];21(6):553–8. http://link.springer.com/https://doi.org/10.1111/j.1525-1497.2006.00413.x
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. As this study involved the use of existing data and did not involve direct interaction with human subjects, no patients were enrolled, and therefore, no informed consent was required. The data used in this research were anonymized and de-identified, ensuring the privacy and confidentiality of individuals in accordance with the Institutional Review Board. The research was conducted in accordance with the ethical principles outlined in the Institutional Review Board. The use of data and materials was carried out with proper authorization and in compliance with all applicable laws and regulations.
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study’s conception and design. Material preparation and data collection were performed by NM. The manuscript was written by NM and MJR. All the authors commented on and revised the manuscript. All the authors read and approved the final manuscript. The study was supervised by MJR.
Corresponding author
Ethics declarations
Conflict of interest
I declare that there are no conflicts of interest related to this manuscript. The study was conducted impartially, and the findings presented in the manuscript are based solely on the analysis and interpretation of the data. M.J.R receives salary support for his position in the leadership of the Abdominal Core Health Quality Collaborative (ACHQC), which is the data source for the present submission, and he receives board member support and stock options from Ariste Medical. He also has a research grant paid to his institution by Tela Bio for a clinical trial. A.S.P. has received funding paid to her institution from Intuitive Surgical Inc. and personal fees from Medtronic, Intuitive Surgical, CMR Surgical, and Verb Surgical. L.R.B has received an honorarium from Intuitive.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Messer, N., Miller, B.T., Beffa, L.R. et al. The impact of diabetes and presurgical glycemic control on wound morbidity following open complex abdominal wall reconstruction: a single-center experience. Hernia (2024). https://doi.org/10.1007/s10029-024-03161-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10029-024-03161-2