Abstract
Introduction
Elevated preoperative glycated hemoglobin (HbA1c) is believed to predict complications in diabetic patients undergoing ventral hernia repair (VHR). Our objective was to assess the association between HbA1c and outcomes of VHR in diabetic patients.
Methods
We conducted a retrospective cohort study using the Abdominal Core Health Quality Collaborative (ACHQC) database. We included adult diabetic patients who underwent elective VHR with an available HbA1c result. The patients were divided into two groups (HbA1c < 8% and HbA1c ≥ 8%). Patient demographics, comorbidities, hernia characteristics, operative details, and surgical outcomes were compared. Multivariable logistic regression analysis of complications was performed. Cox proportional hazard regression was used to assess probability of composite recurrence at different HbA1c levels.
Results
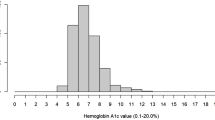
2167 patients met the inclusion criteria (HbA1c < 8% = 1,776 and HbA1c ≥ 8% = 391). Median age was 61 years and median body mass index was 34 kg/m2. 75% had an American Society of Anesthesiology class of 3. The median HbA1c was 6.5% in the HbA1c < 8% group versus 8.7% in the HbA1c ≥ 8% group. 73% were incisional hernias, 34% were recurrent, and median hernia width was 6 cm. Open approach was used in 63% and myofascial release was performed in 46%. Median follow-up was 27 days. There were no clinically significant differences in the rates of overall 30-day complications, wound complications, reoperation, readmission, mortality, length of stay and quality of life and pain scores between the two groups. Regression analyses did not identify an association between HbA1c and the rates of complications, surgical site infection or composite recurrence across the spectrum of HbA1c values.
Conclusion
Our study finds no evidence of an association between HbA1c and operative outcomes in diabetic patients undergoing elective VHR.
Graphical abstract




Similar content being viewed by others
References
Jones CE, Graham LA, Morris MS, Richman JS, Hollis RH, Wahl TS, Copeland LA, Burns EA, Itani KMF, Hawn MT (2017) Association between preoperative hemoglobin A1c levels, postoperative hyperglycemia, and readmissions following gastrointestinal surgery. JAMA Surg 152:1031–1038. https://doi.org/10.1001/jamasurg.2017.2350
Ata A, Lee J, Bestle SL, Desemone J (1960) Stain SC (2010) postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg Chic Ill 145:858–864. https://doi.org/10.1001/archsurg.2010.179
King JT, Goulet JL, Perkal MF, Rosenthal RA (2011) Glycemic control and infections in patients with diabetes undergoing noncardiac surgery. Ann Surg 253:158–165. https://doi.org/10.1097/SLA.0b013e3181f9bb3a
Noordzij PG, Boersma E, Schreiner F, Kertai MD, Feringa HHH, Dunkelgrun M, Bax JJ, Klein J, Poldermans D (2007) Increased preoperative glucose levels are associated with perioperative mortality in patients undergoing noncardiac, nonvascular surgery. Eur J Endocrinol 156:137–142. https://doi.org/10.1530/eje.1.02321
Jackson RS, Amdur RL, White JC, Macsata RA (2012) Hyperglycemia is associated with increased risk of morbidity and mortality after colectomy for cancer. J Am Coll Surg 214:68–80. https://doi.org/10.1016/j.jamcollsurg.2011.09.016
Won EJ, Lehman EB, Geletzke AK, Tangel MR, Matsushima K, Brunke-Reese D, Pichardo-Lowden AR, Pauli EM, Soybel DI (2015) Association of postoperative hyperglycemia with outcomes among patients with complex ventral hernia repair. JAMA Surg 150:433–440. https://doi.org/10.1001/jamasurg.2014.3160
Goodenough CJ, Liang MK, Nguyen MT, Nguyen DH, Holihan JL, Alawadi ZM, Roth JS, Wray CJ, Ko TC, Kao LS (2015) Preoperative glycosylated hemoglobin and postoperative glucose together predict major complications after abdominal surgery. J Am Coll Surg 221:854-861.e1. https://doi.org/10.1016/j.jamcollsurg.2015.07.013
Moitra VK, Greenberg J, Arunajadai S, Sweitzer B (2010) The relationship between glycosylated hemoglobin and perioperative glucose control in patients with diabetes. Can J Anesth Can Anesth 57:322–329. https://doi.org/10.1007/s12630-010-9266-8
Chamberlain JJ, Rhinehart AS, Shaefer CF, Neuman A (2016) Diagnosis and management of diabetes: synopsis of the 2016 american diabetes association standards of medical care in diabetes. Ann Intern Med 164:542. https://doi.org/10.7326/M15-3016
Albers JW, Herman WH, Pop-Busui R, Feldman EL, Martin CL, Cleary PA, Waberski BH, Lachin JM, Effect of prior intensive insulin treatment during the diabetes control and complications trial (DCCT) on peripheral neuropathy in type 1 diabetes during the epidemiology of diabetes interventions and complications (EDIC) study (2010) Effect of prior intensive insulin treatment during the diabetes control and complications trial (DCCT) on peripheral neuropathy in type 1 diabetes during the epidemiology of diabetes interventions and complications (EDIC) study. Diabetes Care 33:1090–1096. https://doi.org/10.2337/dc09-1941
Dronge AS (2006) Long-term glycemic control and postoperative infectious complications. Arch Surg 141:375. https://doi.org/10.1001/archsurg.141.4.375
Engoren M, Schwann TA, Habib RH (2014) Elevated hemoglobin A1c is associated with readmission but not complications. Asian Cardiovasc Thorac Ann 22:800–806. https://doi.org/10.1177/0218492313515895
Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R (2014) Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care 37:611–616. https://doi.org/10.2337/dc13-1929
Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JRF, Askenasy EP, Ballecer C, Chong HS, Goldblatt MI, Greenberg JA, Harvin JA, Keith JN, Martindale RG, Orenstein S, Richmond B, Roth JS, Szotek P, Towfigh S, Tsuda S, Vaziri K, Berger DH (2017) Ventral hernia management: expert consensus guided by systematic review. Ann Surg 265:80–89. https://doi.org/10.1097/SLA.0000000000001701
Mehaffey JH, Hawkins RB, Charles EJ, Turrentine FE, Hallowell PT, Friel C, Jones RS, Tracci MC (2020) Socioeconomic “distressed communities index” improves surgical risk-adjustment. Ann Surg 271:470–474. https://doi.org/10.1097/SLA.0000000000002997
Baucom RB, Ousley J, Feurer ID, Beveridge GB, Pierce RA, Holzman MD, Sharp KW, Poulose BK (2016) Patient reported outcomes after incisional hernia repair-establishing the ventral hernia recurrence inventory. Am J Surg 212:81–88. https://doi.org/10.1016/j.amjsurg.2015.06.007
Krpata DM, Schmotzer BJ, Flocke S, Jin J, Blatnik JA, Ermlich B, Novitsky YW, Rosen MJ (2012) Design and initial implementation of HerQLes: a hernia-related quality-of-life survey to assess abdominal wall function. J Am Coll Surg 215:635–642. https://doi.org/10.1016/j.jamcollsurg.2012.06.412
Renshaw SM, Gupta A, Poulose BK (2021) Establishing the minimal clinically important difference for the hernia-related quality of life survey (HerQLes). Am J Surg S0002–9610(21):00349–00354. https://doi.org/10.1016/j.amjsurg.2021.06.018
Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, DeVellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai J-S, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R (2010) The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 63:1179–1194. https://doi.org/10.1016/j.jclinepi.2010.04.011
Hwang JS, Kim SJ, Bamne AB, Na YG, Kim TK (2015) Do glycemic markers predict occurrence of complications after total knee arthroplasty in patients with diabetes? Clin Orthop 473:1726–1731. https://doi.org/10.1007/s11999-014-4056-1
Jehan F, Khan M, Sakran JV, Khreiss M, O’Keeffe T, Chi A, Kulvatunyou N, Jain A, Zakaria ER, Joseph B (2018) Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: What is the role of plasma hemoglobin A1c? J Trauma Acute Care Surg 84:112–117. https://doi.org/10.1097/TA.0000000000001724
Kotagal M, Symons RG, Hirsch IB, Umpierrez GE, Dellinger EP, Farrokhi ET, Flum DR (2015) Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg 261:97–103. https://doi.org/10.1097/SLA.0000000000000688
Karimian N, Niculiseanu P, Amar-Zifkin A, Carli F, Feldman LS (2018) Association of elevated pre-operative hemoglobin A1c and post-operative complications in non-diabetic patients: a systematic review. World J Surg 42:61–72. https://doi.org/10.1007/s00268-017-4106-4
Rollins KE, Varadhan KK, Dhatariya K, Lobo DN (2016) Systematic review of the impact of HbA1c on outcomes following surgery in patients with diabetes mellitus. Clin Nutr Edinb Scotl 35:308–316. https://doi.org/10.1016/j.clnu.2015.03.007
Ban KA, Minei JP, Laronga C, Harbrecht BG, Jensen EH, Fry DE, Itani KMF, Dellinger EP, Ko CY, Duane TM (2017) American college of surgeons and surgical infection society: surgical site infection guidelines, 2016 update. J Am Coll Surg 224:59–74. https://doi.org/10.1016/j.jamcollsurg.2016.10.029
Berríos-Torres SI, Umscheid CA, Bratzler DW, Leas B, Stone EC, Kelz RR, Reinke CE, Morgan S, Solomkin JS, Mazuski JE, Dellinger EP, Itani KMF, Berbari EF, Segreti J, Parvizi J, Blanchard J, Allen G, Kluytmans JAJW, Donlan R, Schecter WP, Committee HICPA (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152:784–791. https://doi.org/10.1001/jamasurg.2017.0904
Shohat N, Goswami K, Breckenridge L, Held MB, Malkani AL, Shah RP, Schwarzkopf R, Parvizi J (2021) Fructosamine is a valuable marker for glycemic control and predicting adverse outcomes following total hip arthroplasty: a prospective multi-institutional investigation. Sci Rep 11:2227. https://doi.org/10.1038/s41598-021-81803-6
Acknowledgements
The authors would like to thank Dan Neal of the University of Florida for his help in providing statistical review for the study protocol and Thomas Stewart of Vanderbilt University School of Medicine for his help in reviewing the statistical analysis.
Funding
Melanie Vargas received an award for this project as Medical Summer Research Scholarship from the University of Florida College of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Mazen R. Al-Mansour received speaker fees from Medtronic Inc., educational support from Intuitive Surgical and general payments from W. L. Gore & Associates, Inc. and ConMed Corporation. The ACHQC has contracted with Weill Cornell Medicine to provide biostatistical support for ACHQC projects. The work provided for this manuscript was performed under the umbrella of the Weill Cornell Medicine and ACHQC collaboration plan. Mazen R. Al‑Mansour, Melanie Vargas, Molly A. Olson, Anand Gupta, Thomas E. Read and Nelson N. Algarra have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Al-Mansour, M.R., Vargas, M., Olson, M.A. et al. S-144 lack of association between glycated hemoglobin and adverse outcomes in diabetic patients undergoing ventral hernia repair: an ACHQC study. Surg Endosc 37, 3180–3190 (2023). https://doi.org/10.1007/s00464-022-09479-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09479-1