Abstract
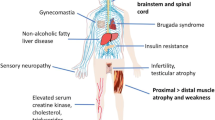
Spinal and bulbar muscular atrophy (SBMA), also known as Kennedy’s disease, is a rare, X-linked hereditary lower motor neuron disease, characterized by progressive muscular weakness. An expanded trinucleotide repeat (CAG > 37) in the androgen receptor gene (AR), encoding glutamine, is the mutation responsible for Kennedy’s disease. Toxicity of this mutant protein affects both motor neurons and muscles. In this review, we provide a comprehensive, clinically oriented overview of the current literature regarding Kennedy’s disease, highlighting gaps in our knowledge that remain to be addressed in further research. Kennedy’s disease mimics are also discussed, as are ongoing and recently completed therapeutic endeavours.


Similar content being viewed by others
References
La Spada AR, Wilson EM, Lubahn DB et al (1991) Androgen receptor gene mutations in X-linked spinal and bulbar muscular atrophy. Nature 352:77–79. https://doi.org/10.1038/352077a0
Pennuto M, Rinaldi C (2017) From gene to therapy in spinal and bulbar muscular atrophy: are we there yet? Mol Cell Endocrinol. https://doi.org/10.1016/j.mce.2017.07.005
Kennedy WR, Alter M, Sung JH (1968) Progressive proximal spinal and bulbar muscular atrophy of late onset. Neurology 18
Harding AE, Thomas PK, Baraitser M et al (1982) X-linked recessive bulbospinal neuronopathy: a report of ten cases. J Neurol Neurosurg Psychiatry 45:1012–1019. https://doi.org/10.1136/jnnp.45.11.1012
Koutsis G, Kladi A, Breza M et al (2015) Spinobulbar muscular atrophy (Kennedy’s disease): a rare diagnosis in the Greek population. J Neurol Sci 359:450–451. https://doi.org/10.1016/j.jns.2015.10.021
Fratta P, Nirmalananthan N, Masset L et al (2014) Correlation of clinical and molecular features in spinal bulbar muscular atrophy. Neurology 82:2077–2084. https://doi.org/10.1212/WNL.0000000000000507
Mariotti C, Castellotti B, Pareyson D et al (2000) Phenotypic manifestations associated with CAG-repeat expansion in the androgen receptor gene in male patients and heterozygous females: a clinical and molecular study of 30 families. Neuromuscul Disord 10:391–397. https://doi.org/10.1016/S0960-8966(99)00132-7
Fischbeck KH (1997) Kennedy disease. J Inherit Metab Dis 20:152–158. https://doi.org/10.1023/A:1005344403603
Guidetti D, Sabadini R, Ferlini A, Torrente I (2001) Epidemiological survey of X-linked bulbar and spinal muscular atrophy, or Kennedy disease, in the province of Reggio Emilia, Italy. Eur J Epidemiol 17:587–591. https://doi.org/10.1023/A:1014580219761
Udd B, Juvonen V, Hakamies L et al (1998) High prevalence of Kennedy’s disease in Western Finland—is the syndrome underdiagnosed? Acta Neurol Scand 98:128–133
Tanaka F, Doyu M, Ito Y et al (1996) Founder effect in spinal and bulbar muscular atrophy (SBMA). Hum Mol Genet 5:1253–1257. https://doi.org/10.1093/hmg/5.9.1253
Li M, Miwa S, Kobayashi Y et al (1998) Nuclear inclusions of the androgen receptor protein in spinal and bulbar muscular atrophy. Ann Neurol 44:249–254. https://doi.org/10.1002/ana.410440216
Grunseich C, Fischbeck KH (2015) Spinal and bulbar muscular atrophy. Neurol Clin 33:847–854. https://doi.org/10.1016/j.ncl.2015.07.002
Amato A, Prior TW, Barohn RJ et al (1993) Kennedy’s disease: a clinicopathologic correlation with mutations in the androgen receptor gene. Neurology 43:791–794
Cortes CJ, Ling SC, Guo LT et al (2014) Muscle expression of mutant androgen receptor accounts for systemic and motor neuron disease phenotypes in spinal and bulbar muscular atrophy. Neuron 82:295–307. https://doi.org/10.1016/j.neuron.2014.03.001
Adachi H, Katsuno M, Minamiyama M et al (2005) Widespread nuclear and cytoplasmic accumulation of mutant androgen receptor in SBMA patients. Brain 128:659–670. https://doi.org/10.1093/brain/awh381
Rinaldi C, Bott LC, Fischbeck KH (2014) Muscle matters in Kennedy’s disease. Neuron 82:251–253. https://doi.org/10.1016/j.neuron.2014.04.005
Rocchi A, Milioto C, Parodi S et al (2016) Glycolytic to oxidative fiber type switch and mTOR signaling activation are early-onset features of SBMA muscle modified by high fat diet. Acta Neuropathol 132:127–144. https://doi.org/10.1007/s00401-016-1550-4
Ishihara H, Kanda F, Nishio H et al (2001) Clinical features and skewed X-chromosome inactivation in female carriers of X-linked recessive spinal and bulbar muscular atrophy. J Neurol 248:856–860. https://doi.org/10.1007/s004150170069
La Spada A (1996) Spinal and bulbar muscular atrophy. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K, Amemiya A (eds) GeneReviews®. University of Washington, Seattle. http://www.ncbi.nlm.nih.gov/books/NBK1333/. Accessed 10 mar 2018
Biancalana V, Serville F, Pommier J et al (1992) Moderate instability of the trinucleotide repeat in spinobulbar muscular atrophy. Hum Mol Genet 1:255–258
Atsuta N, Watanabe H, Ito M et al (2006) Natural history of spinal and bulbar muscular atrophy (SBMA): a study of 223 Japanese patients. Brain 129:1446–1455. https://doi.org/10.1093/brain/awl096
Grunseich C, Kats IR, Bott LC et al (2014) Early onset and novel features in a spinal and bulbar muscular atrophy patient with a 68 CAG repeat. Neuromuscul Disord 24:978–981. https://doi.org/10.1016/j.nmd.2014.06.441
Kooy RF, Reyniers E, Storm K et al (1999) CAG Repeat contraction in the androgen receptor gene in three brothers with mental retardation. Am J Med Genet 213:209–213
Kuhlenbäumer G, Kress W, Ringelstein EB, Stögbauer F (2001) Thirty-seven CAG repeats in the androgen receptor gene in two healthy individuals. J Neurol 248:23–26. https://doi.org/10.1007/s004150170265
Koutsis G, Karadima G, Kladi A, Panas M (2014) Late-onset Huntington’s disease: diagnostic and prognostic considerations. Parkinsonism Relat Disord 20:726–730. https://doi.org/10.1016/j.parkreldis.2014.03.017
Chahin N, Sorenson EJ (2009) Serum creatine kinase levels in spinobulbar muscular atrophy and amyotrophic lateral sclerosis. Muscle Nerve 40:126–129. https://doi.org/10.1002/mus.21310
Rhodes LE, Freeman BK, Auh S et al (2009) Clinical features of spinal and bulbar muscular atrophy. Brain 132:3242–3251. https://doi.org/10.1093/brain/awp258
Querin G, Bertolin C, Da Re E et al (2015) Non-neural phenotype of spinal and bulbar muscular atrophy: results from a large cohort of Italian patients. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2015-311305
Manzano R, Sorarú G, Grunseich C et al (2018) Beyond motor neurons: expanding the clinical spectrum in Kennedy’ s disease. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2017-316961
Hijikata Y, Hashizume A, Yamada S et al (2018) Biomarker-based analysis of preclinical progression in spinal and bulbar muscular atrophy. Neurology. https://doi.org/10.1212/WNL.0000000000005360.
Rhodes LE, Freeman BK, Auh S et al (2009) Clinical features of spinal and bulbar muscular atrophy. Brain 25:285–287. https://doi.org/10.1093/brain/awp258
Parboosingh JS, Figlewicz D, Krizus A et al (1997) Spinobulbar muscular atrophy can mimic ALS: the importance of genetic testing in male patients with atypical ALS. Neurology 49:568–572. https://doi.org/10.1212/WNL.49.2.568
Ferrante M, Wilbourn AJ (1997) The characteristic electrodiagnostic features of Kennedy’s disease. Muscle Nerve 20:323–329
Garg N, Park SB, Vucic S et al (2016) Differentiating lower motor neuron syndromes. J Neurol Neurosurg Psychiatry. https://doi.org/10.1136/jnnp-2016-313526
Fischbeck KH (2016) Spinal and Bulbar Muscular Atrophy. J Mol Neurosci 58:317. https://doi.org/10.1007/s12031-015-0674-7
Sumner CJ, Fischbeck KH (2002) Jaw drop in Kennedy’s disease. Neurology 59:1471–1472. https://doi.org/10.1212/01.WNL.0000033325.01878.13
Praline J, Guennoc AM, Malinge MC et al (2008) Pure bulbar motor neuron involvement linked to an abnormal CAG repeat expansion in the androgen receptor gene. Amyotroph Lateral Scler 9:40–42. https://doi.org/10.1080/17482960701553915
Araki K, Nakanishi H, Nakamura T et al (2015) Myotonia-like symptoms in a patient with spinal and bulbar muscular atrophy. Neuromuscul Disord 25:913–915. https://doi.org/10.1016/j.nmd.2015.08.006
Finsterer J, Soraru G (2015) Onset manifestations of spinal and bulbar muscular atrophy (Kennedy’s disease). J Mol Neurosci. https://doi.org/10.1007/s12031-015-0663-x
Finsterer J (2009) Bulbar and spinal muscular atrophy (Kennedy’s disease): a review. Eur J Neurol 16:556–561. https://doi.org/10.1111/j.1468-1331.2009.02591.x
Nishiyama A, Sugeno N, Tateyama M et al (2014) Postural leg tremor in X-linked spinal and bulbar muscular atrophy. J Clin Neurosci 21:799–802. https://doi.org/10.1016/j.jocn.2013.07.026
Warnecke T, Oelenberg S, Teismann I et al (2009) Dysphagia in X-linked bulbospinal muscular atrophy (Kennedy disease). Neuromuscul Disord 19:704–708. https://doi.org/10.1016/j.nmd.2009.06.371
Hashizume A, Banno H, Katsuno M et al (2017) Quantitative assessment of swallowing dysfunction in patients with spinal and bulbar muscular atrophy. Intern Med 56:3159–3165. https://doi.org/10.2169/internalmedicine.8799-16
Sperfeld AD, Hanemann CO, Ludolph AC, Kassubek J (2005) Laryngospasm: an underdiagnosed symptom of X-linked spinobulbar muscular atrophy. Neurology 64:753–754. https://doi.org/10.1212/01.WNL.0000151978.74467.E7
Finsterer J (2010) Perspectives of Kennedy’s disease. J Neurol Sci 298:1–10. https://doi.org/10.1016/j.jns.2010.08.025
Pedroso JL, Vale TC, Barsottini OG et al (2018) Perioral and tongue fasciculations in Kennedy’s disease. Neurol Sci 39:777–779. https://doi.org/10.1007/s10072-017-3170-8
Jokela ME, Udd B (2015) Diagnostic clinical, electrodiagnostic and muscle pathology features of spinal and bulbar muscular atrophy. J Mol Neurosci. https://doi.org/10.1007/s12031-015-0684-5
Rocchi C, Greco V, Urbani A, Giorgio A (2011) Subclinical autonomic dysfunction in spinobulbar muscular atrophy. Muscle Nerve 44:737–740. https://doi.org/10.1002/mus.22159
Romigi A, Liguori C, Placidi F et al (2014) Sleep disorders in spinal and bulbar muscular atrophy (Kennedy’s disease): a controlled polysomnographic and self-reported questionnaires study. J Neurol 261:889–893. https://doi.org/10.1007/s00415-014-7293-z
Araki A, Katsuno M, Suzuki K et al (2014) Brugada syndrome in spinal and bulbar muscular atrophy. Neurology 82:1813–1821. https://doi.org/10.1212/WNL.0000000000000434
Rosenbohm A, Hirsch S, Volk AE et al (2018) The metabolic and endocrine characteristics in spinal and bulbar muscular atrophy. J Neurol 265:1–11. https://doi.org/10.1007/s00415-018-8790-2
Guber RD, Takyar V, Kokkinis A et al (2017) Nonalcoholic fatty liver disease in spinal and bulbar muscular atrophy. Neurology 89:2481–2490. https://doi.org/10.1212/WNL.0000000000004748
Kassubek J, Juengling FD, Sperfeld A (2007) Widespread white matter changes in Kennedy disease: a voxel based morphometry study. J Neurol Neurosurg Psychiatry 78:1209–1213. https://doi.org/10.1136/jnnp.2006.112532
Soukup GR, Sperfeld AD, Uttner I et al (2009) Frontotemporal cognitive function in X-linked spinal and bulbar muscular atrophy (SBMA): a controlled neuropsychological study of 20 patients. J Neurol 256:1869–1875. https://doi.org/10.1007/s00415-009-5212-5
Di Rosa E, Sorarù G, Kleinbub JR et al (2014) Theory of mind, empathy and neuropsychological functioning in X-linked Spinal and Bulbar Muscular Atrophy: a controlled study of 20 patients. J Neurol 262:394–401. https://doi.org/10.1007/s00415-014-7567-5
Lai TH, Liu RS, Yang BH et al (2013) Cerebral involvement in spinal and bulbar muscular atrophy (Kennedy’s disease): a pilot study of PET. J Neurol Sci 335:139–144. https://doi.org/10.1016/j.jns.2013.09.016
Sperfeld AD, Karitzky J, Brummer D et al (2002) X-linked bulbospinal neuronopathy. Arch Neurol 59:1921. https://doi.org/10.1001/archneur.59.12.1921
Igarashi S, Tanno Y, Onodera O et al (1992) Strong correlation between the number of CAG repeats in androgen receptor genes and the clinical onset of features of spinal and bulbar muscular atrophy. Neurology 42:2300–2302
Nakatsuji H, Araki A, Hashizume A et al (2017) Correlation of insulin resistance and motor function in spinal and bulbar muscular atrophy. J Neurol 264:839–847. https://doi.org/10.1007/s00415-017-8405-3
Sobue G, Doyu M, Kachi T et al (1993) Subclinical phenotypic expressions in heterozygous females of X-linked recessive bulbospinal neuronopathy. J Neurol Sci 117:74–78. https://doi.org/10.1016/0022-510X(93)90157-T
Manganelli F, Iodice V, Provitera V et al (2007) Small-fiber involvement in spinobulbar muscular atrophy (Kennedy’s disease). Muscle Nerve 36:816–820. https://doi.org/10.1002/mus.20872
Antonini G, Gragnani F, Romaniello A et al (2000) Sensory involvement in spinal-bulbar muscular atrophy (Kennedy’s disease). Muscle Nerve 23:252–258
Banno H (2012) Molecular pathophysiology and disease-modifying therapies for spinal and bulbar muscular atrophy. Arch Neurol 69:436. https://doi.org/10.1001/archneurol.2011.2308
Meriggioli MN, Rowin J, Sanders DB (1999) Distinguishing clinical and electrodiagnostic features of X-linked bulbospinal neuronopathy. Muscle Nerve 22:1693–1697
Fernández-Rhodes LE, Kokkinis AD, White MJ et al (2011) Efficacy and safety of dutasteride in patients with spinal and bulbar muscular atrophy: a randomised placebo-controlled trial. Lancet Neurol 10:140–147. https://doi.org/10.1016/S1474-4422(10)70321-5
Dahlqvist JR, Vissing J (2016) Exercise therapy in spinobulbar muscular atrophy and other neuromuscular disorders. J Mol Neurosci 58:388–393. https://doi.org/10.1007/s12031-015-0686-3
Katsuno M, Adachi H, Doyu M et al (2003) Leuprorelin rescues polyglutamine-dependent phenotypes in a transgenic mouse model of spinal and bulbar muscular atrophy. Nat Med 9:768–773. https://doi.org/10.1038/nm878
Banno H, Katsuno M, Suzuki K et al (2009) Phase 2 trial of leuprorelin in patients with spinal and bulbar muscular atrophy. Ann Neurol 65:140–150. https://doi.org/10.1002/ana.21540
Hashizume A, Katsuno M, Suzuki K et al (2017) Long-term treatment with leuprorelin for spinal and bulbar muscular atrophy: Natural history-controlled study. J Neurol Neurosurg Psychiatry 88:1026–1032. https://doi.org/10.1136/jnnp-2017-316015
Querin G, D’Ascenzo C, Peterle E et al (2013) Pilot trial of clenbuterol in spinal and bulbar muscular atrophy. Neurology 80:2095–2098. https://doi.org/10.1212/WNL.0b013e318295d766
Pourshafie N, Lee PR, Chen K et al (2016) MiR-298 counteracts mutant androgen receptor toxicity in spinal and bulbar muscular atrophy. Mol Ther. https://doi.org/10.1038/mt.2016.13
Weydt P, Sagnelli A, Rosenbohm A et al (2015) Clinical trials in spinal and bulbar muscular atrophy—past, present, and future. J Mol Neurosci. https://doi.org/10.1007/s12031-015-0682-7
Pareyson D, Fratta P, Pradat P et al (2016) Towards a european registry and biorepository for patients with spinal and bulbar muscular atrophy. J Mol Neurosci. https://doi.org/10.1007/s12031-015-0704-5
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Institutional Review Board approval was not required for this paper, because it is a review of previously published articles.
Conflicts of interest
None of the authors have any financial disclosure to make or have any conflict of interest relevant to the manuscript. G. Koutsis has received research grants from Genesis Pharma and Teva, consultation fees, advisory boards and honoraria from Genzyme, Genesis Pharma, Teva, and Novartis.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video legend: Fasciculations of tongue in a 61-year-old SBMA patient with wasting of the tongue, scalloping of the borders, and midline furrowing. (MOV 15253 KB)
Rights and permissions
About this article
Cite this article
Breza, M., Koutsis, G. Kennedy’s disease (spinal and bulbar muscular atrophy): a clinically oriented review of a rare disease. J Neurol 266, 565–573 (2019). https://doi.org/10.1007/s00415-018-8968-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8968-7