Abstract
Purpose
The purpose of this prospective study was to determine the diagnostic impact and influence on patient treatment of posttherapeutic 131I SPECT-CT when the findings on planar posttherapeutic whole-body scintigraphy (ptWBS) were inconclusive.
Materials and methods
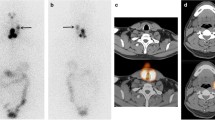
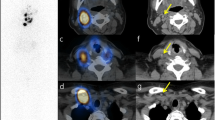
A total of 53 SPECT-CT scans were performed in 41 patients with thyroid cancer after high-dose 131I therapy (2.944 to 7.526 GBq 131I) because of diagnostic uncertainty on ptWBS. Physiological uptake in the salivary glands, gastric mucosa, gut, nasal mucosa, urinary tract and liver were considered to be normal. Any other foci of increased 131I uptake, except iodine uptake clearly located in the thyroid bed, were considered to be abnormal. The data were evaluated on a lesion and a patient basis.
Results
Regarding neck lesions, SPECT-CT provided a diagnostic impact in 26/90 lesions (28.9%) and confirmed the diagnosis in 64/90 lesions (71.1%). On a patient basis, SPECT-CT changed N status in 12/33 patients (36.4%), provided a diagnostic impact in 21/33 patients (63.6%) and led to a treatment change in 8/33 patients (24.2%). Regarding lesions distant from the neck, SPECT-CT confirmed the diagnosis in 62/71 lesions (87.3%) and had a diagnostic impact in 9/71 lesions (12.7%). On a patient basis, SPECT-CT changed M status in 4/19 patients (21.1%), had a diagnostic impact in 14/19 patients (73.7%) and led to a treatment change in 2/19 patients (10.5%). Considering all patients, SPECT-CT led to a treatment change in 10/41 patients (24.4%).
Conclusion
Integrated SPECT-CT is a useful tool, especially in cases of diagnostic uncertainty and helps to individualize patient management.




Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.References
Pacini F, Schlumberger M, Dralle H, Elisei R, Smit JWA, Wiersinga W; European Thyroid Cancer Taskforce. European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol 2006;154:787–803.
Fatourechi V, Hay ID, Mullan BP, Wiseman GA, Eghbali-Fatourechi GZ, Thorson LM, et al. Are posttherapy radioiodine scans informative and do they influence subsequent therapy of patients with differentiated thyroid cancer? Thyroid 2000;10:573–7.
Schlumberger M, Berg G, Cohen O, Duntas L, Jamar F, Jarzab B, et al. Follow-up of low risk patients with differentiated thyroid carcinoma: a European perspective. Eur J Endocrinol 2004;150:105–12.
Schlumberger M, Pacini F, Wiersinga WM, Toft A, Smit JW, Franco FS, et al. Follow-up and management of differentiated thyroid carcinoma: a European perspective in clinical practice. Eur J Endocrinol 2004;151:539–48.
Spies WG, Wojtowicz CH, Spies SM, Shah AY, Zimmer AM. Value of post-therapy whole-body imaging in the evaluation of patients with thyroid carcinoma having undergone high-dose I-131 therapy. Clin Nucl Med 1989;14:793–800.
Cavalieri RR. Nuclear imaging in the management of thyroid carcinoma. Thyroid 1996;6:485–92.
Sherman SI, Tielens ET, Sostre S, Wharam MD Jr, Ladenson PW. Clinical utility of posttreatment radioiodine scans in the management of patients with thyroid carcinoma. J Clin Endocrinol Metab 1994;78:629–34.
Pacini F, Schlumberger M, Harmer C, Berg GG, Cohen O, Duntas L, et al. Post-surgical use of radioiodine (131 I) in patients with papillary and follicular thyroid cancer and the issue of remnant ablation: a consensus report. Eur J Endocrinol 2005;153:651–9.
Lind P, Kohlfürst S. Respective roles of thyroglobulin, radioiodine imaging, and positron emission tomography in the assessment of thyroid cancer. Semin Nucl Med 2006;36:194–205.
Shapiro B, Rufini V, Jarwan A. Artifacts, anatomical and physiological variants, and unrelated diseases that might cause false-positive whole-body 131 I scans in patients with thyroid cancer. Semin Nucl Med 2000;30:115–32.
Bakheet SM, Hammami MM. False positive radioiodine whole-body scan in thyroid cancer patients due to unrelated pathology. Clin Nucl Med 1994;19:325–9.
Andreas J, Bruhl K, Eissner D. False-positive I-131 whole-body imaging after I-131 therapy for a follicular carcinoma. Clin Nucl Med 1997;22:123–4.
Sherman SI, Tielens ET, Sostre S, Wharam MD Jr, Ladenson PW. Clinical utility of posttreatment radioiodine scans in the management of patients with thyroid carcinoma. J Clin Endocrinol Metab 1994;78:629–34.
Leitha T, Staudenherz A. Frequency of diagnostic dilemmas in 131 I whole body scanning. Nuklearmedizin 2003;42:55–62.
Yamamoto Y, Nishiyama Y, Monden T, Matsumura Y, Satoh K, Ohkawa M. Clinical usefulness of fusion of 131I SPECT and CT images in patients with differentiated thyroid carcinoma. J Nucl Med 2003;44:1905–10.
Krausz Y, Klein M, Uziely B, et al. Impact of SPECT/CT on assessment of 131 I-avid sites in differentiated thyroid cancer (abstract). J Nucl Med 2004;45:349.
Ruf J, Lehmkuhl L, Bertram H, Sandrock D, Amthauer H, Humplik B, et al. Impact of SPECT and integrated low-dose CT after radioiodine therapy on the management of patients with thyroid carcinoma. Nucl Med Commun 2004;25:1177–82.
Tharp K, Israel O, Hausmann J, Bettman L, Martin WH, Daitzchman M, et al. Impact of 131I-SPECT/CT images obtained with an integrated system in the follow-up of patients with thyroid carcinoma. Eur J Nucl Med Mol Imaging 2004;31:1435–42.
Krausz Y, Israel O. Single-photon emission computed tomography/computed tomography in endocrinology. Semin Nucl Med 2006;36:267–74.
Cherng SC, Wang YF, Fan YM, Chen CY, Yuan YN, Cheng CY. Malignant struma ovarii with peritoneal implants and pelvic structures and liver metastases demonstrated by I-131 SPECT and low-dose CT. Clin Nucl Med 2005;30:797–8.
von Falck C, Beer G, Gratz KF, Galanski M. Renal metastases from follicular thyroid cancer on SPECT/CT. Clin Nucl Med 2007;32:751–2.
Sakahara H, Yamashita S, Suzuki K, Imai M, Kosugi T. Visualization of nasolacrimal drainage system after radioiodine therapy in patients with thyroid cancer. Ann Nucl Med 2007;21:525–7.
Aide N, Lehembre E, Gervais R, Bardet S. Unusual intratracheal metastasis of differentiated thyroid cancer accurately depicted by SPECT/CT acquisition after radioiodine ablation. Thyroid 2007;17:1305–6.
Mazzaferri EL, Jiang SM. Long term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med 1994;49:418–28.
Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at an institution during 1940 through 1989. Surgery 1993;114:1050–7.
Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1990): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg 2002;8:879–85.
Byar DP, Green SB, Dor P, Williams ED, Colon J, van Gilse HA, et al. A prognostic index for thyroid carcinoma. A study of the E.O.R.T.C. Thyroid Cancer Cooperative Group. Eur J Cancer 1979;15:1033–41.
Tenvall J, Biorklund A, Moller T, Ranstam J, Akerman M. Is the EORTC prognostic index of thyroid cancer valid in differentiated thyroid carcinoma? Retrospective multivariate analysis of differentiated thyroid carcinoma with long follow-up. Cancer 1986;57:1405–14.
Shaha AR, Loree TR, Shah JP. Prognostic factors and risk group analysis in follicular carcinoma of the thyroid. Surgery 1995;118:1131–6.
Sherman SI, Brierly JD, Sperling M, Ain KB, Bigos ST, Cooper DS, et al. Prospective multicenter study of thyroid cancer treatment: initial analysis of staging and outcome. National Thyroid Cancer Treatment Study Registry Group. Cancer 1998;83:1012–21.
Links TP, van Tol KM, Jager PL, Plukker JT, Piers DA, Boezen HM, et al. Life expectancy in differentiated thyroid cancer: a novel approach to survival analysis. Endocr Relat Cancer 2005;12:273–80.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kohlfuerst, S., Igerc, I., Lobnig, M. et al. Posttherapeutic 131I SPECT-CT offers high diagnostic accuracy when the findings on conventional planar imaging are inconclusive and allows a tailored patient treatment regimen. Eur J Nucl Med Mol Imaging 36, 886–893 (2009). https://doi.org/10.1007/s00259-008-1044-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-008-1044-2