Abstract
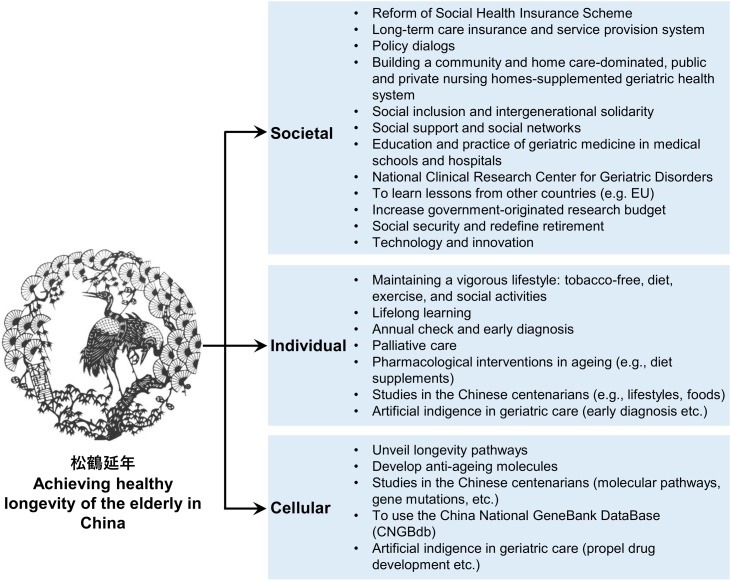
One of the key issues facing public healthcare is the global trend of an increasingly ageing society which continues to present policy makers and caregivers with formidable healthcare and socio-economic challenges. Ageing is the primary contributor to a broad spectrum of chronic disorders all associated with a lower quality of life in the elderly. In 2019, the Chinese population constituted 18 % of the world population, with 164.5 million Chinese citizens aged 65 and above (65+), and 26 million aged 80 or above (80+). China has become an ageing society, and as it continues to age it will continue to exacerbate the burden borne by current family and public healthcare systems. Major healthcare challenges involved with caring for the elderly in China include the management of chronic non-communicable diseases (CNCDs), physical frailty, neurodegenerative diseases, cardiovascular diseases, with emerging challenges such as providing sufficient dental care, combating the rising prevalence of sexually transmitted diseases among nursing home communities, providing support for increased incidences of immune diseases, and the growing necessity to provide palliative care for the elderly. At the governmental level, it is necessary to make long-term strategic plans to respond to the pressures of an ageing society, especially to establish a nationwide, affordable, annual health check system to facilitate early diagnosis and provide access to affordable treatments. China has begun work on several activities to address these issues including the recent completion of the of the Ten-year Health-Care Reform project, the implementation of the Healthy China 2030 Action Plan, and the opening of the National Clinical Research Center for Geriatric Disorders. There are also societal challenges, namely the shift from an extended family system in which the younger provide home care for their elderly family members, to the current trend in which young people are increasingly migrating towards major cities for work, increasing reliance on nursing homes to compensate, especially following the outcomes of the ‘one child policy’ and the ‘empty-nest elderly’ phenomenon. At the individual level, it is important to provide avenues for people to seek and improve their own knowledge of health and disease, to encourage them to seek medical check-ups to prevent/manage illness, and to find ways to promote modifiable health-related behaviors (social activity, exercise, healthy diets, reasonable diet supplements) to enable healthier, happier, longer, and more productive lives in the elderly. Finally, at the technological or treatment level, there is a focus on modern technologies to counteract the negative effects of ageing. Researchers are striving to produce drugs that can mimic the effects of ‘exercising more, eating less’, while other anti-ageing molecules from molecular gerontologists could help to improve ‘healthspan’ in the elderly. Machine learning, ‘Big Data’, and other novel technologies can also be used to monitor disease patterns at the population level and may be used to inform policy design in the future. Collectively, synergies across disciplines on policies, geriatric care, drug development, personal awareness, the use of big data, machine learning and personalized medicine will transform China into a country that enables the most for its elderly, maximizing and celebrating their longevity in the coming decades. This is the 2nd edition of the review paper (Fang EF et al., Ageing Re. Rev. 2015).
Keywords: Ageing policy, Sexually transmitted diseases, Inflammageing, Dementia, Oral ageing, Square dancing
1. Introduction
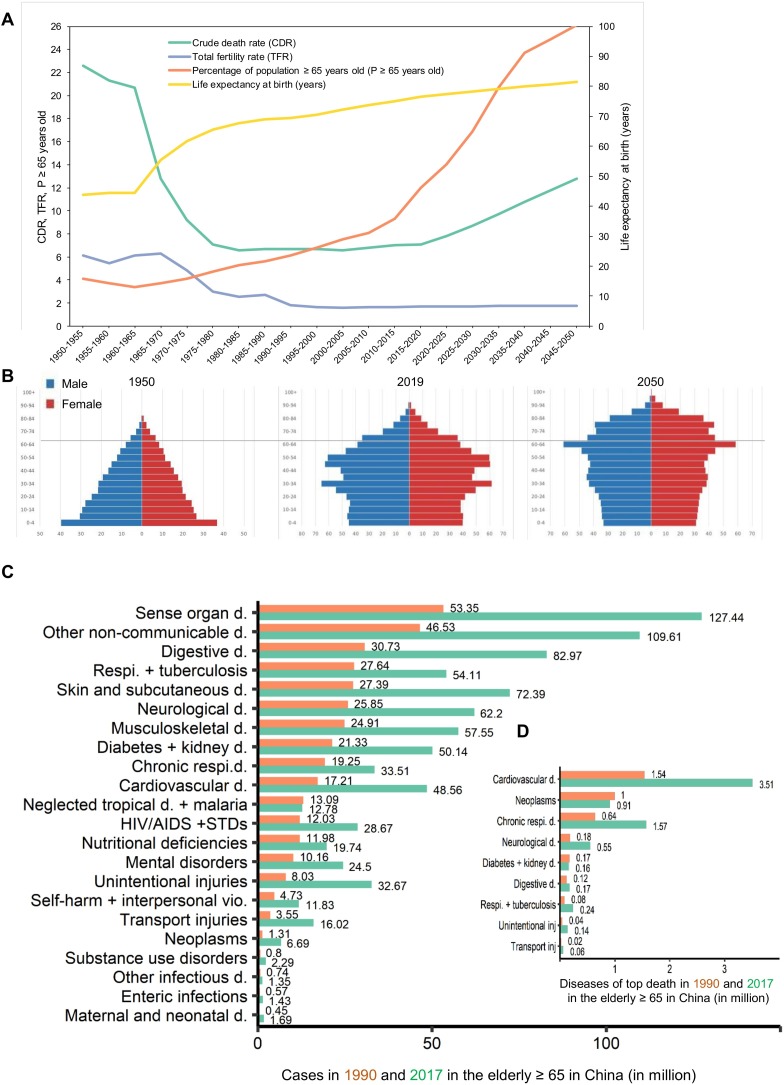
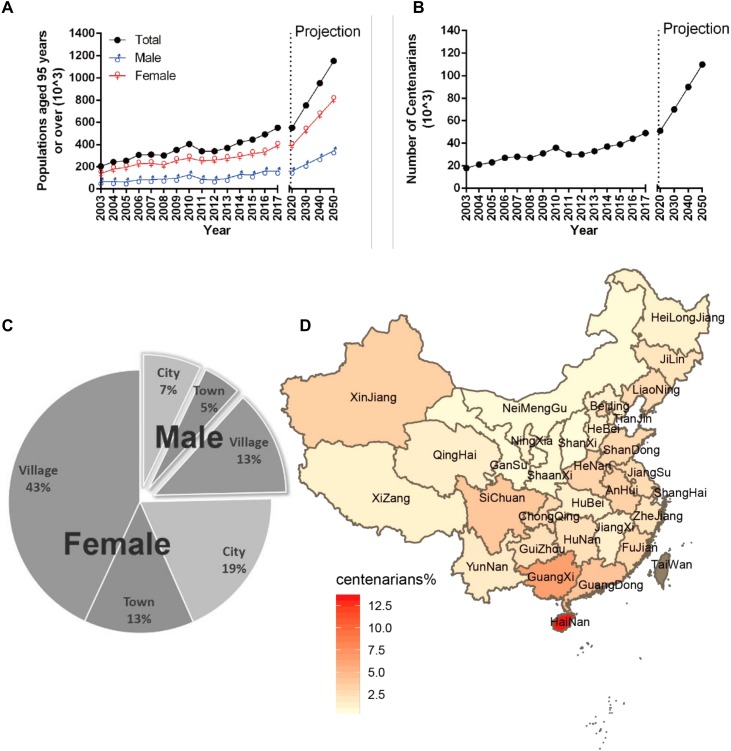
The research agenda in response to rapid population ageing in China has been broad, covering areas including the study of the ageing process itself in laboratory and animal studies, to clinical-level studies of drugs or other treatments for common chronic diseases, and finally policy-level research for the care of the elderly in hospital, community and residential care settings, and its influence on health and social care policies (Fang et al., 2015). Chinese population statistics taken between 1950–2050 show a reduction in crude death rate (CDR) and total fertility rate (TFR), accompanied by an increase in life expectancy at birth and an expansion of the population aged 65 and above (65+, termed the elderly) (Fig. 1 A). As of 2019, the population of mainland China constitutes 18 % of global total, with 164.5 million Chinese citizens aged 65+, 26 million of whom are 80 + . By 2050, it is expected that there will be 1.4 billion Chinese, with 365 million aged 65+, a number representing 26.1 % of the country’s total population (Fig. 1B). Furthermore, among this ageing population, 115 million are expected to reach an age of at least 80 and 0.6 million are expected to become centenarians (Fig. 1B). When compared with their counterparts born a decade earlier, the current 80+ generation has reduced annual mortality and disability rates, but has increased cognitive impairment and reduced objective physical performance capacity (Zeng et al., 2017b).
Fig. 1.
Age-related demographic factors and the changing population demographics over time, as well as disease demographics in the elderly in Mainland China. A. Changes of crude death rate (CDR), total fertility rate (TFR), % population ≥ 65 years old, and life expectancy at birth (years) from 1950 to 2050. B. The changing population demographics in China in 1950, 2019, and a predicted figure in 2050. Horizontal bars are proportional to number of males (blue) and females (red). *For 1950, data of 5-year groups over 80 are absent, thus are shown in 80 + . Data source: Population Division of the Department of Economic and Social Affairs of the United Nations. (see: https://population.un.org/wpp for more details). C-D. Demographics showing the major diseases affected to (C), and death in (D) the elderly in China between 1990 (yellow) and 2017 (green). Data source: Global Burden of Disease Study 2017 (GBD 2017) Results, Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2018. Available from http://ghdx.healthdata.org/gbd-results-tool.
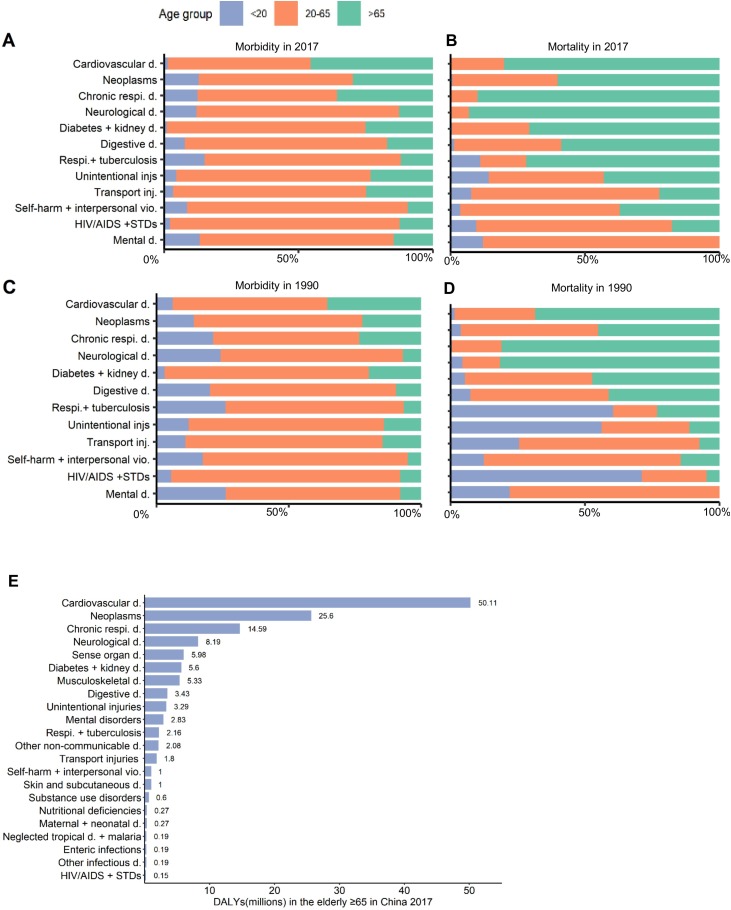
To achieve what may be considered a ‘healthy ageing society’, it is first important to address and prepare for the challenges and issues that are associated with rapidly ageing populations. Ageing is the primary driver of most, if not all, chronic diseases, including cancer, cardiovascular diseases, diabetes, and neurodegenerative diseases, particularly Alzheimer’s disease (AD) and Parkinson’s disease (PD) (Kerr et al., 2017; Lautrup et al., 2019; Lopez-Otin et al., 2013). The most predominant diseases affecting the elderly in China (65+, data from 2017) include sensory diseases, other non-communicable diseases, digestive diseases, respiratory infections and tuberculosis, skin and subcutaneous diseases, neurological diseases, and musculoskeletal disorders, among others (Fig. 1C). From 1990–2017, there were dramatic increases in prevalence of all 21 diseases, excluding a very minor reduction in ‘neglected tropical diseases and malaria’ (Fig. 1C). The major diseases responsible for death of the elderly in China are cardiovascular diseases, neoplasms, chronic respiratory diseases, and neurological diseases, among others (Figs. 1D and 2 ). Compared to their younger counterparts, the elderly population are more fragile, and susceptible to conditions such as cardiovascular diseases, chronic respiratory diseases, diabetes, kidney diseases, unintentional injuries, HIV/AIDS and sexually transmitted diseases (STDs), among others (Fig. 2B). In comparison with data from 1990, new patterns of disease mortality characterize the modern elderly, such as a dramatic reduction in the percentage of death contributed by ‘neurological disorders’ with an increase in deaths due to HIV/AIDS and STDs (Fig. 2B, D). Recognition of the current disease demographics in the elderly in China, and accurate prediction of future trends will enable us to be best prepared for different healthcare needs at different times.
Fig. 2.
Morbidity and mortality of selected diseases by age in 2017and 1990. (AB)— Morbidity (A) and mortality (B) in the elderly in China in 2017. (CD)— Morbidity (C) and mortality (D) in the elderly in China in 1990. The three age groups used were <20 years, 20-65 years, and >65. Data source: Global Burden of Disease Study 2017 (GBD 2017) Results, Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2018. Available from http://ghdx.healthdata.org/gbd-results-tool. (E) Disability-adjusted life years (DALYs) (millions) in the elderly (65+) in China in 2017.
In wake of the expanding ageing society in China, and the formidable socio-economic and healthcare challenges, we offer the 2nd edition of our previously published review (Fang et al., 2015). Here, we aim to provide an update regarding the situation of the elderly in China using a range of expertise and suggestions from multiple fields which may further propel the exciting and ongoing reforms to China’s healthcare system. We hope to explore different ageing care models that can be used to best produce a healthy ageing society (Chen, 2009; Yip et al., 2019; Zhan et al., 2019). The following sections highlight recent developments in the above areas as well as areas for future research.
2. Primary challenges for the elderly in China
Based on ageing phenotypes and the major disease demographics in the elderly in China (Fig. 1, Fig. 2), we chose to focus on frailty (including sarcopenia as an independent subsection), CNCDs (including cardiovascular disease as an independent subsection), mental health disorders, dental health challenges, elderly infections and immune diseases, as well as HIV, syphilis, and other STDs. In view of recent reviews on other grand challenges, including cancer (Chen et al., 2016; Tsoi et al., 2017), chronic respiratory diseases (Zhu et al., 2018), diabetes and kidney diseases (Hu and Jia, 2018; Wei et al., 2019), these areas will not explored here.
2.1. Frailty
Frailty is a biologic syndrome characterized by deteriorating function across a broad spectrum of physiological symptoms (Fried et al., 2001). It can be thought of as a state of vulnerability. Some have proposed an index approach to categorize different degrees of frailty; however, these attempts are complicated by the multidimensionality of the underlying causes of frailty, thus creating a dynamic, ever-changing value that is difficult to index (Rockwood et al., 2006). The term physical frailty has been applied to age-related loss of muscle mass and function, that is sarcopenia (detailed in the next section). In recent years, frailty research has increased rapidly in China as a strategy to prevent disability in response to an ageing population (Chhetri et al., 2019). Research projects were showcased in the following scientific conferences: The 1st and 2nd International China Conference on Frailty in China, jointly organized by the WHO Collaborating Centre on Frailty, Clinical Research and Geriatric Training at the Gerontopole, Toulouse, France, the Chinese Embassy in Paris, and the National Clinical Centre for Geriatric Diseases, China, and the 4th Asian Conference for Frailty and Sarcopenia in Dalian in October 2018, organized by the Chinese Geriatrics Society, Beijing Institute of Geriatrics and Gerontology and the Chinese Health Promotion Foundation. Wide-ranging topics included basic science, epidemiology, definitions and measurements, management, as well as service models. Such conferences greatly accelerate basic and clinical research on as well as clinical treatment for frailty.
Frailty may be used as a population indicator of ageing, and be a useful indicator of a need for treatment. Research into prevalence, risk factors, prevention, and incorporation into service delivery models in community, hospital and residential care settings are an important part of the ageing research agenda for China. The importance of recognizing frailty in community-dwelling older people in China has been highlighted in a systematic review and meta-analysis by He et al. (He et al., 2019a). Risk factors for a worsening in frailty among community-living older adults include hospitalizations, older age, previous stroke, lower cognitive function, diabetes and osteoarthritis, while higher socioeconomic status and neighborhood green space were protective factors (Lee et al., 2014; Yu et al., 2018c). A comparison of prevalence and incidence of frailty between populations may stimulate further research into prevention strategies and inform government policies. Using data from a nationally representative study, Wu et al. found that 7% of community-dwelling adults aged 60 years or above were frail in mainland China and the prevalence increased dramatically with age, reaching 32.5 % for those aged 85 years or above (Wu et al., 2017). Substantial regional disparities exist in the prevalence as well as incidence of frailty in mainland China. For example, the incidence rate of frailty in the Northeast was more than double than that in the Southeast (Xu et al., 2019). Furthermore, a comparison of frailty and its contributory factors across three Chinese populations (Hong Kong, urban and rural populations of Taiwan) using the ratio of frailty index (FI) to life expectancy (LE) as an indicator of compression of morbidity showed higher FI/LE in Taiwan compared with Hong Kong. Risk factors include low physical activity and living alone (Yu et al., 2017). The importance of protein intake to slow the decline in muscle mass and physical function over four years supports the importance of nutrition as an underlying factor for physical frailty (Chan et al., 2014).The role of inflammatory cytokines in the pathophysiology of sarcopenia is supported by the finding of slower decline in grip strength for those in the highest quartile of telomere length (Woo et al., 2014b). Simple tools for frailty and sarcopenia may be used in a community setting as case finding, without the need for professionally trained personnel (Woo et al., 2014a, b). This may represent the first step in the approach to community-based intervention such as group exercises with or without nutritional supplementation for frailty and sarcopenia (Yu et al., 2020; Zhu et al., 2019).
How community services may be developed to make frailty as a cornerstone of health and social care systems (Woo, 2018) depends on the development of existing community infrastructures. Two examples have been described previously: the Tai Po Cadenza Hub, and the Jockey Club E health project, where screening data based on the WHO Integrated Care for Older People Toolkit (WHO, 2020) were collected via iPad, followed by action algorithms for items where action is indicated: e.g., frailty, sarcopenia. This model emphasizes the empowerment of older people and their care-givers, societal-level behavioral changes, and the use of technology in the absence of a low cost primary care system orientated to meeting the needs of older people (Woo, 2019). In the hospital setting, detection of frailty may inform choice of therapies and prognosis, such as mortality and hospitalization in chronic heart failure (Yang et al., 2018).
2.2. Sarcopenia
Closely related to the concept of frailty, sarcopenia is an age-related gradual loss of mass and strength of skeletal muscles resulting in reduced physical performance. Major pathological features include a loss of satellite cells and motor neurons, as well as less active neuromuscular junctions (Cruz-Jentoft et al., 2010). Following the publication of the European Consensus Group on Sarcopenia (Cruz-Jentoft et al., 2019, 2014), an Asian group including Chinese researchers formed a panel to arrive at a consensus on the definition of sarcopenia, published in 2014 (Chen et al., 2014), and recently updated in 2019. The Asian criteria differed from the European Consensus Definitions. An individual International Statistical Classification of Diseases and Related Health Problems code (M62.84) was assigned to ‘sarcopenia’ which has stimulated both diagnostic and therapeutic trials worldwide. In China, sarcopenia diagnosis requires some special considerations, including anthropometric and cultural differences. The 2019 guideline of Asia Working Group of Sarcopenia (AWGS) provides updated guidelines on epidemiology, case-finding, the diagnostic algorithm, measurements of muscle mass, muscle strength and physical performance, and intervention and treatment. The prevalence of sarcopenia is estimated to be between 7.3–12.0 % among the general older population and was over 25 % in the oldest populations (85+) (Hu et al., 2017; Wang et al., 2018a; Woo et al., 2015a; Xu et al., 2020a, 2020b; Yu et al., 2014). While old age is the primary risk factor for sarcopenia, other risk factors in the Chinese population include household status, lifestyle, physical inactivity, poor nutritional and dental status, and some diseases (osteoporosis, metabolic diseases, etc.). In terms of longer-term clinical outcomes, AWGS-defined sarcopenia was significantly associated with increased risks of physical limitations at 4 years, slowness at 7 years, and 10-year mortality, but not of hospitalization (Hu et al., 2017; Wang et al., 2018a; Woo et al., 2015a; Yu et al., 2014).
Interventional strategies for the elderly of China have been the subject of recent research. For instance, an intervention for community-dwelling older adults yielded significant improvements in muscle function based on which when protein was offered as an oral nutritional supplement in combination with resistance exercises (Kang et al., 2019). Similar findings were reported in a community-based intervention in Hong Kong where resistance exercise plus nutritional supplements comprised of branched chain amino acids, vitamin D, whey protein, and hydroxymethylbutyrate (HMB)-enriched milk were found to significantly increase physical function, muscle mass and strength (Zhu et al., 2019). Additionally, pharmacotherapies against sarcopenia are emerging in the West, which may be further tested in the Chinese population. Selective androgen receptor modulators were partially effective in increasing muscle mass but not muscle strength or function, while myostatin neutralizing antibodies or induction of an IIB receptor blockade may increase skeletal muscle mass (ASM) and aspects of functional performance, though these findings need to be further verified in the clinic (Rooks and Roubenoff, 2019).
2.3. Non-neuronal chronic non-communicable diseases (CNCDs)
In addition to frailty, the most common health problems among the elderly of China are chronic diseases, especially CNCDs. China has experienced an epidemiological transition, shifting from death due to acute infectious diseases to death due to CNCDs in a much shorter time than many developed countries. CNCDs account for an estimated 86.6 % of total deaths in China, with the five leading causes of death in 2017 being stroke, ischemic heart disease, lung cancer, chronic obstructive pulmonary disease (COPD), and liver cancer (Zhou et al., 2019). Cardiovascular diseases (covering ischemic, etc.) are common in the elderly of China, and this will be detailed in the next section. Nearly 45 % of the disability-adjusted life years (DALYs) in China are attributable to health conditions among older adults, with cardiovascular disease, cancer, pain, and COPD being the leading causes (Wang et al., 2019b; WHO, 2014). The prevalence of CNCDs is high among older community-dwelling Chinese adults and increases with age. In total, 76.3 % of adults aged 60+ years have at least one CNCD (Wang et al., 2019b; Yao et al., 2019). Among adults aged 60+ years, nearly 60 % have hypertension, 25 % have arthritis, ∼20 % have diabetes, over 15 % have COPD, and ∼7% have cardiovascular disease (CVD, 2.1 % myocardial infarction and 4.8 % stroke) (Wang et al., 2019b; WHO, 2015a). There are huge socio-demographic disparities in the burden of CNCDs among older Chinese adults. For example, diabetes is more prevalent among women, urban residents, and those with a higher level of education. Multimorbidity—co-occurrence of two or more chronic conditions—is strongly associated with an increased risk of hospitalization, disability, and mortality (Lochner and Cox, 2013; Tinetti et al., 2012). Multimorbidity is common among older Chinese adults. Over 40 % of adults aged 50+ have multiple, simultaneously occurring NCDs and the prevalence increases with age (Yao et al., 2019).
Major behavioral risk factors that are responsible for CNCDs are prevalent among the elderly in China. Nearly 80 % of deaths are attributable to unhealthy diet, high blood pressure, smoking, high glucose, air pollution (indoor and outdoor), and physical inactivity (WHO, 2014). In China, 56.6 % of adults aged 60+ have insufficient dietary balance (daily intake of <400 g fruit and vegetables), 22.4 % are current smokers, 45 % use unclean fuel for cooking, 84 % are physically inactive, and 11.4 % have harmful alcohol use (WHO, 2012). Risk factors for major CNCDs, particularly smoking and alcohol use, are unevenly distributed among older men and women. The prevalence of cigarette smoking is substantially higher among men (41.5 %) than women (4.3 %). The prevalence of harmful alcohol use among men is more than three times as much as that among women (13.3 % vs. 4%). Substantial rural-urban disparities in the distribution of risk factors exist among older Chinese adults. Rural residents have a higher prevalence of smoking (23.7 % vs. 19.9 %), harmful alcohol use (13.3 % vs. 7.5 %), insufficient dietary intake (60 % vs. 49.5 %), and unclean fuel use (89 % vs. 7.1 %) than those in urban areas, while residents of urban areas have a substantially higher prevalence of physical inactivity than their rural counterparts.
2.4. Cardiovascular disease
Cardiovascular disease (CVD) constitutes a significant part of CNCDs and because of its prevalence in the elderly of China, we decided it warranted an independent section. It is estimated that the current number of patients with CVD is 290 million (Zhao et al., 2019). In 2016, CVD was ranked first in mortality rates, higher than the mortality rates attributed to tumors and other prevalent diseases. Studies have shown that in 2013, age-standardized CVD mortality in China was 21 % lower than in 1990 (GBD, 2015; Zhou et al., 2019). Although the age-standardized CVD mortality rate has declined, the absolute number of CVD deaths is still rising rapidly, and increased by 46 % between 1990 and 2013. CVD is a large burden for the Chinese healthcare system. With the development of medical technology, and the government's focus on chronic disease management, the problem of CVD in China has improved. However, due to the problems arising from population ageing, CVD still has a great impact on national health.
Major factors for CVD include hypertension, dyslipidemia, diabetes, air pollution, and excess weight (overweight and obesity). Some risk factors are specific to China compared to other countries, however, this is changing as China's economy develops and the population ages. Hypertension is an important public health problem in China. The prevalence of hypertension in China among those over the age of 18 is 23.2 %, and the number of patients with hypertension in China is estimated to be 245 million (Wang et al., 2018c). In 2013, 2.5 million deaths were attributed to hypertension in China, accounting for 27.5 % of all causes of death (Trammell et al., 2016). With the rapid development of the economy and the ageing population, problems with blood lipid levels in China have gradually increased, and the prevalence of dyslipidemia has increased significantly. The main symptoms of dyslipidemia seen in China are low levels of low-density lipoprotein cholesterol (LDL-C) and hypertriglyceridemia (Pan et al., 2016), while dyslipidemia in the West is characterized by hypercholesterolemia and high levels of LDL-C (Toth et al., 2012). With the change of lifestyle following China’s economic development, the number of Chinese diabetic patients is growing. Overall, 47 % of adults in China have diabetes or pre-diabetes, which is slightly lower than the 49–52 % in the United States (Wang et al., 2017). In recent years, there has been a significant increase in the prevalence of excess weight (BMI: 24.0–27.9 kg/m2) and obesity (BMI ≥ 28.0 kg/m2) in Chinese residents, as noted over a five-year study period (He et al., 2017b). The prevalence of combined overweight and obesity among men was 33.8 %.
Air pollution is another important factor leading to CVD. Among different particles, PM2.5 (an aerodynamic diameter of 2.5 μm or less) is most closely related to CVD (Brook et al., 2010). A follow-up study of cohorts of elderly people 65+ in Hong Kong showed that for every 10 μg /m3 increase in PM2.5 concentration, the risk of total CVD death increased by 22 % (Wong et al., 2015). Air pollution is also associated with increased blood pressure. For each 10 μg/m3 increase in PM2.5 concentration, the per capita systolic blood pressure level increased by 1.30 mmHg, the per capita diastolic blood pressure level increased by 1.04 mmHg, and the risk of hypertension increases by 14 % (Lin et al., 2017).
Coronary heart disease, atrial fibrillation (AF), heart failure, and atherosclerosis are common forms of CVD. Technological developments have allowed for an increase in treatment options and testing methods, including percutaneous coronary intervention (PCI), radiofrequency ablation, Implantable Cardiac Defibrillator (ICD) and pacemaker implantation. Since elderly patients are often associated with more complications, treatment decisions for CVD in elderly patients need to be adjusted individually based on an overall scoring of health. Coronary heart disease is a common fatal CVD. For the treatment of coronary heart disease, the number of PCI cases has steadily increased in China (Zhao et al., 2018b). The CREATIVE study explored antiplatelet treatment options for patients after PCI in China, and studies have shown that for patients with low response to antiplatelet drugs after PCI, a triple antiplatelet intensive therapy combined with cilostazol is safe and effective (Tang et al., 2018). Bleeding events should be paid special attention when administrating dual antiplatelet treatment to ACS patients aged 75 and older receiving PCI (Zhao et al., 2018a). The risk of all-cause, cardiovascular, and stroke deaths in patients with AF is significantly higher than in patients with sinus rhythm (Li et al., 2015). The proportion of Chinese patients receiving anticoagulation treatments is low. Only 12.7 % of patients with AF and a CHADS2 score of 2 or more received anticoagulation treatment (Zhang et al., 2014). Patients with AF aged 75+ tend to higher CHADS2 scores but receive less anticoagulation therapy. The risk of one-year follow-up deaths and adverse events in the elderly is more than doubled compared to other populations (Shao et al., 2014; Yang et al., 2014). Cases of AF ablation procedures and ICD implantation have steadily increased in China. However, European DANISH studies suggest that primary prevention through ICD implantation has limited benefits in elderly patients with non-ischemic cardiac diseases (Kober et al., 2016). Therefore, it is necessary to pay attention to the indications when expanding the population eligible for ICD implantation in China.
In recent years, the etiology of heart failure in China has changed significantly. The proportion of valvular disease (especially rheumatic valvular disease) has decreased. As China is becoming an ageing society, the number of elderly patients with heart failure has increased. At present, most studies suggest that coronary heart disease is a common cause of heart failure in the elderly, and the proportion of hypertension and pulmonary heart disease in elderly patients with heart failure increases with age. In recent years, the use of diuretics in hospitalized heart failure patients in China has not changed significantly, while the usage rate of digoxin has shown a downward trend. The use of ACEI, ARB, aldosterone receptor antagonists and beta-blockers have shown a significant upward trend (Zhang et al., 2017). Lower extremity atherosclerotic disease (LEAD) is a common disease in the elderly and an important starting point for systemic atherosclerosis. Early detection of LEAD is of great value in the diagnosis and treatment of systemic atherosclerosis (Hiramoto et al., 2018).
To reduce the burden of CVD in China, we recommend interventions directed at altering lifestyles and programs dedicated to the detection and management of risk factors, especially for elderly people. Research modeling has shown that if dyslipidemia and hypertension are effectively managed, medical expenses to the tone of $932 billion US from 2016−2030(Stevens et al., 2016). Controlling blood lipids and blood pressure of elderly people over 65 years of age represents the most cost-effective strategy (Stevens et al., 2016).
2.5. Mental health disorders
Mental health disorders, particularly dementia and depression, are major diseases in the elderly of China. Alzheimer’s Disease International (ADI) estimates that over 50 million people worldwide were living with dementia in 2019, and that this figure will rise to 152 million by 2050; the current annual cost of dementia is estimated at 1 trillion US dollars which will be doubled by 2030 (ADI, 2019). It is estimated that the number of patients with dementia in China constitutes 25 % of the dementia population worldwide, with the prevalence of dementia ranging from 5.14 % (95 % Ci 4.71–5.57, in 2014) to 5.60 % (95 % Ci 3.50–7.60, in 2019) for individuals aged 65+ (Huang et al., 2019; Jia et al., 2014, 2020). The patterns and spread of dementia in China vary geographically and between genders. Women are 1.65 times more susceptible than men. Western China has a higher prevalence at 7.2 %, while Central and Northern China are lower at 5.2 and 5.5 %, respectively, Southern China has the lowest prevalence at 4.8 %, this variation is possibly due to a variety of reasons including diet, exercise, social networks, healthcare, etc. (Chan et al., 2013; Jia et al., 2020; Wu et al., 2018b). The incidence of dementia in individuals aged 65+ ranged from 17.7–24.0 per 1000 person-years using 10/66 Dementia Research Group Criteria, while it was 12.14 per 1000 person-years using DSM-IV Criteria (Jia et al., 2020; Prince et al., 2012; Yuan et al., 2016). While health conditions such as depression, diabetes mellitus, and insomnia correlate with dementia in a global fashion, epidemiological evidence from different regions in China also suggests smoking and heavy alcohol consumption as high risk factors (Fan et al., 2019; Pei et al., 2014; Xue et al., 2019).
Depression, a risk factor for dementia, is a common but often neglected disease in the elderly in China (Fang et al., 2015). Data from a cross-sectional study suggest a prevalence of depression of 39 % in the elderly which increases to 45 % in the most elderly (Yu et al., 2012). In view of the stigma of mental illness in some areas of China coupled with inadequate health services in rural areas, depression is likely underdiagnosed suggesting the real prevalence may be higher. In addition to its contribution to dementia, depression aggravates the quality of life of the elderly and of their family members, brings the risk of death caused by different reasons, and accordingly is a heavy burden on the society and the healthcare system (Zhang and Li, 2011).
Much effort should be made to address mental health disorders in China, including increasing government investment, the training of more geriatric care professionals with specialties in mental disorders, and raising public awareness, especially in conjunction with more active social activities and exercises. Although there have been increased care facilities for citizens 65+ and improved access to health services, the diagnosis and management of dementia and depression are still inadequate, especially in rural areas (Jia et al., 2020). The inclusion of steps to manage dementia in the 13th Five-Year Plan of the central Chinese Government marked a major step forwards, and such efforts need to be continued. In view of the insufficiency of medical professionals in regards to mental disorders, especially in rural areas, we recommend increased training to such professionals, and the development of policies to encourage health professionals to work (at least for a short period) in rural areas (Fang et al., 2015). In recent years, the public awareness of mental disorders, especially AD, has greatly improved thanks to efforts from social media (e.g., drama shows on AD) and dementia organizations. Professional interventions, comprising medicine and combined cognitive-psychological-physical intervention (e.g., family and community support plus playing mahjong and practicing Taichi) can mitigate subclinical depression and improve overall mental health (Kong et al., 2019; Wang et al., 2019c; Wong et al., 2014). Although no drug at present is available to cure AD, recent progress on the understanding of AD etiology, such as the involvement of impaired mitophagy and reduced grid-cell-like representations in the human AD brain, along with the development of novel stem cell models, and the use of artificial intelligence (AI), will undoubtedly propel the development of novel drugs (Fang, 2019; Fang et al., 2019; Gilmour et al., 2020; Kunz et al., 2015; Lin et al., 2018). The China Brain Project, covering studies on basic neuroscience, brain diseases, and brain-inspired computing, will greatly benefit the development of novel drugs for different neurological diseases (Poo et al., 2016).
2.6. Dental health challenges
While oral health is an important part of the whole body, the prevalence of oral disease is high in the elderly in China, but is largely ignored, while here we focus on dental health. Dental caries (tooth decay), periodontal disease and tooth loss in the elderly are issues of global health concern. The burden on healthcare cost and the quality of life of these dental diseases in the elderly remain high (Lopez et al., 2017). Maintaining good dental health is an integral part of healthy ageing. As such, developing effective preventive and therapeutic interventions are needed to protect and enhance dental health and well-being (Lopez et al., 2017; Tonetti et al., 2017). Dental caries and periodontal diseases are common oral diseases in the elderly and often lead to tooth loss, edentulism (toothlessness), impaired masticatory function and poor nutrition. According to the 4th National Oral Health Epidemiological Survey (FNOHES, 2015–2016) covering the whole of mainland China, caries and periodontal diseases are highly prevalent in the elderly in China; while the prevalence of caries was above 50 % in all age groups (3–5, 12–15, 35–44, 55–64, and 65–74 years), the rate was 98 % in the 65–74 years groups (Lu et al., 2018; Si et al., 2019). In adults aged 65–74 years, 90.7 % had periodontal diseases, including gingival bleeding (82.6 %), dental calculus (90.3 %) and a deep periodontal pocket (14.7 %) (Lu et al., 2018; Si et al., 2019). Human oral tissues naturally and gradually degrade with age; a fact also exacerbated by modern lifestyle choices, including the prevalence of sugary diets and a lack of oral hygiene (Belibasakis, 2018; Lamster et al., 2016). More specifically, age-dependent changes include a reduction in periodontal support, loss of elastic fibers, and thickening and disorganization of collagen bundles in the connective tissue of the oral mucosa (Belibasakis, 2018; Lamster et al., 2016; Wu et al., 2016b). Severe dental health challenges can cause loss of self-esteem, social difficulties, while also being drivers of common diseases, such as AD, PD, diabetes, and hypertension (Belibasakis, 2018; Bollero et al., 2017; Dominy et al., 2019; Lamster et al., 2016).
Major risk factors of the high prevalence of dental diseases in the elderly in China include the scarcity of dental health knowledge in the general population, low frequency of daily oral hygiene practices, insufficiency of dental care services, and unhealthy diet habits. Daily oral hygiene practices are effective for removing plaque and preventing gingivitis. The average awareness rate of dental health in the Chinese elderly was 47.6 %, only 30.1 % of the elderly brush their teeth twice daily, and a mere 0.8 % used dental floss (Lu et al., 2018; Si et al., 2019; Xu et al., 2020a).
Increased attention to the dental health needs of an ageing population urgently requires combined efforts by relevant stakeholders (Lu et al., 2018; Si et al., 2019; Tonetti et al., 2017; Xu et al., 2020a). Specifically in the case of older adults, knowledge and competence in oral care, awareness of medical comorbidities and of medications relevant to oral care should all be strengthened. Epidemiological surveillance and monitoring of oral diseases and oral health-related quality of life in the elderly is needed. Oral self-care, access to treatments and preventive services and assuring the affordability of dental care are critical for oral health. Looking after teeth and gums by brushing twice a day with fluoride toothpaste and cleaning with dental floss are effective in achieving a good oral health status. Likewise, the control of risk factors, such as refraining from the frequent consumption of foods and drink high in sugar, and refraining from smoking, are also important. Provisions to expand services to older adults, to meet increasing oral healthcare needs in the ageing population, and to ensure the affordability of dental care should all be emphasized by policymakers. We suggest programs that promote general oral health education as well as public outreach programs directed towards the elderly via understandable brochures, and the use of television and other social medias. Additionally, it is important to improve the country’s dental care infrastructure by training more dentists and oral specialists and ensuring the provision of affordable dental healthcare.
2.7. Elderly infections and immune diseases
It has been well documented that altered immune system components and function are characteristic of ageing and form part of the causes of age-related diseases (Nikolich-Zugich, 2018). In ageing, a significant decline in the homeostatic, defensive, and surveillance functions of the immune system is noted. Prominent features of the ageing immune system include thymus involution, a decrease in naïve lymphocytes, and an accumulation of memory and senescent lymphocytes; more recently, the concept of ‘inflammageing’ has been developed (Ferrucci and Fabbri, 2018). Functionally, impaired immune defense, especially against new antigens for which no memory exists, makes older adults increasingly vulnerable to incident and more severe infections. In addition, a decline in immune surveillance hampers the elimination of premalignant cells, leading to cancer development. Older adults also manifest a chronic low-grade inflammatory phenotype (CLIP), a manifestation of the inflammageing concept, that likely results from uncompensated inhibitory immune regulation and/or an inability to eliminate senescent cells (Chen and Yung, 2019; Chen et al., 2019b). As such, immune dysregulation is a general feature of ageing.
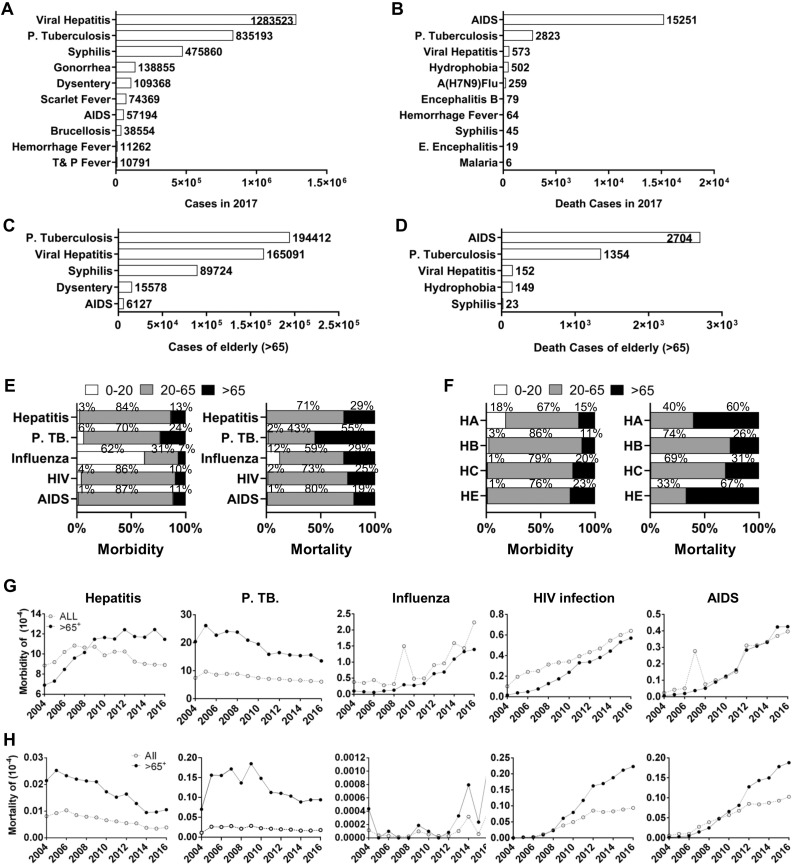
Here we provide an update on infectious diseases in the elderly in China. We carried out a comprehensive review on infections in China based on the following public databases: the Chinese Center for Disease Control and Prevention (CCDC), The Data-center of China Public Health Science (CCDC, 2019), and the National Bureau of Statistics of China (NBSC, 2019). The three most common infectious diseases in 2017 were viral hepatitis, pulmonary tuberculosis (TB) and syphilis (detailed in section 2.8) while the three with the highest mortality rate were AIDS, TB, and viral hepatitis (Fig. 3 A-D). Of note, pulmonary TB was more prevalent than the other two in older adults over 65 years of age (Fig. 3C). Generally speaking, infectious diseases are more frequent and deadly in older adults, as seen with the recent 2019-nCoV epidemic worldwide (Chen et al., 2020; Huang et al., 2020); thus, infectious diseases deserve more attention.
Fig. 3.
A summary of morbidity and mortality of major infectious diseases in China. A-B. Reported infectious cases (A) and death cases (B) of statutory top 10 infectious diseases by Chinese Center for Disease Control and Prevention (CCDC) in 2017. C-D. The top 5 infectious cases (C) and death cases (D) of the 65 years or older in 2016. E. The morbidity and mortality of viral hepatitis, pulmonary tuberculosis (P.TB), influenza, HIV infection and AIDS by Age. The 3 age groups used were as <20 years, 20-65 years, and 65 years or older. F. The morbidity and mortality of the subtypes of viral hepatitis by Age. The 3 age groups used were as <20 years, 20-65 years, and 65 years or older. G-H. Morbidity and mortality trends of five infectious diseases by age from 2004 to 2016. The morbidity (C) and mortality (D) rate (per 10,000 people) of viral hepatitis, pulmonary tuberculosis (P.TB), influenza, HIV infection and AIDS from 2004 to 2016 were extracted and presented as general (open) or aged (65 years or older, closed) population. All data were collected from China Public Science and Health Data Center (CPC) (www.phsciencedata.cn).
2.7.1. Viral hepatitis
Viral hepatitis is caused by the hepatitis viruses A, B, C, D, and E (HAV, HBV, HCV, HDV, HEV) and is prevalent throughout the world, posing a significant threat to human health. China is a highly epidemic area of viral hepatitis with 86.6 million people infected with HBV and 7.6 million infected with HCVas of 2018 (WHO, 2018). In 2018, there were 1.28 million new cases and 531 deaths among the Chinese population (NBSC, 2018). According to the Chinese Statutory Infectious Disease Report, viral hepatitis mainly occurred in adults between 20–65 years old (83.68 %, Fig. 3E). Its morbidity in older adults was estimated to be 13.52 % in 2016 (Fig. 3E). However, compared with the morbidity, the mortality of viral hepatitis was higher (28.31 %) in the aged population (Fig. 3E). From the survey, the morbidity and mortality rate of viral hepatitis have ranked in the top five for many years. The morbidity of viral hepatitis was stable in last decade, which is likely due to the wide usage of the hepatitis vaccine (Fig. 3G, H). However, the morbidity of hepatitis in the elderly continues to increase yearly. Since most cases of viral hepatitis developed into chronic hepatitis, the lifespan extension seen in China has contributed to a higher number of elderly hepatitis cases. Luckily, the mortality of hepatitis has declined in both the aged population and the population at large (Fig. 3H).
Among the five hepatitis viruses, HDV is rarely detected and is not discussed here. HCV (20.13 %) and HEV (22.6 %) demonstrated high morbidity in the aged population (Fig. 3F). However, the highest mortality is caused by two acute types, HAV (60 %) and HEV (66.7 %) (Fig. 3F), indicating a weakened immune responses against acute infection in the elderly. Significantly, both the morbidity and mortality of HBV in the aged population were lowest among the four types (Fig. 3F), further indicating the benefit of the HBV vaccine. However, prophylactic vaccines for HCV and other types of viral hepatitis are still lacking. For patients who have been infected, current treatments are still limited, especially for the elderly patients. One of the reasons for this is the lack of a long-term infection model for use in laboratory conditions (Winer et al., 2017). Developing an elderly-representative model would be a useful tool for screening treatment options for those affected by hepatitis diseases.
2.7.2. Tuberculosis
Tuberculosis (TB) is a potentially serious infectious disease affecting the lungs caused by Mycobacterium tuberculosis and is typically transmitted through coughs and sneezes. The lack of global TB control is the result of several factors, including HIV coinfection, limited vaccine efficacy, a lack of highly specific and sensitive diagnostic tests, and the rise of multi-drug-resistant (MDR) and extensively drug-resistant (XDR) TB strains (Venketaraman et al., 2015). According to the WHO’s 2019 Global Tuberculosis Report, China is ranked third in terms of TB burden when compared with other countries (WHO, 2019a). Pulmonary tuberculosis (P-TB) is the second highest ranked cause of morbidity and mortality among the 28 infectious diseases ranked in 2017 (Fig. 3A, B). However, it is the most frequent infectious disease in the elderly (Fig. 3C). The elderly occupied more than half (54.9 %) of all deaths from P-TB (Fig. 3E). In the last decade, the incidence of P-TB has decreased year to year, however, the incidence and mortality rates of P-TB in the elderly remains high in China (Fig. 3G, F). There are several reasons for the high incidence and mortality rates of P-TB in the elderly: i) An increasingly ageing population; ii) immune decline; iii) delay of diagnosis and treatment. With the increase of the number of elderly patients, P-TB is rapidly becoming a new public health challenge.
Several risk factors, such as immune decline, smoking, malnutrition, HIV infection and other chronic diseases, make the elderly susceptible to TB (Zhang et al., 2019a). Compared with P—TB in the young, PT—B in the elderly has its own characteristics. Elderly patients with P—TB are more contagious than the young, and elderly men are more likely to suffer from tuberculosis than elderly women (Lee et al., 2017). In the elderly, early symptoms of TB are atypical and insidious, and can result in misdiagnosis (Rajagopalan, 2001). Furthermore, chronic fibrous cavitation and hematogenous disseminated TB are more common in the elderly population. Most elderly patients with P—TB get TB in their youth at which time it is better controlled but, as they age, P—TB can result as immune function declines. Moreover, elderly TB patients usually present with several complications, which further complicates diagnosis and treatment (Nagu et al., 2017). All these characteristics have brought special focus on the treatment and diagnosis of TB in the elderly. At present, there are several TB guidelines for high-risk groups (WHO, 2016b), but few for the elderly. Previous studies in the elderly have also focused less on the evaluation of targeted strategies for control and prevention. Thus it is necessary to pay more attention in the future to the production of control programs and evaluation of targeted interventions for TB in the elderly.
2.7.3. AIDS
AIDS is a chronic, potentially life-threatening infectious disease caused by HIV, which was first detected in the United States in 1983 (Barré-Sinoussi et al., 1983). In the last decade, the morbidity and mortality of HIV/AIDS has increased yearly (Fig. 3G, H), and it has become the top cause of death by infectious disease in China, including in the elderly (Fig. 3B, D). The morbidity and mortality of HIV/AIDS in the elderly population is also rising significantly, and notably the mortality in the elderly is much higher than that seen in the young (CCDC, 2016). Furthermore, because elderly people have many basic diseases and low awareness of self-testing after HIV infection, the elderly are more likely to already be AIDS patient at the time of diagnosis of their HIV infection (Xing et al., 2014). A study has shown that 35.5 % of newly diagnosed elderly HIV infectors had already developed into the AIDS stage (Liu et al., 2012).
With increasing use and efficacy of antiretroviral therapy for HIV infection, the lifespan of HIV/AIDS patients has been greatly extended, and more and more HIV/AIDS patients will enter old age (Nizami et al., 2019). The problem of HIV/AIDS in the elderly will become increasingly serious in the future. Firstly, HIV infection is not commonly checked in the elderly in China upon visit to the hospital, which may lead to uncontrolled disease progression and infection to others. Second, the treatment of aged HIV/AIDS patients may cause more adverse effects, such as cardiovascular disease (Hanna et al., 2016; Kramer et al., 2009), AD (Brousseau et al., 2009), and diabetes (Guaraldi et al., 2018). Furthermore, cognitive disorders, loneliness, shame and depression may increase the likelihood that they fail to follow their drug regimen, or refuse treatment altogether (Greene et al., 2018; Vincent et al., 2017). Interestingly, HIV infection is also likely a driver of early ageing, as AIDS patients age more rapidly than the general healthy population (He et al., 2019b; Lin et al., 2019). To address these problems, the diagnostic process in the aged population should be addressed more cautiously; therapeutic drugs and technologies suitable for the elderly patients should be developed. Special attention should also be paid to psychological problems of elderly patients. The HIV epidemic as a sexually transmitted disease will be discussed further below.
2.7.4. Influenza and pneumonia
Influenza is an acute viral infection caused by the influenza virus. At present, a total of four types of influenza viruses have been identified, including influenza A, B, C, and D (IAV, IBV, ICV and IDV) (Petrova and Russell, 2018). Among them, only IAV and IBV are able to cause seasonal epidemics and clinical disease. Yearly, the extent of the influenza pandemic varies around the world, which causes high morbidity and mortality. Because elderly individuals above 65 years of age are immunocompromised and may have preexisting conditions, they are more susceptible to influenza infection and its complications.
Data accumulated in the last decade showed that the morbidity of influenza has increased in both the general and aged populations (Fig. 3G). Like other acute infections, the mortality of influenza in aged patients was higher than in younger population (Fig. 3H). During January 1, 2018 to September 28, 2019, a total of 1626 severe influenza cases were reported in Hong Kong, among which 1058 patients (65.07 %) were over 65 years old (CHP, 2019b). In 2018, a total of 5984 influenza cases were reported in Macau, among which there were 188 cases were over 65 years (HBGM, 2019a). However, only a small number of influenza cases acquires laboratory confirmation, as patients usually die of other related illnesses brought on by influenza. Thus, the influenza-related mortality rate is greatly underestimated. In 2012, the CCDC estimated that the death rate caused by influenza was 18/100,000 in Northern China and 11.3/100,000 in Southern China, and most of the deaths occurred among people aged over 65 years (77.8 % in southern cities and 69.6 % in the northern) (Feng et al., 2012). The excess mortality of respiratory and circulatory diseases caused by influenza was 12.4/100,000 and 8.8/100,000, respectively, among which 86 % occurred in people aged over 65 years (Feng et al., 2012).
Pneumonia is an acute respiratory infection that affects the lungs, which is especially deadly in children under 5 years and in the elderly (65+). Pneumonia has become one of the major causes of death for the elderly over 65 years. The harm and mortality of pneumonia increases with age. The “2018 China Health Statistics Yearbook” reported that the mortality rate (/100,000) of urban residents aged 65–69, 70–74, 75–79, 80–84, and over 85 with pneumonia was 19.63, 34.48, 68.38, 219.07 and 865.53, respectively; and that of rural residents was 11.62, 23.67, 48.61, 127.90 and 445.93, respectively (NBSC, 2018). Since 2003, pneumonia has been one of the top three causes of death in Hong Kong (CHP, 2019a). According to statists by the Hong Kong Centre for Health Protection, the mortality rate of pneumonia was 39/100,000 in 2017, with a total of 8032 pneumonia-related deaths. Of these cases, 94.68 % occurred in people aged over 65 years (CHP, 2019c). In Macau, pneumonia also has been cited as one of the top three causes of death for many years (HBGM, 2019b).
In summary, old age is known to affect the immune system negatively. Immunocompromised elderly adults are more susceptible to common diseases such as influenza and pneumonia, both of which were responsible for many deaths in this age group. In some cases, these infections may lead to complications that then lead to death, and this likely contributes to under-reporting, hiding the true effects of influenza and pneumonia. There are multiple methods for improving and maintaining healthy immune function in the elderly: physical activity and exercise are known to enhance the immune system, however effective ranges still need to be established and disseminated (Venjatraman and Fernandes, 1997). Additionally, the development of vaccines must be prioritized, although challenges exist such as finding suitable mass production methods.
2.8. HIV, syphilis, and other sexually transmitted diseases (STDs)
Perhaps surprisingly, sexually transmitted diseases (STDs) are becoming an increasing problem among older age groups. Many people aged 50 years or older in China remain sexually active, and the shift towards nursing homes has led to an increase in exposure to possible sexual partners (Yang and Yan, 2016). Unfortunately, many older adults do not take precautions in their sex life, due to reasons such as a decreased worry about pregnancy (THT_UK, 2018). High-risk sexual behaviors render them vulnerable to the transmission of HIV and other sexually transmitted diseases (STDs), likewise low awareness of the potential risks and low use of sexual health services can result in late diagnosis and treatment of STDs among older adults. We here describe the current situation of HIV/AIDS and other STDs in older adults in China, and propose potential preventative measures.
As mentioned before the incidence and proportion of older adults in the total number of reported HIV/AIDS cases is on the rise in China (Fig. 3A-D). The rise in both the number of absolute cases and the proportion of STD infections was observed in both genders. The vast majority of cases in older adults resulted from heterosexual copulation, and has brought about an alarming increase in the rate of new infections. For example, in Chongqing, the proportion of HIV infections reported in those aged 50 years and older increased dramatically from 27 to 58.4 % between 2011 and 2019 (Chinanews, 2019) – at the same time, the overall number of male cases quadrupled, and the female cases tripled between 2012–2018 (Wu, 2019). Among women newly diagnosed with HIV in China between 2010–2016, the proportion of those aged 50 years and older increased from 17.8 % in 2010 (2 959/16 603) to 38.1 % in 2016 (9 981/26 196) (Chen et al., 2018). This proportion is even higher in regions with larger rural populations. In Guangxi, 46 % of newly reported HIV cases in 2014 were men aged 50+ (Hu et al., 2019a). In addition to the increase in newly reported infection among older adults, people infected with HIV can now survive to an older age, increasing the proportion of advanced-age HIV cases.
In addition to HIV other STDs are increasing in prevalence among the elderly in China. From 2000–2013, the incidence of syphilis in people over 60 years of age increased by over 30 %. The proportion of people aged 60 years and older among all syphilis cases was also on the rise, from 8.5 % in 2004 to 22.0 % in 2013 (Gong et al., 2014). Between 2008–2016, the incidence of condyloma acuminate in China showed a downward trend, with an average annual decline of 2.2 %. However, the incidence rate among people aged 50 and over increased by 4.8 % annually (Yue et al., 2017). Gonorrhea is not common in the elderly, and China saw an average annual decline of 7.9 % in the incidence of gonorrhea. This trend was also seen in older adults (4.5 %–10.9 %) (Gong et al., 2015). This phenomenon may be related to the short incubation period of gonorrhea, the high self-medication rate of patients, the sensitivity of gonococcal bacteria to antibiotics, and the insignificant clinical symptoms of female patients (Wang and Ni, 2008).
There are several contributing factors behind HIV/STDs transmission in older adults. Ageing is associated with various physiological changes in the human body collectively known as frailty. However, physiological changes in sexual function often fail to attract societal attention. Male sexual dysfunction and disorders often manifest in the slowing of penile erection, prolonged ejaculation, the dampening of sexual desire, impotence, etc. As women age, their vaginal tissue becomes thinner, drier, and less likely to become fertile. For the above reasons, the use of condoms in the elderly seems to be less important. Older women may have less interest in or need for sexual intercourse; however, their male counterparts may continue to be sexually active for a long period of time. Cravings for sex combined with loneliness may push men to resort to commercial sex to quench their desire for sex. In rural areas, the HIV prevalence is high among street-based female sex workers and female sex workers working at sex-on-premise venues with low quality of hygiene, such as hairdressing shops. Use of condoms and other precautions in these scenarios is likely to be lacking (Chen et al., 2017).
Sexual education in older adults is nearly absent, and it is generally assumed that “age is a condom”. Embarrassment may discourage older adults from obtaining condoms and other precautions. In a survey in Guangxi, although 87.9 % of respondents were willing to accept condoms issued free of charge by healthcare services, 64.1 % of the respondents were unwilling to take them of their own due to embarrassment (Qi and Pang, 2012). Despite the growing importance of sexual health among older adults, many of them do not seek health services for sexual problems. In China, data on sexual health in older adults are scarce. Existing research focuses mostly on males (Jiang, 2016). Few actions have been taken to accommodate older adults’ sexual health needs in China. Engaging older adults in health program development and policy changes is particularly challenging due to concurrent incidences of disability, frailty, and other comorbidities. Conventional top-down strategies are often unappealing and less trusted by the target audience. Innovative solutions are needed to develop contextualized sexual health services and ensure that they are inclusive, trusted, and reliable.
Collectively, HIV/STDs are becoming an increasing problem in the elderly in China due to diminished precautions in their sex life, a lack of condom usage, and insufficient sexual education, among other issues. Future research focuses should include a) routine sexual healthcare and screening for HIV/STDs among older adults, especially those who have high-risk sexual behaviors; b) Sexual health education and HIV/STDs prevention among older adults; c) Late diagnosis of HIV/STDs among older adults; and d) Healthcare providers’ attitude on the sexual health of older adults.
3. Responses to the challenges of ageing in China
3.1. Maintaining a vigorous lifestyle: free of tobacco, diet, exercise, and social activities
Modifiable health-related behaviors (HRBs) are key contributors to chronic diseases and early mortality, such that by maintaining a vigorous lifestyle, the processes of frailty, disability, and dementia can be postponed or even prevented (Lafortune et al., 2016; Rizzuto and Fratiglioni, 2014; WHO, 2019c). Similar public health recommendations for HRBs have been promoted worldwide, namely, refraining from smoking and excessive alcohol consumption, consuming a balanced diet, partaking in regular physical exercise, and maintaining frequent social engagements (WHO, 2015d). An international comparison study revealed a large degree of consistency in HRB clustering across six nationally-representative ageing cohorts in the East and West, alongside considerable gender- and country-specific variations (Liao et al., 2019b). Particularly, older Chinese males were characterized by a much higher probability of being smokers (57 %) than their counterparts in Japan (28 %), Korea (38 %), USA (17 %), UK (15 %), and in other European countries (21 %∼33 %) (Liao et al., 2019b). Comparable findings have been reported in the WHO’s 2019 Report on the Global Tobacco Epidemic, which further indicates that the progress of smoking reduction tends to be noticeably slower in China than the global average (WHO, 2019d). Nevertheless, positive developments of China’s concerted tobacco control efforts, such as smoke-free public places, a strengthened ban on tobacco advertising, etc., should be acknowledged (Li and Galea, 2019). These smoke-free movements have challenged and hope to gradually change social norms regarding smoking, though they may be less effective among older generations with poor health literacy (Hu et al., 2016).
The implementation of the Healthy China 2030 Action Plan provides an opportunity to increase tobacco control (Li and Galea, 2019), as well as to address a range of risk factors via a population-based multi-sectoral approach (NHCPRC, 2019a). Aiming to enhance the overall health of the Chinese population, the plan prioritizes 15 major actions, including the promotion of health literacy, the improvement of nutrition, a new national exercise campaign, more tobacco control measures, the promotion of mental health and environmental health; and specific actions dedicated to four target populations (i.e. women and children, teenagers, older adults, and those undertaking special occupations) and five categories of diseases, i.e. cardiovascular and cerebrovascular diseases, cancer, respiratory diseases (e.g. COPD), diabetes, and infectious diseases. Besides health-related targets for the health promotion actions for older adults, the importance of building an elderly-friendly and engaging environment is highlighted, which embodies “ageing in place” with humane, equitable and sustainable health and social care resources.
Social engagement is a key determinant of active ageing (World Health Organization, 2002), especially within China’s collective cultural background (Liao et al., 2019b, 2020). In tandem with physical exercise, social activities may generate health benefits not only for the body but also for the soul. Chinese square dancing is a social group-based exercise performed to music in public squares or parks. This low-cost and easy-participation activity is highly popular among middle-aged and retired Chinese women, estimated at 100 million participants in 2015 (Fang, 2015). Square dancers can meet as often as every day, usually in the early morning or evening after dinner, and sometimes both, upon meeting they organize themselves into rank and file, and exercise for nearly two hours, led by the most proficient dancer (Liao et al., 2019a). As an aerobic exercise accompanied by a dance rhythm, square dancing mobilizes the participants’ whole body, improving their balance and cardiopulmonary function (Liu and Guo, 2013). It is also cognitively challenging, requiring participants to listen to and process the music, focus on movement and balance, and dance to the rhythm with coordinated body movements (Kattenstroth et al., 2010). Moreover, square dancing creates a socially enriched environment for participants to interact with peers, keeping them socially engaged and dispelling loneliness (Liao et al., 2019a, 2020). Square dancing is a typical example of a grassroots group activity that may serve as inspiration for the design of culturally appropriate health promotion programs for older adults. One possibility is developing similar programs that can be implemented throughout the country, and possibly tailoring them to the local needs and/or cultures.
3.2. A community and homecare-dominated, public and private nursing home-supplemented system: notes on development, challenges, and opportunities
In the past five years, central and local governments in China have made enormous efforts in establishing a multi-dimensional geriatric care system to support healthy ageing in Chinese society. More than 30 national policies have been issued to drive the development of this care system, including cross-ministerial policy measures for promoting the growth of elderly services and the integrated development of medical, health and elderly care, through the Guiding Opinions on Advancing the Development of Age-Friendly Livable Environment (NDRC, 2016), and the State Council Opinions on Promoting the Development of Elderly Care Services (NHCPRC, 2019b, c). Following the strategies of the national 5-year plan, provincial and municipal governments have all issued local implementation plans. In places such as Shanghai, Shandong, Jiangsu, Zhejiang and Guangdong, political will has been accompanied by strong financial support (CNCA, 2020).
As compared to Q3 2014, in Q3 2019 there was an additional 2.4 million beds added in public and private nursing homes across China, resulting in a total national supply of 7.55 million beds (MCAPRC, 2019a, b). In 2018, the Ministry of Civil Affairs allocated RMB 2.9 billion (USD 400 million) to support the local expansion of care beds in nursing homes as well as the development of community and home care services. In terms of service utilization, the occupancy rate of nursing home beds is at around 50 %, i.e. at any time, there are less than 3.8 million residents in these facilities. 748,000 elderly benefited from nursing care subsidies while 5.22 million benefited from social care subsidies (MCAPRC, 2019a, b). In July 2016, the first national pilot of a long-term care insurance (LTCI) program was announced in 15 cities across different regions of China (MHRSSPRC, 2016). Identification of elderly people with severe care dependency was carried out, and local models of financing care for them in nursing homes, community centers as well as at home were implemented. By June 2019 this pilot program covered a total of 88.54 million people, funding services for 426,000 beneficiaries at RMB 9200 per year per person (NHSAPRC, 2019). While geriatric care system development has attracted strong attention from stakeholders and become a major theme for policy, research and investment, the following challenges need to be understood and addressed before meaningful progress can be made to prepare the country for its rapid entrance into an ageing society.
The first challenge is that care needs must be assessed comprehensively and should be subject to regular reassessment in order to develop personalized care plans and identify goals that are aligned among care recipients, providers and payers (WHO, 2017). Generally, there are currently two types of assessments in use in China: one conducted before admission into nursing homes, the other for entry into the LTCI programs. The first type can be quite comprehensive but is often used to decide the charge levels associated with the care service. The second type uses a simple 6-item ADL questionnaire and links its results to the funding schemes, e.g. maximum hours of care per month. As the assessment of care needs tends to be one-off and disconnected to care plans or goals (Hua, 2019; Ma, 2017), it is difficult to allocate resources dynamically and to analyze care performance or economics. The second challenge involves problems with service capacity. On the one hand, 45 % of nursing home beds are left unoccupied and, contrary to international best practice, for the beds that are occupied, only less than 20 % are actually utilized by people with severe dependency; on the other hand, according to the National Health Commission, nearly 188 million seniors have chronic diseases, and 40 million have various levels of disabilities (NHCPRC, 2019b, c). Among the over 40 million people with different degrees of care dependency and care needs, under 10 % have been served by community and home, and the majority have yet to be cared for (MCAPRC, 2019a, b). Some policies have been put in place to attempt to fill the huge gap in caregivers, stating that 10 million more caregivers are needed just to care for the existing group of dependent seniors. However, if the current mainstream model of “replacive care” is not changed, growing care service capacity will only lead to an accelerated rate of care dependency among the high-risk population. Additionally, such a model of care is highly unattractive to potential workforce candidates. As a corrective move, the central government has now set a goal to train 2 million more caregivers by 2022 (MCAPRC, 2019a, b).
The third challenge is distorted allocation of resources. Up until the end of 2018, despite plans to establish a home care-dominant, community-backed and nursing home-supplemented system, investment has remained predominantly in heavy assets, i.e. the development of nursing homes as well as senior-living property projects, resulting in the above-mentioned “oversupply” of care beds (Qiao, 2019). Since the 13th Five-Year Plan, the central government has committed to an annual funding of RMB 1 billion to support innovative pilots of home- or community-based care models (MCAPRC, 2017-2019). However, for many local governments, the first and foremost priority when developing local care capacity is to specify land for elderly care use and invest in care facilities construction before or while looking for operators of such facilities. In addition to resistance and reluctance from nursing homes and preexisting policymakers, difficulty in understanding senior population’s care needs and evaluating care competency among community and home care providers have prevented financial support schemes from materializing in most parts of China. Typical examples of the insufficient support for community and home care service development can be seen in the number of government purchase tenders that fell through without enough qualified bidders.
While there is no lack of political will and resources to be invested in further developing the care system, there is an urgent need to pay for access and quality. A value-based resource allocation model focusing on improving population health rather than the current fee-for-service care model would provide China a rare opportunity to benefit from a healthily ageing society (Gyurmey and Kwiatkowski, 2019; Mandal et al., 2017).
To address the above-mentioned challenges and seize the opportunity associated with them, pilots should be designed based on local evidence and should be established in four dimensions. Firstly, development of care plans should be focused on individually centered goal based on comprehensive assessments. As highlighted in the latest WHO ICOPE (Integrated Care for Older Persons) package, it is essential for countries and health systems to align the efforts of different stakeholders with a shared care plan that is customized to serve the individuals’ priorities and goals. Secondly, health and social care resources should be integrated to support the realization of personalized goals of care and, at the population level, to delay and reduce care dependency. Rather than further developing passive care capacity to compensate for the increasing need for other fragmented services, devoting resources to the reaching of a consensus among care providers and receivers will serve to empower the population itself, and maximize the pooling of financial and human resources, decreasing the need for an expansion of passive services (WHO, 2019b). Thirdly, the education and training of “integrated care managers” should be developed, whose job would be to work actively in primary care settings to identify care needs and coordinate care resources crucial to achieving societal and individual care goals. Mobilizing talents with various backgrounds to understand and operate under the comprehensiveness of geriatric health needs, developing their capability to better communicate and coordinate care efforts across public and private sectors would not only facility the integration of various care services, but make the care work more attractive for those seeking long-term career opportunities (Wang and Song, 2019). Fourthly, a reform of the payment model used in elderly care services should be carried out, focusing on value rather than volume of care for populations at risk of care dependency. Healthcare payments have long been moving from an inefficient, fragmented, fee-for-service model to a value-based capitation or bundled payment model. For geriatric care financing, this reform is likely to develop faster than the reform of payments for healthcare services. Setting sustainable goals for care and allocating resources accordingly will be a viable realistic solution to caring for the millions of Chinese citizens in need (Chen et al., 2019a).
We recognize the complexity of establishing such a health-oriented care system. For the four dimensions of an integrated care system to be aligned around common goals as discussed above, a pre-requisite should be the interconnectivity of data: linking results across personal health records, assessments of geriatric care needs, and total costs of care, including: social and commercial health insurance payment, out-of-pocket private payment, social welfare payment, as well as other sources of funding for elderly care (Threapleton et al., 2017).
3.3. Palliative care for the elderly in China
Palliative care is emerging as a new alternative for hospitalized elderly with life-threatening illness. The WHO defines palliative care as the prevention and relief of suffering of adult and pediatric patients and their families facing the problems associated with life-threatening illness (including malignant and non-malignant diseases). These problems include physical, psychological, social and spiritual suffering of both patients and their family members The aim of palliative care is to enhance the quality of life, promote dignity and comfort, and may also positively influence the course of illness (WHO, 2016a). Palliative care is the basic skill of medical staff in departments where medical care is provided to end-stage patients (e.g. ICUs, emergency rooms, geriatric and oncology departments) (Ning, 2018). The 2015 quality of death index survey showed that the death quality of mainland China ranked 71st out of 80 countries, while Taiwan and Hong Kong ranked 6th and 22nd, respectively (EIU, 2015). While palliative care is widely available in Western countries, it is limited in mainland China. According to a report in 2016, only 0.7 % (146/22,000) of hospitals offered palliative care services. In China, the proportion of course in palliative medicine at medical schools is relatively low and, often only available as electives for undergraduates or postgraduates (Liu and Yuan, 2009). Questionnaire data of 5th year medical students in 2017 and of geriatric nurses in 2016, showed that 58.7 % of medical students and 55.7 % of nurses had no training or education regarding death or terminal care, and 93 % of medical students and 94.3 % of nurses had not received any education about hospice and palliative care. Thus the need for course education in hospice and palliative care at Chinese medical schools is extremely urgent.
Palliative care is recommended to be introduced early in curative treatments when patients are diagnosed with a life-limiting disease or when the palliative care needs of patients are identified. Current palliative care in mainland China is still mainly focused on patients with cancer, with only a few palliative care resources available for other chronic conditions such as COPD, HIV and renal failure (Liu et al., 2019). Therefore, in the future, palliative care should be extended to both patients with cancer, with other life-limiting diseases, and their families.
Many palliative care guidelines have emphasized that the discussion of advanced decision-making among patients and their families should be initiated when patients still possess decision-making capacity (Cheng, 2018). Patients in Mainland China sometimes fail to grasp or accept the truth of a diagnosis and limited survival time (Cheng, 2018). Moreover, according to questionnaire reports from 1084 patients in 2016, awareness of the concept of advance care planning or advance directives in China is still low (Kang et al., 2017). In Mainland China, family members are often held responsible for making decisions for the elderly in their care, despite a lack of knowledge or training, and thus may resort to homeopathic remedies. Healthcare professionals generally have to “respect’’ any decision made by the families and try their best to “save’’ patients’ lives using many life-sustaining treatments, although they generally hold negative attitudes to useless treatments. Such an approach is regarded as an appropriate measure in terms of protecting themselves from medical conflicts. Misunderstanding of palliative care as ‘giving up on treatment and waiting for the death of the patients’ by family members of the patients as well as even by some doctors, should be corrected (Hu et al., 2019b; Ning, 2018; Xiao et al., 2019).
There is an urgent need for the development of hospice and palliative care in China. In recent years, hospice and palliative care have witnessed rapid development. More and more patients, families, and health-care professionals come into contact with the concept and realize the benefit of hospice and palliative care, while more and more educators, organizations, government and other intermediary leaders have paid more attention to the promotion and development of hospice and palliative care.
3.4. The importance of the national clinical research center for geriatric disorders
The current trend towards an ageing society poses difficulties due to the additional challenges seen in diseases in the elderly, including longer disease durations, more complications, underwhelming responses to treatment, and poor prognosis, thus in response to this trend, China has established the National Clinical Research Center for Geriatric Disorders (NCRCGD) (O’Meara, 2020; Yu et al., 2018a). Funded by the central government, the NCRCGD aims to provide innovative models for the diagnosis, management and further research into geriatric diseases at a national level. The NCRCGD focuses mainly on comprehensive and systematic research into pathogenesis, prevention, diagnosis and treatment of age-related diseases such as AD, PD, and cerebrovascular disease (XWHOSP, 2017b, 2019). At the same time, it is committed to building a national elderly medical service network and scientific innovation system by integrating resources of clinical and basic research. For instance, a health data management platform for the elderly could provide a scientific basis for management and decision making. Furthermore, through the education and promotion of new theories and technologies of geriatrics to grassroots hospitals, the NCRCGD can build a better medical service system, improving the health of elderly people. The NCRCGD strives to promote the combination of academic and clinical research (XWHOSP, 2017b, 2019). Research on age-related diseases has been carried on such various aspects as diagnosis, treatment, and prevention in fields such as immunology and molecular biology (O’Meara, 2020). The characterization of the gene pool, a series of research findings and new technologies have been applied at the clinic, which promotes the development of gerontology in the direction of precision medicine for early diagnosis, early prevention, and early treatment. The NCRCGD also serves as an educational harbor to foster the training of geriatricians and promote academic exchange (Frailty-China, 2019; XWHOSP, 2017b, 2019). The organization also undertakes other social responsibilities, including partnerships with hundreds of institutions across the country, relying on their collaborative research network to successfully carry out a comprehensive assessment of multiple systems for the elderly (XWHOSP, 2017a). Through a comprehensive assessment of the multiple aspects of the elderly's diseases, fitness, cognition, psychology and society, it may be possible to develop a system for early identification of health imbalances in the elderly that characterize certain diseases, aiding in their early prevention, and helping to reduce the burden of the ageing Chinese society, as well as improving the elderly health service system. Prospectively, the NCRCGD will also play its essential role in guiding the research and clinical guidelines for elderly people care as well as making more contributions to improve elderly people's quality of life in China.
3.5. Towards pharmacological interventions for ageing
In order to deal with the ongoing boom in the elderly population, the Chinese government has put more effort into funding research on ageing and its related diseases in recent decades. During the recent (2019) outbreak of coronavirus in China, older patients with pre-existing ageing-related diseases were found to have a much higher casualty rates than younger patients (Chen N et al., 2019), again highlighting the importance of preventing ageing-related diseases. In response to this, along with the growing need for improving the quality of life of the elderly in China, more attention has been placed on the development of pharmacological strategies against ageing, organ degeneration and major ageing-related diseases. In this section, we will discuss recent world-wide progress in pharmacological attempts to improve healthspan, and the significant contributions that Chinese researchers have made.
3.5.1. Targeting classic longevity pathways
Calorie restriction (CR) was first demonstrated as an effective way to extend lifespan in rodents (de Cabo and Mattson, 2019d), however the physiological mechanisms behind its anti-ageing effectiveness were not fully understood at the time, and remain uncertain. Later studies have suggested that CR might extend lifespan by regulating insulin-like growth factor (IGF) and mammalian target of rapamycin (mTOR) pathways. Metformin is primarily known for treating type 2 diabetes, with its underlying molecular mechanisms leading to the to down-regulation of IGF-1 signaling, and the inhibition of cellular proliferation, mitochondrial biogenesis, ROS production, DNA damage, activity of the mTOR pathway, etc. (Barzilai et al., 2016). The anti-ageing effect of metformin is under investigation by the TAME (Targeting Ageing with Metformin) trial in the USA. Acarbose, an antidiabetic drug, could also disrupt the IGF pathway. Acarbose has been shown to partially mimic the effects of CR and extend lifespan in mice by controlling blood sugar and slowing carbohydrate digestion (Harrison et al., 2019). A clinical trial on acarbose (ClinicalTrials.gov Identifier: NCT02953093), named Study of Acarbose in Longevity (SAIL), is in phase 2, and will hopefully shed some light on its pro-longevity effect in humans. mTOR is a pivotal nutrition sensor that links cellular metabolism with proliferation, growth and survival by regulating amino acid metabolism, proteostasis, mitochondria dynamics, cellular senescence, etc. (Liu and Sabatini, 2020). Rapamycin, a well-known inhibitor of mTOR, has shown life-extending effects in all model organisms and postpones the onset of age-associated diseases (Fang et al., 2016; Harrison et al., 2009; Liu and Sabatini, 2020). Despite the promising pro-longevity outcome of using rapamycin in animals, its clinical application in human has been obstructed by growing concern of potential side effects from immunosuppression and hyperglycemia (Pallet and Legendre, 2013). Whether the dosage can be fine-tuned to avoid these side effects will be the determining factor in whether or not rapamycin becomes a future pro-longevity drug. The application of induced pluripotent stem cells (iPSCs) from healthy and pathological ageing individuals (Liu et al., 2011) is also propelling further mechanistic studies and translational applications for CR.
3.5.2. NAD+ boosters
Nicotinamide adenine dinucleotide (NAD+) is a fundamental molecule in human life and health; while there is an age-dependent reduction of NAD+, NAD+ augmentation extends lifespan and improves healthspan in different animal models as well as shows potential to treat different neurodegenerative diseases based on phase I clinical trials (Gilmour et al., 2020; Lautrup et al., 2019; Yoshino et al., 2018). NAD+ precursors such as nicotinamide riboside (NR) and nicotinamide mononucleotide (NMN) have emerged as promising approaches for intervention against ageing phenotypes and age-related diseases. Supplementation via these precursors can elevate NAD+ level in vivo and improve glucose metabolism, mitochondria biogenesis, DNA repair, neovascularization and neuroprotection (Lautrup et al., 2019). Additionally, more than five phase I clinical trials indicate that orally taking NR is well tolerated and able to elevate NAD+ in the blood (Gilmour et al., 2020; Lautrup et al., 2019). Several clinical trials are currently operating in parallel, investigating NR’s effects on metabolic function in bones (NCT03818802), in immunity (NCT02812238), and NMN’s effect in cardiometabolic function (NCT03151239), with others also ongoing. In China, although NAD+ precursors have become widely available commercially as supplements, clinical trials exploring their disease-treating ability in humans are still lacking.
3.5.3. Senolytics
Senescent cells accumulate in aged tissues and this accumulation is considered one of the driving forces of ageing. Senolytics are a class of molecules specifically designed to induce apoptosis of these senescent cells. Clearing senescent cells in mice has been shown to substantially alleviate ageing phenotypes, producing potent therapeutic effects in ageing-related diseases such as AD (Bussian et al., 2018; Zhang et al., 2019b), atherosclerosis (Childs et al., 2016) and osteoarthritis (Jeon et al., 2017). In 2016, a joint research team of Chinese and American researchers found that the molecule ABT263 reduced irradiation-induced senescent bone marrow hematopoietic stem cells (HSCs) and muscle stem cells (MuSCs) in mice (Zhang et al.,2016). ABT263 (a Bcl-2 family inhibitor), together with dasatinib (an anticancer drug) and quercetin (an apoptosis inducer) are the most commonly used senolytic drugs. The senolytic cocktail of dasatinib plus quercetin (DQ) decreased naturally occurring senescent cells, improved mobility and reduced the risk of mortality (Xu et al., 2018). However, a small pilot clinical study using the same DQ cocktail in patients with idiopathic pulmonary fibrosis (IPF) reported no change in pulmonary function, frailty index, clinical chemistries and reported health, though the beneficial effects on mobility were still noted (Justice et al., 2019). While clinical trials on senolytic drugs are mainly conducted in the USA, the concept of reducing senescent cells to delay the ageing progress has attracted interest from all over the world. Since 2016, the National Natural Science Foundation of China (NSFC) has set up special programs, providing millions of RMB to support research on cellular senescence and organ degeneration. As such, it is recommended that China further expand its investment in senolytics research.
Targeting the microbiota may also improve age-related diseases, including AD. In 2019, China approved the first domestically invented AD drug, oligomannate (GV-971) (Wang et al., 2019d). Considering there has been no new approved anti-AD drugs in the past 17 years, this has been exciting news. Despite the potential of these advances, more work is necessary to understand how GV-971 works. Additionally, due to the relatively short clinical trial period, further investigation with longer lasting trials is highly recommended.
Most human trials for potential anti-ageing drug candidates are conducted in patients with certain age-related diseases. Despite partial overlap of the pathologies of these diseases, the knowledge from these trials cannot be interpreted as treating ageing itself. Therefore, to reach the goal of identifying anti-ageing compounds, a more comprehensive study on disease-free, healthily ageing groups with no obvious health issues is in immediate need. China has the advantage of a large and diverse population, providing an ideal subject pool for this type of study. The knowledge gained from such studies would likely open new avenues to better understand the fundamental aspects of ageing mechanisms, facilitating their treatment.
3.6. Examples from the Hong Kong SAR
From a public health and policy perspective, it can be seen that continuing research into prevention and management strategies will be important for both non-communicable diseases as well as geriatric syndromes, to ensure that it is not only life expectancy that is increased, but also the quality of life, by promoting independence and reducing reliance on elderly care services. Regular monitoring of trends in incidence and case fatalities of common chronic diseases would enable estimates of future disease burdens and guide preventive health policies (Chau et al., 2013a, b). In addition, solutions to trends in the occurrence of disability and frailty are also needed (Yu et al., 2018b). Such data would inform the design of elder-friendly service delivery models across the whole spectrum, from prevention to primary care, hospital and residential care settings (Woo et al., 2013; Yu et al., 2019). Currently, Hong Kong, a Special Administrative Region (SAR) of China, has the longest life expectancies in the world for both men and women, such that the need to redesign service models is particularly pressing. By 2064, it is predicted that 33 % of the population in Hong Kong will be aged 65 years and over; 70 % will have at least one chronic condition, with an increasing prevalence of disability also predicted (Yeoh and Lai, 2016). While the health and social care systems are well developed, there is a mismatch of needs as those with chronic conditions are predominantly managed in the public hospital systems, whereas primary care is predominantly in the private sector. A recent review concluded that better integration of health and social care systems with a primary emphasis on the community could be the best way forward for the ageing population in Hong Kong (Threapleton et al., 2017), exemplified by the formation of nurse-led District Health Centers in 2019 (FHB, 2019). Other community models with an emphasis on promoting group activities to prevent frailty and aid self-management of chronic diseases have also been developed (Cadenza, 2020). Such developments have the potential to enhance the role of primary healthcare professionals in preventing functional decline (Morley et al., 2017), so that many can retain independence even as life expectancy increases. The WHO’s Integrated Care for Older People (ICOPE), formally launched in October 2019, will form a useful blueprint for policymakers to build on their existing health and social care infrastructure (WHO, 2015c).
3.7. A comparison of elderly healthcare between China and the EU
Experiences of elderly healthcare in the European Union (EU) may provide useful tips for the situation in China (Table 1 ). In the EU, elderly care is provided in each country based on its own social security system and cultural norms. In most European countries, the family and the state are the main providers of support to older people both in activities of daily living (ADL) and in instrumental activities of daily living (IADL) (Schmid et al., 2012). Europe is characterized by three types of care provision: 1) ‘crowding out’, whereby the state largely replaces family care; 2) ‘crowding in’, whereby the state promotes family care; 3) ‘mixed responsibility’, whereby both the state and the family take a joint responsibility for care, yet have separate functions (Brandt et al., 2009). In China, family is still the traditional provider for elderly care (Wu et al., 2016a). Under current national and social developmental conditions of China, the Chinese government encourages a ‘90/7/3′ pattern of eldercare system, namely: 90 % of all older people are cared for at home, 7% are cared for in communities, and 3% are cared for in institutions (Mayston et al., 2017).
Table 1.
Macro-level indicators on active ageing for the elderly (65+ years) by countries.
| Country | Population 65+ % of total population (2018)c | Old-age dependency ratio (2015)d | Pension spending % of GDP (2015)e | Health expenditure % of GDP (2017) |
|---|---|---|---|---|
| OECD membersa,c | ||||
| Australia | 15.7 | 25.0 | 4.3 | 9.2 |
| Austria | 19.0 | 30.5 | 13.3 | 10.4 |
| Belgium | 18.8 | 30.6 | 10.7 | 10.3 |
| Canada | 17.2 | 26.1 | 4.7 | 10.7 |
| Czech Republic | 19.4 | 28.8 | 8.1 | 7.2 |
| Denmark | 19.8 | 33.0 | 8.1 | 10.1 |
| Estonia | 19.6 | 31.0 | 7.0 | 6.4 |
| Finland | 21.7 | 35.0 | 11.4 | 9.2 |
| France | 20.0 | 33.3 | 13.9 | 11.3 |
| Germany | 21.5 | 34.8 | 10.1 | 11.2 |
| Greece | 21.7 | 33.0 | 16.9 | 8.0 |
| Hungary | 19.2 | 27.9 | 9.2 | 6.9 |
| Iceland | 14.8 | 23.1 | 2.1 | 8.3 |
| Ireland | 13.9 | 22.3 | 3.6 | 7.2 |
| Italy | 22.8 | 37.8 | 16.2 | 8.8 |
| Japan | 27.6 | 46.2 | 9.4 | 10.9 |
| Latvia | 20.0 | 31.5 | 7.0 | 6.0 |
| Lithuania | 19.7 | na | 6.7 | 6.5 |
| Luxembourg | 14.2 | 22.0 | 8.4 | 5.5 |
| Netherlands | 19.2 | 30.2 | 5.4 | 10.1 |
| Norway | 17.0 | 27.4 | 6.6 | 10.4 |
| Poland | 17.5 | 24.3 | na | 6.5 |
| Portugal | 22.0 | 34.6 | 13.3 | 9.0 |
| Slovak Republic | 15.6 | 21.5 | 7.3 | 6.7 |
| Slovenia | 19.6 | 28.8 | 11.1 | 8.2 |
| Spain | 19.4 | 30.6 | 11.0 | 8.9 |
| Sweden | 20.1 | 33.8 | 7.2 | 11.0 |
| Switzerland | 18.6 | 29.0 | 6.5 | 12.3 |
| United Kingdom | 18.4 | 31.0 | 6.2 | 9.6 |
| United States | 15.8 | 24.6 | 7.1 | 17.1 |
| Chinab,c | 10.9 | 14.3 | na | 6.4 |
Sources: a: OECD database; b: China National Bureau of Statistics; c: World Bank database. Notes: d: The old-age dependency ratio is defined as the ratio between people aged 65 and over and the working age population between 20 and 64; e: Pension spending is defined as all cash expenditures (including lump-sum payments) on old-age and survivors’ pensions.
A ‘crowd out’ system dominates in the Nordic countries (Denmark, Finland, Norway, Sweden, Iceland), where the government strives to create a comprehensive system of care services in order to reduce the care obligation of the family. In continental European countries such as Austria, Belgium, France, Germany and the Netherlands, systems are more mixed in their provision of elderly care, though tend towards a ‘crowd out’ approach (Kasearu and Kutsar, 2013). In the island countries, i.e. the UK and Ireland, the system is more mixed, and the private market is the dominant welfare provider, with the government providing two main social care services to older people, one being old age pensions and the other being healthcare (Wu et al., 2014). Southern European countries (e.g. Greece, Italy, Portugal, Spain) have a ‘crowd in’ system whereby families have more responsibilities for care services to older people (Kasearu and Kutsar, 2013; Wu et al., 2014). Eastern European countries have undergone dramatic political, social and economic changes after the Soviet era and experienced a rapid change from ‘crowd out’ to a ‘crowd in’ system where family is the main care provider and the government provides basic formal care services (Kasearu and Kutsar, 2013; Wu et al., 2014). In China, owing to Confucian culture and its emphasis on the family, it is taken for granted that the family, most notably adult children, has the responsibility to care for older parents, especially in the rural areas of China, thus older people rely mainly on their children or family for support (Chen and Silverstein, 2000; Wu et al., 2016a).
Rapid demographic ageing increases the demand for care in all ageing societies. Currently, European countries face the enormous challenge of implementing major reforms to elderly care in order to ensure that the needs of older people can be continuously met in the future (Brandt et al., 2009; Broese van Groenou and De Boer, 2016). To this end, European governments have increasingly relied on informal care in addition to regular and traditional formal care providers from professional home care services, day care units and nursing homes (Broese van Groenou and De Boer, 2016; Verbakel et al., 2017). Informal care for older people is generally provided by caregivers from both kin and non-kin groups, including spouses, children, relatives, neighbors, friends, etc. (Swinkels et al., 2016). In Europe, around a third of people aged 50 years or older provide informal care to older people. However, shrinking family sizes, the increasing participation of females in the workplace, and rising retirement ages, may pose a drastic challenge to informal care in the future (Verbakel et al., 2017). China is currently facing challenges in its family-based elderly care model due to new family formation, the spread of individualistic values, and frequent internal migration from rural to urban areas encouraged by rapid economic development (Wu et al., 2018a). Moreover, China’s one-child policy (1979–2015) has sped up the process of population ageing by accelerating the change of the fertility rate and, in turn, has weakened the family-based elderly care model in China (Fang et al., 2015).
In Europe, new elderly care arrangements have been gradually developing based on a new combination of family obligations, market provision and public support. In Nordic countries, the state, family and market have been changing with regards to their roles in the provision of elderly care, specifically by increasing the provision of publicly funded care services in a for-profit capacity (marketization of elderly care) and increasing the importance of family care (Szebehely and Meagher, 2018). In Estonia, the idea of community-based support for older people has been increasingly set forth in order to postpone the need for institutional eldercare (Tulva et al., 2016) (Tulva et al., 2017). When it comes to the current trend of eldercare in China, marketization has also been discussed to a large extent both at academic and policy levels. The ‘public-private-partnership’ (PPP) model may improve the efficiency of family-based eldercare. In the 13th Five-Year Plan for National Economic and Social Development (2016–2020), the opening-up of the market for elderly care services (e.g. purchase of services by the government) was clearly stated (Du and Wang, 2016). Elderly care reforms might create new challenges for both Europe and China, an important challenge being an increase in inequality in eldercare service utilization among different social groups of older people. Older people with higher socioeconomic status will be able purchase private care services whereas those with less social capital will have to rely on more family-based care. In addition, for the Chinese government, there is a need to take into account larger inequalities derived from immense resource variations across regions during the development and reform of elderly care services. While mainland China can learn many successful experiences from Hong Kong, the EU, etc., there remains many unique features that demand the creation of an elderly care system tailored to mainland China.
In addition to responding to changes and preparing to adapt to an ageing society at the societal and individual levels, understanding of the mystery of ageing at a molecular level will aid the development of novel strategies to slow ageing and to promote healthy longevity. In the below sub-sections, we will focus on how to use centenarians, the China National GeneBank DataBase (CNGBdb), and AI to further propel ageing research.
3.8. Studies in Chinese centenarians
In China, the numbers of the oldest-old individuals (those aged 80+), near-centenarians (95+), and centenarians are increasing at roughly 10 % yearly (Fig. 4 A-B), providing unique resources for both basic research and clinical studies. There were 3384 centenarians in 1953, with the number rising to 35,934 by 2010 (Abida and Gu, 2008). Based on the UN’s medium variant projection, by 2050 over a quarter of the global oldest-old population will live in China.
Fig. 4.
Yearly increase of the Chinese centenarians as well as gender, regional, and geographical differences. A-B. Changes of the numbers of centenarians in China over time. By 2017, the population of near-centenarians (those aged 95+, A) and centenarians (B), increased nearly 10 % per year. The data exacted from the Population Sample Survey (2003-2009, 2011-2017), the 6th Population Census of China (2010) and projection (2020-2050) of China's National Bureau of Statistics. C. Women account for 75 % of the total number of centenarians in China and the proportion of rural centenarians is far higher than that of urban area. Data source: China's 2010 population census, excluding Hong Kong, Macau and Taiwan area. The map was made by R. D. Geographical distribution of the relative number of centenarians. The proportion of centenarians in China's total population (centenarian ratio) has a significant regional imbalance. Data, China's 2010 population census, excluding Hong Kong, Macau and Taiwan area.
As the numbers of the most elderly have expanded, the gender structure of centenarians, the proportion from urban and rural areas, and differences in geographical distribution have formed "three-high" trends in China (Data from China's 2010 population census, excluding Hong Kong, Macau and Taiwan). First, there is a gender difference, with 75 % of centenarians being female (Peng, 2011) (Fig. 4A). Data from the 6th Population Census of China (2010) reported 27,082 (75.37 %) female and 8852 (24.63 %) male centenarians. This could be due to both physiological (e.g., female hormone estrogen) and cultural differences (women often do more housework, pay more attention to healthcare) (Austad and Fischer, 2016; Peng, 2011). Second, urban and rural disparities were clear, wherein more centenarians (56 %) live in rural areas, possibly due to a healthier living environment, diet and lifestyle in these regions (Cai, 2013; Peng, 2011; Zeng et al., 2017a) (Fig. 4C). And third, there was geographical difference in the distribution of centenarians. The distribution of longevity areas in China presents several significant characteristics, including province-specific: being majorly in Hainan, Guangxi, Sichuan, Yunnan, Guangdong and Xinjiang, and mostly distributed along river basins, with more centenarians along the Pearl and Yangtze rivers and the Lancang river basins. These characteristics of the area distribution of centenarian suggest that areas beneficial to longevity can be divided into two types: ‘natural’ and ‘economically developed’ longevity areas (He et al., 2017; Zeng et al., 2017a) (Fig. 4D).
Studies of centenarians can provide valuable information for early prevention of major diseases, premature ageing, and early death, thus providing the scientific support necessary to cope with the quickly approaching arrival of an ageing society in China. Centenarians may represent a prototype of successful ageing. A longitudinal study of a Danish 1905 cohort suggests exceptional longevity does not result in excessive levels of disability (Christensen et al., 2008). In fact, some centenarians experience a delayed onset of age-related illnesses (delayers), whereas others did not succumb to any age-related illnesses (escapers) (Christensen et al., 2008; Hitt et al., 1999). In addition, one case-control study showed that older individuals had a delayed age of onset of cancer, cardiovascular disease, diabetes mellitus, hypertension and osteoporosis than their respective younger reference groups (Ismail et al., 2016). The China Hainan Centenarian Cohort Study (CHCCS) on 1002 centenarians is now in progress, focusing primarily on examining biological indicators and medical aspects, and extensively examining psychological and sociological factors (He et al., 2017). All in all, the study of centenarians is a topic of immense importance for population and health policymakers, as well as for the larger aim to achieve long, healthy lives.
3.9. The China National GeneBank DataBase (CNGBdb) as a foundation for the progression of gerontology research in China
State-of-the-art technologies enable the ‘Big Data’-based investigation of the molecular mechanisms of human ageing and its associated diseases, providing unique information for therapies and interventions. The CNGBdb is a centralized ‘Big Data’ hub of biological data, providing data sharing, knowledge search, computational analysis, management authorization, and visualization services to the global research community. Built and maintained by the China National GeneBank (CNGB), CNGBdb draws from 3 “banks”: the Living Biobank, the Biorepository, and the Bioinformatics Center, and from 2 “platforms”: the Digitization Platform and the Synthesis and Editing Platform. The research data system of CNGBdb integrates molecular data from internal and external sources into nine sub-databases including Literature, Gene, Variation, Protein, Sequence, Project, Sample, Experiment, and Assembly (https://db.cngb.org/news/2/).
Comparative analyses of species and tissues can identify the molecular causes of ageing phenotypes, corroborate or disprove theories on ageing, and help to understand differences in the mechanisms of ageing across species. Genotype comparisons within a species at the level of individuals and populations can help identify genetic reason for differences in lifespan. This approach may be used to compare populations from different regions of China, or Chinese and foreign populations, such as Ashkenazi Jews and Okinawan centenarians in Japan, two populations well-known for their longevity, facilitating the discovery of Chinese-specific age-modifying genes. The identification of potential life-extending genes eases the design of therapeutics that can mimic the effect of these genes in people without those genes. Likewise, treatments can be designed for age-related diseases that result from mutated or nonfunctional genes in specific populations. It is also possible to comparatively analyze gene expression at the tissue level, as tissues age at different speeds. Since many age-related diseases, such as AD, occur within a specific tissue, understanding the speed at which tissues age can help Chinese gerontologists assess the risk of and help to prevent tissue-specific age-related diseases (Wieser et al., 2011).
3.10. Artificial intelligence in geriatric care
The advent of ‘Big Data’ and machine learning have eased the collection and identification of biomarkers associated with biological age and may allow for the development of personalized clinical diagnostic tools for physicians in the near future (Aman et al., 2019). In the field of medicine, biomarkers refer to measurable indices capable of identifying a condition, state of being, disease, or environmental marker whose presence may reflect a pathophysiological state (Naylor, 2003). The use of biomarkers has been applied to the field of anti-ageing technologies, including the prevention and treatment of age-related disease, and has been used to explore methods to delay or offset the ageing process altogether, and will likely serve as key components to advances in the field (Campisi et al., 2019). In some cases biomarkers may more accurately represent a patient’s ‘biological age’, as opposed to a patient's simple ‘chronological age’, the former of which is thought to be more clinically relevant (Lopez-Otin et al., 2013). The following sections will review three applications of biomarkers at the molecular, individual and societal levels, including current findings as well as potential research directions.
3.10.1. Biomarkers at the molecular level
As stated above, there are multiple tests that can be used to obtain molecular biomarkers, and several have been validated to some degree by current research. Molecular biomarker studies can be roughly separated into 2 classes: smaller scale studies attempting to determine the utility of a given biomarker, and machine learning studies involving thousands of samples with the intention of developing clinical assessment tools. As an example of this, a recent study involving elderly hypertensive patients was used to investigate a wide library of potentially useful biomarkers. Here, 416 elderly Chinese participants were matched with subjects from a pool of 9000 normal volunteers. After adjusting for confounding covariate factors, the researchers found that only elevated triglyceride levels were strongly linked to high blood pressure (Hong et al., 2017).
While these cross-sectional studies are certainly important for determining which biomarkers should be considered for clinical evaluation, one of the limitations, at least in comparison to machine learning studies, is that they have a low number of samples. In the above examples, most participant groups contained less than 500 people. While this is a surplus number in other medical contexts, one of the advantages of machine learning is its ability to process thousands of samples granting increased accuracy. Fittingly, one of its primary uses is to draw meaningful conclusions from mass, simple, cheap, and non-invasive tests. Another key limitation is that biomarker assessment studies using these ‘smaller’ cohorts tend to lack any external validation. Perhaps one of the most easily accessible tests that comes to mind is a standard blood test, here the usefulness of machine learning has been demonstrated by Putin and colleagues, who designed a modular ensemble of 21 deep neural networks (DNNs) of varying depth, structure and optimization for the prediction of human chronological age using a basic blood test (Putin et al., 2016). The team trained the DNNs using a collection of over 600,000 samples from routine blood biochemistry and cell counting assays. The researchers reported that the accuracy of their results provided evidence to suggest that machine learning algorithms could be used to design minimally invasive biomarker tracking methods for ageing that would only improve with greater access to training samples (Putin et al., 2016). Another study examined 19 serum biomarkers, and its results were externally validated using a separate data set from the Framingham Heart Study (Sebastiani et al., 2017). Such studies highlight the ability of machine learning techniques to infer conclusions from basic samples, and to externally validate such conclusions. Still, this was one of the very few studies with this type of external validation and more are needed for clinical application.
3.10.2. ‘Big Data’, machine learning and personalized medicine
Big data can also be used to assist geriatricians for personalized medicine, defined as a medical approach in which treatment is customized on an individual basis based upon disease subtype, genetics, risk, prognosis, or treatment response using specialized diagnostic tests (Frohlich et al., 2018). For instance, predictive biomarkers for the early detection of certain diseases, may help both patients and doctors to decide on appropriate treatment pathways. In addition, the ‘Internet of Things’ refers to the ability of technology to send and receive data via the Internet. As wearable/compact technologies become more prevalent (i.e., phone pedometers, pacemakers, insulin trackers) and their data becomes easier to store and share, so too does it become easier to use life-logging data to track individual’s well-being. Unfortunately, while there is great potential for this type of technical approach, there are currently very few cases of applications within clinical practice (Frohlich et al., 2018), with many studies still in an exploratory phase, requiring further research. For example, one study shows that machine learning techniques have significant potential in developing personalized decision support for chronic disease tele-monitoring systems; however, it was noted that the system would be improved with a larger library of comprehensive predictive markers (Finkelstein and Jeong, 2017). The use of radiomics, the high-throughput mining of quantitative image features from standard-of-care medical imaging that enables data to be extracted and applied within clinical-decision support systems, has also been proposed, especially within the realm of dementia prevention and detection (Wang et al., 2019a). These studies have benefited from large sample sizes (>1000 images) using machine learning. This brings us to the issue of noise reduction, which is crucial for effective use of big data and will enable a more robust extraction of features. Given the immense amount of data expected to be handled in future projects, finding ways to store, process, and analyze this data also presents a challenge for future research.
3.10.3. Biomarkers and policy design
At the societal level biomarkers have numerous applications. Monitoring population-level biomarkers will likely provide an accurate, real-time view of the health state of a given area. This will allow for targeted interventions catered to suit the specific needs of a population. As stated earlier in this piece, modern medicine has provided for major increases in both quality of life at old age, and life expectancy, however, this can also be considered a potential societal burden. Earlier the use of federated systems with respect to online medical records and data sharing was discussed as a potential hurdle to some countries and medical systems in the world. China has recently embraced a centralized health informatics scheme, with over 80 % of medical organizations above the county/district level, 27 % of town level hospitals and all CDC above the county/district level capable of transmitting real-time reporting on the status of epidemics via the public health information system (Zhang et al., 2007). In the future, the data provided by a centralized medical record system has the capacity to train numerous machine learning algorithms for use with biomarkers. Another challenge for population-level biomarker implementation is to select low-cost, minimally invasive testing that can be used at a large scale. With respect to China, great advances have been made in the use of medical informatics within the past 30 years. However one of the hurdles going forward for the country is that much of this investment has been driven by industry and the private sector, and a major priority for the country's future should be to divert resources to academic research (Liang et al., 2017). This is especially true for the poorer members of society, or those without ready access to healthcare, as biomarker are an asset in devising appropriate healthcare plans for populations in need (Fang et al., 2015). Addressing rural areas may be a challenge both in terms of healthcare delivery and biomarker testing, as these regions may lack sufficient infrastructure for both, posing a challenge for the future (Fang et al., 2015). We recommend the use of mobile-equipped information technology services to reach more remote regions.
In summary, biomarkers have a great deal of potential for how doctors can prevent, diagnose, and treat illness associated with ageing. While there are many hurdles going forward, the application of machine learning and big data to biomarker research will provide new opportunities to understand ageing at the molecular level, deliver personalized treatment at the individual level, and design influential and effective policy at the societal and population level.
4. Policy dialog and the renovation of China’s healthcare system
4.1. Reform of social health insurance schemes
Since the beginning of the 21st century, China started to enter a period where it may be classified as an ageing society. At the same time, the compulsory healthcare insurance systems in China has undergone a comprehensive and rapid development, while still emphasizing the ideologies of health equity and social justice (Liu et al., 2016). Three major health insurance schemes have been launched, achieving near-universal coverage in a short time, which gained early appraisal by emulating the goal of the provision of affordable and equitable basic healthcare for all by 2020 (Yip et al., 2012). After the establishment of the Urban Employee Basic Medical Insurance (UEBMI) in 1998, the Chinese government implemented the New Rural Cooperative Medical Scheme (NCMS) for rural residents in 2003, and the Urban Residents Basic Medical Insurance (URBMI) for urban residents without employment in 2007. As a result, social health insurance coverage increased from 29.7–87.9% between 2003 and 2008, and further to 95.7 % by 2011, and has been stable since (Meng et al., 2012). In order to further reform the fragmented health insurance system, the latter two of these schemes were combined into the Basic Medical Insurance for Rural and Urban Residents in early 2016, with a target of making the system less complicated, but more equitable for various social groups.
In the past 10 years of the new round of healthcare reform beginning in 2009, the Chinese government dramatically increased financial investment, with half of all investment in the form of funded premium subsidies for residents to be covered by the social health insurance system (Yip et al., 2019). Universal coverage has since led to improved access to and utilization of healthcare (Meng et al., 2019), decreased the prevalence of catastrophic health expenditure (Yip et al., 2019), and reduced out-of-pocket expenditure as a proportion of total health expenditure, especially for vulnerable groups, including older adults (Xu and Mills, 2019). However, the social health insurance system in China still faces the dual challenge of population ageing (demand) and inefficient delivery on the side of the healthcare system (supply), raising both health expenditures and individual disease burden. Out-of-pocket expenditure as a proportion of disposable personal income increased from 4.98 % in urban regions and 5.17 % in rural areas in 2008 to 5.59 % in 2017 (Xu and Mills, 2019).
Concretely speaking, population ageing addressed the increasing health and social care needs of older people. According to the Report on the Fifth National Health Services Survey, the prevalence of Non-Communicable Disease had increased more than 20 % between 2003–2012, from 50.1–71.8%, while the inpatient rate rose from 7.6–17.9% in between 2003−2013. The outpatient rate also increased to 49.7 % in 2013 (NHFPC, 2015). The reimbursement of social health insurance improved rapidly and accounted for 42 % of total health expenditure in 2017, though while out-of-pocket payments dropped from 60 % in 2000 to 28 % to 2017, financial protection and services packages were insufficient for the elderly (Meng et al., 2019), especially for those in rural regions. Li (2014) reported a three times-higher risk of catastrophic health expenditure among the old population in rural regions (Li et al., 2014). In 2013, expenditures on hospitalization for older people in urban areas were reimbursed 64 % by social health insurance and 53 % were covered for their rural counterparts (WHO, 2015b).
Regional disparity in health benefits for the elderly with insurance aside, a problem of inequity among different health insurance schemes on health outcomes for older adults is still a great challenge. UEBMI recipients were found to have better physical and psychological health outcomes compared to those with URBMI or NCMS insurance. This demonstrates a transformation in health insurance reform from an emphasis on the opportunity-oriented health equity measured by coverage and healthcare accessibility to stressing outcome-based equity composed of health outcomes for the elderly, namely “outcome-based health equity”, giving priority to disadvantaged groups (Liu and Wong, 2016).
In terms of supply-side deficiency and unsatisfied progress in the past 10 years, gaps in the public hospital and pharmaceutical reform have tremendously limited the effectiveness of social health insurance reform, even though the public hospital has removed mark-ups for drug sales, adjusted pricing mechanism, reformed provider payment systems and changed governance structures at the county level (Yip et al., 2019). The hospital-centered health delivery system has induced the growth of both health expenditure and health insurance expenses, which worsened the control of Non-Communicable Diseases and health outcome improvement in ageing society. Unexpectedly, the usage of outpatient and inpatient services in primary health facilities declined from 62 % and 29 % in 2009 to 54 % and 18 % in 2017 (Ma et al., 2019). Due to the lack of qualified long-term care facilities, the length of hospitalization was longer for the old population aged 60 and over (WHO, 2015b), demanding higher expenditure input to cope while wasting health resources. We advocate the immediate application of an integrated health and social care-oriented, particularly in community settings, with the objective of increasing affordability and improving the quality of care for older people.
4.2. Results from pilots of long-term care insurance (LTCI)
Population ageing, family structure shift, and migration, were three major challenges limiting the efficacy of traditional informal care provided by families and their networks. A large proportion of older people with functional disability or dementia will continue to create enormous challenges for an immature Long-Term Care system in China (Liu et al., 2017). It was estimated about 40 million (19.5 % of the elderly) older people had some sort of functional disability by 2015, among which 12.4 million (6.05 % of old population) had a serious status of disability (NHFPC, 2015). At the same time, China has become the largest country in the world to have over 9.5 million people with dementia (Jia et al., 2020).
In response to the increasing need for social care of older people with disability, the central government of China has implemented a pilot practice of LTCI policies in 15 cities, while some local governments were also encouraged by the central government to initiate county-level pilot experiments on LTCI since 2016, in hopes of stimulating the growth of long-term care providers (Luo and Zhan, 2018). Most LTCI schemes were based on the social health insurance system, though these pilots had distinct and diverse eligibility conditions, premium contributions, need assessment instruments, and benefit packages. The reason for carrying out a pilot practice rather than fully implementing a uniform nation-wide scheme reflected the complexity of LTCI, and a worry about cost escalation noted LTCI introduction in the more mature ageing societies of Japan and Germany. After two years of practice, a few evaluations were conducted to estimate the outcome of these pilot practices, identifying a host of problems.
There are several characteristics and unique features present in the Chinese LTCI scheme. At first, coverage was narrow and limited only to older people with the most serious degrees of disability, and excluded older adults with dementia due to security issues and lower quality of care skills. By the end of 2017, less than 2% of the older population in the pilot cities were covered by LTCI plans in Qingdao (Zhu and Osterle, 2019), which was the first city to launch the LTCI scheme in China, a higher proportion of those 65 years and older was achieved in the LTCI practice of the mature ageing populations in Germany (11.7 %) and Japan (12.8 %) (OECD, 2013). Secondly, the need assessment tools used by each pilot city were fragmented and biased. Some pilot cities or counties only employed the Barthel Index to measure physically functional disability, but did not measure cognitive function with any scales, thus leading to the exclusion of older people with dementia from LTCI coverage. More seriously, the results of need assessment were not applied to long-term care service provision, but only used as a “gate keeper” for receiving the fixed benefit package. Assessment tools should be transformed from simple to comprehensive, from a physically oriented test to a multi-dimension health status one, even from health assessment to service assessment. Thirdly, in most pilot plans, long-term care was provided by designated institutions through a contract, and a home- and-community-based caregiver was paid by the insurance scheme, however reimbursements were limited such that a large proportion of costs was still paid out-of-pocket by service users themselves, and unmet needs were still high among the disabled elderly (Yang et al., 2016). In addition, the inequality in access to long-term care services between advantaged and vulnerable elderly was enlarged. In most pilot schemes, higher numbers of benefit packages were allocated to insured groups living in nursing homes or receiving formal care than to those living at home receiving informal care. Retired people with UEBMI had higher affordability and preferred to live in the institutions and received higher reimbursements from insurance. Rural residents could not access good quality long-term care facilities, and received fewer benefits.
The inequality that remains in LTCI practices highlights how policy reform ought to reevaluate and reconstruct the currently fragmented schemes and direct more attention to the disabled elderly with lower socio-economic status and without financial or family support. Although China attempted the LTCI scheme, its most urgent priority was to establish a unified means-test public budget system to cover the most vulnerable social groups regardless of their living locations. Through Lu et al. (2017)’s projection, an investment as small as 0.25 % of GDP (equivalent to about 1.25 % of fiscal revenue) would greatly benefit the frail elderly and those with serious problems of functional disability and/or poor financial status (Lu et al., 2017).
4.3. Policy dialog
In 2016, the Central Committee of the Communist Party of China and the State Council issued the Healthy China 2030 plan. Corresponding with the health-related Sustainable Development Goal (SDG), this is a national mid-term and long-term strategic plan for moving towards universal health coverage and improving health equity, with emphases on health coverage for the whole life circle, including healthy ageing (PRC, 2019). In 2018, China made a major restructuring of national healthcare governance. The National Health Commission (originally called the Ministry of Health) administers and regulates the healthcare delivery system and include two new areas of responsibility: elderly care and tobacco control (Yip et al., 2019). In addition, the National Healthcare Security Administration was established. It is in charge of administering essential health insurances (Urban Employee Basic Health Insurance, Urban-Rural Resident Basic Health Insurance, which integrated the original Urban Resident Basic Health Insurance and New Cooperative Medical Scheme) and Medical Assistance for the poor and vulnerable groups as well as deciding on pricing and drug procurement.
Rapid ageing and an alarming increase in non-communicable diseases (NCDs) have arisen as major health concerns in China (Fang et al., 2015; Marten et al., 2014). In 2009, the National Basic Public Health Service Program was established, which included health management for elderly people, patients with major NCDs (hypertension and diabetes), among others (NHFPC, 2017). The program is financed by government funds, and the government’s per capita allocation increased from 15 to 55 RMB between 2009–2018 (NHFPC, 2017, 2018). China’s ongoing healthcare system reform prioritizes transforming hospital-centered treatment care to integrated and continued care through a tiered healthcare delivery system (Meng et al., 2019). A tiered healthcare delivery model defines the functions at each health facility level, and coordinates care across levels. A common model is that hospitals lead medical alliances to deliver integrated care, and provide support and training to strengthen primary health services (Li et al., 2019; Wang et al., 2018b; WBWHO, 2019). In addition, residents are able to register with a family doctor team who provide preventive and basic healthcare as well as referral services. The government target is universal registration by 2020 (NHC et al., 2016).
China has made good progress in improving equal access to healthcare and financial risk protection for socially vulnerable people over the past decade (Fu et al., 2018; Meng et al., 2019; Yip et al., 2019), but challenges remain. There is a lack of qualified primary healthcare providers who are able to serve as gatekeepers, and the quality of primary healthcare is poorly characterized (Li et al., 2017; Meng et al., 2019). Previous studies reported very low proportions of blood pressure and blood glucose control among patients with hypertension and diabetes seeking care from primary health facilities, and common over-prescription of antibiotics (Li et al., 2017; Su et al., 2017; Wang et al., 2014). Patients persistently bypass primary health facilities and seek perceived good quality of care in high level hospitals, despite many patients complaining of high medical costs and long wait times (Li et al., 2017). On the other hand, most hospitals still largely rely on fee-for-service payment and tie doctors’ salary to the hospital revenue generation, which gives hospitals an incentive to attract and retain patients rather than shifting them primary healthcare. Overuse and overprovision of health services are common in China (Meng et al., 2019; Yip et al., 2019). Consequently, health expenditure has continued to escalate, a trend which threatens the long-term financial sustainability of basic health insurance schemes. The efficiency in using health resources is low (Meng et al., 2019; Yip et al., 2019).
As China continues to progress as an ageing society, strengthening primary healthcare system to provide integrated care will be fundamental to meet growing health needs and obtain the best value from existent health resources. It is difficult to shift from treatment-based intensive care to population-based preventive care and health management while perverse financial incentive for hospitals are not controlled or eliminated. This requires effective collaboration across related sectors led by a strong coordinating authority and needs to bridge policy dialog to ensure health in all policies workable and achievable.
5. Conclusions and future perspectives
China’s prolonged demographic shift has led to decreased fertility, elevated sex ratios, rapid ageing, fast urbanization and major geographic redistributions (Peng, 2011), an inter-disciplinary collaborative approach is necessary to prepare and face the challenges as society continues to age. We present a summary on ways to achieve a healthy ageing society in China at societal, individual, and molecular levels (Fig. 5). Breaking knowledge gaps and eliminating boundaries among different sectors to further integrate and synergize different healthcare-related parties at societal, individual, and molecular levels will optimize the outputs of the Chinese healthcare system. The Chinese Government has adopted a positive stance to investment across the whole spectrum of ageing policies, medical education and training, basic ageing and geriatric research, prevention, primary care, and hospital and residential care. It is necessary to establish updated ageing policies on retirement age, to incentivize employment of the elderly, to encourage lifelong learning, and to invest in senior volunteer programs (Yeoh and Lai, 2016). The education and practice of geriatric medicine has been and will continue to be enhanced, including to further increase the teaching of geriatrics-related subjects in medical school, to design high-quality residency and fellowship programs, and to further integrate geriatric principles into general clinical practice (Yu et al., 2018a). The establishment of the national alliance of NCRCGD has been highly appreciated and welcomed and it will continue to serve as a national platform to educate and train geriatricians.
Fig. 5.
A summary of responses to achieve healthy longevity of the elderly in China. In response to the ageing society and in order to improve the quality of life of the elderly in China, strategies at societal, individual, and cellular levels are presented, detailed in the text. The art of traditional Chinese paper cutting ‘松鶴延年’ (May you enjoy longevity like the pines and the cranes, whereby both considered long living in Chinese culture) was from shutterstock with paid standard license.
While the achievement of healthy ageing and longevity is emerging as an important task for China as in many other countries, this may also be accompanied by socio-economic challenges. One of the major concern is that creating a society where healthy and active ageing and longevity are taken for granted may lead to a swelling of the elderly in the workforce, leading to limitations in job availability for the young, and proving to be a potent economic issue. Countries like China and South Korea are entering a society of population ageing, showing low birth rates and increased life expectancy, which changes the whole economy (Fang et al., 2015; Korea, 2017). Population ageing will likely have several macro-economic effects, touching various domains such as overall industrial structure, current account and inflation, output growth, household finance, labor markets, consumption, and even fiscal and monetary policy (Korea, 2017). It is therefore imperative to give a comprehensive assessment of population ageing in view of its effects on society and the economy in the long-term, to provide evidence to inform future policies. While a challenging task, some suggested responses to the early-emerging changes that could be taken to offset the effects of the ageing society include promoting the production of larger families in the young, finding ways to ensure jobs remain for the young should the elderly be able to continue longer in their positions, along with more general preparations on transform to an elderly-friendly society.
It is delightful to witness the progress of basic and translational ageing research in China, as supported by increases in the number of grants and funding opportunities, as well as by rising numbers of high profile publications and discoveries (He et al., 2019c). Joint efforts from the government and stakeholders of each and every sector should be encouraged to nurture an elderly-friendly society, of most import are reforming the Social Support System to support China’s ageing society, and the introduction of health service/investment interventions aimed at reducing inequalities in health among older people in China. We suggest current research focus on basic and translational gerontology to improve healthy longevity in the elderly, and on developing an integrated and affordable health and social care delivery system to meet the complex needs of a growing elderly population, and to finally transform China into an age-enabling country where well-being and healthy longevity can be celebrated for decades to come.
Declaration of Competing Interest
E.F.F. has CRADA arrangements with ChromaDex and is consultant to Aladdin Healthcare Technologies and the Vancouver Dementia Prevention Centre. N.Y.W is Founder CEO of Pinetree Care Group (paid executive), consultant to China Research Center on Ageing and National Health Commission, as well as member of WHO Consortium on Healthy Ageing and World Economic Forum Global Future Council on Health and Healthcare, Standing Committee Member of China Association of Gerontology and Geriatrics (voluntary roles). Z.N. is CTO of Aladdin Healthcare Technologies. CW provides paid consultant services to HealthKeeperS.
Acknowledgements
The authors acknowledge the valuable work of the many investigators whose published articles they were unable to cite owing to space limitations. The authors thank Dr. Vilhelm Bohr at the NIA and University of Copenhagen for reading of the manuscript. E.F.F. is supported by HELSE SØR-ØST (#2017056, #2020001), the Research Council of Norway (#262175 and #277813), the National Natural Science Foundation of China (#81971327), an Akershus University Hospital Strategic grant (#269901), and a Rosa Sløyfe grant (#207819) from the Norwegian Cancer Society. H.C.Z. is supported by the Natural Science Foundation of China Young Scientist Fund (81703278), Australian National Health and Medical Research Council Early Career Fellowship (APP1092621), National Science and Technology Major Project of China (2018ZX10721102), Sanming Project of Medicine in Shenzhen [SZSM201811071] and the Open Research Fund of State Key Laboratory of Molecular Vaccinology and Molecular Diagnostics (SKLVD2019KF001). J.L. is supported by the National Natural Science Foundation of China (71804201), the Natural Science Foundation of Guangdong Province (#2018A0303130046, #2017A030310346) and SYSU Scientific Research Foundation (#17ykpy15). L.K. is supported by National Key R&D Program of China (No. 2018YFC2002104) and the CAMS Innovation Fund for Medical Sciences (CIFMS #2017-I2M-3-008). G.B.C. is supported by the National Natural Science Foundation of China (#U1801285), National Key R&D Program of China (#2018YFC2002000) and the Natural Science Foundation of Guangzhou City (#201904010111). X.T.L is supported by a Major Project of National Social Science Foundation of China (13&ZD163), and a Major Project of Zhejiang Social Science Foundation (19YSXK02ZD). C.W. is supported by the Suzhou Municipal Science and Technology Bureau (SS2019069). QL is supported by Kunshan Government Research Fund. We thank Bowen Liang (Sun Yat-Sen University), Chuyao Wang (University of California, Davis) for their contribution to the manuscript. Z. Niu is supported by Aladdin Healthcare Technologies.
References
- Abida W.M., Gu W. p53-Dependent and p53-independent activation of autophagy by ARF. Cancer Res. 2008;68:352–357. doi: 10.1158/0008-5472.CAN-07-2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ADI . 2019. World Alzheimer Report 2019: Attitudes to dementia. Alzheimer’s disease International. [Google Scholar]
- Aman Y., Frank J., Lautrup S.H., Matysek A., Niu Z., Yang G., Shi L., Bergersen L.H., Storm-Mathisen J., Rasmussen L.J., et al. The NAD(+)-mitophagy axis in healthy longevity and in artificial intelligence-based clinical applications. Mech. Ageing Dev. 2019 doi: 10.1016/j.mad.2019.111194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austad S.N., Fischer K.E. Sex differences in lifespan. Cell Metab. 2016;23:1022–1033. doi: 10.1016/j.cmet.2016.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barré-Sinoussi F., Chermann J., Rey F., Nugeyre M., Chamaret S., Gruest J., Dauguet C., Axler-Blin C., Vézinet-Brun F., Rouzioux C., et al. Isolation of a T-Lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) Science. 1983;220:868–871. doi: 10.1126/science.6189183. [DOI] [PubMed] [Google Scholar]
- Barzilai N., Crandall J.P., Kritchevsky S.B., Espeland M.A. Metformin as a tool to target aging. Cell Metab. 2016;23:1060–1065. doi: 10.1016/j.cmet.2016.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belibasakis G.N. Microbiological changes of the ageing oral cavity. Arch. Oral Biol. 2018;96:230–232. doi: 10.1016/j.archoralbio.2018.10.001. [DOI] [PubMed] [Google Scholar]
- Bollero P., Franco R., Cecchetti F., Miranda M., Barlattani A., Jr., Dolci A., Ottria L. Oral health and implant therapy in Parkinson’s patients: review. Oral Implantol. (Rome) 2017;10:105–111. doi: 10.11138/orl/2017.10.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt M., Haberkern K., Szydlik M. Intergenerational help and care in Europe. Eur. Sociol. Rev. 2009;25:585–601. [Google Scholar]
- Broese van Groenou M.I., De Boer A. Providing informal care in a changing society. Eur. J. Ageing. 2016;13:271–279. doi: 10.1007/s10433-016-0370-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brook R.D., Rajagopalan S., Pope C.A., 3rd., Brook J.R., Bhatnagar A., Diez-Roux A.V., Holguin F., Hong Y., Luepker R.V., Mittleman M.A., et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- Brousseau K., Filley C., Kaye K., Kiser J., Adler L., Connick E. Dementia with features of Alzheimer’s disease and HIV-associated dementia in an elderly man with AIDS. AIDS. 2009;23:1029–1031. doi: 10.1097/QAD.0b013e32832ac380. [DOI] [PubMed] [Google Scholar]
- Bussian T.J., Aziz A., Meyer C.F., Swenson B.L., van Deursen J.M., Baker D.J. Clearance of senescent glial cells prevents tau-dependent pathology and cognitive decline. Nature. 2018;562:578–582. doi: 10.1038/s41586-018-0543-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadenza. http://www.cadenza.hk/index.php?lang=en.
- Cai Y. China’s new demographic reality: learning from the 2010 census. Popul. Dev. Rev. 2013;39:371–396. doi: 10.1111/j.1728-4457.2013.00608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campisi J., Kapahi P., Lithgow G.J., Melov S., Newman J.C., Verdin E. From discoveries in ageing research to therapeutics for healthy ageing. Nature. 2019;571:183–192. doi: 10.1038/s41586-019-1365-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CCDC . 2016. AIDS Database.http://www.phsciencedata.cn/Share/ky_sjml.jsp?id=%22c2ca694e-3995-4c7f-9078-3ed0aaf14556%22: [Google Scholar]
- CCDC . 2019. Infectious Diseases.http://www.phsciencedata.cn/Share/en/index.jsp The Data-center of China Public Health Science. [Google Scholar]
- Chan K.Y., Wang W., Wu J.J., Liu L., Theodoratou E., Car J., Middleton L., Russ T.C., Deary I.J., Campbell H., et al. Epidemiology of Alzheimer’s disease and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet. 2013;381:2016–2023. doi: 10.1016/S0140-6736(13)60221-4. [DOI] [PubMed] [Google Scholar]
- Chan R., Leung J., Woo J., Kwok T. Associations of dietary protein intake on subsequent decline in muscle mass and physical functions over four years in ambulant older Chinese people. J. Nutr. Health Aging. 2014;18:171–177. doi: 10.1007/s12603-013-0379-y. [DOI] [PubMed] [Google Scholar]
- Chau P.H., Wong M., Lee A., Ling M., Woo J. Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001-09. Age Ageing. 2013;42:229–233. doi: 10.1093/ageing/afs177. [DOI] [PubMed] [Google Scholar]
- Chau P.H., Wong M., Woo J. Trends in ischaemic heart disease hospitalisation and case fatality in the Hong Kong Chinese population 2000-2009: a secondary analysis. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-002963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z. Launch of the health-care reform plan in China. Lancet. 2009;373:1322–1324. doi: 10.1016/S0140-6736(09)60753-4. [DOI] [PubMed] [Google Scholar]
- Chen X., Silverstein M. Intergenerational social support and the psychological well-being of older parents in China. Res. Aging. 2000;22:43–65. [Google Scholar]
- Chen G., Yung R. Meta‐inflammageing at the crossroad of geroscience. Aging Med. 2019;2:157–161. doi: 10.1002/agm2.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L.K., Liu L.K., Woo J., Assantachai P., Auyeung T.W., Bahyah K.S., Chou M.Y., Chen L.Y., Hsu P.S., Krairit O., et al. Sarcopenia in Asia: consensus report of the asian working group for sarcopenia. J. Am. Med. Dir. Assoc. 2014;15:95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- Chen W., Zheng R., Baade P.D., Zhang S., Zeng H., Bray F., Jemal A., Yu X.Q., He J. Cancer statistics in China, 2015. CA Cancer J. Clin. 2016;66:115–132. doi: 10.3322/caac.21338. [DOI] [PubMed] [Google Scholar]
- Chen L., His J.H., Wu X., Shen Z., Lu H., Chen H., Huang H., Zhang H., Ruan Y., Shao Y., et al. Disparities in HIV and syphilis prevalence and risk factors between older male clients with and without steady sex partners in southwestern rural China. BMC Infect. Dis. 2017;17:269. doi: 10.1186/s12879-017-2367-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Wei G., Qin Q., Cai C., Cui Y. Temporal and spatial distribution characteristics of HIV-infected and AIDS patients aged 15 years and over in China from 2010 to 2016. Chinese Journal of Epidemiology. 2018;39:739–744. [Google Scholar]
- Chen S., Guo L., Wang Z., Mao W., Ge Y., Ying X., Fang J., Long Q., Liu Q., Xiang H., et al. Current situation and progress toward the 2030 health-related Sustainable Development Goals in China: a systematic analysis. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Liu S., Leng S.X. Chronic low-grade inflammatory phenotype (CLIP) and senescent immune dysregulation. Clin. Ther. 2019;41:400–409. doi: 10.1016/j.clinthera.2019.02.001. [DOI] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H.W.B. Advance care planning in chinese seniors: cultural perspectives. J. Palliat. Care. 2018;33:242–246. doi: 10.1177/0825859718763644. [DOI] [PubMed] [Google Scholar]
- Chhetri J.K., Chan P., Ma L., Peng D., Rodriguez-Manas L., Cesari M., Vellas B. Prevention of disability in the frail chinese older population. J. Frailty Aging. 2019;8:2–6. doi: 10.14283/jfa.2018.27. [DOI] [PubMed] [Google Scholar]
- Childs B.G., Baker D.J., Wijshake T., Conover C.A., Campisi J., van Deursen J.M. Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science. 2016;354:472–477. doi: 10.1126/science.aaf6659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinanews . 2019. Proportion of People Aged 50 Years and Older in HIV-infected Cases Doubled in 9 Years.http://www.chinanews.com/jk/2019/11-30/9021488.shtml [Google Scholar]
- CHP . 2019. Age-standardised Death Rates by Leading Causes of Death; pp. 2001–2018.https://www.chp.gov.hk/en/statistics/data/10/27/ 339.html: Centre for Health Protection. [Google Scholar]
- CHP . 2019. Flu Express.https://www.chp.gov.hk/en/resources/29/ 304.html.: Centre for Health Protection) [Google Scholar]
- CHP . 2019. Number of Deaths by Leading Causes of Death by Sex by Age in 2017.https://www.chp.gov.hk/en/statistics/data/10/27/ 340.html: Centre for Health Protection) [Google Scholar]
- Christensen K., McGue M., Petersen I., Jeune B., Vaupel J.W. Exceptional longevity does not result in excessive levels of disability. Proc. Natl. Acad. Sci. U.S.A. 2008;105:13274–13279. doi: 10.1073/pnas.0804931105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CNCA . 2020. National and Local Government Policies at.http://www.cncaprc.gov.cn/zcfg/index.jhtml# [Google Scholar]
- Cruz-Jentoft A.J., Baeyens J.P., Bauer J.M., Boirie Y., Cederholm T., Landi F., Martin F.C., Michel J.P., Rolland Y., Schneider S.M., et al. Sarcopenia: european consensus on definition and diagnosis: report of the european working group on Sarcopenia in older people. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Jentoft A.J., Landi F., Schneider S.M., Zuniga C., Arai H., Boirie Y., Chen L.K., Fielding R.A., Martin F.C., Michel J.P., et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS) Age Ageing. 2014;43:748–759. doi: 10.1093/ageing/afu115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz-Jentoft A.J., Bahat G., Bauer J., Boirie Y., Bruyere O., Cederholm T., Cooper C., Landi F., Rolland Y., Sayer A.A., et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Cabo R., Mattson M.P. Effects of intermittent fasting on health, aging, and disease. N. Engl. J. Med. 2019;381:2541–2551. doi: 10.1056/NEJMra1905136. [DOI] [PubMed] [Google Scholar]
- Dominy S.S., Lynch C., Ermini F., Benedyk M., Marczyk A., Konradi A., Nguyen M., Haditsch U., Raha D., Griffin C., et al. Porphyromonas gingivalis in Alzheimer’s disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci. Adv. 2019;5:eaau3333. doi: 10.1126/sciadv.aau3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du P., Wang Y. Population ageing and the development of social care service systems for older persons in China. International Journal on Ageing in Developing Countries. 2016;1:40–52. [Google Scholar]
- EIU . 2015. The 2015 Quality of Death Indexranking Palliative Care Across the Worldan Economist Intelligence Unit Study, Commissioned by the Lien FoundationKEY FINDINGS INFOGRAPHIC (The Economist Intelligence Unit 2015) Link.https://www.pallnetz.ch/cm_data/2015_Quality_of_Death_Index_Infographic.pdf [Google Scholar]
- Fan L., Xu W., Cai Y., Hu Y., Wu C. Sleep duration and the risk of dementia: a systematic review and meta-analysis of prospective cohort studies. J. Am. Med. Dir. Assoc. 2019;20(1480–1487):e1485. doi: 10.1016/j.jamda.2019.06.009. [DOI] [PubMed] [Google Scholar]
- Fang H. 2015. Report on Square-dancing in China. [Google Scholar]
- Fang E.F. Mitophagy and NAD(+) inhibit alzheimer disease. Autophagy. 2019;15:1112–1114. doi: 10.1080/15548627.2019.1596497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang E.F., Scheibye-Knudsen M., Jahn H.J., Li J., Ling L., Guo H., Zhu X., Preedy V., Lu H., Bohr V.A., et al. A research agenda for aging in China in the 21st century. Ageing Res. Rev. 2015;24:197–205. doi: 10.1016/j.arr.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang E.F., Scheibye-Knudsen M., Chua K.F., Mattson M.P., Croteau D.L., Bohr V.A. Nuclear DNA damage signalling to mitochondria in ageing. Nat. Rev. Mol. Cell Biol. 2016;17:308–321. doi: 10.1038/nrm.2016.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang E.F., Hou Y., Palikaras K., Adriaanse B.A., Kerr J.S., Yang B., Lautrup S., Hasan-Olive M.M., Caponio D., Dan X., et al. Mitophagy inhibits amyloid-beta and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease. Nat. Neurosci. 2019;22:401–412. doi: 10.1038/s41593-018-0332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng L., Shay D.K., Jiang Y., Zhou H., Chen X., Zheng Y., Jiang L., Zhang Q., Lin H., Wang S., et al. Influenza-associated mortality in temperate and subtropical Chinese cities, 2003-2008. Bull. World Health Organ. 2012;90:279B–288B. doi: 10.2471/BLT.11.096958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrucci L., Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat. Rev. Cardiol. 2018;15:505–522. doi: 10.1038/s41569-018-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FHB . 2019. District Health Centres.https://www.fhb.gov.hk/dhc/en/index.html [Google Scholar]
- Finkelstein J., Jeong I.C. Machine learning approaches to personalize early prediction of asthma exacerbations. Ann. N. Y. Acad. Sci. 2017;1387:153–165. doi: 10.1111/nyas.13218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frailty-China . 2019. Frailty Asia-China Conference at.http://www.frailty-china.com/ABOUT-FRAILTY-CHINA-9158 [Google Scholar]
- Frohlich H., Balling R., Beerenwinkel N., Kohlbacher O., Kumar S., Lengauer T., Maathuis M.H., Moreau Y., Murphy S.A., Przytycka T.M., et al. From hype to reality: data science enabling personalized medicine. BMC Med. 2018;16:150. doi: 10.1186/s12916-018-1122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu W., Zhao S., Zhang Y., Chai P., Goss J. Research in health policy making in China: out-of-pocket payments in Healthy China 2030. BMJ. 2018;360:k234. doi: 10.1136/bmj.k234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GBD Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilmour B.C., Gudmundsrud R., Frank J., Hov A., Hindkjaer Lautrup S., Aman Y., Rosjo H., Brenner C., Ziegler M., Tysnes O.B., et al. Targeting NAD(+) in translational research to relieve diseases and conditions of metabolic stress and ageing. Mech. Ageing Dev. 2020 doi: 10.1016/j.mad.2020.111208. [DOI] [PubMed] [Google Scholar]
- Gong X., Yue X., Teng F., Jiang N., Men P. Epidemiological characteristics and trends of Chinese syphilis from 2000 to 2013. Chinese Journal of Dermatology. 2014;47:310–315. [Google Scholar]
- Gong X., Yue X., Jiang N., Teng F., Men P., Li J., Wang J. Epidemiological characteristics and trends of gonorrhea in China from 2000 to 2014. Chinese Journal of Dermatology. 2015:301–306. [Google Scholar]
- Greene M., Hessol N.A., Perissinotto C., Zepf R., Hutton Parrott A., Foreman C., Whirry R., Gandhi M., John M. Loneliness in older adults living with HIV. AIDS Behav. 2018;22:1475–1484. doi: 10.1007/s10461-017-1985-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guaraldi G., Malagoli A., Calcagno A., Mussi C., Celesia B.M., Carli F., Piconi S., De Socio G.V., Cattelan A.M., Orofino G., et al. The increasing burden and complexity of multi-morbidity and polypharmacy in geriatric HIV patients: a cross sectional study of people aged 65 - 74 years and more than 75 years. BMC Geriatr. 2018;18:99. doi: 10.1186/s12877-018-0789-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gyurmey T., Kwiatkowski J. Program of all-inclusive care for the elderly (PACE): integrating health and social care since 1973. R. I. Med. J. (2013) 2019;102:30–32. [PubMed] [Google Scholar]
- Hanna D.B., Ramaswamy C., Kaplan R.C., Kizer J.R., Anastos K., Daskalakis D., Zimmerman R., Braunstein S.L. Trends in Cardiovascular Disease Mortality Among Persons With HIV in New York City, 2001-2012. Clin. Infect. Dis. 2016;63:1122–1129. doi: 10.1093/cid/ciw470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison D.E., Strong R., Sharp Z.D., Nelson J.F., Astle C.M., Flurkey K., Nadon N.L., Wilkinson J.E., Frenkel K., Carter C.S., et al. Rapamycin fed late in life extends lifespan in genetically heterogeneous mice. Nature. 2009;460:392–395. doi: 10.1038/nature08221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison D.E., Strong R., Alavez S., Astle C.M., DiGiovanni J., Fernandez E., Flurkey K., Garratt M., Gelfond J.A.L., Javors M.A., et al. Acarbose improves health and lifespan in aging HET3 mice. Aging Cell. 2019;18 doi: 10.1111/acel.12898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HBGM . 2019. 2018 Annual Report of Notifiable Diseases.http://www.ssm.gov.mo/docs/15564/15564_03bd28c6114b4e2fbd0c19537525c398_000.pdf.: Health Bureau of the Government of the Macao) [Google Scholar]
- HBGM . 2019. Statistical Yearbook.https://www.ssm.gov.mo/portal/: Health Bureau of the Government of the Macao) [Google Scholar]
- He Y., Luan F.X., Yao Y., Yang S.S., Xie H.G., Li J., Liu M., Wang J.H., Wu L., Zhu Q., et al. [China Hainan Centenarian Cohort Study: study design and preliminary results] Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38:1292–1298. doi: 10.3760/cma.j.issn.0254-6450.2017.09.029. [DOI] [PubMed] [Google Scholar]
- He B., Ma Y., Wang C., Jiang M., Geng C., Chang X., Ma B., Han L. Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. J. Nutr. Health Aging. 2019;23:442–450. doi: 10.1007/s12603-019-1179-9. [DOI] [PubMed] [Google Scholar]
- He N., Ding Y., Li J., Yuan S., Xu L., Qiao S., Xu X., Zhu B., Shi R., Barile J.P., et al. HIV and aging in Mainland China: implications for control and prevention research. Curr. HIVAIDS Rep. 2019;16:439–447. doi: 10.1007/s11904-019-00473-2. [DOI] [PubMed] [Google Scholar]
- He X., Song M., Qu J., Guo Y., Cao H., Sun R., Liu G.H., Shen Y., Major Program Expert, G Basic and translational aging research in China: present and future. Protein Cell. 2019;10:476–484. doi: 10.1007/s13238-019-0617-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiramoto J.S., Teraa M., de Borst G.J., Conte M.S. Interventions for lower extremity peripheral artery disease. Nat. Rev. Cardiol. 2018;15:332–350. doi: 10.1038/s41569-018-0005-0. [DOI] [PubMed] [Google Scholar]
- Hitt R., Young-Xu Y., Silver M., Perls T. Centenarians: the older you get, the healthier you have been. Lancet. 1999;354:652. doi: 10.1016/S0140-6736(99)01987-X. [DOI] [PubMed] [Google Scholar]
- Hong X., Wongtongkam N., Ward P.R., Xiaio S., Wang S., Peng Q., al E., Wang C. Association of demographic, lifestyle factors and serum biomarkers with hypertension in elderly Chinese people. Ageing Soc. 2017;37:661–674. [Google Scholar]
- Hu C., Jia W. Diabetes in China: epidemiology and genetic risk factors and their clinical utility in personalized medication. Diabetes. 2018;67:3–11. doi: 10.2337/dbi17-0013. [DOI] [PubMed] [Google Scholar]
- Hu T.-W., Lee A.H., Mao Z. Economics of Tobacco Control in China: From Policy Research to Practice. World Scientific; 2016. WHO framework convention on tobacco control in China: barriers, challenges and recommendations; pp. 247–263. [Google Scholar]
- Hu X., Jiang J., Wang H., Zhang L., Dong B., Yang M. Association between sleep duration and sarcopenia among community-dwelling older adults: a cross-sectional study. Medicine (Baltimore) 2017;96:e6268. doi: 10.1097/MD.0000000000006268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu W., Zhang L., Li M.X., Shen J., Liu X.D., Xiao Z.G., Wu D.L., Ho I.H.T., Wu J.C.Y., Cheung C.K.Y., et al. Vitamin D3 activates the autolysosomal degradation function against Helicobacter pylori through the PDIA3 receptor in gastric epithelial cells. Autophagy. 2019;15:707–725. doi: 10.1080/15548627.2018.1557835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Li F., Chiou J.F. Psychometric properties of the Chinese mainland version of the Palliative Care Spiritual Care Competency Scale (PCSCCS-M) in nursing: a cross-sectional study. BMC Palliat. Care. 2019;18:27. doi: 10.1186/s12904-019-0409-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hua P. Analysis on the problems and countermeasures of the needs assessment of long-term care insurance in China (in Chinese) Labor Security World. 2019 [Google Scholar]
- Huang Y., Wang Y., Wang H., Liu Z., Yu X., Yan J., Yu Y., Kou C., Xu X., Lu J., et al. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail K., Nussbaum L., Sebastiani P., Andersen S., Perls T., Barzilai N., Milman S. Compression of morbidity is observed across cohorts with exceptional longevity. J. Am. Geriatr. Soc. 2016;64:1583–1591. doi: 10.1111/jgs.14222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeon O.H., Kim C., Laberge R.M., Demaria M., Rathod S., Vasserot A.P., Chung J.W., Kim D.H., Poon Y., David N., et al. Local clearance of senescent cells attenuates the development of post-traumatic osteoarthritis and creates a pro-regenerative environment. Nat. Med. 2017;23:775–781. doi: 10.1038/nm.4324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia J., Wang F., Wei C., Zhou A., Jia X., Li F., Tang M., Chu L., Zhou Y., Zhou C., et al. The prevalence of dementia in urban and rural areas of China. Alzheimers Dement. 2014;10:1–9. doi: 10.1016/j.jalz.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Jia L., Quan M., Fu Y., Zhao T., Li Y., Wei C., Tang Y., Qin Q., Wang F., Qiao Y., et al. Dementia in China: epidemiology, clinical management, and research advances. Lancet Neurol. 2020;19:81–92. doi: 10.1016/S1474-4422(19)30290-X. [DOI] [PubMed] [Google Scholar]
- Jiang Q. Analysis of risk factors for male sexual dysfunction. Electronic Journal of Clinical Medical Literature. 2016;3:11111. [Google Scholar]
- Justice J.N., Nambiar A.M., Tchkonia T., LeBrasseur N.K., Pascual R., Hashmi S.K., Prata L., Masternak M.M., Kritchevsky S.B., Musi N., et al. Senolytics in idiopathic pulmonary fibrosis: results from a first-in-human, open-label, pilot study. EBioMedicine. 2019;40:554–563. doi: 10.1016/j.ebiom.2018.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Liu X.H., Zhang J., Shan P.Y., Wang J.P., Zhong P., Du X.H., Du Y.F., Yu B.C., Wei N., et al. Attitudes toward advance directives among patients and their family members in China. J. Am. Med. Dir. Assoc. 2017;18(808):e807–e808. doi: 10.1016/j.jamda.2017.05.014. e811. [DOI] [PubMed] [Google Scholar]
- Kang L., Gao Y., Liu X., Liang Y., Chen Y., Liang Y., Zhang L., Chen W., Pang H., Peng L.N. Effects of whey protein nutritional supplement on muscle function among community-dwelling frail older people: a multicenter study in China. Arch. Gerontol. Geriatr. 2019;83:7–12. doi: 10.1016/j.archger.2019.03.012. [DOI] [PubMed] [Google Scholar]
- Kasearu K., Kutsar D. In: In Intergenerational Relations: European Perspectives on Family and Society. Albert I., Ferring D., editors. The Policy Press; Bristol: 2013. Intergenerational solidarity in families: interplay between the family and the state; pp. 25–38. [Google Scholar]
- Kattenstroth J.-C., Kolankowska I., Kalisch T., Dinse H.R. Superior sensory, motor, and cognitive performance in elderly individuals with multi-year dancing activities. Front. Aging Neurosci. 2010;2:31. doi: 10.3389/fnagi.2010.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr J.S., Adriaanse B.A., Greig N.H., Mattson M.P., Cader M.Z., Bohr V.A., Fang E.F. Mitophagy and alzheimer’s disease: cellular and molecular mechanisms. Trends Neurosci. 2017;40:151–166. doi: 10.1016/j.tins.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kober L., Thune J.J., Nielsen J.C., Haarbo J., Videbaek L., Korup E., Jensen G., Hildebrandt P., Steffensen F.H., Bruun N.E., et al. Defibrillator implantation in patients with nonischemic systolic heart failure. N. Engl. J. Med. 2016;375:1221–1230. doi: 10.1056/NEJMoa1608029. [DOI] [PubMed] [Google Scholar]
- Kong J., Wilson G., Park J., Pereira K., Walpole C., Yeung A. Treating depression with Tai Chi: state of the art and future perspectives. Front. Psychiatry. 2019;10:237. doi: 10.3389/fpsyt.2019.00237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korea Bo. 2017. Population Aging: Impacts and Policy Imperatives. Bank of Korea.https://ssrn.com/abstract=3258199 Forthcoming, Available at SSRN: or. [DOI] [Google Scholar]
- Kramer A., Lazzarotto A., Sprinz E., Manfroi W. Metabolic abnormalities, antiretroviral therapy and cardiovascular disease in elderly patients with HIV. Arq. Bras. Cardiol. 2009;93 doi: 10.1590/s0066-782x2009001100019. [DOI] [PubMed] [Google Scholar]
- Kunz L., Schroder T.N., Lee H., Montag C., Lachmann B., Sariyska R., Reuter M., Stirnberg R., Stocker T., Messing-Floeter P.C., et al. Reduced grid-cell-like representations in adults at genetic risk for Alzheimer’s disease. Science. 2015;350:430–433. doi: 10.1126/science.aac8128. [DOI] [PubMed] [Google Scholar]
- Lafortune L., Martin S., Kelly S., Kuhn I., Remes O., Cowan A., Brayne C. Behavioural risk factors in mid-life associated with successful ageing, disability, dementia and frailty in later life: a rapid systematic review. PLoS One. 2016;11 doi: 10.1371/journal.pone.0144405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamster I.B., Asadourian L., Del Carmen T., Friedman P.K. The aging mouth: differentiating normal aging from disease. Periodontol. 2016;2000(72):96–107. doi: 10.1111/prd.12131. [DOI] [PubMed] [Google Scholar]
- Lautrup S., Sinclair D.A., Mattson M.P., Fang E.F. NAD+ in brain ageing and neurodegenerative disorders. Cell Metab. 2019;30:630–655. doi: 10.1016/j.cmet.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.S., Auyeung T.W., Leung J., Kwok T., Woo J. Transitions in frailty states among community-living older adults and their associated factors. J. Am. Med. Dir. Assoc. 2014;15:281–286. doi: 10.1016/j.jamda.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Lee C.H., Wang J.Y., Lin H.C., Lin P.Y., Chang J.H., Suk C.W., Lee L.N., Lan C.C., Bai K.J. Treatment delay and fatal outcomes of pulmonary tuberculosis in advanced age: a retrospective nationwide cohort study. BMC Infect. Dis. 2017;17:449. doi: 10.1186/s12879-017-2554-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Galea G. Healthy China 2030: an opportunity for tobacco control. Lancet. 2019;394:1123–1125. doi: 10.1016/S0140-6736(19)32048-3. [DOI] [PubMed] [Google Scholar]
- Li Y., Wu Q., Liu C., Kang Z., Xie X., Yin H., Jiao M., Liu G., Hao Y., Ning N. Catastrophic health expenditure and rural household impoverishment in China: what role does the new cooperative health insurance scheme play? PLoS One. 2014;9 doi: 10.1371/journal.pone.0093253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L.H., Sheng C.S., Hu B.C., Huang Q.F., Zeng W.F., Li G.L., Liu M., Wei F.F., Zhang L., Kang Y.Y., et al. The prevalence, incidence, management and risks of atrial fibrillation in an elderly Chinese population: a prospective study. BMC Cardiovasc. Disord. 2015;15:31. doi: 10.1186/s12872-015-0023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Lu J., Hu S., Cheng K.K., De Maeseneer J., Meng Q., Mossialos E., Xu D.R., Yip W., Zhang H., et al. The primary health-care system in China. Lancet. 2017;390:2584–2594. doi: 10.1016/S0140-6736(17)33109-4. [DOI] [PubMed] [Google Scholar]
- Li H., Chen Y., Gao H., Chang J., Su D., Lei S., Jiang D., Hu X., Tan M., Chen Z. Effect of an integrated payment system on the direct economic burden and readmission of rural cerebral infarction inpatients: evidence from Anhui. China. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16091554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J., Wei K., Meng Q., Chen Z., Zhang J., Lei J. Development of medical informatics in China over the past 30 years from a conference perspective and a Sino-American comparison. PeerJ. 2017;5:e4082. doi: 10.7717/peerj.4082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao J., Chen S., Chen S., Yang Y.J. Personal and social environmental correlates of square dancing habits in chinese middle-aged and older adults living in communities. J. Aging Phys. Act. 2019;27:696–702. doi: 10.1123/japa.2018-0310. [DOI] [PubMed] [Google Scholar]
- Liao J., Mawditt C., Scholes S., Lu W., Umeda M., Muniz Terrera G., Hao Y., Mejia S. Similarities and differences in health-related behavior clustering among older adults in Eastern and Western countries: a latent class analysis of global aging cohorts. Geriatr. Gerontol. Int. 2019;19:930–937. doi: 10.1111/ggi.13737. [DOI] [PubMed] [Google Scholar]
- Liao J., Yang Y.J., Xu D.R. Multiyear square dancing is associated with superior mental processing capacity but not memory in middle-aged and older chinese women: a cross-sectional propensity score matching analysis. J. Phys. Act. Health. 2020:1–8. doi: 10.1123/jpah.2019-0336. [DOI] [PubMed] [Google Scholar]
- Lin H., Guo Y., Zheng Y., Di Q., Liu T., Xiao J., Li X., Zeng W., Cummings-Vaughn L.A., Howard S.W., et al. Long-term effects of ambient PM2.5 on hypertension and blood pressure and attributable risk among older chinese adults. Hypertension. 2017;69:806–812. doi: 10.1161/HYPERTENSIONAHA.116.08839. Dallas, Tex : 1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.T., Seo J., Gao F., Feldman H.M., Wen H.L., Penney J., Cam H.P., Gjoneska E., Raja W.K., Cheng J., et al. APOE4 causes widespread molecular and cellular alterations associated with alzheimer’s disease phenotypes in human iPSC-Derived brain cell types. Neuron. 2018;98:1141–1154. doi: 10.1016/j.neuron.2018.05.008. e1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H., Ding Y., Ning C., Qiao X., Chen X., Chen X., Shen W., Liu X., Hong Y., He N. Age-specific associations between HIV infection and carotid artery intima-media thickness in China: a cross-sectional evaluation of baseline data from the CHART cohort. Lancet HIV. 2019;6:e860–e868. doi: 10.1016/S2352-3018(19)30263-2. [DOI] [PubMed] [Google Scholar]
- Liu S.J., Guo X.D. Comparative research of middel-aged women fitness effects of Taiji Quan and sqaure dance. China Sport Science and Technology. 2013;49:103–105. [Google Scholar]
- Liu G.Y., Sabatini D.M. mTOR at the nexus of nutrition, growth, ageing and disease. Nat. Rev. Mol. Cell Biol. 2020 doi: 10.1038/s41580-019-0199-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Wong H. The reform of the medical welfare system and health equity for the elderly in China: a study in Zhejiang. J. Chinese Sociol. 2016;3:1–22. [Google Scholar]
- Liu L., Yuan C. Construction of palliative care training contents in China: a Delphi study. Cancer Nurs. 2009;32:446–455. doi: 10.1097/NCC.0b013e3181ab572e. [DOI] [PubMed] [Google Scholar]
- Liu G.H., Barkho B.Z., Ruiz S., Diep D., Qu J., Yang S.L., Panopoulos A.D., Suzuki K., Kurian L., Walsh C., et al. Recapitulation of premature ageing with iPSCs from Hutchinson-Gilford progeria syndrome. Nature. 2011;472:221–225. doi: 10.1038/nature09879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Lin X., Xu Y., Chen S., Shi J., Morisky D. Emerging HIV epidemic among older adults in Nanning, China. AIDS Patient Care STDS. 2012;26:565–567. doi: 10.1089/apc.2012.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Wong H., Liu K. Outcome-based health equity across different social health insurance schemes for the elderly in China. BMC Health Serv. Res. 2016;16:9. doi: 10.1186/s12913-016-1261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Lu B., Feng Z. Intergenerational transfers and informal care for disabled elderly persons in China: evidence from CHARLS. Health Soc. Care Community. 2017;25:1364–1374. doi: 10.1111/hsc.12441. [DOI] [PubMed] [Google Scholar]
- Liu C.W., Hung C.H., Yang W.P. [A challenge for home-based hospice care: good death at home] Hu Li Za Zhi. 2019;66:74–81. doi: 10.6224/JN.201912_66(6).10. [DOI] [PubMed] [Google Scholar]
- Lochner K.A., Cox C.S. Prevalence of multiple chronic conditions among Medicare beneficiaries, United States, 2010. Prev. Chronic Dis. 2013;10:E61. doi: 10.5888/pcd10.120137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez R., Smith P.C., Gostemeyer G., Schwendicke F. Ageing, dental caries and periodontal diseases. J. Clin. Periodontol. 2017;44(Suppl 18):S145–S152. doi: 10.1111/jcpe.12683. [DOI] [PubMed] [Google Scholar]
- Lopez-Otin C., Blasco M.A., Partridge L., Serrano M., Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu B., Liu X., Yang M. A budget proposal for China’s public long-term care policy. J. Aging Soc. Policy. 2017;29:84–103. doi: 10.1080/08959420.2016.1187058. [DOI] [PubMed] [Google Scholar]
- Lu H.X., Tao D.Y., Lo E.C.M., Li R., Wang X., Tai B.J., Hu Y., Lin H.C., Wang B., Si Y., et al. The 4th national oral health survey in the mainland of China: background and methodology. Chin. J. Dent. Res. 2018;21:161–165. doi: 10.3290/j.cjdr.a41079. [DOI] [PubMed] [Google Scholar]
- Luo B., Zhan S. Crossing the river by feeling for the stones: contesting models of marketization and the development of China’s long-term care services. J Chinese Governance. 2018;3:438–460. [Google Scholar]
- Ma X. A comparative study on the needs assessment and rating assessment of long-term care insurance at home and abroad: taking Qingdao and Japan as examples (in Chinese) China Market. 2017;20:60–63. [Google Scholar]
- Ma X., Wang H., Yang L., Shi L., Liu X. Realigning the incentive system for China’s primary healthcare providers. BMJ. 2019;365:l2406. doi: 10.1136/bmj.l2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal A.K., Tagomori G.K., Felix R.V., Howell S.C. Value-based contracting innovated Medicare advantage healthcare delivery and improved survival. Am. J. Manag. Care. 2017;23:e41–e49. [PubMed] [Google Scholar]
- Marten R., McIntyre D., Travassos C., Shishkin S., Longde W., Reddy S., Vega J. An assessment of progress towards universal health coverage in Brazil, Russia, India, China, and South Africa (BRICS) Lancet. 2014;384:2164–2171. doi: 10.1016/S0140-6736(14)60075-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayston R., Lloyd-Sherlock P., Gallardo S., Wang H., Huang Y., Montes de Oca V., Ezeah P., Guerra M., Sosa A.L., Liu Z., et al. A journey without maps-understanding the costs of caring for dependent older people in Nigeria, China, Mexico and Peru. PLoS One. 2017;12 doi: 10.1371/journal.pone.0182360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCAPRC . 2017. The 1st, 2nd 3rd, 4th Circular of the Central Government on Supporting the Pilot Areas of Home-based and Community-based Elderly Care Service Reform. at:http://s.mca.gov.cn/so/s?qt=%E5%B1%85%E5%AE%B6%E5%92%8C%E7%A4%BE%E5%8C%BA%E5%85%BB%E8%80%81%E6%9C%8D%E5%8A%A1%E6%94%B9%E9%9D%A9%E8%AF%95%E7%82%B9&button=+&token=7826&siteCode=bm12000003Ministry of Civil Affairs of the People’s Republic of China. [Google Scholar]
- MCAPRC . 2019. 2018 Annual Statistics Data. 2020 at:http://images3.mca.gov.cn/www2017/file/201908/1565920301578.pdfaccessed on February 9th,Ministry of Civil Affairs of the People’s Republic of China. [Google Scholar]
- MCAPRC . 2019. Suggestions on Further Expanding the Supply and Promoting the Consumption of Elderly Care Services, Accessed at February 9th, 2020 at.http://xxgk.mca.gov.cn:8081/new_gips/contentSearch?id=160822 [Google Scholar]
- Meng Q., Xu L., Zhang Y., Qian J., Cai M., Xin Y., Gao J., Xu K., Boerma J.T., Barber S.L. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379:805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- Meng Q., Mills A., Wang L., Han Q. What can we learn from China’s health system reform? BMJ. 2019;365:l2349. doi: 10.1136/bmj.l2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MHRSSPRC . 2016. The Guiding Opinions on Piloting Long-term Care Insurance Regulations 2016 at.http://www.mohrss.gov.cn/SYrlzyhshbzb/shehuibaozhang/zcwj/yiliao/201607/t20160705_242951.html Ministry of Human Resources and Social Security of the People’s Republic of China. [Google Scholar]
- Morley J.E., Arai H., Cao L., Dong B., Merchant R.A., Vellas B., Visvanathan R., Woo J. Integrated care: enhancing the role of the primary healthcare professional in preventing functional decline: a systematic review. J. Am. Med. Dir. Assoc. 2017;18:489–494. doi: 10.1016/j.jamda.2017.03.015. [DOI] [PubMed] [Google Scholar]
- Nagu T., Ray R., Munseri P., Moshiro C., Shayo G., Kazema R., Mugusi F., Pallangyo K. Tuberculosis among the elderly in Tanzania: disease presentation and initial response to treatment. Int. J. Tuberc. Lung Dis. 2017;21:1251–1257. doi: 10.5588/ijtld.17.0161. [DOI] [PubMed] [Google Scholar]
- NBSC . China Statistics Press; Beijing: 2018. China Statistical Yearbook-2018. [Google Scholar]
- NBSC . National Bureau of Statistics of China; 2019. Statistics Data.http://www.stats.gov.cn/english/ [Google Scholar]
- NDRC . . National Development and Reform Commission; 2016. The Guiding Opinions on Advancing the Development of Age-friendly Livable Environment.http://www.gov.cn/xinwen/2016-11/25/content_5137617.htm 2016, accessed on February 9th, 2020 at: [Google Scholar]
- NHC . the State Council Healthcare Reform Office, National Health and Family Planning commission, National Development Reform Commission; 2016. Opinions on Promoting Contracted Family Doctor Services. 2016.http://www.nhc.gov.cn/tigs/s3577/201606/e3e7d2670a8b4163b1fe8e409c7887af.shtml [Google Scholar]
- NHCPRC . 2019. Healthy China Action Plan (2019–2030) by the National Health Commission of the People’s Republic of China.http://en.nhc.gov.cn/HealthyChinaActionPlan.html) [Google Scholar]
- NHCPRC . National Health Commission of the People’s Republic of China; 2019. Policy Interpretation of Notice on Strengthening Elderly Care Services.http://www.nhc.gov.cn/yzygj/s7652ms/201912/df41796dbb3e47ef854fcdbc97aed3b0.shtml at: [Google Scholar]
- NHCPRC . National Health Commission of the People’s Republic of China; 2019. The State Council Opinions on Promoting the Development of Elderly Care Services 2019.http://www.nhc.gov.cn/lljks/s7785/201911/cf0ad12cb0ec4c96b87704fbbeb5bbde.shtml at: [Google Scholar]
- NHFPC . China Union Medical University Press; 2015. Center for Health Statistics and Information, NHFPC. An Analysis Report of National Health Services Survey in China (Chapter 8) pp. 137–168. [Google Scholar]
- NHFPC . 2017. National Health and Family Planning Commission. National Basic Public Health Services Guideline (third edition) 2017.http://www.nhfpc.gov.cn/ewebeditor/uploadfile/2017/03/20170329103413888.pdf Available from: [Google Scholar]
- NHFPC . 2018. Official paper: Implementation of National Basic Public Health Services in 2018. by the National Health and Family Planning Commission of the People’s Republic of China. [Google Scholar]
- NHSAPRC . National Healthcare Security Administration of the People’s Republic of China; 2019. Reply to Proposal No.3662 (Social Administration 273)http://www.nhsa.gov.cn/art/2019/11/1/art_26_1899.html at: [Google Scholar]
- Nikolich-Zugich J. The twilight of immunity: emerging concepts in aging of the immune system. Nat. Immunol. 2018;19:10–19. doi: 10.1038/s41590-017-0006-x. [DOI] [PubMed] [Google Scholar]
- Ning X.H. Hospice and palliative care in Mainland China: history, current status and challenges. Chin. Med. Sci. J. 2018;33:199–203. doi: 10.24920/003524. [DOI] [PubMed] [Google Scholar]
- Nizami S., Morales C., Hu K., Holzman R., Rapkiewicz A. Trends in mortality from human immunodeficiency virus infection, 1984-2016: an autopsy-based study. Arch. Pathol. Lab. Med. 2019 doi: 10.5858/arpa.2019-0144-OA. [DOI] [PubMed] [Google Scholar]
- O’Meara S. How health research will support China’s ageing population. Nature. 2020;578:S1–S3. doi: 10.1038/d41586-020-00279-y. [DOI] [PubMed] [Google Scholar]
- OECD . OECD Publishing; 2013. Health at a Glance: OECD INDICATORS. Retrieved from. [DOI] [Google Scholar]
- Pallet N., Legendre C. Adverse events associated with mTOR inhibitors. Expert Opin. Drug Saf. 2013;12:177–186. doi: 10.1517/14740338.2013.752814. [DOI] [PubMed] [Google Scholar]
- Pan L., Yang Z., Wu Y., Yin R.X., Liao Y., Wang J., Gao B., Zhang L. The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis. 2016;248:2–9. doi: 10.1016/j.atherosclerosis.2016.02.006. [DOI] [PubMed] [Google Scholar]
- Pei J.J., Giron M.S., Jia J., Wang H.X. Dementia studies in Chinese populations. Neurosci. Bull. 2014;30:207–216. doi: 10.1007/s12264-013-1420-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peng X. China’s demographic history and future challenges. Science. 2011;333:581–587. doi: 10.1126/science.1209396. [DOI] [PubMed] [Google Scholar]
- Petrova V.N., Russell C.A. The evolution of seasonal influenza viruses. Nat. Rev. Microbiol. 2018;16:47–60. doi: 10.1038/nrmicro.2017.118. [DOI] [PubMed] [Google Scholar]
- Poo M.M., Du J.L., Ip N.Y., Xiong Z.Q., Xu B., Tan T. China brain project: basic neuroscience, brain diseases, and brain-inspired computing. Neuron. 2016;92:591–596. doi: 10.1016/j.neuron.2016.10.050. [DOI] [PubMed] [Google Scholar]
- PRC . 2019. The Chinese Government: Healthy China 2030 Plan.http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm [Google Scholar]
- Prince M., Acosta D., Ferri C.P., Guerra M., Huang Y., Llibre Rodriguez J.J., Salas A., Sosa A.L., Williams J.D., Dewey M.E., et al. Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: a 10/66 Dementia Research Group population-based cohort study. Lancet. 2012;380:50–58. doi: 10.1016/S0140-6736(12)60399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putin E., Mamoshina P., Aliper A., Korzinkin M., Moskalev A., Kolosov A., Ostrovskiy A., Cantor C., Vijg J., Zhavoronkov A. Deep biomarkers of human aging: application of deep neural networks to biomarker development. Aging (Albany NY) 2016;8:1021–1033. doi: 10.18632/aging.100968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi G., Pang Y. A survey of AIDS cognitive attitudes among middle-aged and elderly men in high-risk areas. Chinese Journal of Gerontology. 2012;32:784–785. [Google Scholar]
- Qiao X. Why is old-care industry unable to be prosperous? (in chinese) Social Policy Research. 2019;2:7–21. [Google Scholar]
- Rajagopalan S. Tuberculosis and aging_ a global health problem. Clin. Infect. Dis. 2001;33:1034–1039. doi: 10.1086/322671. [DOI] [PubMed] [Google Scholar]
- Rizzuto D., Fratiglioni L. Lifestyle factors related to mortality and survival: a mini-review. Gerontology. 2014;60:327–335. doi: 10.1159/000356771. [DOI] [PubMed] [Google Scholar]
- Rooks D., Roubenoff R. Development of pharmacotherapies for the treatment of Sarcopenia. J. Frailty Aging. 2019;8:120–130. doi: 10.14283/jfa.2019.11. [DOI] [PubMed] [Google Scholar]
- Schmid T., Brandt M., Haberkern K. Gendered support to older parents: do welfare states matter? Eur. J. Ageing. 2012;9:39–50. doi: 10.1007/s10433-011-0197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebastiani P., Thyagarajan B., Sun F., Schupf N., Newman A.B., Montano M., Perls T.T. Biomarker signatures of aging. Aging Cell. 2017;16:329–338. doi: 10.1111/acel.12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao X.H., Yang Y.M., Zhu J., Zhang H., Liu Y., Gao X., Yu L.T., Liu L.S., Zhao L., Yu P.F., et al. Comparison of the clinical features and outcomes in two age-groups of elderly patients with atrial fibrillation. Clin. Interv. Aging. 2014;9:1335–1342. doi: 10.2147/CIA.S67123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si Y., Tai B.J., Hu D.Y., Lin H.C., Wang B., Wang C.X., Zheng S.G., Liu X.N., Rong W.S., Wang W.J., et al. Oral health status of Chinese residents and suggestions for prevention and treatment strategies. Glob. Health Gov. 2019;3:50–54. [Google Scholar]
- Stevens W., Peneva D., Li J.Z., Liu L.Z., Liu G., Gao R., Lakdawalla D.N. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv. Res. 2016;16:175. doi: 10.1186/s12913-016-1420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su M., Zhang Q., Bai X., Wu C., Li Y., Mossialos E., Mensah G.A., Masoudi F.A., Lu J., Li X., et al. Availability, cost, and prescription patterns of antihypertensive medications in primary healthcare in China: a nationwide cross-sectional survey. Lancet. 2017;390:2559–2568. doi: 10.1016/S0140-6736(17)32476-5. [DOI] [PubMed] [Google Scholar]
- Swinkels J.C., Suanet B., Deeg D.J.H., Broese van Groenou M.I. Trends in the informal and formal home-care use of older adults in the Netherlands between 1992 and 2012. Ageing Soc. 2016;36:1870–1890. [Google Scholar]
- Szebehely M., Meagher G. Nordic eldercare: Weak universalism becoming weaker? J. Eur. Soc. Policy. 2018;28:294–308. [Google Scholar]
- Tang Y.D., Wang W., Yang M., Zhang K., Chen J., Qiao S., Yan H., Wu Y., Huang X., Xu B., et al. Randomized Comparisons of Double-Dose Clopidogrel or Adjunctive Cilostazol Versus Standard Dual Antiplatelet in Patients With High Posttreatment Platelet Reactivity: Results of the CREATIVE Trial. Circulation. 2018;137:2231–2245. doi: 10.1161/CIRCULATIONAHA.117.030190. [DOI] [PubMed] [Google Scholar]
- Threapleton D.E., Chung R.Y., Wong S.Y.S., Wong E., Chau P., Woo J., Chung V.C.H., Yeoh E.K. Integrated care for older populations and its implementation facilitators and barriers: a rapid scoping review. Int J Qual Healthcare. 2017;29:327–334. doi: 10.1093/intqhc/mzx041. [DOI] [PubMed] [Google Scholar]
- THT_UK . Terrence Higgins Trust; 2018. Still Got It: Sexual Health of the Over 50s (PDF.https://www.tht.org.uk/sites/default/files/2018-04/Still%20Got%20It%20-%20Over%2050s%20Insight%20Briefing.pdf) [Google Scholar]
- Tinetti M.E., Fried T.R., Boyd C.M. Designing healthcare for the most common chronic condition--multimorbidity. JAMA. 2012;307:2493–2494. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonetti M.S., Bottenberg P., Conrads G., Eickholz P., Heasman P., Huysmans M.C., Lopez R., Madianos P., Muller F., Needleman I., et al. Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing - Consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J. Clin. Periodontol. 2017;44(Suppl 18):S135–S144. doi: 10.1111/jcpe.12681. [DOI] [PubMed] [Google Scholar]
- Toth P.P., Potter D., Ming E.E. Prevalence of lipid abnormalities in the United States: the national health and nutrition examination survey 2003-2006. J. Clin. Lipidol. 2012;6:325–330. doi: 10.1016/j.jacl.2012.05.002. [DOI] [PubMed] [Google Scholar]
- Trammell S.A., Yu L., Redpath P., Migaud M.E., Brenner C. Nicotinamide riboside is a major NAD+ precursor vitamin in cow milk. J. Nutr. 2016;146:957–963. doi: 10.3945/jn.116.230078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsoi K.K., Hirai H.W., Chan F.C., Griffiths S., Sung J.J. Cancer burden with ageing population in urban regions in China: projection on cancer registry data from World Health Organization. Br. Med. Bull. 2017;121:83–94. doi: 10.1093/bmb/ldw050. [DOI] [PubMed] [Google Scholar]
- Tulva T., Wu J., Medar M., Bugarszki Z., Saia K., Kriisk K., Wilken J.-P., Tabur H. Promising community-based practices to postpone the need for institutional elderly care: A descriptive study of community developers in Estonia. East-West Studies. Journal of Social Sciences of Tallinn University School of Governance. Law and Society. 2016:116–125. [Google Scholar]
- Venjatraman J.T., Fernandes G. Exercise, immunity and aging. Aging (Milano) 1997;9:42–56. doi: 10.1007/BF03340127. [DOI] [PubMed] [Google Scholar]
- Venketaraman V., Kaushal D., Saviola B. Mycobacterium tuberculosis. J. Immunol. Res. 2015;2015 doi: 10.1155/2015/857598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbakel E., Tamlagsronning S., Winstone L., Fjaer E.L., Eikemo T.A. Informal care in Europe: findings from the European Social Survey (2014) special module on the social determinants of health. Eur. J. Public Health. 2017;27:90–95. doi: 10.1093/eurpub/ckw229. [DOI] [PubMed] [Google Scholar]
- Vincent W., Fang X., Calabrese S.K., Heckman T.G., Sikkema K.J., Hansen N.B. HIV-related shame and health-related quality of life among older, HIV-positive adults. J. Behav. Med. 2017;40:434–444. doi: 10.1007/s10865-016-9812-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Ni D. Epidemiological characteristics of legally reported sexually transmitted diseases in China from 2004 to 2007. Disease Surveillance. 2008;23:481–483. [Google Scholar]
- Wang Y.N., Song X. International development of integrated care systems (In Chinese) Chinese Nursing Management. 2019;19:161–164. [Google Scholar]
- Wang J., Wang P., Wang X., Zheng Y., Xiao Y. Use and prescription of antibiotics in primary healthcare settings in China. JAMA Intern. Med. 2014;174:1914–1920. doi: 10.1001/jamainternmed.2014.5214. [DOI] [PubMed] [Google Scholar]
- Wang L., Gao P., Zhang M., Huang Z., Zhang D., Deng Q., Li Y., Zhao Z., Qin X., Jin D., et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. Jama. 2017;317:2515–2523. doi: 10.1001/jama.2017.7596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Hai S., Liu Y., Cao L., Liu Y., Liu P., Zhou J., Yang Y., Dong B. Association between depressive symptoms and sarcopenia in older Chinese community-dwelling individuals. Clin. Interv. Aging. 2018;13:1605–1611. doi: 10.2147/CIA.S173146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Sun X., Birch S., Gong F., Valentijn P., Chen L., Zhang Y., Huang Y., Yang H. People-centred integrated care in urban China. Bull. World Health Organ. 2018;96:843–852. doi: 10.2471/BLT.18.214908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Chen Z., Zhang L., Wang X., Hao G., Zhang Z., Shao L., Tian Y., Dong Y., Zheng C., et al. Status of hypertension in China: results from the china hypertension survey, 2012-2015. Circulation. 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- Wang J., Knol M.J., Tiulpin A., Dubost F., de Bruijne M., Vernooij M.W., Adams H.H.H., Ikram M.A., Niessen W.J., Roshchupkin G.V. Gray matter age prediction as a biomarker for risk of dementia. Proc Natl Acad Sci U S A. 2019;116:21213–21218. doi: 10.1073/pnas.1902376116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L.M., Chen Z.H., Zhang M., Zhao Z.P., Huang Z.J., Zhang X., Li C., Guan Y.Q., Wang X., Wang Z.H., et al. [Study of the prevalence and disease burden of chronic disease in the elderly in China] Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:277–283. doi: 10.3760/cma.j.issn.0254-6450.2019.03.005. [DOI] [PubMed] [Google Scholar]
- Wang R., Chen Z., Zhou Y., Shen L., Zhang Z., Wu X. Melancholy or mahjong? Diversity, frequency, type, and rural-urban divide of social participation and depression in middle- and old-aged Chinese: A fixed-effects analysis. Soc Sci Med. 2019;238 doi: 10.1016/j.socscimed.2019.112518. [DOI] [PubMed] [Google Scholar]
- Wang X., Sun G., Feng T., Zhang J., Huang X., Wang T., Xie Z., Chu X., Yang J., Wang H., et al. Sodium oligomannate therapeutically remodels gut microbiota and suppresses gut bacterial amino acids-shaped neuroinflammation to inhibit Alzheimer’s disease progression. Cell Res. 2019;29:787–803. doi: 10.1038/s41422-019-0216-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WBWHO . 2019. World Bank and World Health Organization. Healthy China: Deepening Health Reform in China: Building High-quality and Value-based Service Delivery.http://documents.worldbank.org/curated/en/690791553844042874/pdf/Building-High-Quality-and-Value-Based-Service-Delivery.pdf Available from: [Google Scholar]
- Wei H., Yan Y., Gong J., Dong J. Prevalence of kidney damage in Chinese elderly: a large-scale population-based study. BMC Nephrol. 2019;20:341. doi: 10.1186/s12882-019-1525-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2012. Control SMCfD, Prevention. Study on Global AGEing and Adult Health (SAGE) Wave 1: China National Report. [Google Scholar]
- WHO . World Health Organization; Geneva: 2014. Global Burden of Disease Estimates for 2000-2012. [Google Scholar]
- WHO . World Health Organization; Geneva: 2015. China Country Assessment Report on Ageing and Health. [Google Scholar]
- WHO . 2015. China country assessment report on ageing and health. [Google Scholar]
- WHO . 2015. World Report on Ageing and Health 2015.https://www.who.int/ageing/events/world-report-2015-launch/en/ [Google Scholar]
- WHO . World Health Organization; Geneva: 2015. World Report on Ageing and Health. [Google Scholar]
- WHO . World Health Organization; 2016. WHO Definition of Palliative Care.http://www.who.int/cancer/palliative/definition/en/ [Google Scholar]
- WHO . 2016. WHO Guidelines on Tuberculosis.http://www.who.int/publications/guidelines/tuberculosis/en/) [Google Scholar]
- WHO . 2017. Intergared Care for Older People ICOPE.https://www.who.int/ageing/health-systems/icope/en/ [Google Scholar]
- WHO . World Health Organization; 2018. Epidemiological Estimates for Viral Hepatitis in the Western Pacific.https://www.who.int/westernpacific/health-topics/hepatitis/regional-hepatitis-data) [Google Scholar]
- WHO . 2019. Global Tuberculosis Report 2019.https://www.who.int/tb/publications/global_report/en/) [Google Scholar]
- WHO . 2019. The ICOPE Package of Tools Downloadable at.https://www.who.int/ageing/health-systems/icope/en/ [Google Scholar]
- WHO . World Health Organization; Geneva: 2019. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines.https://www.who.int/mental_health/neurology/dementia/guidelines_risk_reduction/en/) [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2019. WHO Report on the Global Tobacco Epidemic, 2019: Offer Help to Quit Tobacco Use. [Google Scholar]
- WHO Intergared Care for Older People ICOPE. https://www.who.int/ageing/health-systems/icope/en/
- Wieser D., Papatheodorou I., Ziehm M., Thornton J.M. Computational biology for ageing. Philos. Trans. R. Soc. Lond., B, Biol. Sci. 2011;366:51–63. doi: 10.1098/rstb.2010.0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winer B.Y., Huang T.S., Pludwinski E., Heller B., Wojcik F., Lipkowitz G.E., Parekh A., Cho C., Shrirao A., Muir T.W., et al. Long-term hepatitis B infection in a scalable hepatic co-culture system. Nat. Commun. 2017;8:125. doi: 10.1038/s41467-017-00200-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong W.C., Lau H.P., Kwok C.F., Leung Y.M., Chan M.Y., Chan W.M., Cheung S.L. The well-being of community-dwelling near-centenarians and centenarians in Hong Kong: a qualitative study. BMC Geriatr. 2014;14:63. doi: 10.1186/1471-2318-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong C.M., Lai H.K., Tsang H., Thach T.Q., Thomas G.N., Lam K.B., Chan K.P., Yang L., Lau A.K., Ayres J.G., et al. Satellite-based estimates of long-term exposure to fine particles and association with mortality in elderly Hong Kong residents. Environ. Health Perspect. 2015;123:1167–1172. doi: 10.1289/ehp.1408264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J. Challenges of population ageing: putting frailty as a cornerstone of health and social care systems. Eur. Geriatr. Med. 2018;9:273–276. doi: 10.1007/s41999-018-0056-0. [DOI] [PubMed] [Google Scholar]
- Woo J. Combating frailty and sarcopenia in aging populations: switching to a more positive paradigm. Aging Med. 2019;2:7–10. doi: 10.1002/agm2.12052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Chau P.H., Mak B. In: Aging in Hong Kong: A Comparative Perspective, International Perspectives on Aging 5. Powerll J.L., Chen Sheying, editors. Springer Science+Business Media; New York: 2013. Elder-Friendly service delivery models; pp. 211–233. [Google Scholar]
- Woo J., Leung J., Morley J.E. Validating the SARC-F: a suitable community screening tool for sarcopenia? J. Am. Med. Dir. Assoc. 2014;15:630–634. doi: 10.1016/j.jamda.2014.04.021. [DOI] [PubMed] [Google Scholar]
- Woo J., Yu R., Tang N., Leung J. Telomere length is associated with decline in grip strength in older persons aged 65 years and over. Age. 2014;36:9711. doi: 10.1007/s11357-014-9711-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo J., Leung J., Morley J.E. Defining sarcopenia in terms of incident adverse outcomes. J. Am. Med. Dir. Assoc. 2015;16:247–252. doi: 10.1016/j.jamda.2014.11.013. [DOI] [PubMed] [Google Scholar]
- Woo J., Yu R., Wong M., Yeung F., Wong M., Lum C. Frailty screening in the community using the FRAIL scale. J. Am. Med. Dir. Assoc. 2015;16:412–419. doi: 10.1016/j.jamda.2015.01.087. [DOI] [PubMed] [Google Scholar]
- World Health Organization . WHO; Geneva, Switzerland: 2002. Active Ageing: A Policy Framework. [PubMed] [Google Scholar]
- Wu G. Progress of intervention work for high-risk groups in 2018 and work requirements for 2019. Chongqing 2018 High-Risk Population Intervention Work Progress Conference (PeiLing) 2019 [Google Scholar]
- Wu J., Varnik A., Tooding L.M., Varnik P., Kasearu K. Suicide among older people in relation to their subjective and objective well-being in different European regions. Eur. J. Ageing. 2014;11:131–140. doi: 10.1007/s10433-013-0297-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J., Kasearu K., Värnik A., Tooding L.M., Trommsdorff G. Associations between quality of relationships and life satisfaction of older mothers in Estonia, Germany, Russia and China. Ageing Soc. 2016;36:1272–1294. [Google Scholar]
- Wu Y., Dong G., Xiao W., Xiao E., Miao F., Syverson A., Missaghian N., Vafa R., Cabrera-Ortega A.A., Rossa C., Jr., et al. Effect of aging on periodontal inflammation, microbial colonization, and disease susceptibility. J. Dent. Res. 2016;95:460–466. doi: 10.1177/0022034515625962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C., Smit E., Xue Q.L., Odden M.C. Prevalence and correlates of frailty among community-dwelling chinese older adults: the china health and retirement longitudinal study. J. Gerontol. A Biol. Sci. Med. Sci. 2017;73:102–108. doi: 10.1093/gerona/glx098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J., Li X., Yan S. Suicide prevention in old age in China 2002-2017: the linkage to the MIPAA. International Journal on Ageing in Developing Countries. 2018;3:60–68. [Google Scholar]
- Wu Y.T., Ali G.C., Guerchet M., Prina A.M., Chan K.Y., Prince M., Brayne C. Prevalence of dementia in mainland China, Hong Kong and Taiwan: an updated systematic review and meta-analysis. Int. J. Epidemiol. 2018;47:709–719. doi: 10.1093/ije/dyy007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao J., Chow K.M., Chan C.W., Li M., Deng Y. Qualitative study on perceived dignity of cancer patients undergoing chemotherapy in China. Support. Care Cancer. 2019 doi: 10.1007/s00520-019-05123-2. [DOI] [PubMed] [Google Scholar]
- Xing J., Li Y.G., Tang W., Guo W., Ding Z., Ding G., Wang L., Qin Q., Xu Y., Qian S., et al. HIV/AIDS epidemic among older adults in China during 2005-2012: results from trend and spatial analysis. Clin. Infect. Dis. 2014;59:e53–e60. doi: 10.1093/cid/ciu214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Mills A. 10 years of China’s comprehensive health reform: a systems perspective. Health Policy Plan. 2019;34:403–406. doi: 10.1093/heapol/czz026. [DOI] [PubMed] [Google Scholar]
- Xu M., Pirtskhalava T., Farr J.N., Weigand B.M., Palmer A.K., Weivoda M.M., Inman C.L., Ogrodnik M.B., Hachfeld C.M., Fraser D.G., et al. Senolytics improve physical function and increase lifespan in old age. Nat. Med. 2018;24:1246–1256. doi: 10.1038/s41591-018-0092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W., Li Y.X., Wu C. Incidence of frailty among community-dwelling older adults: a nationally representative profile in China. BMC Geriatr. 2019;19:378. doi: 10.1186/s12877-019-1393-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu M., Cheng M., Gao X., Wu H., Ding M., Zhang C., Wang X., Feng X., Tai B., Hu D., et al. Factors associated with oral health service utilization among adults and older adults in China, 2015-2016. Community Dent. Oral Epidemiol. 2020;48:32–41. doi: 10.1111/cdoe.12497. [DOI] [PubMed] [Google Scholar]
- Xu W., Chen T., Cai Y., Hu Y., Fang L., Wu C. Sarcopenia in community-dwelling oldest old is associated with disability and poor physical function. The journal of nutrition, health & aging. 2020 doi: 10.1007/s12603-020-1325-4. in press) [DOI] [PubMed] [Google Scholar]
- Xue M., Xu W., Ou Y.N., Cao X.P., Tan M.S., Tan L., Yu J.T. Diabetes mellitus and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 144 prospective studies. Ageing Res. Rev. 2019;55 doi: 10.1016/j.arr.2019.100944. [DOI] [PubMed] [Google Scholar]
- XWHOSP . 2017. China National Geriatrics Clinical Medical Research Center- Clinical and Scientific Research Collaboration Alliance Established in Beijing (In Chinese) at.https://www.xwhosp.com.cn/Html/News/Articles/10008122.html [Google Scholar]
- XWHOSP . 2017. Opening of the National Clinical Research Center for Geriatric Disorders (Xuanwu Hospital site) at.https://www.xwhosp.com.cn/Html/News/Articles/10008012.html in Chinese by Xuanwu Hospital, Capital Medical University. [Google Scholar]
- XWHOSP . 2019. Introduciton of the National Clinical Research Center for Geriatric Disorders at.https://www.xwhosp.com.cn/Html/Mobile/Articles/10009426.html in Chinese, from Xuanwu Hospital, Capital Medical University. [Google Scholar]
- Yang S., Yan E. Demographic and psychosocial correlates of sexual activity in older Chinese people. J. Clin. Nurs. 2016;25:672–681. doi: 10.1111/jocn.12998. [DOI] [PubMed] [Google Scholar]
- Yang Y.M., Shao X.H., Zhu J., Zhang H., Liu Y., Gao X., Liu L.S., Yu L.T., Zhao L., Yu P.F., et al. Risk factors and incidence of stroke and MACE in Chinese atrial fibrillation patients presenting to emergency departments: a national wide database analysis. Int. J. Cardiol. 2014;173:242–247. doi: 10.1016/j.ijcard.2014.02.040. [DOI] [PubMed] [Google Scholar]
- Yang W., Jingwei He A., Fang L., Mossialos E. Financing institutional long-term care for the elderly in China: a policy evaluation of new models. Health Policy Plan. 2016;31:1391–1401. doi: 10.1093/heapol/czw081. [DOI] [PubMed] [Google Scholar]
- Yang X., Lupon J., Vidan M.T., Ferguson C., Gastelurrutia P., Newton P.J., Macdonald P.S., Bueno H., Bayes-Genis A., Woo J., et al. Impact of Frailty on Mortality and Hospitalization in Chronic Heart Failure: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.008251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao S.S., Cao G.Y., Han L., Chen Z.S., Huang Z.T., Gong P., Hu Y., Xu B. Prevalence and patterns of multimorbidity in a nationally representative sample of older Chinese: results from CHARLS. J. Gerontol. A Biol. Sci. Med. Sci. 2019 doi: 10.1093/gerona/glz185. [DOI] [PubMed] [Google Scholar]
- Yeoh E.K., Lai A.H.Y. Hong Kong: Our Hong Kong Foundation; 2016. An Investment for the Celebration of Aging.https://www.ourhkfoundation.org.hk/sites/default/files/media/pdf/OHKF_20161206_Aging_eng.pdf [Google Scholar]
- Yip W.C., Hsiao W.C., Chen W., Hu S., Ma J., Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379:833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- Yip W., Fu H., Chen A.T., Zhai T., Jian W., Xu R., Pan J., Hu M., Zhou Z., Chen Q., et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet. 2019;394:1192–1204. doi: 10.1016/S0140-6736(19)32136-1. [DOI] [PubMed] [Google Scholar]
- Yoshino J., Baur J.A., Imai S.I. NAD(+) intermediates: the biology and therapeutic potential of NMN and NR. Cell Metab. 2018;27:513–528. doi: 10.1016/j.cmet.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu J., Li J., Cuijpers P., Wu S., Wu Z. Prevalence and correlates of depressive symptoms in Chinese older adults: a population-based study. Int. J. Geriatr. Psychiatry. 2012;27:305–312. doi: 10.1002/gps.2721. [DOI] [PubMed] [Google Scholar]
- Yu R., Leung J., Woo J. Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: results from the Osteoporotic Fractures in Men (MrOs) Study. J. Am. Med. Dir. Assoc. 2014;15:551–558. doi: 10.1016/j.jamda.2014.02.005. [DOI] [PubMed] [Google Scholar]
- Yu R., Wu W.C., Leung J., Hu S.C., Woo J. Frailty and its contributory factors in older adults: a comparison of two asian regions (Hong Kong and Taiwan) Int. J. Environ. Res. Public Health. 2017;14 doi: 10.3390/ijerph14101096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu P., Liu X., Wang J. Geriatric medicine in China: the past, present, and future. Aging Med (Milton) 2018;1:46–49. doi: 10.1002/agm2.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu R., Wong M., Chong K.C., Chang B., Lum C.M., Auyeung T.W., Lee J., Lee R., Woo J. Trajectories of frailty among Chinese older people in Hong Kong between 2001 and 2012: an age-period-cohort analysis. Age Ageing. 2018;47:254–261. doi: 10.1093/ageing/afx170. [DOI] [PubMed] [Google Scholar]
- Yu R.B., Wang D., Leung J., Lau K., Kwok T., Woo J. Is neighborhood green space associated with less frailty? Evidence from the Mr. And ms. Os (Hong Kong) Study. J Am Med Dir Assoc. 2018;19:528–534. doi: 10.1016/j.jamda.2017.12.015. [DOI] [PubMed] [Google Scholar]
- Yu R., Leung J., Lum C.M., Auyeung T.W., Lee J.S.W., Lee R., Woo J. A comparison of health expectancies over 10 years: implications for elderly service needs in Hong Kong. Int. J. Public Health. 2019;64:731–742. doi: 10.1007/s00038-019-01240-1. [DOI] [PubMed] [Google Scholar]
- Yu, R., Tong, C., Ho, F., and Woo, J. (in press). Effects of a multi-component frailty prevention program in pre-frail community-dwelling older persons: A randomized controlled trial. J Am Med Dir Assoc. [DOI] [PubMed]
- Yuan J., Zhang Z., Wen H., Hong X., Hong Z., Qu Q., Tang M., Wu J., Xu Q., Li H., et al. Incidence of dementia and subtypes: a cohort study in four regions in China. Alzheimers Dement. 2016;12:262–271. doi: 10.1016/j.jalz.2015.02.011. [DOI] [PubMed] [Google Scholar]
- Yue X., Gong X., Li J., Teng F., Jiang N., Men P., Wang J., Wang Y., Chen X., Gu H. Epidemiological characteristics of condyloma acuminata in China’s STD surveillance sites from 2008 to 2016. Chinese Journal of Dermatology. 2017;50:321–325. [Google Scholar]
- Zeng Y., Feng Q., Gu D., Vaupel J.W. Demographics, phenotypic health characteristics and genetic analysis of centenarians in China. Mech. Ageing Dev. 2017;165:86–97. doi: 10.1016/j.mad.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y., Feng Q., Hesketh T., Christensen K., Vaupel J.W. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet. 2017;389:1619–1629. doi: 10.1016/S0140-6736(17)30548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhan Q., Shang S., Li W., Chen L. Bridging the GP gap: nurse practitioners in China. Lancet. 2019;394:1125–1127. doi: 10.1016/S0140-6736(19)32209-3. [DOI] [PubMed] [Google Scholar]
- Zhang B., Li J. Gender and marital status differences in depressive symptoms among elderly adults: the roles of family support and friend support. Aging Ment. Health. 2011;15:844–854. doi: 10.1080/13607863.2011.569481. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Xu Y., Shang L., Rao K. An investigation into health informatics and related standards in China. Int. J. Med. Inform. 2007;76:614–620. doi: 10.1016/j.ijmedinf.2006.05.003. [DOI] [PubMed] [Google Scholar]
- Zhang H., Yang Y., Zhu J., Shao X., Liu Y., Zhao L., Yu P., Zhang H., He Q., Gu X. Baseline characteristics and management of patients with atrial fibrillation/flutter in the emergency department: results of a prospective, multicentre registry in China. Intern. Med. J. 2014;44:742–748. doi: 10.1111/imj.12487. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Zhang J., Butler J., Yang X., Xie P., Guo D., Wei T., Yu J., Wu Z., Gao Y., et al. Contemporary epidemiology, management, and outcomes of patients hospitalized for heart failure in China: results from the china heart failure (China-HF) registry. J. Card. Fail. 2017;23:868–875. doi: 10.1016/j.cardfail.2017.09.014. [DOI] [PubMed] [Google Scholar]
- Zhang C.Y., Zhao F., Xia Y.Y., Yu Y.L., Shen X., Lu W., Wang X.M., Xing J., Ye J.J., Li J.W., et al. Prevalence and risk factors of active pulmonary tuberculosis among elderly people in China: a population based cross-sectional study. Infect. Dis. Poverty. 2019;8:7. doi: 10.1186/s40249-019-0515-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang P., Kishimoto Y., Grammatikakis I., Gottimukkala K., Cutler R.G., Zhang S., Abdelmohsen K., Bohr V.A., Misra Sen J., Gorospe M., et al. Senolytic therapy alleviates Abeta-associated oligodendrocyte progenitor cell senescence and cognitive deficits in an Alzheimer’s disease model. Nat. Neurosci. 2019;22:719–728. doi: 10.1038/s41593-019-0372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao G., Zhou M., Ma C., Huo Y., Smith S.C., Jr., Fonarow G.C., Ge J., Han Y., Liu J., Hao Y., et al. In-hospital outcomes of dual loading antiplatelet therapy in patients 75 years and older with acute coronary syndrome undergoing percutaneous coronary intervention: findings from the CCC-ACS (Improving care for cardiovascular disease in china-acute coronary syndrome) project. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.117.008100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao R., Xu K., Li Y., Qiu M., Han Y. Percutaneous coronary intervention in patients with acute coronary syndrome in Chinese Military Hospitals, 2011-2014: a retrospective observational study of a national registry. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2018-023133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao D., Liu J., Wang M., Zhang X., Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat. Rev. Cardiol. 2019;16:203–212. doi: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- Zhou M., Wang H., Zeng X., Yin P., Zhu J., Chen W., Li X., Wang L., Wang L., Liu Y., et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394:1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Osterle A. China’s policy experimentation on long-term care insurance: implications for access. Int. J. Health Plann. Manage. 2019;34:e1661–e1674. doi: 10.1002/hpm.2879. [DOI] [PubMed] [Google Scholar]
- Zhu B., Wang Y., Ming J., Chen W., Zhang L. Disease burden of COPD in China: a systematic review. Int. J. Chron. Obstruct. Pulmon. Dis. 2018;13:1353–1364. doi: 10.2147/COPD.S161555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L.Y., Chan R., Kwok T., Cheng K.C., Ha A., Woo J. Effects of exercise and nutrition supplementation in community-dwelling older Chinese people with sarcopenia: a randomized controlled trial. Age Ageing. 2019;48:220–228. doi: 10.1093/ageing/afy179. [DOI] [PubMed] [Google Scholar]