Abstract
The objective of this study is to investigate musculoskeletal complaints (MSCs) in healthcare workers (HCWs) in 3 community hospital–based departments [internal medicine (IM), general surgery (GS), and emergency department (ED)] and its effects on the quality of work life (QWL) of hospital HCW.
This prospective cross-sectional study was performed in the 700-bed community training hospital. All HCW staffed in 3 departments (IM, GS, ED) of the hospital were asked to respond to items in the study data sheet. Enrolled personnel were inquired about their demographic data, work history and schedule, and medical history. The 16-item Cornell Musculoskeletal Discomfort Questionnaire (CMDQ) Turkish version was applied to evaluate MSC. A total of 216 HCW constituted the study sample and demographic characteristics, history, and clinical findings were analyzed.
Among all, 103 personnel (47.7%) were women (n = 42, 41.1% in physicians, n = 57, 87.6% in nurses and n = 4, 8% in other HCW) (P = .000). A total of 173 personnel (79.7%) reported MSC in some part of their bodies. Female personnel had MSC significantly more commonly than males (chi-square = 40.7, P = .000). Numbers and percentages of the personnel with MSC in 3 departments (IM, GS, ED) were 51/61, 52/65, and 70/90, respectively (P = .67). Total QWL score of those without MSC was significantly higher than others (74.7 + −12 vs 63.2 + −15, respectively; t test, P = .000). Total frequency score of MSC as elicited via CMDQ was significantly higher in those without MSC compared to the others (8.1 + −7.6 vs 0.1 + −0.6, respectively, t test, P = .000).
Female sex, high-income, university graduation, being a nurse or a physician, and older age impose risk for HCW in hospital with respect to having MSC. Presence of MSC affects QWL negatively.
Keywords: healthcare workers, musculoskeletal complaint, musculoskeletal disorders, occupational disease, quality of work life
1. Introduction
Musculoskeletal disorders (MSDs) comprise inflammatory and degenerative conditions, which may involve muscles, tendons, ligaments, nerves, and bones. These problems are known to cause high costs and impair the quality of life in general. Every fourth person in developed countries are estimated to suffer from chronic pain originating from MSD. These conditions trigger substantial losses of workforce and schooldays resulting in a decrease in productivity which, in turn, afflict the whole society.[1–7]
Despite substantial bulk of research on the subject, health hazards associated with job-related MSD is thought to be a leading cause of workforce losses worldwide.[8]
One major source of injury to healthcare workers (HCWs) is MSDs.[9] Physicians, dentists, nurses, physiotherapists, and other HCW face repetitive trauma and incessant strains in their routine patient care activities, paving the way to chronic illness and musculoskeletal injuries.[10] In this context, Occupational Safety and Health Administration (OSHA) foresaw the hazards arising from this issue and cited that “Patient transfer and lifting devices are key components of an effective program to control the risk of injury to patients and staff associated with lifting, transferring, repositioning or movement of patients”.[9] They also reported that nursing aides, orderlies, and attendants had the highest rates of MSDs among all industries. In 2010, there were 27,020 cases, which equate to an incidence rate of 249 per 10,000 workers, more than 7 times the average for all industries. In Turkey, predefined types of healthcare personnel do not include “nurse assistants” with a medical background and education to help nurses in their work, instead, personnel—that is, those called “other HCW” means other allied health in this study—helps major work such that carrying, lifting patients, etc in the patient care areas. These personnel are generally graduated from secondary education and have undergone some in-service training, without a firm medical background.
Job-related stress is associated with lumbar pain, neck pain, and other forms of occupational MSD.[11] Individuals affected by a combination of physical and psychosocial influences tend to have worse outcomes when compared to those affected either physically or psychosocially alone.[12] Another example is that physiotherapists working actively in long-term caregiving areas have lower stress scores compared to colleagues accepting ambulatory patients.[13] Fatigue is attributed to stress and emotional exhaustion, eventually leading to do the unwanted job constantly.[14,15]
One of the instruments most commonly used to assess MSD suffered by the individual is “Cornell Musculoskeletal Discomfort Questionnaire (CMDQ)” which was firstly devised by Hedge et al.[11] The tool questions the MSD with regard to frequency, severity, and presence or absence of work impairment caused by the disorder. It has diverse forms for both sexes and also those working in ambulatory and sedentary work environments. Erdinc et al[12] have performed the validity and reliability studies for Turkish population and conducted the validity and reliability studies in the native language.
Many researches have been conducted in the field of health sector workers’ quality of life and motivation in the last decades. Major triggers of big numbers of studies include large workloads, needs of the care for the seriously ill, having to render emotional support to the patients and relatives, inadequate infrastructure in healthcare facilities, unequal distribution of workforce, services, and salaries paid to HCW. All these factors contribute frustration and stress on the HCW and affect their quality of work life (QWL) and motivation negatively. Martel and Gilles[16] described QWL as an assessment of work conditions, satisfaction and dissatisfaction of the workers, productivity, social environment in the organization, style of management, and the relationship of the working and out-of-working life; briefly, a general concept comprising strong and weak points of the whole work environment.
Bearfield et al[17] inquired about improving the QWL in a study on 1032 professionals including physicians and nurses in Australia. The workers gave an order of better compensation, better work hours, better management, and gaining appreciation, respectively.
The relationship between variables affecting QWL (i.e., organizational commitment, job involvement, empowerment, and job satisfaction, and turnover rate) and human relations model was investigated on 276 HCW in 7 American hospitals.[18] The study put forth that unit organizational culture does affect nurses’ QWL factors and that human relations cultural values are positively related to organizational commitment, job involvement, empowerment, and job satisfaction, and negatively related to intent to turnover.
QWL was translated and devised in Turkish by Aydın et al[19] on 207 personnel in 2011, because of the lack of such a standard measure to quantify the current status of the HCW's work life in the country. Cronbach's alpha reliability coefficient was calculated as 0.882 for the scale as a whole, and reliability level as 0.924 (very high), which also demonstrated internal consistency.
There is dearth of research exploring the relationship of musculoskeletal complaints (MSCs) and QWL. The objective of this study was to investigate MSC in HCW in a high-volume community hospital-based emergency department (ED) actively taking part in the healthcare, its effects on the QWL in interdepartmental comparison to the colleagues in general surgery (GS), and internal medicine (IM) departments.
2. Materials and methods
This prospective cross-sectional study was performed in the community training hospital, which has a total of 700 beds with an annual volume of 105,000 inpatients. The study protocol was approved by the institutional review board before recruitment of the subjects. Informed consent was obtained from all enrolled HCW. All items in the scale were responded and signed by the HCW themselves.
All HCW staffed in 3 departments (ED, GS, IM) of the hospital were asked to participate in the study. The survey forms were filled in out of the work hours, in a distinct place separated from the active health care in a 7 days’ period. Pregnant personnel, those who have rejected to take part in the study, and who had been on sick leave for longer than 7 days or hospitalized for a treatment were excluded from the study. Separate sheets comprising the scale items were handed to the participant HCW to be filled in and they were asked to answer each question. Demographic characteristics, history, and clinical findings were analyzed.
Enrolled personnel were inquired about their demographic data, work history and schedule (hours spent working on the computer/hours sitting at the table), presence or absence of MSD, any diagnoses received, drugs used, relevant medical history, systemic diseases, and additional symptoms such as perceived stress, sleep disorder, and addictions if any. Then the 16-item CMDQ Turkish version was applied to evaluate MSD status individualized for men and women (Fig. 1). Personnel were asked to mark the painful body area(s) if any, frequency (5-point Likert scale) and severity (3-point Likert scale) of painful episodes, and whether the complaints impair the work life (3-point Likert scale) of the individual. Each body part takes a score between 0 and 90 in accordance with the responses. In addition, the respondents were asked to rate the 16-item “Quality of Work Life Scale” in which each item is organized as seven-point Likert scale—ranging from “Very Untrue” (value of 1) to “Very True” (value of 7).
Figure 1.
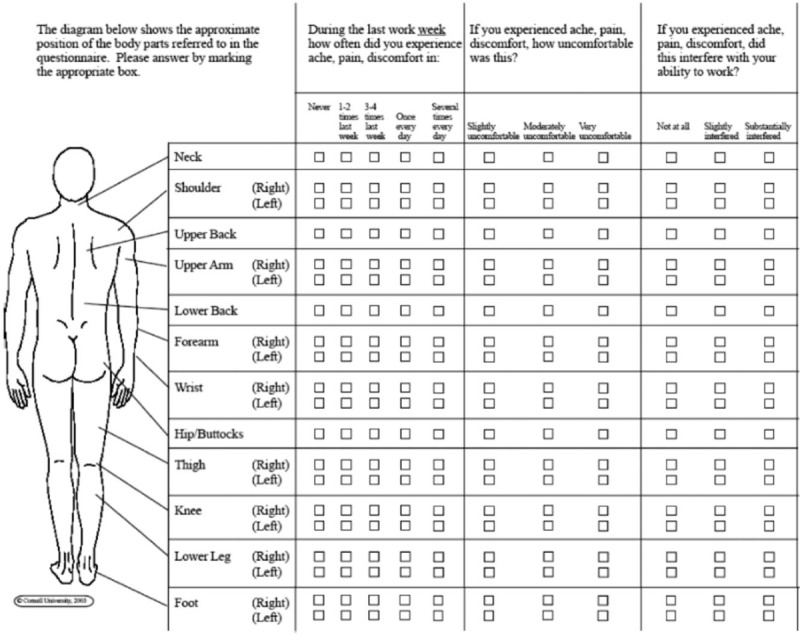
Male version of the Cornell Musculoskeletal Discomfort Questionnaire (CMDQ) used for the present study.
Statistical analysis was performed using the MedCalc Statistical Software version 12.7.7 (MedCalc Software bvba, Ostend, Belgium; http://www.medcalc.org; 2013). The normality of continuous variables was investigated by Shapiro-Wilk's test. Descriptive statistics were presented using mean and standard deviation for normally distributed variables and median (and minimum-maximum) for the non-normally distributed variables. For comparison of 2 normally distributed groups Student t test was used. Nonparametric statistical methods were used for values with skewed distribution. For comparison of 2 non-normally distributed groups Mann Whitney U test was used. The χ2 test was used for categorical variables and expressed as observation counts (and percentages). To investigate the effect of parameters on a dichotomous dependent variable binary logistic regression was used. Statistical significance was accepted when 2-sided P value was <.05.
3. Results
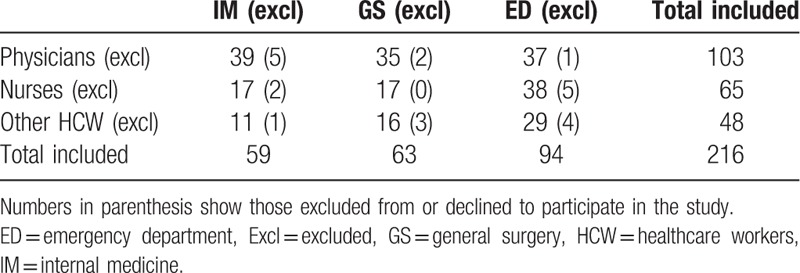
A total of 239 personnel were deemed eligible in 3 departments, and 23 were excluded (6 personnel were pregnant, 3 were on sick leave for longer than 7 days, 4 were on postpartum leave, 7 others declined to participate in the study, and 3 datasheets had major errors precluding evaluation) and therefore, the remaining 216 HCW constituted the study sample (Table 1).
Table 1.
Distribution of personnel with respect to professions and departments.
Mean age of the sample is 33.1 + −8.4 (range: 20 and 57) and the difference between 3 departments is not statistically significant [analysis of variance (ANOVA), P = .474]. Mean height of the personnel is 169.2 cm + −8.5 cm (range: 146 and 195 cm) and the difference between 3 departments is not statistically significant (ANOVA, P = .346). Mean weight of the sample is 69.6 + −13.8 (range: 40 and 106) and the difference between 3 departments was not statistically significant (ANOVA, P = .780). Among all, 103 personnel (47.5%) were women (n = 42, 41.1% in physicians, n = 57, 87.6% in nurses and n = 4, 8% in other HCW) (P = .000).
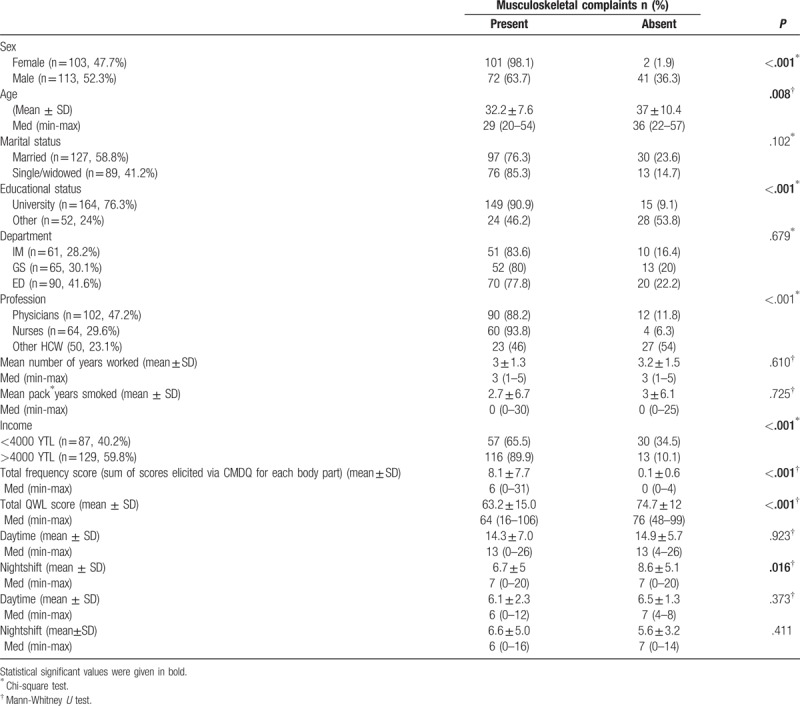
A total of 173 personnel (79.7%) reported MSC in some part of their bodies. Of those, 101 (58.3%) were women. Female personnel had MSC significantly more commonly than male counterparts (Chi-square = 40.7, P = .000). Mean ages of the personnel with and without MSCs were 32.1 + −7.6 and 37.0 + −10.4 respectively (t test, P = .001).
Mean heights of the personnel with and without MSC were 168.8 + −9.2 and 170.6 + −5.4, respectively (t test, P = .24). Mean weights of the personnel with and without MSC were 68.8 + −14.2 and 72.4 + −11.9, respectively (t test, P = .13).
Numbers and percentages of the personnel who reported MSC in 3 departments (IM, GS, ED) were 51/61, 52/65, and 70/91, respectively (Chi-square = 1.014, P = .602).When the personnel's professions were analyzed in relation to the presence of MSC; 90 physicians (88%), 60 nurses (93.7%), and 23 other HCW (46%) reported to have MSC (chi-square = 48.177, P = .000). Mean number of years worked in the profession of the personnel who reported and denied MSC were 3.3 + −1.3 vs 3.1 + −1.5, respectively (t test, P = .52).
Ninety-seven (75.7%) married and 76 (85.3%) single/widowed personnel had MSC (Chi-square = 3.000, P = .089). As far as monthly household income, personnel were assigned to either low (<4000 YTL (Turkish Liras)) or high (≥4000 YTL) income groups. It was calculated that 57 (65.5%) low-income and 116 (89.2%) high-income personnel had MSC; high-income personnel had MSC more commonly than others (chi-square = 18.1, P = .000). All HCW were assigned to either of 2 groups with respect to the educational status: university graduates and high-school or lower grades. A total of 149 (90.3%) university graduates and 24 (46.1%) other personnel had MSC (chi square = 47.6, P = .000).
Mean day-time and nightshift work hours, as well as mean hours spent ambulatory in the day and nightshifts of the personnel with and without MSC are shown in Table 2. Of these, only mean number of nightshift work days a month was found to be significantly related with absence of MSC (t test, P = .027). Mean pack/years of the personnel with and without MSC were statistically similar (Table 2).
Table 2.
Characteristics of the personnel in relation with presence or absence of musculoskeletal complaints.
A sensation of muscle weakness was also present as a complaint in 89 (41%) personnel from the whole sample. Eighty-six (49.7%) personnel out of those with MSC and only 3 (6.8%) of those without MSC reported weakness (chi square, P = .000). The presence of weakness was not affected by the department of HCW (chi square, P = .83). When the personnel's professions were analyzed in relation to the presence of muscle weakness; 41 physicians (40%), 41 nurses (64%), and 7 other HCW (14%) reported to have muscle weakness (chi square = 29.12, P = .000).
Mean total QWL score of those without MSC was significantly higher than others (74.7 + −12 vs 63.2 + −15, respectively; t test, P = .000). Total frequency score of MSC as a sum of scores elicited via CMDQ for each body part was significantly higher in those without MSC compared to the others (8.1 + −7.6 vs 0.1 + −0.6, respectively, t test, P = .000).
As calculated via CMDQ, total severity score of the MSC for those individuals reporting MSC was 6.74 + −6.04 vs 0.11 + −0.62 in those without MSC (t test, P = .000) and total interference with work ability was 2.6 + −3.6 in those with MSC.
MSC related to a specific body region—that is, lower back region—was analyzed. Respecting to the frequency of MSC, a total of 41 patients (18.9%) had MSC in that region at least once a day. Mean total QWL score of those with frequent MSC in their lower back region was lower than others, although not significant statistically (65.9 + −15.8 vs 63.7 + −11.6, P = .41).
Seventy-one (32.7%) personnel described their complaint as of moderate or high severity in the lower back region. Mean total QWL score of those with MSC of moderate and/or high severity in the lower back region was lower than others, although not significant statistically (66.2 + −15.0 vs 64.0 + −15.2, P = .29).
A multiple regression analysis was run to predict total QWL from department worked, age, sex, profession (physician/nurse/other), education status, marital status, monthly income, presence of MSC, total severity scores of MSC, total work inability, and total frequencies of MSC. These variables statistically significantly predicted QWL [F (11, 204) = 6.901, P < .001, R2 = 0.271] and that department worked, education status, monthly income, and presence of MSC added significantly to the prediction of QWL (P < .05).
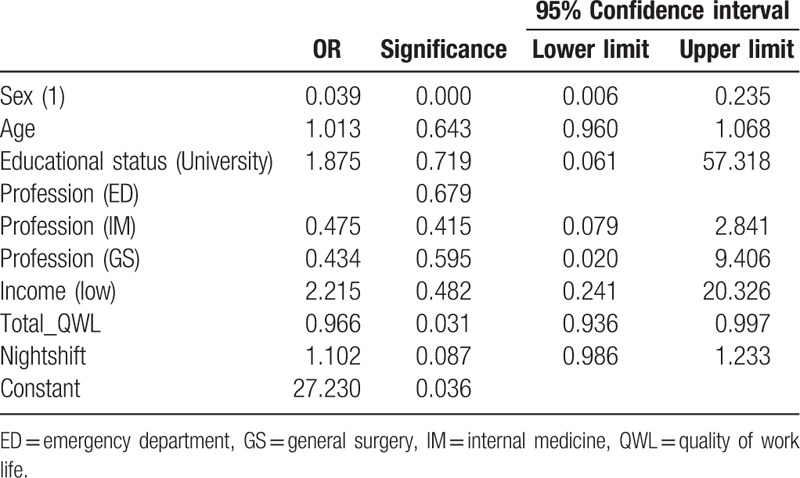
In order to investigate the multivariate effect of parameters (which had statistical significance between groups with positive and negative MS complaints) on dependent variable (MS complaints) binary logistic regression analysis was performed (Table 3). The model was significant (P < .001). According to multivariate logistic regression analysis, sex and the total QWL score had significant impact on MS complaints. Women had 2.56 times more MS complaints than men did in the sample. When the total QWL score increases 1 point, people get 1.04 times less MS complaints.
Table 3.
Multivariate logistic regression analysis.
4. Discussion
This study provides a conceptual framework for the close relationship of well-being of caregivers working in the state-run healthcare sector and QWL reported by themselves. Also, HCW staffed in 3 distinct work environments (IM, GS, ED) were enrolled in the study to help extrapolation of the findings to the sector as a whole with a higher validity and reliability.
QWL is a very broad concept; therefore, there is no one single, clear definition of the entity. As a multidimensional structure, QWL is defined as “a generic phrase that covers a person's feelings about every dimension of work, and a way of thinking about people, work, and organization that involves a concern for employee well-being and organizational effectiveness”,[20] whereas Sirgy et al[21] postulated as “employee satisfaction with a variety of needs through resources, activities, and outcomes stemming from participation in the workplace.” Many researchers revealed that the QWL includes many aspects such as employment conditions, employment security, income adequacy, profit sharing, equity and other rewards, employee autonomy, employee commitment, social interaction, self-esteem, self-expression, democracy, employee satisfaction, employee involvement, advancement, relations with supervisors, and peers and job enrichment. Therefore healthcare needs of the worker cannot be considered a distinct phenomenon from QWL in this context.
Many researchers focused on the question how we can render the work-life and worker more qualified as a vital problem in the last decades, especially in the developed countries.[22–24] So, the QWL is a response both to organizational needs and to workers’ developmental needs, a practice to improve working conditions, and a series of measures. The present study was devised to examine whether QWL differs by the MSC of employees as reported by themselves via a broadly validated tool such as CMDQ and to explore which variables influences the QWL most.
Nearly four-fifth of the participants in the present research reported MSC during the study period. Loghmani et al[25] reported the corresponding figure as 89% in Iran. The findings demonstrated that female sex, high-income, university graduation, being a nurse or a physician, and older age impose risk for having MSC in the healthcare. It is interesting that, working longer in the nightshifts were associated with a lower rate of complaining of MSC among HCW. Further broad-based, well-designed prospective studies would determine whether this finding indicates a significant risk or not. Presence of MSC affected QWL negatively.
A useful tool to diagnose MSD and follow the clinical course after treatment can be ultrasound in most cases. Some well-designed retrospective and prospective researches reported that acquired shoulder disorders can be diagnosed via ultrasound in experienced hands.[26,27] In addition, Chang et al[28] postulated that ultrasound can also be beneficial in the treatment of adults with shoulder pain as a guide for subacromial corticosteroid injections.
In the present study there was a significant negative correlation between pain intensity and job satisfaction. De Jong et al[29] conducted a systematic review of chronic physical diseases of employees with regard to effects on their QWL recently and reported that effect of the disease and treatment including issues about cognitive and physical health and work ability is an important element which influences upon QWL.
Matsudaira et al[30] reported on a substantial variability in regional pain and associated disability between different cultures. For example, incidences of regional pain found in this Japanese study were markedly less than in the UK, with a particularly low prevalence of upper extremity pain among office workers. Findings of the present study also support this phenomenon in that the frequency of lower back pain as an MSC in the present sample was approximately 19%, which is much higher than the findings in Japan.
Afsar[31] reported that out that there is a positive and significant relationship between the QWL and age and gender in Turkey, which was also consistent with the literature.[32–34] These findings may render useful insights to healthcare managers, administrators, and practitioners to design appropriate strategies and interventions to make the working lives of the employees more satisfactory.
There are several limitations of this study. First of all, the sample of this study is consisted of HCW staffed in 3 departments in a single center in the metropol city of Istanbul. In order to extrapolate the findings of the present study to all employees in the whole healthcare sector in Turkey, similar multi-institutional studies focusing on MSC reported by the personnel should be designed.
In conclusion, female sex, high-income, university graduation, working as a nurse or a physician, and older age may demonstrate a greater prevalence of MSC in the hospital HCW. Presence of MSC affects QWL negatively. Based on research results, efforts should be made to highlight MSC affecting the healthcare personnel's QWL and factors that could be improved to mitigate hazards thereof. Further research will broaden our knowledge on the risk for having MSC in the healthcare personnel working in hospital and other related areas.
Author contributions
Conceptualization: Özgür Karcioglu.
Formal analysis: Özgür Karcioglu.
Investigation: Nazmiye Koyuncu.
Methodology: Nazmiye Koyuncu.
Project administration: Nazmiye Koyuncu.
Resources: Nazmiye Koyuncu.
Supervision: Nazmiye Koyuncu.
Validation: Nazmiye Koyuncu.
Visualization: Nazmiye Koyuncu.
Writing – original draft: Özgür Karcioglu.
Writing – review and editing: Özgür Karcioglu.
Özgür Karcioglu orcid: 0000-0002-8814-6164
Ozgur KARCIOGLU orcid: 0000-0002-8814-6164.
Footnotes
Abbreviations: ANOVA = analysis of variance, CMDQ = Cornell Musculoskeletal Discomfort Questionnaire, ED = emergency department, GS = general surgery, HCW = healthcare workers, IM = internal medicine, MSC = musculoskeletal complaints, MSD = musculoskeletal disorder, QWL = quality of work life.
The authors have no conflicts of interest to disclose.
References
- [1].Woolf A, Akesson K. Understanding the burden of musculoskeletal conditions. BMJ 2001;322:1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol 2004;14:13. [DOI] [PubMed] [Google Scholar]
- [3].Smith DR, Wei N, Ishıtake T, et al. Musculoskeletal disorders among Chinese medical students. Kurume Med J 2005;52:139–46. [DOI] [PubMed] [Google Scholar]
- [4].Noack-Cooper KL, Sommerich CM, Mirka GA. College students and computers: assessment of usage patterns and musculoskeletal discomfort. Work 2009;32:285–98. [DOI] [PubMed] [Google Scholar]
- [5].Lorusso A, Vimercati L, L’Abbate##N Musculoskeletal complaints among Italian X ray technology students: a cross-sectional questionnaire survey. BMC Res Notes 2010;3:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Vyas R. Mitigation of musculoskeletal problems and body discomfort of agricultural workers through educational intervention. Work 2012;41:2398–404. [DOI] [PubMed] [Google Scholar]
- [7].Irurhe NK, Okafor UC, Adekola OO, et al. Work related musculoskeletal discomforts (WRMD) in ultrasonologists: prevalence and risk factors. World J MedSci 2013;8:199–204. [Google Scholar]
- [8].Bureau of Labor Statistics News, United States Department of Labor Lost-Worktime Injuries and Illnesses: Characteristics and Resulting Days Away From Work. 2001. Available at: http://www.bls.gov/iif/home.htm. Accessed: December 3, 2017. [Google Scholar]
- [9].Safety and Health Topics: Healthcare. Safe Patient Handling. Occupational Safety and Health Administration. US Department of Labor. Available at: https://www.osha.gov/SLTC/healthcarefacilities/safepatienthandling.html. Accessed: July 23, 2018. [Google Scholar]
- [10].Beynon C, Reilly T. Reilly T. Epidemiology of musculoskeletal disorders in a sample of British nurses and physiotherapists. Musculoskeletal Disorders in Health-Related Occupations. Amsterdam, The Netherlands: IOS Press; 2002. 63–85. [Google Scholar]
- [11].Hedge A, Morimoto S, McCroibe D. Effects of keyboard tray geometry on upper body posture and comfort. Ergonomics 1999;42:1333–49. [DOI] [PubMed] [Google Scholar]
- [12].Erdinc O, Hot K, Ozkaya M. Turkish version of the Cornell Musculoskeletal Discomfort Questionnaire: cross-cultural adaptation and validation. Work 2011;39:251–60. [DOI] [PubMed] [Google Scholar]
- [13].Kuru T, Yeldan I, Zengin A, et al. Erişkinlerde ağrı ve farklı ağrı tedavilerinin prevalansı. Ağrı 2011;23:22–7. [DOI] [PubMed] [Google Scholar]
- [14].Taspinar F, Taspinar B, Cavlak U, et al. Determining the pain-affecting factors of university students with nonspecific low back pain. J Phys Ther Sci 2013;25:1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Shuval K, Donchin M. Prevalence of upper extremity musculoskeletal symptoms and ergonomic risk factors at a Hi-Tech company in Israel. Int J Ind Ergon 2005;6:569. [Google Scholar]
- [16].Martel JP, Gilles D. Quality of work life: theoretical and methodological problems, and presentation of a new model and measuring instrument. Soc Indic Res 2006;77:333–68. [Google Scholar]
- [17].Bearfield S. Quality of working life: comparing the perceptions of professionals and clerical sales and service workers. 2003. Available at: https://ses.library.usyd.edu.au/bitstream/2123/13413/1/WP86.pdf. Accessed: December 3, 2017. [Google Scholar]
- [18].Gifford BD, Zammuto RF, Goodman EA, et al. The relationship between hospital unit culture and nurses’ quality of work life. J Healthc Manag 2002;47:13–25. discussion 25–26. [PubMed] [Google Scholar]
- [19].Aydın I, Celik Y, Uğurluoğlu O. Quality of work life scale for healthcare personnel: development, validity and reliability. Publication of Social Work Department Faculty of Economics and Administrative Sciences, Hacettepe University. 2011;22:79–100. [Google Scholar]
- [20].Yousuf SMA. Evaluating the quality of work life. Manag Labour Stud 1996;21:5–15. [Google Scholar]
- [21].Sirgy MJ, Efraty D, Siegel P, et al. A new measure of quality of work life (QWL) based on need satisfaction and spillover theories. Soc Indic Res 2001;55:241–302. [Google Scholar]
- [22].Spreitzer G, Porath CL. Creating sustainable performance. Harv Bus Rev 2012;90:92–9. [PubMed] [Google Scholar]
- [23].Society for Human Resource Management (SHRM©) Foundation's Effective Practice Guidelines Series. Creating a More Human Workplace Where Employees and Business Thrive. Available at: https://www.shrm.org/hr-today/trends-and-forecasting/special-reports-and-expert-views/Documents/Human-Workplace.pdf. Accessed: July 23, 2018. [Google Scholar]
- [24].Gauthy R. Musculoskeletal Disorders An Ill-understood “Pandemic”. European Trade Union Institute for Research, Education, Health and Safety, 2007. Belgium. ISBN: 978-2-87452-100-3. [Google Scholar]
- [25].Loghmani A, Golshiri P, Zamani A, et al. Musculoskeletal symptoms and job satisfaction among office-workers: a cross-sectional study from Iran. Acta Med Acad 2013;42:46–54. [DOI] [PubMed] [Google Scholar]
- [26].Chang KV, Wu WT, Özçakar L. Association of bicipital peritendinous effusion with subacromial impingement: a dynamic ultrasonographic study of 337 shoulders. Sci Rep 2016;6:38943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hung CY, Chang KV, Özçakar L, et al. Can quantification of biceps peritendinous effusion predict rotator cuff pathologies?: a retrospective analysis of 1352 shoulder ultrasound. Am J Phys Med Rehabil 2016;95:161–8. [DOI] [PubMed] [Google Scholar]
- [28].Chang KV, Wu WT, Han DS, et al. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch Phys Med Rehabil 2017;98:1984–94. [DOI] [PubMed] [Google Scholar]
- [29].De Jong M, De Boer AG, Tamminga SJ, et al. Quality of working life issues of employees with a chronic physical disease: a systematic review. J Occup Rehabil 2015;25:182–96. [DOI] [PubMed] [Google Scholar]
- [30].Matsudaira K, Palmer KT, Reading I, et al. Prevalence and correlates of regional pain and associated disability in Japanese workers. Occup Environ Med 2011;68:191–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Afsar ST. What affects the quality of work life most?: Turkey example. J Sociol Res 2014; 17(2):1–35. [Google Scholar]
- [32].Ssesanga K, Garrett RM. Job satisfaction of university academics: perspectives from Uganda. High Educ 2005;50:33–56. [Google Scholar]
- [33].Igbaria M, Parasuraman S, Badawy MK. Work experiences, job involvement, and quality of work life among information systems personnel. MIS Quart 1994;18:175–201. [Google Scholar]
- [34].Rose RC, Beh L, Uli J, et al. Quality of work life: implications of career dimensions. J Soc Sci 2006;2:61–7. [Google Scholar]


