Abstract
Syphilitic hepatitis in adults is not frequently found in the population and is easily misdiagnosed. The incidence of viral hepatitis is increasing year by year, concomitantly increasing the importance of obtaining a systematic understanding of the clinical features and treatment strategies for this disease. There is, however, a lack of published definitive data regarding the clinical characteristics, diagnosis and standard treatment options for this disease. Searches were made using the MEDLINE database of PubMed and OVID for syphilitic hepatitis publications from 1951 to 2017 in an attempt to analyze and summarize the clinical characteristics.
Keywords: Syphilis, Hepatitis, Liver enzyme, Granuloma
Introduction
Syphilis is a sexually transmitted infection induced by the spirochete Treponema pallidum, which has a huge impact on people’s physical and mental health. In its natural course, the disease progresses from primary syphilis to secondary syphilis and tertiary syphilis if left untreated. A chancre is often seen in primary syphilis. Secondary syphilis is characterized by a distinctive rash, while tertiary syphilis is typified by neurosyphilis, cardiovascular syphilis or gummatous syphilis.1
An infectious venereal disease with multiple organs involved, syphilis has been described as “the great imitator”.2,3 The liver is one of the organs that can be affected.4 Liver disease due to syphilis infection has rarely been reported and little is known about syphilitic hepatitis (SH). Maryam et al.5 reported a case of a male with SH who showed multiple liver lesions, while the case published by Aggarwal et al.6 presented with raised alkaline phosphatase levels. Syphilis, especially in its early stages, is often asymptomatic and easily misdiagnosed.7 The increasing incidence of syphilis will result in more SH,8 therefore it is important to improve the understanding of this disease. Fehér et al.9 reported 17 pathologically-confirmed cases of SH from 175 patients with syphilis, in 1975. However, coinfection with hepatitis C virus cannot be ruled out from this population. In 2004, Mullick et al.10 defined SH in detail, however, the reports of this disease are still rare.
There is still a lack of definitive data published about the clinical characteristics, diagnosis and standard treatments of SH. To this end, we searched the MEDLINE database for SH publications from 1951 to 2017, analyzing and summarizing the clinical characteristics through a systematic literature review.
Methods
We searched the MEDLINE database of PubMed and OVID for case reports, case series and descriptions of adult-onset SH. The electronic databases were searched for publications up to January 2017 with the following MeSH terms: “syphilitic hepatitis”, “syphilis and liver”, “syphilis and jaundice”, “syphilis and hepatitis”. We also manually searched the references and related reviews of each included study for other possible citations. The searches were restricted to English-language publications.
Results
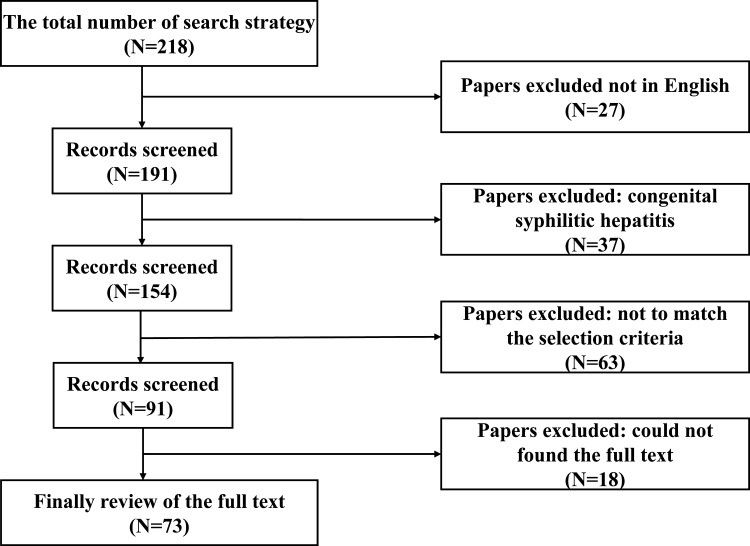
Finally, a total of 73 articles containing 144 cases of SH in adults with medical records were discovered2,3,5,6,10–78 (Fig. 1). The earliest article dated back to 195178 and the latest was published in 2016.11 The largest contribution came from the study by Jung et al.36 with 19 patients. Only 129 of the total 144 patients had complete demographic information. The mean age of the 129 cases with information available was 40.5 years, ranging from 14 to 76. The majority were male (130/144, 90.3%), with a sex ratio of 9.3 (130/14, male/female). The number of homosexual patients were 56 out of 103 recorded (54.4%), and all of them were men who had sex with men. Only 127 of the 129 patients had provided information on human immunodeficiency virus (HIV) infection. The number of patients coinfected with HIV and syphilis were 78 out of 127 with information available (61.4%). The stage of syphilis was recorded for all of the 144 patients, and included 128 (88.9%) with early syphilis (including primary and secondary syphilis), 7 (4.9%) with latent syphilis, and 9 (6.3%) with tertiary syphilis.
Fig. 1. A flow chart of the procedure followed for this systematic review.
A total of 97 cases had detailed clinical data available. The symptoms of SH were nonspecific in nature. Rashes were the most common clinical manifestations of SH (74/97, 77.9%), followed by fatigue or poor appetite (55/97, 56.7%), icterus (34/97, 35.1%), fever (25/97, 25.8%), weight loss (22/97, 22.7%), abdominal pain (21/97, 21.6%), phallodynia (13/97, 13.4%), sore throat (8/97, 8.2%), headache (7/97, 7.2%) and arthralgia or myodynia (6/97, 6.2%). In addition, physical examination revealed cases of hepatomegaly (52/97, 53.6%), lymphadenopathy (30/97, 30.9%), splenomegaly (14/97, 14.4%) and uveitis (8/97, 8.2%).
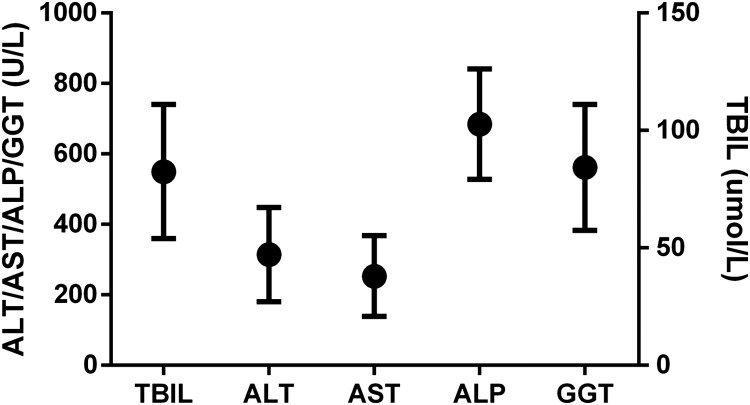
Information of the liver laboratory values was available for 99 out of the 144 patients (68.8%). The mean and 95% confidence interval (CI) of laboratory values have been summarized in the diagram below (Fig. 2). The mean for the laboratory values were 82.5 μmol/L (total bilirubin, TBIL), 314.5 U/L (alanine aminotransferase, ALT), 253.0 U/L (aspartate aminotransferase, AST), 684.5 U/L (alkaline phosphatase, ALP) and 561.8 U/L (gamma-glutamyl transpeptidase, GGT). We found an obvious rise in ALP and GGT outside of the normal ranges and slight elevations of ALT and TBIL.
Fig. 2. The mean and 95% CI of laboratory values.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate aminotransferase; CI, confidence interval; GGT, gamma-glutamyl transpeptidase; TBIL, total bilirubin.
A total of 55 cases had liver biopsy taken. The hallmark histopathological features found in the hepatic tissue included inflammatory cell infiltration of portal areas or hepatic lobules (48/55, 87.2%), hepatocellular necrosis (25/55, 45.5%), granuloma with multinucleated giant cells (11/55, 20%), cholestasis (27/55, 49.0%) and fibrosis (10/55, 18.2%). Immunohistochemical staining or Warthin–Starry staining were performed in 28 cases. In 19 of the 28 cases, treponema spirochetes were visualized in liver tissue, 15 of which were discovered by immunohistochemical staining and 4 by Warthin–Starry stain.
All the patients received antibiotic therapy. Among the 144 cases, 129 took intramuscular or intravenous penicillin therapy, 5 took oral doxycycline, 7 had oral amoxicillin hydrate and 3 used ceftriaxone. Jarisch-Herxheimer reaction occurred in 7 patients, with 6 of them responding to penicillin and one to amoxicillin hydrate treatment. All patients responded well to treatment.
Discussion
This systematic review showed that liver damage usually occurred in early syphilis, which was easily missed as a diagnosis because of the nonspecific nature of presenting symptoms. The results also found that SH was more often diagnosed in men, especially those who had sex with men, which could be linked to the route of sexual transmission. There were four large studies carried out to explore the relationship between SH and autoimmune deficiency syndrome, with a total of 54 patients.34,36,48,49 The studies showed that SH is common in HIV-positive patients with syphilis infection. Syphilis should be included in the differential diagnosis of HIV patients presenting with liver test abnormalities, rash and/or sexual risk factors. Liver damage is very common in HIV-infected patients because of their use of antiretroviral therapy, opportunistic infections and increased malignancy rates.10 In light of this, clinicians should try to maintain a broad list of differential diagnoses.
The clinical manifestations of SH in adults are often nonspecific and multifaceted. Rashes, fatigue or poor appetite, hepatomegaly and icterus were the most common. The rashes often presented as multiple nonpruritic, erythematous, nonconfluent maculopapular lesions, generally concentrated on the trunk, palms and soles of the feet. Hepatosplenomegaly is often found on physical examination or imaging. The laboratory tests of SH will show abnormal liver enzymes with a marked increase of ALP and GGT, in contrast to a mild elevation in ALT or AST levels. Histological features of SH include bile duct inflammatory infiltration, which may be linked to the elevated blood ALP and GGT levels. Hepatic granuloma is another feature of SH.79 It is very difficult to identify the spirochetes in liver tissue among these patients. Only 19 patients showed spirochetes in the liver tissue on immunohistochemical staining11,16,24 or Warthin–Starry staining.43,51,52
This is the first systematic review of SH. The results will help clinicians better understand this disease. The main limitations of this study were the retrospective design and the heterogeneous sources of the data. The heterogeneity and lack of data may cause bias.
Conclusions
The clinical characteristics of SH were its nonspecific presentation, elevated liver enzymes, especially ALP and GGT and bile duct inflammation or granuloma formation as seen by hepatic histopathology. Together, these facets of SH can provide some direction for clinicians regarding the approach to diagnosis of this disease.
Acknowledgments
We thank Bharat Velani, MD, PhD, from University College London (UK) for editing the English grammar of a draft of this manuscript. This study was funded by the Science and Technology Project of Fujian Education Department (JA15207) and Fujian Natural Science Foundation (2016Y0040, 2017J01187) and Fujian Medical Innovation Project (2016-cx-033).
Abbreviations
- ALP
alkaline phosphatase
- ALT
alanine transaminase
- AST
aspartate aminotransferase
- GGT
gamma-glutamyl transpeptidase
- HCV
hepatitis C virus
- SH
syphilitic hepatitis
- TBIL
total bilirubin
References
- 1.Dupin N, Farhi D. Syphilis. Presse Med. 2013;42:446–453. doi: 10.1016/j.lpm.2012.09.024. [DOI] [PubMed] [Google Scholar]
- 2.Suzuki I, Orfanidis N, Moleski S, Katz LC, Kastenberg D. The “great imitator” presents with abnormal liver enzymes. The Medicine Forum. 2009;11:17. doi: 10.29046/TMF.011.1.015. [DOI] [Google Scholar]
- 3.Sabbatani S, Manfredi R, Attard L, Chiodo F. The “great imitator” syphilis as causative agent of isolated, concurrent, acute hepatitis and meningitis. Infect Dis Clin Pract. 2005;13:261–264. doi: 10.1097/01.idc.0000168478.73470.69. [DOI] [Google Scholar]
- 4.Goodridge HF. A case of acute atrophy of the liver complicating early secondary syphilis. Br Med J. 1871;1:609–610. doi: 10.1136/bmj.1.545.609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keshtkar-Jahromi M, Rassaei N, Bruno MA, Maneval ML, Whitener CJ. Photo quiz. a 59-year-old man with multiple liver lesions, rash, and uveitis. Clin Infect Dis. 2016;62:82–83. doi: 10.1093/cid/civ754. [DOI] [PubMed] [Google Scholar]
- 6.Aggarwal SK, Radhakrishnan S. Syphilitic hepatitis: Look for raised alkaline phosphatase level. Med J Armed Forces India. 2016;72:192–193. doi: 10.1016/j.mjafi.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hook EW., Rd Syphilis. Lancet. 2017;389:1550–1557. doi: 10.1016/S0140-6736(16)32411-4. [DOI] [PubMed] [Google Scholar]
- 8.Patton ME, Su JR, Nelson R, Weinstock H. Primary and secondary syphilis–United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63:402–406. [PMC free article] [PubMed] [Google Scholar]
- 9.Fehér J, Somogyi T, Timmer M, Józsa L. Syphilitic hepatitis: clinical, immunological and morphological aspects. Acta Med Acad Sci Hung. 1975;32:155–161. [PubMed] [Google Scholar]
- 10.Mullick CJ, Liappis AP, Benator DA, Roberts AD, Parenti DM, Simon GL. Syphilitic hepatitis in HIV-infected patients: a report of 7 cases and review of the literature. Clin Infect Dis. 2004;39:e100–e105. doi: 10.1086/425501. [DOI] [PubMed] [Google Scholar]
- 11.Rubio-Tapia A, Hujoel IA, Smyrk TC, Poterucha JJ. Emerging secondary syphilis presenting as syphilitic hepatitis. Hepatology. 2017;65:2113–2115. doi: 10.1002/hep.28974. [DOI] [PubMed] [Google Scholar]
- 12.Batteiger T. Painless jaundice and transaminitis as a presentation of secondary syphilis. 2016 STD Prevention Conference 2016; Available from: https://cdc.confex.com/cdc/std2016/webprogram/Paper37674.html . [Google Scholar]
- 13.Vukšić Polić M1, Plužarić V, Kuric I. Syphilitic hepatitis: rare or just unrecognized? Acta Dermatovenerol Croat. 2015;23:70–71. [PubMed] [Google Scholar]
- 14.Pilozzi-Edmonds L, Kong LY, Szabo J, Birnbaum LM. Rapid progression to gummatous syphilitic hepatitis and neurosyphilis in a patient with newly-diagnosed HIV. Int J STD AIDS. 2015;26:985–987. doi: 10.1177/0956462414564401. [DOI] [PubMed] [Google Scholar]
- 15.Mulder CJ, Cho RS, Harrison SA, Cebe K, Francis JM. Syphilitic hepatitis uncommon presentation of an old scourge. Mil Med. 2015;180:e611–e613. doi: 10.7205/MILMED-D-14-00530. [DOI] [PubMed] [Google Scholar]
- 16.Khambaty M, Singal AG, Gopal P. Spirochetes as an almost forgotten cause of hepatitis. Clin Gastroenterol Hepatol. 2015;13:A21–A22. doi: 10.1016/j.cgh.2014.09.043. [DOI] [PubMed] [Google Scholar]
- 17.Ishiwatari A, Hasegawa J, Hoshino Y, Kaga T, Abe Y, Wakai S. Simultaneous nephrotic syndrome and hepatitis in secondary syphilis: case report and review of the literature. CEN Case Rep. 2015;4:223–227. doi: 10.1007/s13730-015-0173-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Clement ME, Okeke NL, Hicks CB. Fever and rash in a patient with hepatitis. JAMA. 2015;314:400–401. doi: 10.1001/jama.2015.3401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yoshikawa K, Aida Y, Seki N, Miyazaki T, Itagaki M, Ishiguro H, et al. Early syphilitic hepatitis concomitant with nephrotic syndrome followed by acute kidney injury. Clin J Gastroenterol. 2014;7:349–354. doi: 10.1007/s12328-014-0499-x. [DOI] [PubMed] [Google Scholar]
- 20.Sprenger K, Furrer H. Chameleons everywhere. BMJ Case Rep 2014. 2014 doi: 10.1136/bcr-2014-205608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solari PR, Jones C, Wallace MR. Hepatic lesions with secondary syphilis in an HIV-infected patient. Case Rep Med. 2014;2014:604794. doi: 10.1155/2014/604794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hagen CE, Kamionek M, McKinsey DS, Misdraji J. Syphilis presenting as inflammatory tumors of the liver in HIV-positive homosexual men. Am J Surg Pathol. 2014;38:1636–1643. doi: 10.1097/PAS.0000000000000264. [DOI] [PubMed] [Google Scholar]
- 23.Gaslightwala I, Khara HS, Diehl DL. Syphilitic gummas mistaken for liver metastases. Clin Gastroenterol Hepatol. 2014;12:e109–e110. doi: 10.1016/j.cgh.2014.04.022. [DOI] [PubMed] [Google Scholar]
- 24.Fielding CM, Angulo P. Right upper-quadrant pain in a patient with drug abuse, secondary syphilis and occult hepatitis B virus. Med Princ Pract. 2014;23:471–474. doi: 10.1159/000360401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bork JT, Macharia T, Choi J, Gilliam BL, Buchwald UK. Syphilitic hepatitis treated with doxycycline in an HIV-infected patient and review of the literature. Sex Transm Dis. 2014;41:507–510. doi: 10.1097/OLQ.0000000000000143. [DOI] [PubMed] [Google Scholar]
- 26.Baveja S, Garg S, Rajdeo A. Syphilitic hepatitis: an uncommon manifestation of a common disease. Indian J Dermatol. 2014;59:209. doi: 10.4103/0019-5154.127711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Palacios R, Navarro F, Narankiewicz D, Marcos M, Jiménez-Oñate F, de la Torre J, et al. Liver involvement in HIV-infected patients with early syphilis. Int J STD AIDS. 2013;24:31–33. doi: 10.1177/0956462412472316. [DOI] [PubMed] [Google Scholar]
- 28.Malincarne L, Pasticci MB, Angeli G, Baldelli F, De Socio GV. Syphilis as a diagnosis of liver abnormalities in HIV. Scand J Infect Dis. 2013;45:703–705. doi: 10.3109/00365548.2013.793819. [DOI] [PubMed] [Google Scholar]
- 29.Lee M, Wang C, Dorer R, Ferguson L. A great masquerader: acute syphilitic hepatitis. Dig Dis Sci. 2013;58:923–925. doi: 10.1007/s10620-012-2322-1. [DOI] [PubMed] [Google Scholar]
- 30.Kim M, Echevarria L, Savilo E. Answer to June 2013 Photo Quiz. J Clin Microbiol. 2013;51:2016. doi: 10.1128/JCM.00703-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.da Silva BA, Soi TS, Cameron D, Karikkineth AC, Williams RB. Syphilis, hepatitis, and pancreatitis: is the uncommon becoming common in the HIV(+) patient? Case Rep Infect Dis. 2013;2013:293823. doi: 10.1155/2013/293823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Aggarwal A, Sharma V, Vaiphei K, Duseja A, Chawla YK. An unusual cause of cholestatic hepatitis: syphilis. Dig Dis Sci. 2013;58:3049–3051. doi: 10.1007/s10620-013-2581-5. [DOI] [PubMed] [Google Scholar]
- 33.Adachi E, Koibuchi T, Okame M, Sato H, Kikuchi T, Koga M, et al. Liver dysfunction in patients with early syphilis: a retrospective study. J Infect Chemother. 2013;19:180–182. doi: 10.1007/s10156-012-0440-5. [DOI] [PubMed] [Google Scholar]
- 34.Manavi K, Dhasmana D, Cramb R. Prevalence of hepatitis in early syphilis among an HIV cohort. Int J STD AIDS. 2012;23:e4–e6. doi: 10.1258/ijsa.2009.009386. [DOI] [PubMed] [Google Scholar]
- 35.Lin H, Russo P, Rook M. Secondary syphilitic hepatitis in a 17-year-old girl. J Pediatr Gastroenterol Nutr. 2012;55:e134–e135. doi: 10.1097/MPG.0b013e31824177cf. [DOI] [PubMed] [Google Scholar]
- 36.Jung N, Kümmerle T, Brengelmann SD, Gielen J, Lehmann C, Wyen C, et al. Liver involvement in HIV-infected patients diagnosed with syphilis. Infection. 2012;40:543–547. doi: 10.1007/s15010-012-0264-3. [DOI] [PubMed] [Google Scholar]
- 37.Hosein SR. Hepatitis caused by syphilis. Canadian AIDS Treatment Information Exchange. 2012. Available from: http://www.thebodypro.com/content/69370/hepatitis-caused-by-syphilis.html .
- 38.Filho FB, Santos MVPQ, Perez VPF, Jaber NM, Alves AO, Azulay DR, et al. Cutaneous and visceral syphilis: unusual presentation. DST-J bras Doenças Sex Transm. 2012;24:195–197. doi: 10.5533/DST-2177-8264-201224310. [DOI] [Google Scholar]
- 39.Canney M, Liu E, Vonthethoff L, Weatherall C, Ong S. Nephrotic syndrome and hepatitis due to acquired syphilis: an uncommon presentation of a re-emerging disease. NDT Plus. 2011;4:67–70. doi: 10.1093/ndtplus/sfq194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Adachi E, Koibuchi T, Okame M, Sato H, Imai K, Shimizu S, et al. Case of secondary syphilis presenting with unusual complications: syphilitic proctitis, gastritis, and hepatitis. J Clin Microbiol. 2011;49:4394–4396. doi: 10.1128/JCM.01240-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rutland E, Harindra VK. Syphilis: an important cause of infectious hepatitis. Int J STD AIDS. 2010;21:215–216. doi: 10.1258/ijsa.2009.009031. [DOI] [PubMed] [Google Scholar]
- 42.Miura H, Nakano M, Ryu T, Kitamura S, Suzaki A. A case of syphilis presenting with initial syphilitic hepatitis and serological recurrence with cerebrospinal abnormality. Intern Med. 2010;49:1377–1381. doi: 10.2169/internalmedicine.49.3414. [DOI] [PubMed] [Google Scholar]
- 43.Kim GH, Kim BU, Lee JH, Choi YH, Chae HB, Park SM, et al. Cholestatic hepatitis and thrombocytosis in a secondary syphilis patient. J Korean Med Sci. 2010;25:1661–1664. doi: 10.3346/jkms.2010.25.11.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bjekić M, Marković M, Sipetić S. Early syphilis and syphilitic hepatitis following unprotected insertive oral sexual intercourse: case report. Acta Dermatovenerol Croat. 2010;18:276–278. [PubMed] [Google Scholar]
- 45.Ibáñez M, Varela M, Rodríguez-Peláez M, Mancebo A, García-Mayor MA, Pereira R, et al. Luetic hepatitis. An emerging entity. Gastroenterol Hepatol. 2009;32:610–613. doi: 10.1016/j.gastrohep.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 46.Hosein SR. Syphilis can attack the liver in HIV-positive men. Canadian AIDS Treatment Information Exchange. 2009. Available from: http://www.thebody.com/content/art51480.html .
- 47.Doyle RJ, Desai M, White J. Response to Crum-Cianflone et al., syphilitic hepatitis among HIV-infected patients. Int J STD AIDS. 2009;20:739–740. doi: 10.1258/ijsa.2009.009297. [DOI] [PubMed] [Google Scholar]
- 48.Crum-Cianflone N, Weekes J, Bavaro M. Syphilitic hepatitis among HIV-infected patients. Int J STD AIDS. 2009;20:278–284. doi: 10.1258/ijsa.2008.008324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Béraud G, Pierre-François S, Theodose R, Desbois N, Abel S, Liautaud B, et al. Anicteric cholestasis among HIV infected patients with syphilis. Scand J Infect Dis. 2009;41:524–527. doi: 10.1080/00365540902798325. [DOI] [PubMed] [Google Scholar]
- 50.Albandea Moreno C, Aguilar Urbano VM, Rivera Irigoin R, Gonzalo Marín J, Rosales Zabal JM, Moreno García A, et al. Syphilitic hepatitis: case report. Rev Esp Enferm Dig. 2009;101:813–814. doi: 10.4321/S1130-01082009001100011. [DOI] [PubMed] [Google Scholar]
- 51.Noto P, Del Nonno F, Licci S, Chinello P, Petrosillo N. Early syphilitic hepatitis in an immunocompetent patient: really so uncommon? Int J STD AIDS. 2008;19:65–66. doi: 10.1258/ijsa.2007.007037. [DOI] [PubMed] [Google Scholar]
- 52.Noto P, Boumis E, Passarelli F, Licci S. An old disease makes a comeback. Liver Int. 2008;28:1417. doi: 10.1111/j.1478-3231.2008.01771.x. [DOI] [PubMed] [Google Scholar]
- 53.Tanyel E, Taşdelen Fişgin N, Sarikaya Genç H, Tülek N. A case of secondary syphilis with hepatitis. Mikrobiyol Bul. 2007;41:291–296. [PubMed] [Google Scholar]
- 54.Lo JO, Harrison RA, Hunter AJ. Syphilitic hepatitis resulting in fulminant hepatic failure requiring liver transplantation. J Infect. 2007;54:e115–e117. doi: 10.1016/j.jinf.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 55.Keskin S, Sayali E, Keskin E, Celebi A, Senol EG, Gürler M, et al. A case of syphilis investigated due to high liver enzymes. Turk J Gastroenterol. 2007;18:62–63. [PubMed] [Google Scholar]
- 56.Greenstone CL, Saint S, Moseley RH. Clinical problem solving. A hand-carried diagnosis. N Engl J Med. 2007;356:2407–2411. doi: 10.1056/NEJMcps062271. [DOI] [PubMed] [Google Scholar]
- 57.Camara B, Kamar N, Bonafe JL, Danjoux M, Suc B, Rostaing L. Syphilis hepatitis and liver transplantation. Med Mal Infect. 2007;37:121–123. doi: 10.1016/j.medmal.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 58.Camara B, Kamar N, Bonafe JL, Danjoux M, Suc B, Rostaing L. Syphilis-related hepatitis in a liver transplant patient. Exp Clin Transplant. 2007;5:724–726. [PubMed] [Google Scholar]
- 59.Wolf SC, Kempf VA, Tannapfel A, Petersen P, Risler T, Brehm BR. Secondary syphilis after liver transplantation: case report and review of the literature. Clin Transplant. 2006;20:644–649. doi: 10.1111/j.1399-0012.2006.00531.x. [DOI] [PubMed] [Google Scholar]
- 60.Mandache C, Coca C, Caro-Sampara F, Haberstezer F, Coumaros D, Blicklé F, et al. A forgotten aetiology of acute hepatitis in immunocompetent patient: syphilitic infection. J Intern Med. 2006;259:214–215. doi: 10.1111/j.1365-2796.2005.01596.x. [DOI] [PubMed] [Google Scholar]
- 61.Ishikawa M, Shimizu I, Uehara K, Fujiwara S, Shiraishi T, Yamamoto H, et al. A patient with early syphilis complicated by fatty liver who showed an alleviation of hepatopathy accompanied by jaundice after receiving anti-syphilitic therapy. Intern Med. 2006;45:953–956. doi: 10.2169/internalmedicine.45.1746. [DOI] [PubMed] [Google Scholar]
- 62.Sabbatani S, Manfredi R, Attard L, Salfi N, Chiodo F. Secondary syphilis presenting with acute severe hepatic involvement in a patient with undiagnosed HIV disease. AIDS Patient Care STDS. 2005;19:545–549. doi: 10.1089/apc.2005.19.545. [DOI] [PubMed] [Google Scholar]
- 63.Cooper C, MacPherson P, Angel JB. Liver toxicity resulting from syphilis and Jarish-Herxheimer reaction in cases of coinfection with HIV and hepatitis C virus. Clin Infect Dis. 2005;40:1211–1212. doi: 10.1086/428848. [DOI] [PubMed] [Google Scholar]
- 64.Watson KM, White JM, Salisbury JR, Creamer D. Lues maligna. Clin Exp Dermatol. 2004;29:625–627. doi: 10.1111/j.1365-2230.2004.01630.x. [DOI] [PubMed] [Google Scholar]
- 65.Ridruejo E, Mordoh A, Herrera F, Avagnina A, Mando OO. Severe cholestatic hepatitis as the first symptom of secondary syphilis. Dig Dis Sci. 2004;49:1401–1404. doi: 10.1023/B:DDAS.0000042237.40205.c6. [DOI] [PubMed] [Google Scholar]
- 66.Jamieson A. Deranged liver function tests in type 1 diabetes mellitus: an unusual presentation of Treponema pallidum infection. Eur J Intern Med. 2003;14:113–115. doi: 10.1016/S0953-6205(02)00218-2. [DOI] [PubMed] [Google Scholar]
- 67.Ozaki T, Takemoto K, Hosono H, Miyagawa K, Akimoto S, Nishimura N. Secondary syphilitic hepatitis in a fourteen-year-old male youth. Pediatr Infect Dis J. 2002;21:439–441. doi: 10.1097/00006454-200205000-00022. [DOI] [PubMed] [Google Scholar]
- 68.Almoujahed MO, Johnson LB, Khatib R. Syphilitic hepatitis presenting with fever and inguinal lymphadenopathy without rash: a case report. Infectious Diseases in Clinical Practice. 2002;11:286–287. doi: 10.1097/00019048-200206000-00006. [DOI] [Google Scholar]
- 69.Taniguchi Y, Nakae Y, Ikoma K, Ishihara Y, Kumamoto M, Nakazawa K, et al. Subclinical syphilitic hepatitis, which was markedly worsened by a Jarisch-Herxheimer reaction. Am J Gastroenterol. 1999;94:1694–1696. doi: 10.1111/j.1572-0241.1999.01168.x. [DOI] [PubMed] [Google Scholar]
- 70.Gschwantler M, Gulz W, Schrutka-Kölbl C, Kogelbauer G, Schober G, Bibus B, et al. Acute hepatitis as the leading symptom of secondary syphilis. Dtsch Med Wochenschr. 1996;121:1457–1461. doi: 10.1055/s-2008-1043168. [DOI] [PubMed] [Google Scholar]
- 71.Shapiro MP, Gale ME. Tertiary syphilis of the liver: CT appearance. J Comput Assist Tomogr. 1987;11:546–547. doi: 10.1097/00004728-198705000-00038. [DOI] [PubMed] [Google Scholar]
- 72.Cronin EB, Williams WH, Tow DE. Radionuclide imaging in a case of tertiary syphilis involving the liver and bones. J Nucl Med. 1987;28:1047–1051. [PubMed] [Google Scholar]
- 73.Haburchak DR, Davidson H. Anorectal lesions and syphilitic hepatitis. West J Med. 1978;128:64–67. [PMC free article] [PubMed] [Google Scholar]
- 74.Fehér J, Somogyi T, Timmer M, Józsa L. Early syphilitic hepatitis. Lancet. 1975;2:896–899. doi: 10.1016/S0140-6736(75)92129-7. [DOI] [PubMed] [Google Scholar]
- 75.Bhowmick BK, Simpsom B, Way SP. Secondary syphilis presenting jaundice. Postgrad Med J. 1975;51:412–416. doi: 10.1136/pgmj.51.596.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Le Clair RA. Early syphilitic hepatitis. A possible case. Br J Vener Dis. 1971;47:212. doi: 10.1136/sti.47.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pierce HE. Early acute syphilitic benign hepatitis; a case report. J Natl Med Assoc. 1953;45:219–220. [PMC free article] [PubMed] [Google Scholar]
- 78.Nicol CS, Terry RB. Late syphilis of the liver treated with penicillin. Br J Vener Dis. 1951;27:20–22. doi: 10.1136/sti.27.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lamps LW. Hepatic Granulomas: A Review With Emphasis on Infectious Causes. Arch Pathol Lab Med. 2015;139:867–875. doi: 10.5858/arpa.2014-0123-RA. [DOI] [PubMed] [Google Scholar]