Autosomal-recessive IL-17RA, IL-17RC, and ACT1 deficiencies and autosomal-dominant IL-17F deficiency in humans underlie susceptibility to chronic mucocutaneous candidiasis.
Abstract
Chronic mucocutaneous candidiasis (CMC) is characterized by recurrent or persistent infections of the skin, nail, oral, and genital mucosae with Candida species, mainly C. albicans. Autosomal-recessive (AR) IL-17RA and ACT1 deficiencies and autosomal-dominant IL-17F deficiency, each reported in a single kindred, underlie CMC in otherwise healthy patients. We report three patients from unrelated kindreds, aged 8, 12, and 37 yr with isolated CMC, who display AR IL-17RC deficiency. The patients are homozygous for different nonsense alleles that prevent the expression of IL-17RC on the cell surface. The defect is complete, abolishing cellular responses to IL-17A and IL-17F homo- and heterodimers. However, in contrast to what is observed for the IL-17RA– and ACT1-deficient patients tested, the response to IL-17E (IL-25) is maintained in these IL-17RC–deficient patients. These experiments of nature indicate that human IL-17RC is essential for mucocutaneous immunity to C. albicans but is otherwise largely redundant.
In humans, chronic mucocutaneous candidiasis (CMC) is characterized by infections of the skin, nail, digestive, and genital mucosae with Candida species, mainly C. albicans, a commensal of the gastrointestinal tract in healthy individuals (Puel et al., 2012). CMC is frequent in acquired or inherited disorders involving profound T cell defects (Puel et al., 2010b; Vinh, 2011; Lionakis, 2012). Human IL-17 immunity has recently been shown to be essential for mucocutaneous protection against C. albicans (Puel et al., 2010b, 2012; Cypowyj et al., 2012; Engelhardt and Grimbacher, 2012; Huppler et al., 2012; Ling and Puel, 2014). Indeed, patients with primary immunodeficiencies and syndromic CMC have been shown to display impaired IL-17 immunity (Puel et al., 2010b). Most patients with autosomal-dominant (AD) hyper-IgE syndrome (AD-HIES) and STAT3 deficiency (de Beaucoudrey et al., 2008; Ma et al., 2008; Milner et al., 2008; Renner et al., 2008; Chandesris et al., 2012) and some patients with invasive fungal infection and autosomal-recessive (AR) CARD9 deficiency (Glocker et al., 2009; Lanternier et al., 2013) or Mendelian susceptibility to mycobacterial diseases (MSMD) and AR IL-12p40 or IL-12Rβ1 deficiency (de Beaucoudrey et al., 2008, 2010; Prando et al., 2013; Ouederni et al., 2014) have low proportions of IL-17A–producing T cells and CMC (Cypowyj et al., 2012; Puel et al., 2012). Patients with AR autoimmune polyendocrine syndrome type 1 (APS-1) and AIRE deficiency display CMC and high levels of neutralizing autoantibodies against IL-17A, IL-17F, and/or IL-22 (Browne and Holland, 2010; Husebye and Anderson, 2010; Kisand et al., 2010, 2011; Puel et al., 2010a).
These findings paved the way for the discovery of the first genetic etiologies of CMC disease (CMCD), an inherited condition affecting individuals with none of the aforementioned primary immunodeficiencies (Puel et al., 2011; Casanova and Abel, 2013; Casanova et al., 2013, 2014). AR IL-17RA deficiency, AR ACT1 deficiency, and AD IL-17F deficiency were described, each in a single kindred (Puel et al., 2011; Boisson et al., 2013). A fourth genetic etiology of CMCD, which currently appears to be the most frequent, has also been reported: heterozygous gain-of-function (GOF) mutations of STAT1 impairing the development of IL-17–producing T cells (Liu et al., 2011; Smeekens et al., 2011; van de Veerdonk et al., 2011; Hori et al., 2012; Takezaki et al., 2012; Tóth et al., 2012; Al Rushood et al., 2013; Aldave et al., 2013; Romberg et al., 2013; Sampaio et al., 2013; Soltész et al., 2013; Uzel et al., 2013; Wildbaum et al., 2013; Frans et al., 2014; Kilic et al., 2014; Lee et al., 2014; Mekki et al., 2014; Mizoguchi et al., 2014; Sharfe et al., 2014; Yamazaki et al., 2014). We studied three unrelated patients with CMCD without mutations of IL17F, IL17RA, ACT1, or STAT1. We used a genome-wide approach based on whole-exome sequencing (WES). We found AR complete IL-17RC deficiency in all three patients.
RESULTS
Clinical reports
The experiments described here were conducted in accordance with French regulations and were approved by the French Ministry of Research (IE-2010-547), the French Ethics committee (ID-RCB 2010-A00636-33), and ANSM (French National Agency for Medicines and Health Products Safety; B100712-40). Informed consent was obtained from all patients or their families, in the case of minors, in accordance with the World Medical Association, the Helsinki Declaration, and EU directives.
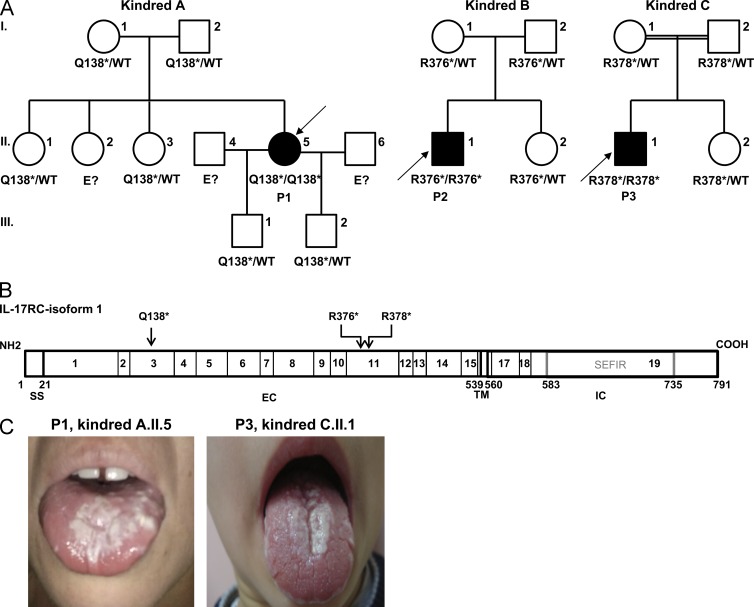
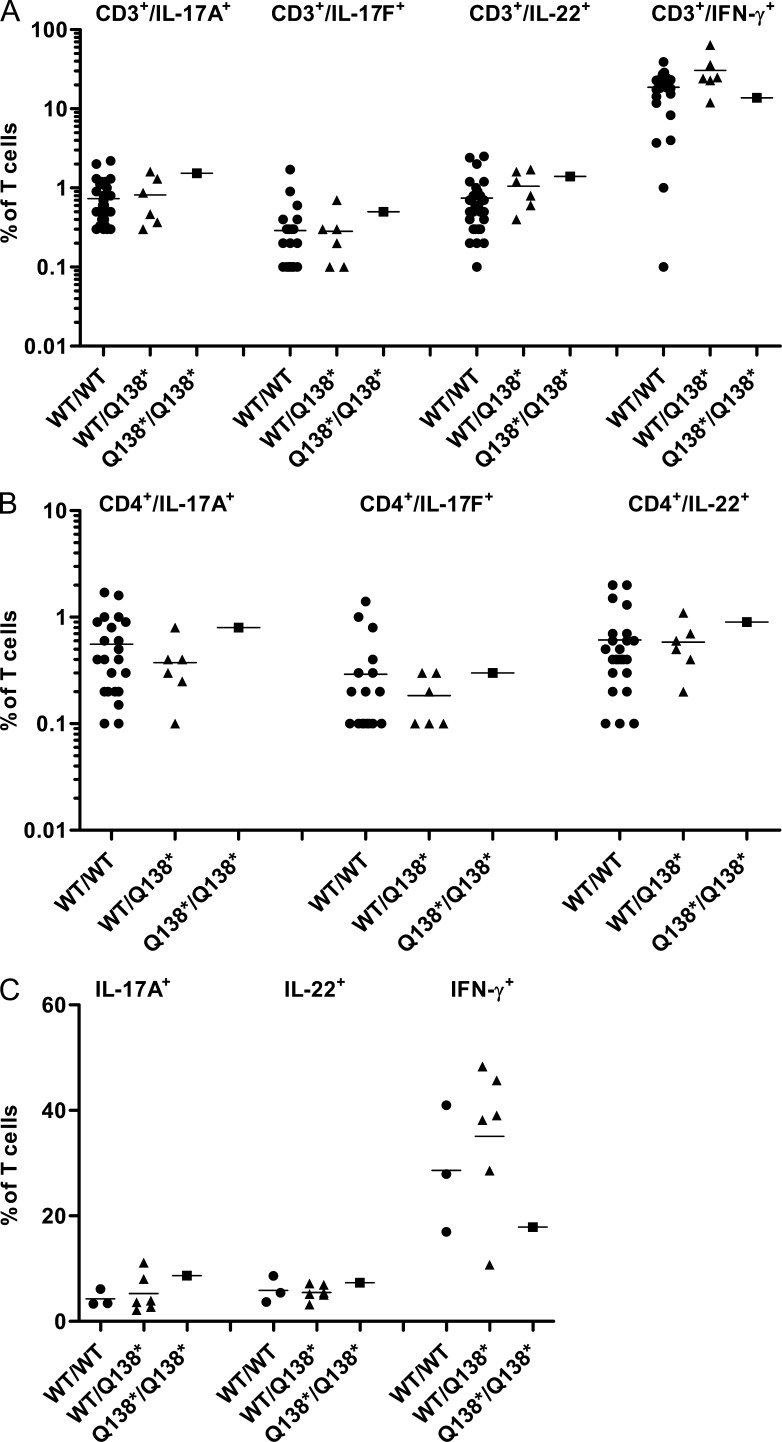
The index patient of kindred A (P1, kindred A.II.5, Fig. 1 A) is a 37-yr-old woman of Argentinean origin, living in Argentina, with no known parental consanguinity. The calculated homozygosity rate for P1 was 0.008 (not depicted; Purcell et al., 2007), providing further support for the notion that P1 was not from closely related parents. However, the mutation was located in a homozygous region of 7.1 Mb, which may be consistent with a cryptic consanguinity. Since the age of 4 yr, P1 has suffered from chronic intertrigo and pustules on her face, but with a normal scalp, nails, teeth, and sweating. She also developed recurrent oral (P1, kindred A.II.5, Fig. 1 C) and esophageal thrush. She had never suffered from any severe bacterial (staphylococcal, in particular), viral, or other fungal infection. P1 was treated with oral fluconazole. The response to treatment was good, with no drug resistance, but relapses occurred when treatment was stopped. Laboratory investigations showed normal immunophenotype (T, B, and NK). The T cell proliferations in response to phytohemagglutinin and antigens (tuberculin, candidin, and anatoxin) were normal. No endocrine, metabolic, or autoimmune abnormalities were reported. In particular, the patient did not display anti-DNA, antinuclear, or antithyroglobulin antibodies and had normal TSH levels. P1 had normal proportions of circulating IL-17A–, IL-17F–, IL-22–producing CD3+ and CD4+ T cells (Fig. 2, A–C) and displayed normal IL-17A production by freshly prepared leukocytes (Fig. 3 A). None of her sisters, parents, or sons had any particular relevant clinical history.
Figure 1.
Three kindreds with AR IL-17RC deficiency. (A) Pedigrees and familial segregation of the identified IL-17RC nonsense mutations. The proband is indicated in black and by an arrow. I, II, and III indicate the generations. E? indicates individuals whose genetic status could not be evaluated. (B) Schematic diagram of the IL-17RC protein, showing the signal sequence (SS), extracellular (EC), transmembrane (TM), intracellular (IC), and SEFIR (expression similar to fibroblast growth factor IL-17R) domains and the exons and amino acids affected by the mutations. (C) Recurrent thrush on tongue of P1 (kindred A.II.5) and P3 (kindred C.II.1).
Figure 2.
Normal ex vivo development and in vitro differentiation of IL-17– and IL-22–producing T cells from P1. (A–C) Each symbol represents a value from a healthy control individual (black circles), a heterozygous (WT/Q138*) relative of P1 (black triangles), and P1 (black squares). Horizontal bars represent means. (A and B) Percentages are shown of CD3+/IL-17A+, CD3+/IL-17F+, CD3+/IL-22+, and CD3+/IFN-γ+ (A) and CD4+/IL-17A+, CD4+/IL-17F+, and CD4+/IL-22+ (B) cells, as determined by flow cytometry, among nonadherent PBMCs activated by incubation for 12 h with PMA and ionomycin. (C) Percentages are shown of IL-17A+, IL-22+, and IFN-γ+ T cell blasts after in vitro expansion in the presence of anti-CD3 antibody, IL-2, IL-1β, and IL-23 for 5 d, followed by 12 h of stimulation with PMA and ionomycin. The experiments were repeated at least three times.
Figure 3.
Normal secretion of IL-17A and IL-22 by whole blood cells from patients. (A–E) IL-17A (A–C) and IL-22 (D and E) secretion was determined by ELISA, in the absence of stimulation (open symbols) and after stimulation with PMA and ionomycin for 24 h (closed symbols). Horizontal bars represent medians. Each symbol represents a value from healthy control individuals (circles), heterozygous patients’ relatives (triangles), or patients (squares). The experiments were repeated at least three times.
The index patient of kindred B (P2, kindred B.II.1, Fig. 1 A) is a 12-yr-old boy born to Turkish parents, with no known parental consanguinity. The calculated homozygosity rate of P2 was 0.021 (not depicted), consistent with P2 originating from a family without close consanguinity. P2 has suffered from CMC since the age of 2 mo, with chronic intertrigo, aphthous stomatitis, oral thrush, and onychomycosis, but with no reported severe bacterial (staphylococcal in particular), viral, or other fungal infections. CMC was long lasting in this patient. It was treated with courses of oral and i.v. fluconazole and local nystatin, and a response to treatment was observed, but with relapse after treatment cessation. Routine laboratory investigations showed that lymphocyte counts were normal and serum IgG, IgA, IgM, and IgE levels were within the normal ranges. Thyroid function, as evaluated by determining TSH (2.4 IU/l) and T4 (1.19 ng/dl) levels, was normal. Normal levels of IL-17A and IL-22 were produced after ex vivo stimulation with PMA and ionomycin by freshly prepared leukocytes of P2 and other members of his family (Fig. 3, B and D). No endocrine, metabolic, or autoimmune abnormalities were reported. Neither the parents nor the siblings of this patient have ever suffered from severe infections.
The index patient of kindred C (P3, kindred C.II.1, Fig. 1 A) is an 8-yr-old boy from a third-degree consanguineous Turkish family. This information is consistent with the homozygosity rate of 0.039 obtained for this patient (not depicted). P3 displayed persistent oral candidiasis, with white plaques all over the buccal mucosa and dorsal surface of the tongue since early infancy (P3, kindred C.II.1, Fig. 1 C) and pustules on the skin and scalp. P3 had no history of any other significant infectious (bacterial, staphylococcal in particular, viral, or other fungal) disease or significant developmental defects, with normal hair, nails, teeth, and sweating. Leukocyte counts and absolute neutrophil and lymphocyte counts were normal. Serum IgG, IgA, and IgM levels were normal. No autoimmune antibodies, such as antinuclear, antiperoxisomal (anti-TPO and anti-TG), and antiparietal antibodies, were detected in the serum. Peripheral blood lymphocyte subsets were within the normal range. In vitro T cell proliferation tests showed that the percentages of CD3+CD25+ (66%; normal 43–97%) and CD3+CD69+ (68%; normal 45–100%) cells were within the normal ranges after stimulation with phytohemagglutinin. Normal levels of IL-17A and IL-22 secretion by freshly prepared leukocytes after ex vivo stimulation with PMA and ionomycin were observed for P3 and other members of his family (Fig. 3, C and E). No endocrine or metabolic abnormalities were found. Systemic antifungal therapy with oral fluconazole was initiated and moniliasis resolved. However, oral moniliasis recurred and persisted for some time after the cessation of treatment. Neither the parents nor the siblings of P3 had ever suffered from a severe infectious disease.
Homozygous nonsense mutations of IL17RC
WES revealed the presence of different homozygous nonsense mutations of IL17RC in these patients. We chose to investigate these mutations further as potential disease-causing mutations because of their likely impact on IL-17 immunity. In addition, IL17RC displayed a very short biological distance between the known CMCD-causing genes IL17RA and ACT1 (P-values of 0.0005 and 0.0007, respectively), making it a very likely novel candidate gene for CMCD (Itan et al., 2013). P1 was found to be homozygous for the c.412C>T nonsense mutation in exon 3 of the IL17RC gene. This mutation replaces the glutamine codon at position 138 with a premature stop codon (Q138*; Fig. 1 B). The healthy parents, tested siblings, and children of P1 were all heterozygous (WT/Q138*) for the mutant allele, consistent with AR inheritance for this trait (Fig. 1 A). P2 was found to be homozygous for the c.1126C>T nonsense mutation in exon 11 of the IL17RC gene. This mutation replaces the arginine codon in position 376 with a premature stop codon (R376*; Fig. 1 B). The parents and sister of P2 are healthy and heterozygous for the mutant allele, consistent with AR inheritance (Fig. 1 A). P3 was found to be homozygous for the c.1132C>T nonsense mutation in exon 11 of the IL17RC gene, replacing the arginine codon in position 378 with a premature stop codon (R378*; Fig. 1 B). The parents and sister of P3 are healthy and heterozygous for the mutant allele, consistent with AR inheritance (Fig. 1 A). The mutant allele (Q138*) from P1 was not found in any of the various public databases (Human Gene Mutation Database, Ensembl, NHLBI GO Exome Sequencing Project [ESP], 1000 Genomes Project, and the Exome Aggregation Consortium [ExAC]) or in our in-house WES database (∼1,800 exomes), ruling out the possibility of an irrelevant polymorphism and suggesting that this mutation may define a rare AR CMCD-causing allele. The R376* mutant allele, found in P2, has been reported in the ExAC database, only at the heterozygous state, in 5 out of 59,269 individuals. The R378* mutant allele found in P3 has been reported previously (dbSNP accession no. rs143600903), but with a low frequency (0.057%); only one European from a population of 59,318 individuals has been found to be homozygous for this variant, consistent with the notion that this mutation may define a rare AR CMCD-causing allele. The three premature stop codons are located upstream from the segment encoding the transmembrane domain of IL-17RC (Fig. 1 B). No rare coding mutations were found in STAT1, IL17RA, IL17A, IL17F, ACT1, IL22, or IL22RA1 by WES in the three patients.
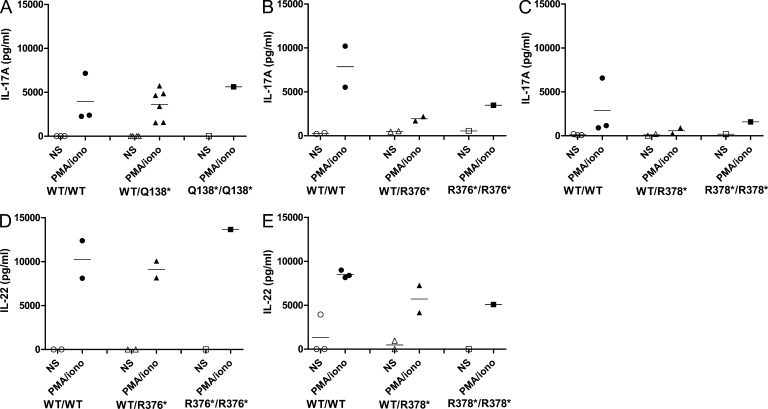
Impaired production of IL17RC mRNA and protein
We used RT-PCR or TaqMan assays to determine the levels of full-length IL17RC mRNA, which we found to be lower in fibroblasts from the patients than in cells from healthy controls (Fig. 4, A and B). However, no band of the correct size corresponding to IL-17RC could be detected by Western blot in control fibroblasts without transfection. Therefore, the patients’ fibroblasts were then transfected with various expression vectors: an empty vector or vectors encoding the WT or any of the three mutant alleles (Q138*, R376*, or R378*). In this overexpression system, the IL17RC mRNAs generated by transcription from the WT allele or the three mutant alleles were detected equally well by qPCR (Fig. 4 C). A product of ∼85 kD, corresponding to isoform 1, was detected in cells transfected with the WT IL17RC allele, whereas no product of this molecular mass was detected in fibroblasts transfected with any of the three mutant IL17RC alleles (Fig. 4 D). No product with a lower molecular mass was detected in cells transfected with the Q138* IL-17RC–encoding construct, with an anti–IL-17RC antibody directed against the epitope covering amino acids 113–258. A product with a lower molecular mass (∼40 kD), corresponding to a C-terminally truncated protein, was detected in cells transfected with the constructs encoding R376* or R378* IL-17RC. A product of ∼80 kD was detected in cells transfected with the WT allele and a product of ∼35 kD was detected in cells transfected with the R376* or R378* allele. These products were probably the result of posttranscriptional modifications. In addition, HEK-293T cells transfected with various constructs encoding IL-17RC WT, Q138*, R376*, or R378* displayed a strong membrane expression, as detected by total internal reflection fluorescence (TIRF) imaging, only when transfected with the WT allele but none of the mutants alleles (Fig. 5 A). The absence of IL-17RC had no impact on the expression of IL-17RA, which was found to be expressed to similar levels on the fibroblasts of patients and controls (Fig. 5 B).
Figure 4.
Expression of IL-17RC in fibroblasts from controls and patients. (A and B) Amounts of IL17RC cDNA generated from SV40-immortalized fibroblasts from two controls and two patients (P1 and P2), as determined by full-length RT-PCR (A) and TaqMan assays (B). (C) Amounts of IL17RC cDNA obtained from the SV40 fibroblasts of P1 and P2 either left untransfected (NT) or transfected with pUNO1, either empty (MCS) or encoding the WT, Q138*, R376*, or R378* IL-17RC. Results are also shown for the SV40 fibroblasts of two controls tested in parallel (C1 and C2). Means ± SD (error bars) of three independent experiments, as detected by quantitative PCR, are shown. β-ACTIN and GUS were used as endogenous controls. The experiments were repeated at least three times. (D) IL-17RC expression in P1’s and P2’s SV40 fibroblasts transfected with WT or mutant IL17RC alleles, as assessed by Western blotting. IL-17RC protein levels in SV40 fibroblasts from P1 and P2 transfected with the empty pUNO1mcs plasmid (mock) or the pUNO1 plasmid, encoding the WT or one of the three mutant (Q138*, R376*, or R378*) IL-17RC proteins, as determined by Western blotting with an anti–IL-17RC antibody (directed against amino acids 113–258). The anti-GAPDH antibody was used as a control for protein loading. These experiments were repeated at least three times.
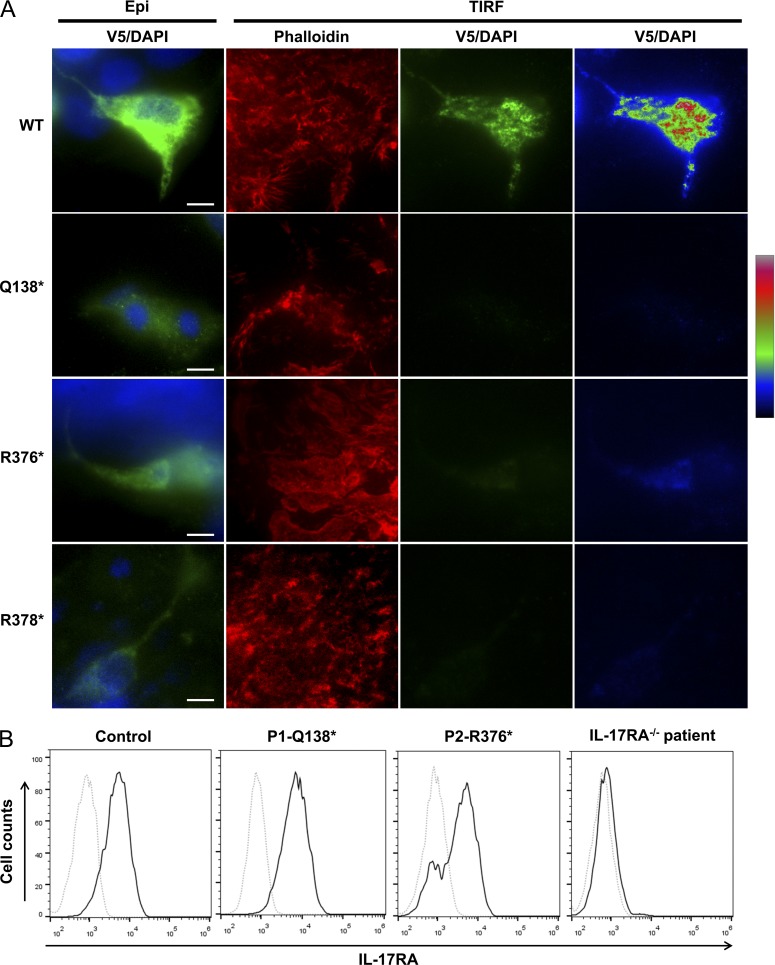
Figure 5.
Expression of WT, mutant IL-17RC, and IL-17RA at the cell surface. (A) IL-17RC expression in HEK-293T cells transfected with V5 tag plasmid encoding IL-17RC WT or mutant alleles, as assessed by TIRF imaging. HEK-293T cells were transfect with V5 tag–IL17RC-pcDNA 3.1 encoding WT or mutant (Q138*, R376*, or R378*) IL-17RC. The “Epi” was assessed by epifluorescence illumination, and the “TIRF” was detected by TIRF microscopy. DAPI binds double-stranded DNA, and phalloidin binds F-actin. The “pseudocolor” scales were used to indicate the intensity staining in TIRF. For each setting condition, 20 cells have been analyzed from cumulating three independent experiments. Bars, 5 µm. (B) IL-17RA expression on SV40-immortalized fibroblasts from a control, P1 (Q138*/Q138*), P2 (R376*/R376*), and an IL-17RA–deficient patient (Q284*/Q284*), as assessed by flow cytometry. Isotype control, gray dotted lines; IL-17RA antibody, black lines. The experiments were repeated at least three times.
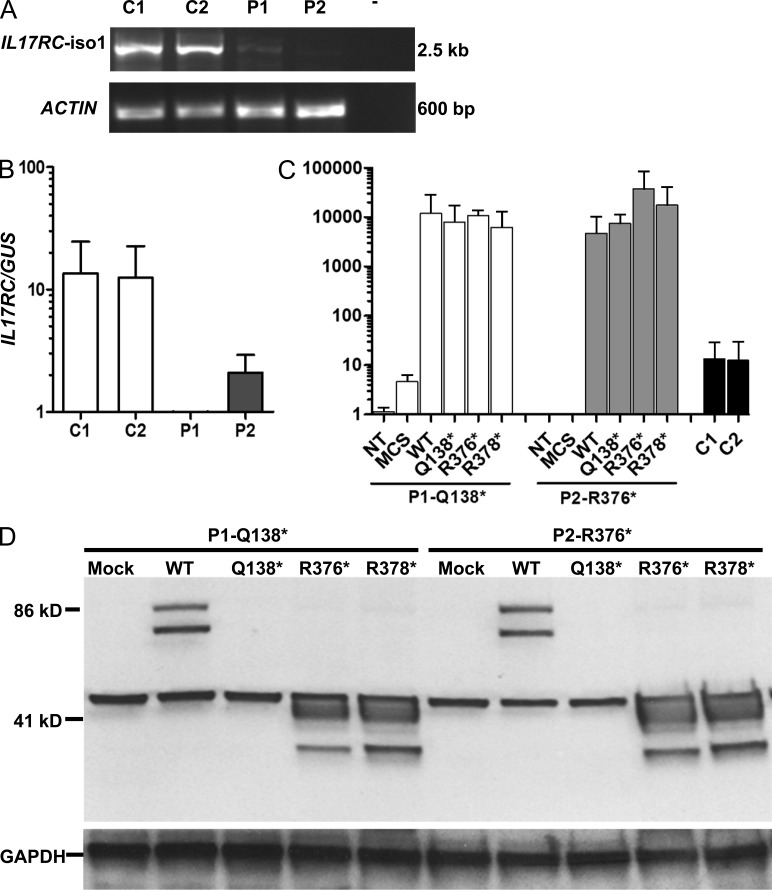
Impaired responses to IL-17A and IL-17F, but normal responses to IL-17E/IL-25
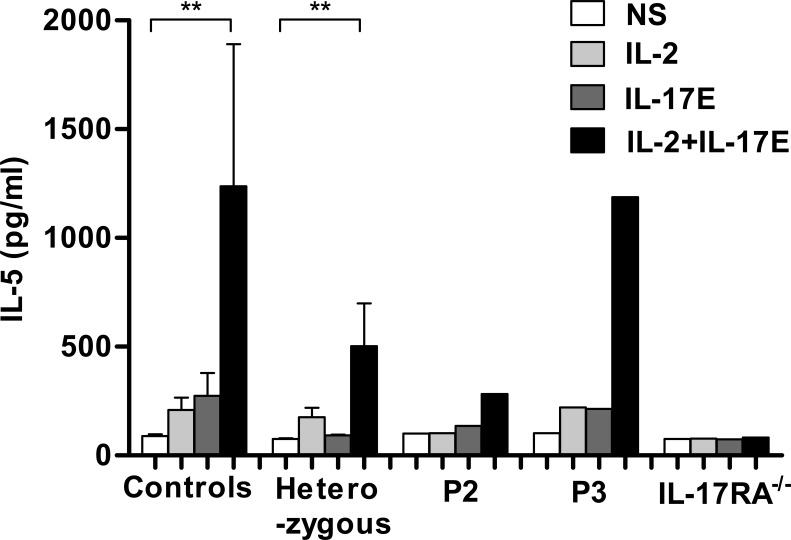
We investigated whether the three IL17RC mutations identified had any functional consequences in terms of the response to IL-17 cytokines by testing the responses of the patients’ fibroblasts to various concentrations (10 and 100 ng/ml) of recombinant IL-17A and IL-17F homodimers and IL-17A/F heterodimers. Unlike fibroblasts from healthy controls, the patients’ fibroblasts did not respond to any of the three IL-17 dimers, whatever the concentration of cytokine used. These results were similar to those obtained for the IL-17RA–deficient patient carrying the homozygous Q284* mutation tested in parallel, in terms of IL-6 and GRO-α (growth-regulated oncogene-α) induction, as assessed by ELISA (Fig. 6, A and B). In contrast, the responses of the patients’ fibroblasts to IL-1β stimulation were within the same range as the controls. Transfection of the patients’ fibroblasts with a WT IL17RC construct, but not with an empty vector or with any of the three mutant constructs, restored the response to IL-17 cytokines in the patients’ fibroblasts (Fig. 7, A and B). In contrast, PBMCs from P2 and P3 stimulated with IL-17E/IL-25 in the presence of IL-2 produced IL-5 to levels in the control range, in contrast to what was observed for PBMCs from an IL-17RA–deficient patient. Thus, IL-17E/IL-25 signaling in humans is dependent on IL-17RA but not IL-17RC (Fig. 8). The three patients described here display a complete form of AR IL-17RC deficiency, with a lack of cellular responses to IL-17A and IL-17F homo- and heterodimers but normal responses to IL-17E/IL-25.
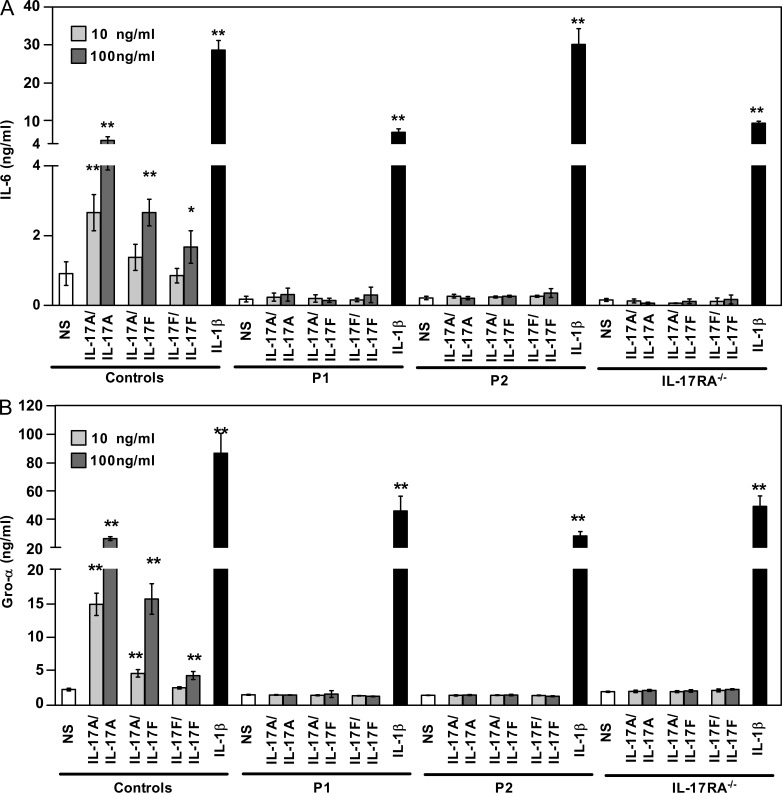
Figure 6.
Responses of P1’s and P2’s fibroblasts to IL-17 cytokines. (A and B) IL-6 (A) and GRO-α (B) production by SV40-immortalized fibroblasts from controls, P1 (IL-17RC Q138*/Q138*), P2 (IL-17RC Q376*/Q376*), and an IL-17RA–deficient patient (IL-17RA Q284*/Q284*), after 24 h of stimulation with IL-17A (10 and 100 ng/ml), IL-17F (10 and 100 ng/ml), and IL-17A/IL-17F (10 and 100 ng/ml), as determined by ELISA on supernatants. Means ± SD (error bars) of three independent experiments are shown. Statistical analyses were performed by the nonparametric statistical test (Mann–Whitney test), comparing NS (nonstimulated) and activated samples (*, P < 0.05; **, P < 0.01). The experiments were repeated at least three times.
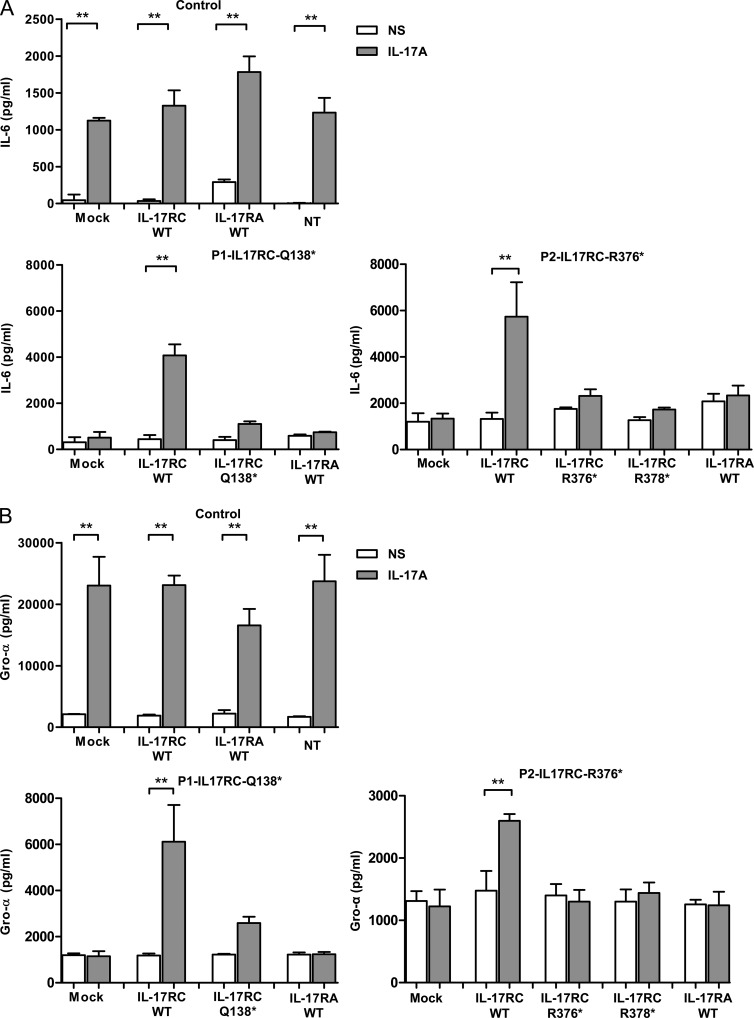
Figure 7.
Production of IL-6 and GRO-α by the patients’ fibroblasts in responses to IL-17 cytokines, after transfection with the WT or mutant IL17RC alleles. (A and B) IL-6 and GRO-α production by SV40-immortalized fibroblasts from a control, P1, P2, and an IL-17RA–deficient patient transfected with an empty vector (mock) or an IL-17RC vector encoding the WT or each one of the mutant (Q138*, R376*, or R378*) proteins, after 24 h of stimulation with 100 ng/ml IL-17A, as determined by ELISA on supernatants. NS, nonstimulated; NT, not transfected. Means ± SD (error bars) of three independent experiments are shown. Statistical analyses were performed by the nonparametric statistical test (Mann–Whitney test; **, P < 0.01). The experiments were repeated at least three times.
Figure 8.
IL-17E/IL-25 response of the patients’ T cells. PBMCs from 14 controls, P2 and P3, 11 healthy heterozygous relatives, and an IL-17RA–deficient patient were cultured in thymic stromal lymphopoietin for 24 h, harvested, and restimulated with IL-2 and IL-17E/IL-25 for an additional 72 h. IL-5 concentrations in the culture supernatants were determined by ELISA. Errors bars represent SEM. Statistical analyses were performed by the nonparametric statistical test (Mann–Whitney test; **, P < 0.01). The experiments were repeated at least three times.
Normal cellular responses to fungal compounds
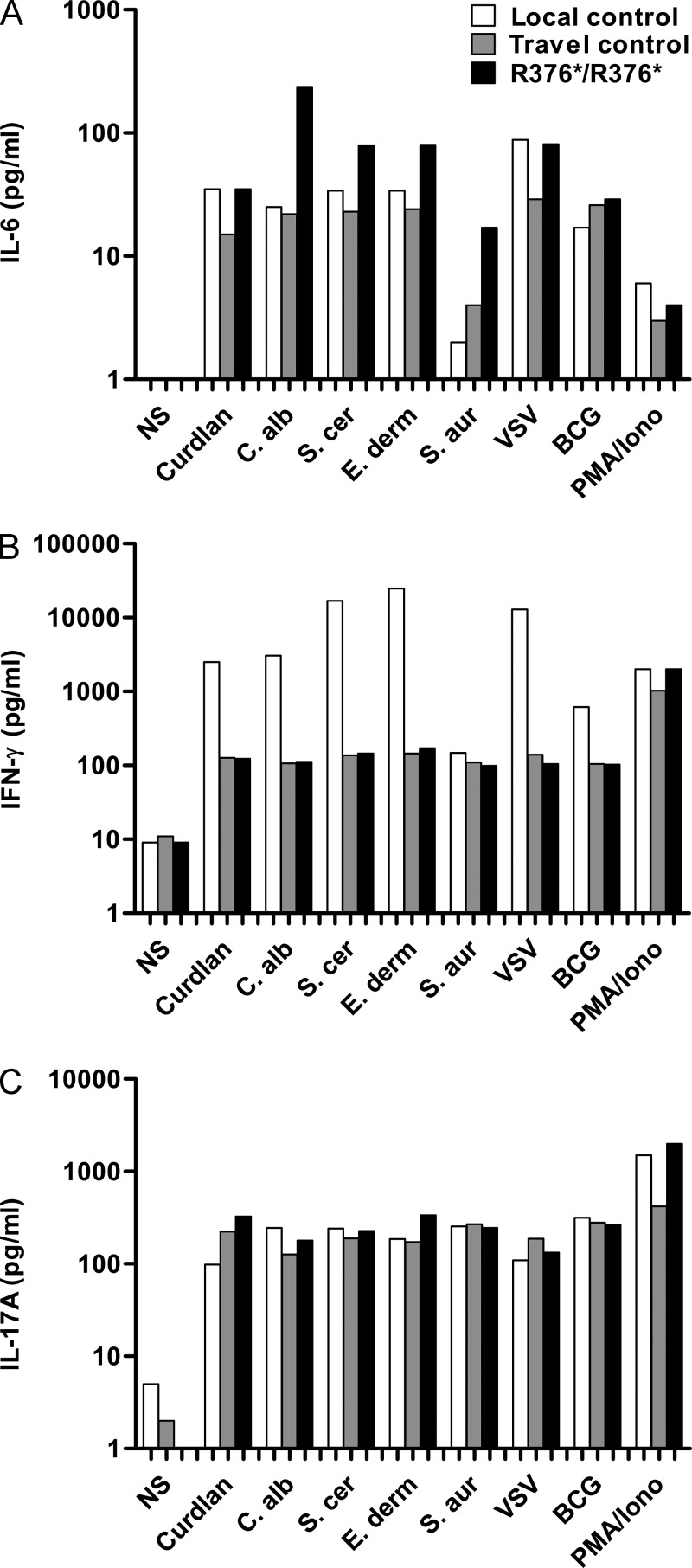
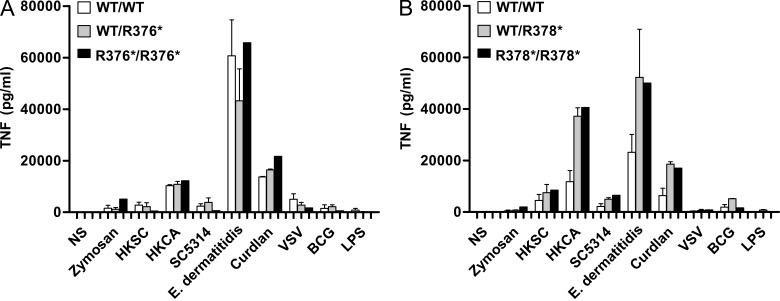
Finally, we investigated IL-6, IFN-γ, and IL-17A production by P2’s whole blood upon 48 h of stimulation with fungal compounds (Curdlan, heat-killed C. albicans, Saccharomyces cerevisiae, and Exophiala dermatitidis), as well as heat-killed Staphylococcus aureus, vesicular stomatitis virus (VSV), bacillus Calmette–Guérin (BCG), and PMA/ionomycin. The levels of all three cytokines produced were comparable with those obtained after whole blood stimulation of a local or a travel control (Fig. 9, A–C). Similarly, monocyte-derived DCs (MDDCs) from P2, P3, and their relatives, activated with various fungal compounds (including zymosan, heat-killed S. cerevisiae, C. albicans, E. dermatitidis, and Curdlan), as well as VSV, BCG, or LPS, produced levels of TNF comparable with the healthy controls tested in the same conditions (Fig. 10, A and B). Altogether, these results suggest that IL-17RC deficiency does not impair the whole blood or MDDC response to fungal compounds, at least for the cytokines measured, including IL-17A. Altogether, these data suggest that the patients’ defective IL-17RC–dependent responsive pathway is primarily responsible for CMC, as it does not affect the production of IL-17A and other cytokines by leukocytes and MDDCs in response to stimulation by C. albicans.
Figure 9.
Normal IL-6, IFN-γ, and IL-17A production by P2’s whole blood upon 48 h of stimulation with fungal compounds. (A–C) Whole blood from a local control (white bars), a travel control (gray bars), and P2 (black bars) were stimulated with fungal compounds (Curdlan, heat-killed C. albicans, S. cerevisiae, E. dermatitidis: a black yeast), as well as heat-killed S. aureus, VSV, BCG, or PMA/ionomycin for 48 h. IL-6 (A), IFN-γ (B), and IL-17A (C) were measured by ELISA. The experiments were repeated two times.
Figure 10.
Normal TNF production by P2’s and P3′s MDDCs upon 48 h of stimulation with fungal compounds. (A and B) MDDCs from four healthy control individuals (white bars), four heterozygous patients’ relatives (gray bars), and P2 or P3 (black bars) were stimulated with fungal compounds (zymosan, heat-killed S. cerevisiae [HKSC], C. albicans [HKCA and SC5314], E. dermatitidis, and Curdlan), as well as with VSV, BCG, or LPS for 48 h. TNF was measured by ELISA. Error bars represent SEM. The experiments were repeated two times.
DISCUSSION
The molecular and cellular basis of human CMC, which is common in patients with various conditions, was eventually deciphered thanks to the study of rare patients with CMCD, in whom CMC appears as the main clinical manifestation, without other severe infectious or autoimmune clinical signs (Puel et al., 2010b, 2012). Four genetic etiologies of CMCD have been described. AR IL-17RA and AD IL-17F deficiencies were the first two genetic etiologies to be discovered, through a candidate gene approach (Puel et al., 2011). IL-17RA deficiency is complete, abolishing cellular responses to IL-17A and IL-17F homo- and heterodimers and to IL-17E/IL-25 (Puel et al., 2011; Boisson et al., 2013). In contrast, IL-17F deficiency is partial, with impairment but not total abolition of the activity of homo- and heterodimers containing the mutant IL-17F (Puel et al., 2011). Genome-wide approaches subsequently led to the discovery of heterozygous GOF mutations of STAT1 as the third and, to date, by far the most frequent genetic etiology of CMCD (Boisson-Dupuis et al., 2012). Stronger STAT1-dependent cellular responses to the STAT1-dependent IL-17 inhibitors IFN-α/β, IFN-γ, and IL-27 and to the STAT3-dependent IL-17 inducers IL-6, IL-21, and IL-23 may account for the poor development of IL-17–producing T cells observed in patients bearing such mutations (Liu et al., 2011). An AR deficiency of the adaptor molecule ACT1 was recently found in two siblings and identified as the fourth genetic etiology of CMCD (Boisson et al., 2013). The patients’ fibroblasts failed to respond to IL-17A and IL-17F, and their T cells did not respond to IL-17E/IL-25 (Boisson et al., 2013). We describe here AR complete IL-17RC deficiency, a new genetic etiology of CMCD, in three unrelated sporadic cases, further documenting the crucial role of human IL-17 immunity in mucocutaneous protection against C. albicans.
IL-17RC, one of the five members of the IL-17 receptor family, is a key component of the IL-17A and IL-17F receptor, as it forms a heterotrimeric receptor complex together with IL-17RA (Moseley et al., 2003; Toy et al., 2006; Weaver et al., 2007; Ely et al., 2009; Gaffen, 2009; Ho and Gaffen, 2010; Ho et al., 2010). Mouse IL-17RC (mIL-17RC), like mIL-17RA (McAllister et al., 2005), is essential for signaling downstream from mIL-17A, mIL-17F, and mIL-17A/F, both in vitro and in vivo (Ho and Gaffen, 2010; Hu et al., 2010), as in humans (Puel et al., 2011). However, mouse and human IL-17RC and IL-17RA have different binding affinities for IL-17A and IL-17F (Kuestner et al., 2007). In humans, IL-17RA binds preferentially to IL-17A and has a lower affinity for IL-17F (Wright et al., 2008). In contrast, IL-17RC binds IL-17A and IL-17F with a similar affinity (Kuestner et al., 2007; Ho and Gaffen, 2010). The opposite situation occurs in mice: mIL-17RA binds mIL-17A and mIL-17F with equal affinities, but mIL-17RC binds preferentially to mIL-17F (Kuestner et al., 2007; Ho and Gaffen, 2010). Moreover, after its heterodimerization with mIL-17RB, mIL-17RA has been shown to be involved in the IL-17E/IL-25 signaling pathway in mice (Rickel et al., 2008; Hu et al., 2010). Consistently, IL-17RA–deficient patients do not respond to IL-17E/IL-25 (Boisson et al., 2013). In contrast, mIL-17RC has not been shown to be part of another receptor (Ho and Gaffen, 2010), at least for mIL-17E/IL-25 signaling (Hu et al., 2011). We show here that IL-17E/IL-25 signaling is normal in humans with IL-17RC deficiency. Our findings demonstrate that human IL-17RC deficiency prevents cellular responses to IL-17A and IL-17F dimers but not to IL-17E/IL-25.
The infectious phenotype of the IL-17RC–deficient patients is consistent with that of mIL-17RC–deficient mice (Ho and Gaffen, 2010; Hu et al., 2010). IL-17RC–deficient mice displayed a large fungal burden in the oral cavity in a model of oropharyngeal candidiasis (OPC; Ho and Gaffen, 2010; Trautwein-Weidner et al., 2015). Likewise, the IL-17RC–deficient patients displayed recurrent or persistent oral candidiasis with or without skin and/or nail involvement from early infancy onward. This phenotype, restricted to isolated CMC, is similar to that of patients with AD IL-17F, AR IL-17RA, and AR ACT1 deficiencies (Puel et al., 2011; Boisson et al., 2013). However, patients with AR IL-17RA and AR ACT1 deficiencies also display peripheral staphylococcal infections, such as dermatitis (Puel et al., 2011) and blepharitis (Boisson et al., 2013). It is tempting to speculate that these infections might result, at least in part, from impaired IL-17E/IL-25 responses, which are normal in IL-17F– and IL-17RC–deficient patients. Susceptibility to cutaneous staphylococcal disease has been observed in mIL-17RA–deficient mice (Aujla et al., 2007; Curtis and Way, 2009; Vidlak and Kielian, 2012; Aldave et al., 2013). Spontaneous occurrence of peripheral S. aureus infection was also observed in double mIL-17A/mIL-17F but not in single mIL-17A or mIL-17F knockout mice (Ishigame et al., 2009). mIL-17RC– and mACT1-deficient mice have yet to be tested. Finally, patients with AD STAT1 GOF have a broader infectious phenotype, which is probably the result of the broader cellular impact of the mutations (unpublished data). Overall, our data demonstrate that human IL-17 signaling via IL-17RC is essential for mucocutaneous immunity to C. albicans, but suggest that this signaling is redundant for immunity to most other common pathogens, even possibly including S. aureus. Moreover, human IL-17RC is not required for cellular responses to IL-17E/IL-25.
MATERIALS AND METHODS
Molecular genetics.
Genomic DNA was isolated from whole blood by a phenol/chloroform extraction method. IL17RC cDNA was amplified with specific primers. PCR products were analyzed by electrophoresis in 1% agarose gels, sequenced with the Big Dye Terminator cycle sequencing kit (Applied Biosystems), and analyzed on an ABI Prism 3700 apparatus (Applied Biosystems).
Massively parallel sequencing.
3 µg genomic DNA was extracted from the peripheral blood cells of the patients and sheared with an S2 Ultrasonicator (Covaris). An adaptor-ligated library was prepared with the Paired-End Sample Prep kit V1 (Illumina). Exome capture was performed with the SureSelect Human All Exon kit (Agilent Technologies). Single-end sequencing was performed on a Genome Analyzer IIx (Illumina), generating 72 base reads.
Cell purification and culture.
Human PBMCs were isolated from whole blood by Ficoll-Hypaque density gradient centrifugation (GE Healthcare). Primary human fibroblasts, obtained from skin biopsy specimens, were immortalized with SV40T antigen (SV40 fibroblasts) and cultured in DMEM (Gibco, Invitrogen) supplemented with 10% FBS (Gibco, Invitrogen). HEK-293T cells were cultured in DMEM supplemented with 10% FBS. All cells were grown at 37°C, under an atmosphere containing 5% CO2.
RT-PCR for full-length IL-17RC and TaqMan probe detection.
Total RNA was extracted with the RNeasy Mini kit (QIAGEN) and reversed-transcribed to generate cDNA with the High-Capacity cDNA Reverse Transcription kit (Invitrogen). Platinum High-Fidelity Taq DNA Polymerase (Invitrogen) was then used to amplify the full-length IL17RC cDNA.
The following primers were used: F, 5′-CTGAAGAGGGATTCCAGCCC-3′ and R, 5′-GTAGAAAAACAGCGTCTGCC-3′. TaqMan probes for IL-17RC (Invitrogen) were used to detect mRNA, and the results were normalized against those for GUS (Human GUSB Endogenous Control VIC/MGB Probe; Primer Limited, Invitrogen).
IL-17RC detection by Western blotting.
Total protein extracts were prepared from SV40 fibroblasts or HEK-293T cells 48 h after transfection. The proteins were separated by electrophoresis. The bands were electroblotted onto a membrane, which was then probed with an antibody against IL-17RC (Sigma-Aldrich) or GAPDH (Santa Cruz Biotechnology, Inc.).
Fibroblast activation.
SV40-transformed fibroblasts were plated in 48-well plates at a density of 50,000 cells/well in 0.5 ml DMEM/10% FBS per well. The cells were incubated for 24 h and were then left unstimulated or were stimulated for 24 h with various amounts of IL-17 cytokines, recombinant human IL-17A, IL-17F, IL-17A/F, and IL-1β (from R&D Systems). 24 h later, supernatants were collected and IL-6 (Sanquin or R&D Systems) and GRO-α (R&D Systems) levels were assessed with ELISA kits, according to the manufacturer’s instructions.
PBMC culture.
Frozen PBMCs were cultured in the presence of 100 ng/ml thymic stromal lymphopoietin (R&D Systems) in X-VIVO 15 (Lonza) plus 5% human AB serum (Lonza), as previously described (Rickel et al., 2008). PBMCs were collected, washed, and resuspended at a density of 4 × 106 cells/well in 48-well plates, in a final volume of 0.5 ml/well, in the presence of 10 ng/ml recombinant human IL-2 (R&D Systems) and 10 ng/ml recombinant human IL-17E/IL-25 (R&D Systems). After 3 d, the amount of IL-5 secreted into the medium was determined with ELISA kits (R&D Systems).
PBMC activation.
The levels of IL-17A– and IL-22–producing T cells were evaluated by intracellular staining or by ELISA, as previously described (de Beaucoudrey et al., 2008). In brief, PBMCs were purified by centrifugation on a gradient (Ficoll-Paque PLUS; GE Healthcare) and resuspended in RPMI supplemented with 10% FBS (RPMI/10% FBS; Invitrogen). Adherent monocytes were removed from the PBMC preparation by incubation for 2 h at 37°C, under an atmosphere containing 5% CO2. For the ex vivo evaluation of IL-17– and IL-22–producing T cells by flow cytometry, we resuspended 5 × 106 nonadherent cells in 5 ml RPMI/10% FBS in 25-cm2 flasks and stimulated them by incubation with 40 ng/ml PMA (Sigma-Aldrich) and 10−5 M ionomycin (Sigma-Aldrich) in the presence of a secretion inhibitor (1 µl/ml GolgiPlug; BD) for 12 h. For the evaluation of the IL-17– and IL-22–producing T cell blasts after in vitro differentiation, the nonadherent PBMCs were dispensed into 24-well plates at a density of 2.5 × 106 cells/ml in RPMI/10% FBS and activated by incubation with 2 µg/ml of an antibody directed against CD3 (Orthoclone OKT3; Janssen-Cilag) either alone or together with 20 ng/ml IL-23 (R&D Systems), 50 ng/ml IL-6 (R&D Systems), 10 ng/ml IL-1β (R&D Systems), or combinations of these three cytokines. After incubation for 3 d, the cells were restimulated in the same activation conditions, except that the anti-CD3 antibody was replaced with 40 IU/ml IL-2 (Proleukin i.v.; Chiron). We added 1 ml of the appropriate medium, resuspended the cells by gentle pipetting, and then split the cell suspension from each well into two. Flow cytometry was performed on one of the duplicated wells 2 d later, after stimulation by incubation for 12 h with 40 ng/ml PMA and 10−5 M ionomycin in the presence of 1 µl/ml GolgiPlug. Cells were washed in cold PBS, and surface labeling was achieved by incubating the cells with VioBlue-anti–human CD3 (Miltenyi Biotec) or FITC-anti–human CD4 (BD) antibody in 2% FBS in PBS for 20 min on ice. The cells were then washed twice with 2% FBS in cold PBS, fixed by incubation with 100 µl Cytofix for 30 min on ice, and washed twice with Cytoperm (Cytofix/Cytoperm Plus fixation/permeabilization kit; BD). The cells were then incubated for 1 h on ice with Alexa Fluor 488–conjugated anti–human IL-17A (eBioscience), IL-17F PE-conjugated anti–human IL-22 (R&D Systems), or PE-conjugated anti–human IFN-γ (R&D Systems) antibodies, washed twice with Cytoperm, and analyzed with a FACSCanto II system (BD).The contents of the other duplicated well were split into two, with one half left unstimulated and the other stimulated by incubation with 40 ng/ml PMA and 10−5 M ionomycin for another 2 d. Supernatants were collected after 48 h of incubation for ELISA.
Flow cytometry.
SV40 fibroblasts were plated in 24-well plates at a density of 50,000 cells/well, in 0.5 ml of 10% FBS in DMEM per well. The plates were incubated for 24 h. The cells were then subjected to flow cytometry. SV40-transformed fibroblasts or PBMCs were labeled with PE-mouse IgG1 (eBioscience), APC-mouse IgG1 (eBioscience), Alexa Fluor 647 mouse IgG1, κ isotype ctrl (FC) antibody (Sony Biotechnology, Inc.), VioGreen-mouse IgG2a (Miltenyi Biotec), VioBlue-mouse IgG2a (Miltenyi Biotec), FITC-mouse IgG1 (BD), FITC-mouse IgG2b (BD), and PE-mouse IgG1 (BD) antibodies or Alexa Fluor 647–mouse IgG1 (eBioscience) isotype antibodies as a control. PE-anti–human IL-17RA (clone J10MBS; eBioscience), APC-anti–human IL-17RA (clone 424LTS; eBioscience), Alexa Fluor 647 anti–human CD217 (IL-17RA) antibody (Sony Biotechnology, Inc.), VioGreen-anti–human CD14 (Miltenyi Biotec), VioBlue-anti–human CD3 (Miltenyi Biotec), FITC-anti–human CD4 (BD), FITC-anti–human CD8 (BD), FITC-anti–human CD14 (BD), FITC-anti–human CD19 (BD), and FITC-anti–human CD56 (BD) specific antibodies were used according to the manufacturers’ instructions, with the results analyzed by flow cytometry on a FACSCanto II system.
The TIRF assay.
The TIRF assay was performed on the transfected HEK-293T cells as described in “Cell purification and culture.” V5 tag–IL-17RC WT and mutant (Q138*, R376*, and R378*) vectors were constructed at the N terminus by the pcDNA3.1 Directional TOPO Expression kit (Life Technologies). After being fixed in 3.7% paraformaldehyde, the cells coated glass coverslips and were incubated with anti-V5 antibody (Life Technologies) and Phalloidin (Life Technologies) for 3 h at room temperature. After being washed, the glass coverslips were incubated with anti–mouse Alexa Fluor 488 (Life Technologies) for 1 h at room temperature and then stained with DAPI (Sigma-Aldrich). Fluorescence data were acquired with the Eclipse Ti-E TIRF imaging system (Nikon). Images were recorded with the QuanTEM 512 SC camera (Roper Scientific) and acquired with NIS-Elements AR software (version 3.1; Nikon). Image sets were processed with ImageJ version 1.43 software (National Institutes of Health).
Cell complementation.
IL-17RC–deficient and IL-17RA–deficient SV40 fibroblasts were transfected with empty pUNO1-msc vectors, pUNO1–hIL-17RCa encoding WT human IL-17RC, or pUNO1–hIL-17RA encoding WT human IL-17RA (InvivoGen) with the Lipofectamine LTX transfection kit (Invitrogen), used according to the manufacturer’s instructions. The cells were incubated for 24 h and then stimulated with IL-17A, IL-17F, and IL-17A/F (R&D Systems) at a concentration of 10 or 100 ng/ml. After 24 h, supernatants were harvested for the assessment of IL-6 and Gro-α levels by ELISA, and cells were collected for the evaluation of IL-17RC expression by FACS analysis.
Statistical analysis.
Data were analyzed with the nonparametric statistical test (Mann–Whitney test) with Prism software (GraphPad Software), and P < 0.05 or P < 0.01 was considered statistically significant. Biological proximities between IL17RC and the known CMC-causing genes IL17RA and ACT1 were estimated using the human gene connectome method and its online server (Itan et al., 2014).
Healthy controls.
The healthy controls were volunteer blood donors originating from the European Union, Turkey, or Argentina.
Acknowledgments
We thank the members of the laboratory for helpful discussions; Yelena Nemiroskaya, Eric Anderson, Martine Courat, and Lahouari Amar for expert administrative assistance; and Luyan Liu, Malik Bensif, Maya Chrabieh, and Lazaro Lorenzo-Diaz for expert technical assistance.
This work was supported by grants from the French National Research Agency (ANR GENCMCD 11-BSV3–005-01) and the Jeffrey Modell foundation to A. Puel, ANR under the Investissement d’avenir program (ANR-10-IAHU-01), Laboratoire d’Excellence “Integrative Biology of Emerging Infectious Diseases” (ANR-10-LABX-62-IBEID), the Jeffrey Modell Center Network, the St. Giles Foundation, the Rockefeller University, Institut National de la Santé et de la Recherche Médicale (INSERM), and Paris Descartes University. S. Cypowyj and Y. Itan were supported by the AXA Research Fund. Y. Ling was supported by the INSERM international postdoctoral program.
The authors declare no competing financial interests.
Footnotes
Abbreviations used:
- AD
- autosomal dominant
- AR
- autosomal recessive
- BCG
- bacillus Calmette–Guérin
- CMC
- chronic mucocutaneous candidiasis
- CMCD
- CMC disease
- GOF
- gain-of-function
- MDDC
- monocyte-derived DC
- TIRF
- total internal reflection fluorescence
- VSV
- vesicular stomatitis virus
- WES
- whole-exome sequencing
References
- Al Rushood M., McCusker C., Mazer B., Alizadehfar R., Grimbacher B., Depner M., and Ben-Shoshan M.. 2013. Autosomal dominant cases of chronic mucocutaneous candidiasis segregates with mutations of signal transducer and activator of transcription 1, but not of Toll-like receptor 3. J. Pediatr. 163:277–279 10.1016/j.jpeds.2013.02.040 [DOI] [PubMed] [Google Scholar]
- Aldave J.C., Cachay E., Núñez L., Chunga A., Murillo S., Cypowyj S., Bustamante J., Puel A., Casanova J.L., and Koo A.. 2013. A 1-year-old girl with a gain-of-function STAT1 mutation treated with hematopoietic stem cell transplantation. J. Clin. Immunol. 33:1273–1275 10.1007/s10875-013-9947-5 [DOI] [PubMed] [Google Scholar]
- Aujla S.J., Dubin P.J., and Kolls J.K.. 2007. Th17 cells and mucosal host defense. Semin. Immunol. 19:377–382 10.1016/j.smim.2007.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisson B., Wang C., Pedergnana V., Wu L., Cypowyj S., Rybojad M., Belkadi A., Picard C., Abel L., Fieschi C., et al. . 2013. An ACT1 mutation selectively abolishes interleukin-17 responses in humans with chronic mucocutaneous candidiasis. Immunity. 39:676–686 10.1016/j.immuni.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boisson-Dupuis S., Kong X.F., Okada S., Cypowyj S., Puel A., Abel L., and Casanova J.L.. 2012. Inborn errors of human STAT1: allelic heterogeneity governs the diversity of immunological and infectious phenotypes. Curr. Opin. Immunol. 24:364–378 10.1016/j.coi.2012.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne S.K., and Holland S.M.. 2010. Immunodeficiency secondary to anticytokine autoantibodies. Curr. Opin. Allergy Clin. Immunol. 10:534–541 10.1097/ACI.0b013e3283402b41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova J.L., and Abel L.. 2013. The genetic theory of infectious diseases: a brief history and selected illustrations. Annu. Rev. Genomics Hum. Genet. 14:215–243 10.1146/annurev-genom-091212-153448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova J.L., Abel L., and Quintana-Murci L.. 2013. Immunology taught by human genetics. Cold Spring Harb. Symp. Quant. Biol. 78:157–172 10.1101/sqb.2013.78.019968 [DOI] [PubMed] [Google Scholar]
- Casanova J.L., Conley M.E., Seligman S.J., Abel L., and Notarangelo L.D.. 2014. Guidelines for genetic studies in single patients: lessons from primary immunodeficiencies. J. Exp. Med. 211:2137–2149 10.1084/jem.20140520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandesris M.O., Melki I., Natividad A., Puel A., Fieschi C., Yun L., Thumerelle C., Oksenhendler E., Boutboul D., Thomas C., et al. . 2012. Autosomal dominant STAT3 deficiency and hyper-IgE syndrome: molecular, cellular, and clinical features from a French national survey. Medicine (Baltimore). 91:e1–e19 10.1097/MD.0b013e31825f95b9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis M.M., and Way S.S.. 2009. Interleukin-17 in host defence against bacterial, mycobacterial and fungal pathogens. Immunology. 126:177–185 10.1111/j.1365-2567.2008.03017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cypowyj S., Picard C., Maródi L., Casanova J.L., and Puel A.. 2012. Immunity to infection in IL-17-deficient mice and humans. Eur. J. Immunol. 42:2246–2254 10.1002/eji.201242605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beaucoudrey L., Puel A., Filipe-Santos O., Cobat A., Ghandil P., Chrabieh M., Feinberg J., von Bernuth H., Samarina A., Jannière L., et al. . 2008. Mutations in STAT3 and IL12RB1 impair the development of human IL-17–producing T cells. J. Exp. Med. 205:1543–1550 10.1084/jem.20080321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Beaucoudrey L., Samarina A., Bustamante J., Cobat A., Boisson-Dupuis S., Feinberg J., Al-Muhsen S., Jannière L., Rose Y., de Suremain M., et al. . 2010. Revisiting human IL-12Rβ1 deficiency: a survey of 141 patients from 30 countries. Medicine (Baltimore). 89:381–402 10.1097/MD.0b013e3181fdd832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely L.K., Fischer S., and Garcia K.C.. 2009. Structural basis of receptor sharing by interleukin 17 cytokines. Nat. Immunol. 10:1245–1251 10.1038/ni.1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhardt K.R., and Grimbacher B.. 2012. Mendelian traits causing susceptibility to mucocutaneous fungal infections in human subjects. J. Allergy Clin. Immunol. 129:294–305 10.1016/j.jaci.2011.12.966 [DOI] [PubMed] [Google Scholar]
- Frans G., Moens L., Schaballie H., Van Eyck L., Borgers H., Wuyts M., Dillaerts D., Vermeulen E., Dooley J., Grimbacher B., et al. . 2014. Gain-of-function mutations in signal transducer and activator of transcription 1 (STAT1): chronic mucocutaneous candidiasis accompanied by enamel defects and delayed dental shedding. J. Allergy Clin. Immunol. 134:1209–1213 10.1016/j.jaci.2014.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaffen S.L.2009. Structure and signalling in the IL-17 receptor family. Nat. Rev. Immunol. 9:556–567 10.1038/nri2586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glocker E.O., Hennigs A., Nabavi M., Schäffer A.A., Woellner C., Salzer U., Pfeifer D., Veelken H., Warnatz K., Tahami F., et al. . 2009. A homozygous CARD9 mutation in a family with susceptibility to fungal infections. N. Engl. J. Med. 361:1727–1735 10.1056/NEJMoa0810719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho A.W., and Gaffen S.L.. 2010. IL-17RC: a partner in IL-17 signaling and beyond. Semin. Immunopathol. 32:33–42 10.1007/s00281-009-0185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho A.W., Shen F., Conti H.R., Patel N., Childs E.E., Peterson A.C., Hernández-Santos N., Kolls J.K., Kane L.P., Ouyang W., and Gaffen S.L.. 2010. IL-17RC is required for immune signaling via an extended SEF/IL-17R signaling domain in the cytoplasmic tail. J. Immunol. 185:1063–1070 10.4049/jimmunol.0903739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hori T., Ohnishi H., Teramoto T., Tsubouchi K., Naiki T., Hirose Y., Ohara O., Seishima M., Kaneko H., Fukao T., and Kondo N.. 2012. Autosomal-dominant chronic mucocutaneous candidiasis with STAT1-mutation can be complicated with chronic active hepatitis and hypothyroidism. J. Clin. Immunol. 32:1213–1220 10.1007/s10875-012-9744-6 [DOI] [PubMed] [Google Scholar]
- Hu Y., Ota N., Peng I., Refino C.J., Danilenko D.M., Caplazi P., and Ouyang W.. 2010. IL-17RC is required for IL-17A- and IL-17F-dependent signaling and the pathogenesis of experimental autoimmune encephalomyelitis. J. Immunol. 184:4307–4316 10.4049/jimmunol.0903614 [DOI] [PubMed] [Google Scholar]
- Hu Y., Shen F., Crellin N.K., and Ouyang W.. 2011. The IL-17 pathway as a major therapeutic target in autoimmune diseases. Ann. N. Y. Acad. Sci. 1217:60–76 10.1111/j.1749-6632.2010.05825.x [DOI] [PubMed] [Google Scholar]
- Huppler A.R., Bishu S., and Gaffen S.L.. 2012. Mucocutaneous candidiasis: the IL-17 pathway and implications for targeted immunotherapy. Arthritis Res. Ther. 14:217 10.1186/ar3893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husebye E.S., and Anderson M.S.. 2010. Autoimmune polyendocrine syndromes: clues to type 1 diabetes pathogenesis. Immunity. 32:479–487 10.1016/j.immuni.2010.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishigame H., Kakuta S., Nagai T., Kadoki M., Nambu A., Komiyama Y., Fujikado N., Tanahashi Y., Akitsu A., Kotaki H., et al. . 2009. Differential roles of interleukin-17A and -17F in host defense against mucoepithelial bacterial infection and allergic responses. Immunity. 30:108–119 10.1016/j.immuni.2008.11.009 [DOI] [PubMed] [Google Scholar]
- Itan Y., Zhang S.Y., Vogt G., Abhyankar A., Herman M., Nitschke P., Fried D., Quintana-Murci L., Abel L., and Casanova J.L.. 2013. The human gene connectome as a map of short cuts for morbid allele discovery. Proc. Natl. Acad. Sci. USA. 110:5558–5563 10.1073/pnas.1218167110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Itan Y., Mazel M., Mazel B., Abhyankar A., Nitschke P., Quintana-Murci L., Boisson-Dupuis S., Boisson B., Abel L., and Casanova J.L.. 2014. HGCS: an online tool for prioritizing disease-causing gene variants by biological distance. BMC Genomics. 15:256 10.1186/1471-2164-15-256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilic S.S., Puel A., and Casanova J.L.. 2014. Orf infection in a patient with Stat1 gain-of-function. J. Clin. Immunol. In press. [DOI] [PubMed] [Google Scholar]
- Kisand K., Bøe Wolff A.S., Podkrajsek K.T., Tserel L., Link M., Kisand K.V., Ersvaer E., Perheentupa J., Erichsen M.M., Bratanic N., et al. . 2010. Chronic mucocutaneous candidiasis in APECED or thymoma patients correlates with autoimmunity to Th17-associated cytokines. J. Exp. Med. 207:299–308 10.1084/jem.20091669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisand K., Lilic D., Casanova J.L., Peterson P., Meager A., and Willcox N.. 2011. Mucocutaneous candidiasis and autoimmunity against cytokines in APECED and thymoma patients: clinical and pathogenetic implications. Eur. J. Immunol. 41:1517–1527 10.1002/eji.201041253 [DOI] [PubMed] [Google Scholar]
- Kuestner R.E., Taft D.W., Haran A., Brandt C.S., Brender T., Lum K., Harder B., Okada S., Ostrander C.D., Kreindler J.L., et al. . 2007. Identification of the IL-17 receptor related molecule IL-17RC as the receptor for IL-17F. J. Immunol. 179:5462–5473 10.4049/jimmunol.179.8.5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanternier F., Pathan S., Vincent Q.B., Liu L., Cypowyj S., Prando C., Migaud M., Taibi L., Ammar-Khodja A., Boudghene Stambouli O., et al. . 2013. Deep dermatophytosis and inherited CARD9 deficiency. N. Engl. J. Med. 369:1704–1714 10.1056/NEJMoa1208487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee P.P., Mao H., Yang W., Chan K.W., Ho M.H., Lee T.L., Chan J.F., Woo P.C., Tu W., and Lau Y.L.. 2014. Penicillium marneffei infection and impaired IFN-γ immunity in humans with autosomal-dominant gain-of-phosphorylation STAT1 mutations. J. Allergy Clin. Immunol. 133:894–896 10.1016/j.jaci.2013.08.051 [DOI] [PubMed] [Google Scholar]
- Ling Y., and Puel A.. 2014. IL-17 and infections. Actas Dermosifiliogr. 105:34–40 10.1016/S0001-7310(14)70016-X [DOI] [PubMed] [Google Scholar]
- Lionakis M.S.2012. Genetic susceptibility to fungal infections in humans. Curr. Fungal Infect. Rep. 6:11–22 10.1007/s12281-011-0076-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Okada S., Kong X.F., Kreins A.Y., Cypowyj S., Abhyankar A., Toubiana J., Itan Y., Audry M., Nitschke P., et al. . 2011. Gain-of-function human STAT1 mutations impair IL-17 immunity and underlie chronic mucocutaneous candidiasis. J. Exp. Med. 208:1635–1648 10.1084/jem.20110958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma C.S., Chew G.Y., Simpson N., Priyadarshi A., Wong M., Grimbacher B., Fulcher D.A., Tangye S.G., and Cook M.C.. 2008. Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. J. Exp. Med. 205:1551–1557 10.1084/jem.20080218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAllister F., Henry A., Kreindler J.L., Dubin P.J., Ulrich L., Steele C., Finder J.D., Pilewski J.M., Carreno B.M., Goldman S.J., et al. . 2005. Role of IL-17A, IL-17F, and the IL-17 receptor in regulating growth-related oncogene-α and granulocyte colony-stimulating factor in bronchial epithelium: implications for airway inflammation in cystic fibrosis. J. Immunol. 175:404–412 10.4049/jimmunol.175.1.404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekki N., Ben-Mustapha I., Liu L., Boussofara L., Okada S., Cypowyj S., Ghariani N., Saidi W., Denguezli M., Casanova J.L., et al. . 2014. IL-17 T cells’ defective differentiation in vitro despite normal range ex vivo in chronic mucocutaneous candidiasis due to STAT1 mutation. J. Invest. Dermatol. 134:1155–1157 10.1038/jid.2013.480 [DOI] [PubMed] [Google Scholar]
- Milner J.D., Brenchley J.M., Laurence A., Freeman A.F., Hill B.J., Elias K.M., Kanno Y., Spalding C., Elloumi H.Z., Paulson M.L., et al. . 2008. Impaired TH17 cell differentiation in subjects with autosomal dominant hyper-IgE syndrome. Nature. 452:773–776 10.1038/nature06764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizoguchi Y., Tsumura M., Okada S., Hirata O., Minegishi S., Imai K., Hyakuna N., Muramatsu H., Kojima S., Ozaki Y., et al. . 2014. Simple diagnosis of STAT1 gain-of-function alleles in patients with chronic mucocutaneous candidiasis. J. Leukoc. Biol. 95:667–676 10.1189/jlb.0513250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moseley T.A., Haudenschild D.R., Rose L., and Reddi A.H.. 2003. Interleukin-17 family and IL-17 receptors. Cytokine Growth Factor Rev. 14:155–174 10.1016/S1359-6101(03)00002-9 [DOI] [PubMed] [Google Scholar]
- Ouederni M., Sanal O., Ikinciogullari A., Tezcan I., Dogu F., Sologuren I., Pedraza-Sánchez S., Keser M., Tanir G., Nieuwhof C., et al. . 2014. Clinical features of candidiasis in patients with inherited interleukin 12 receptor β1 deficiency. Clin. Infect. Dis. 58:204–213 10.1093/cid/cit722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prando C., Samarina A., Bustamante J., Boisson-Dupuis S., Cobat A., Picard C., AlSum Z., Al-Jumaah S., Al-Hajjar S., Frayha H., et al. . 2013. Inherited IL-12p40 deficiency: genetic, immunologic, and clinical features of 49 patients from 30 kindreds. Medicine (Baltimore). 92:109–122 (published erratum appears in Medicine (Baltimore). 2013. 92:190) 10.1097/MD.0b013e31828a01f9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puel A., Döffinger R., Natividad A., Chrabieh M., Barcenas-Morales G., Picard C., Cobat A., Ouachée-Chardin M., Toulon A., Bustamante J., et al. . 2010a. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J. Exp. Med. 207:291–297 10.1084/jem.20091983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puel A., Picard C., Cypowyj S., Lilic D., Abel L., and Casanova J.L.. 2010b. Inborn errors of mucocutaneous immunity to Candida albicans in humans: a role for IL-17 cytokines? Curr. Opin. Immunol. 22:467–474 10.1016/j.coi.2010.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puel A., Cypowyj S., Bustamante J., Wright J.F., Liu L., Lim H.K., Migaud M., Israel L., Chrabieh M., Audry M., et al. . 2011. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 332:65–68 10.1126/science.1200439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puel A., Cypowyj S., Maródi L., Abel L., Picard C., and Casanova J.L.. 2012. Inborn errors of human IL-17 immunity underlie chronic mucocutaneous candidiasis. Curr. Opin. Allergy Clin. Immunol. 12:616–622 10.1097/ACI.0b013e328358cc0b [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell S., Neale B., Todd-Brown K., Thomas L., Ferreira M.A., Bender D., Maller J., Sklar P., de Bakker P.I., Daly M.J., and Sham P.C.. 2007. PLINK: a tool set for whole-genome association and population-based linkage analyses. Am. J. Hum. Genet. 81:559–575 10.1086/519795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renner E.D., Rylaarsdam S., Anover-Sombke S., Rack A.L., Reichenbach J., Carey J.C., Zhu Q., Jansson A.F., Barboza J., Schimke L.F., et al. . 2008. Novel signal transducer and activator of transcription 3 (STAT3) mutations, reduced TH17 cell numbers, and variably defective STAT3 phosphorylation in hyper-IgE syndrome. J. Allergy Clin. Immunol. 122:181–187 10.1016/j.jaci.2008.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickel E.A., Siegel L.A., Yoon B.R., Rottman J.B., Kugler D.G., Swart D.A., Anders P.M., Tocker J.E., Comeau M.R., and Budelsky A.L.. 2008. Identification of functional roles for both IL-17RB and IL-17RA in mediating IL-25-induced activities. J. Immunol. 181:4299–4310 10.4049/jimmunol.181.6.4299 [DOI] [PubMed] [Google Scholar]
- Romberg N., Morbach H., Lawrence M.G., Kim S., Kang I., Holland S.M., Milner J.D., and Meffre E.. 2013. Gain-of-function STAT1 mutations are associated with PD-L1 overexpression and a defect in B-cell survival. J. Allergy Clin. Immunol. 131:1691–1693 10.1016/j.jaci.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampaio E.P., Hsu A.P., Pechacek J., Bax H.I., Dias D.L., Paulson M.L., Chandrasekaran P., Rosen L.B., Carvalho D.S., Ding L., et al. . 2013. Signal transducer and activator of transcription 1 (STAT1) gain-of-function mutations and disseminated coccidioidomycosis and histoplasmosis. J. Allergy Clin. Immunol. 131:1624–1634 10.1016/j.jaci.2013.01.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharfe N., Nahum A., Newell A., Dadi H., Ngan B., Pereira S.L., Herbrick J.A., and Roifman C.M.. 2014. Fatal combined immunodeficiency associated with heterozygous mutation in STAT1. J. Allergy Clin. Immunol. 133:807–817 10.1016/j.jaci.2013.09.032 [DOI] [PubMed] [Google Scholar]
- Smeekens S.P., Plantinga T.S., van de Veerdonk F.L., Heinhuis B., Hoischen A., Joosten L.A., Arkwright P.D., Gennery A., Kullberg B.J., Veltman J.A., et al. . 2011. STAT1 hyperphosphorylation and defective IL12R/IL23R signaling underlie defective immunity in autosomal dominant chronic mucocutaneous candidiasis. PLoS ONE. 6:e29248 10.1371/journal.pone.0029248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltész B., Tóth B., Shabashova N., Bondarenko A., Okada S., Cypowyj S., Abhyankar A., Csorba G., Taskó S., Sarkadi A.K., et al. . 2013. New and recurrent gain-of-function STAT1 mutations in patients with chronic mucocutaneous candidiasis from Eastern and Central Europe. J. Med. Genet. 50:567–578 10.1136/jmedgenet-2013-101570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takezaki S., Yamada M., Kato M., Park M.J., Maruyama K., Yamazaki Y., Chida N., Ohara O., Kobayashi I., and Ariga T.. 2012. Chronic mucocutaneous candidiasis caused by a gain-of-function mutation in the STAT1 DNA-binding domain. J. Immunol. 189:1521–1526 10.4049/jimmunol.1200926 [DOI] [PubMed] [Google Scholar]
- Tóth B., Méhes L., Taskó S., Szalai Z., Tulassay Z., Cypowyj S., Casanova J.L., Puel A., and Maródi L.. 2012. Herpes in STAT1 gain-of-function mutation [corrected]. Lancet. 379:2500 10.1016/S0140-6736(12)60365-1 [DOI] [PubMed] [Google Scholar]
- Toy D., Kugler D., Wolfson M., Vanden Bos T., Gurgel J., Derry J., Tocker J., and Peschon J.. 2006. Cutting edge: interleukin 17 signals through a heteromeric receptor complex. J. Immunol. 177:36–39 10.4049/jimmunol.177.1.36 [DOI] [PubMed] [Google Scholar]
- Trautwein-Weidner K., Gladiator A., Nur S., Diethelm P., and LeibundGut-Landmann S.. 2015. IL-17-mediated antifungal defense in the oral mucosa is independent of neutrophils. Mucosal Immunol. 8:221–231 10.1038/mi.2014.57 [DOI] [PubMed] [Google Scholar]
- Uzel G., Sampaio E.P., Lawrence M.G., Hsu A.P., Hackett M., Dorsey M.J., Noel R.J., Verbsky J.W., Freeman A.F., Janssen E., et al. . 2013. Dominant gain-of-function STAT1 mutations in FOXP3 wild-type immune dysregulation-polyendocrinopathy-enteropathy-X-linked-like syndrome. J. Allergy Clin. Immunol. 131:1611–1623 10.1016/j.jaci.2012.11.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Veerdonk F.L., Plantinga T.S., Hoischen A., Smeekens S.P., Joosten L.A., Gilissen C., Arts P., Rosentul D.C., Carmichael A.J., Smits-van der Graaf C.A., et al. . 2011. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N. Engl. J. Med. 365:54–61 10.1056/NEJMoa1100102 [DOI] [PubMed] [Google Scholar]
- Vidlak D., and Kielian T.. 2012. Differential effects of interleukin-17 receptor signaling on innate and adaptive immunity during central nervous system bacterial infection. J. Neuroinflammation. 9:128 10.1186/1742-2094-9-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinh D.C.2011. Insights into human antifungal immunity from primary immunodeficiencies. Lancet Infect. Dis. 11:780–792 10.1016/S1473-3099(11)70217-1 [DOI] [PubMed] [Google Scholar]
- Weaver C.T., Hatton R.D., Mangan P.R., and Harrington L.E.. 2007. IL-17 family cytokines and the expanding diversity of effector T cell lineages. Annu. Rev. Immunol. 25:821–852 10.1146/annurev.immunol.25.022106.141557 [DOI] [PubMed] [Google Scholar]
- Wildbaum G., Shahar E., Katz R., Karin N., Etzioni A., and Pollack S.. 2013. Continuous G-CSF therapy for isolated chronic mucocutaneous candidiasis: complete clinical remission with restoration of IL-17 secretion. J. Allergy Clin. Immunol. 132:761–764 10.1016/j.jaci.2013.04.018 [DOI] [PubMed] [Google Scholar]
- Wright J.F., Bennett F., Li B., Brooks J., Luxenberg D.P., Whitters M.J., Tomkinson K.N., Fitz L.J., Wolfman N.M., Collins M., et al. . 2008. The human IL-17F/IL-17A heterodimeric cytokine signals through the IL-17RA/IL-17RC receptor complex. J. Immunol. 181:2799–2805 10.4049/jimmunol.181.4.2799 [DOI] [PubMed] [Google Scholar]
- Yamazaki Y., Yamada M., Kawai T., Morio T., Onodera M., Ueki M., Watanabe N., Takada H., Takezaki S., Chida N., et al. . 2014. Two novel gain-of-function mutations of STAT1 responsible for chronic mucocutaneous candidiasis disease: impaired production of IL-17A and IL-22, and the presence of anti-IL-17F autoantibody. J. Immunol. 193:4880–4887 10.4049/jimmunol.1401467 [DOI] [PubMed] [Google Scholar]